Orthodontic Aligner Incorporating Eucommia ulmoides Exerts Low Continuous Force: In Vitro Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
2.2. Characterization of Eucommia Elastomer
2.3. Evaluation of Orthodontic Force
2.4. Multi-Bracket Orthodontic Appliance Model
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ponitz, R.J. Invisible retainers. Am. J. Orthod. 1971, 59, 266–272. [Google Scholar] [CrossRef]
- A McNamara, J.; Kramer, K.L.; Juenker, J.P. Invisible retainers. J. Clin. Orthod. JCO 1985, 19, 570–578. [Google Scholar] [PubMed]
- Sheridan, J.J. The Essix bracket choice appliance. J. Clin. Orthod. JCO 1996, 30, 203–205. [Google Scholar] [PubMed]
- Zhang, N.; Bai, Y.; Ding, X.; Zhang, Y. Preparation and characterization of thermoplastic materials for invisible orthodontics. Dent. Mater. J. 2011, 30, 954–959. [Google Scholar] [CrossRef] [Green Version]
- Sanchez, J.F.; Ramirez, I.P.; Alonso, J.M. Osamu active retainer for correction of mild relapse. J. Clin. Orthod. JCO 1998, 32, 26–28. [Google Scholar]
- Zawawi, K.H. Orthodontic Treatment of a Mandibular Incisor Extraction Case with Invisalign. Case Rep. Dent. 2014, 2014, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Frongia, G.; Castroflorio, T. Correction of severe tooth rotations using clear aligners: A case report. Aust. Orthod. J. 2012, 28, 245–249. [Google Scholar]
- Schupp, W.; Haubrich, J.; Neumann, I. Treatment of anterior open bite with the Invisalign system. J. Clin. Orthod. JCO 2010, 44, 501–507. [Google Scholar]
- Giancotti, A.; Mampieri, G.; Greco, M. Correction of deep bite in adults using the Invisalign system. J. Clin. Orthod. JCO 2008, 42, 719–726. [Google Scholar]
- Lombardo, L.; Martines, E.; Mazzanti, V.; Arreghini, A.; Mollica, F.; Siciliani, G. Stress relaxation properties of four orthodontic aligner materials: A 24-hour in vitro study. Angle Orthod. 2017, 87, 11–18. [Google Scholar] [CrossRef] [Green Version]
- Sokolowski, W.; Metcalfe, A.; Hayashi, S.; Yahia, L.; Raymond, J. Medical applications of shape memory polymers. Biomed. Mater. 2007, 2, S23–S27. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.-W.; Echarri, P. Clear aligner: An efficient, esthetic, and comfortable option for an adult patient. World J. Orthod. 2007, 8, 13–18. [Google Scholar]
- Nakazawa, Y.; Takeda, T.; Suzuki, N.; Hayashi, T.; Harada, Y.; Bamba, T.; Kobayashi, A. Histochemical study of trans-polyisoprene accumulation by spectral confocal laser scanning microscopy and a specific dye showing fluorescence solvatochromism in the rubber-producing plant, Eucommia ulmoides Oliver. Planta 2013, 238, 549–560. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.; Zhang, N.; Chen, H.; Bai, Y. Dynamic stress relaxation of orthodontic thermoplastic materials in a simulated oral environment. Dent. Mater. J. 2013, 32, 946–951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ryokawa, H.; Miyazaki, Y.; Fujishima, A.; Miyazaki, T.; Maki, K. The mechanical properties of dental thermoplastic materials in a simulated intraoral environment. Orthod. Waves 2006, 65, 64–72. [Google Scholar] [CrossRef]
- Kwon, J.-S.; Lee, Y.-K.; Lim, B.-S.; Lim, Y.-K. Force delivery properties of thermoplastic orthodontic materials. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 228–234. [Google Scholar] [CrossRef]
- Iijima, M.; Kohda, N.; Kawaguchi, K.; Muguruma, T.; Ohta, M.; Naganishi, A.; Murakami, T.; Mizoguchi, I. Effects of temperature changes and stress loading on the mechanical and shape memory properties of thermoplastic materials with different glass transition behaviours and crystal structures. Eur. J. Orthod. 2015, 37, 665–670. [Google Scholar] [CrossRef]
- Inoue, S.; Yamaguchi, S.; Uyama, H.; Yamashiro, T.; Imazato, S. Influence of constant strain on the elasticity of thermoplastic orthodontic materials. Dent. Mater. J. 2020, 39, 415–421. [Google Scholar] [CrossRef] [Green Version]
- Li, X.; Ren, C.; Wang, Z.; Zhao, P.; Wang, H.; Bai, Y. Changes in force associated with the amount of aligner activation and lingual bodily movement of the maxillary central incisor. Korean J. Orthod. 2016, 46, 65–72. [Google Scholar] [CrossRef] [Green Version]
- Barbagallo, L.J.; Shen, G.; Jones, A.S.; Swain, M.; Petocz, P.; Darendeliler, M.A. A Novel Pressure Film Approach for Determining the Force Imparted by Clear Removable Thermoplastic Appliances. Ann. Biomed. Eng. 2007, 36, 335–341. [Google Scholar] [CrossRef] [Green Version]
- Hahn, W.; Fialka-Fricke, J.; Dathe, H.; Fricke-Zech, S.; Zapf, A.; Gruber, R.; Kubein-Meesenburg, D.; Sadat-Khonsari, R. Initial forces generated by three types of thermoplastic appliances on an upper central incisor during tipping. Eur. J. Orthod. 2009, 31, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Elkholy, F.; Panchaphongsaphak, T.; Kilic, F.; Schmidt, F.; Lapatki, B. Forces and moments delivered by PET-G aligners to an upper central incisor for labial and palatal translation. J. Orofac. Orthop./Fortschr. Kieferorthop. 2015, 76, 460–475. [Google Scholar] [CrossRef] [PubMed]
- Kohda, N.; Iijima, M.; Muguruma, T.; A Brantley, W.; Ahluwalia, K.S.; Mizoguchi, I. Effects of mechanical properties of thermoplastic materials on the initial force of thermoplastic appliances. Angle Orthod. 2012, 83, 476–483. [Google Scholar] [CrossRef]
- Dentistry. Polymer-based restorative materials. BSI Br. Stand 2013. [Google Scholar] [CrossRef]
- ISO527-2:2012. Plastics—Determination of Tensile Properties—Part 2: Test Conditions for Moulding and Extrusion Plastics; International Organization for Standardization: Chiswik, London, UK, 2012. [Google Scholar]
- Proffit, W.R.; Fields, H.W.; Sarver, D.M. Contemporary Orthodontics, 4th ed.; Mosby Elsevier: St. Louis, MO, USA, 2007. [Google Scholar]
- Reitan, K. Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am. J. Orthod. 1967, 53, 721–745. [Google Scholar] [CrossRef]
- Chan, E.; Darendeliler, M.A. Physical properties of root cementum: Part 7. Extent of root resorption under areas of compression and tension. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 504–510. [Google Scholar] [CrossRef]
- Schwarz, A.M. Tissue changes incidental to orthodontic tooth movement. Int. J. Orthod. Oral Surg. Radiogr. 1932, 18, 331–352. [Google Scholar] [CrossRef]
- Jepsen, A. Root Surface Measurement and A Method for X-Ray Determination of Root Surface Area. Acta Odontol. Scand. 1963, 21, 35–46. [Google Scholar] [CrossRef]
- Gay, G.; Ravera, S.; Castroflorio, T.; Garino, F.; Rossini, G.; Parrini, S.; Cugliari, G.; Deregibus, A.P. Root resorption during orthodontic treatment with Invisalign®: A radiometric study. Prog. Orthod. 2017, 18, 12. [Google Scholar] [CrossRef]
- Iglesias-Linares, A.; Sonnenberg, B.; Solano, B.; Yañez-Vico, R.-M.; Solano, E.; Lindauer, S.J.; Flores-Mir, C. Orthodontically induced external apical root resorption in patients treated with fixed appliances vs removable aligners. Angle Orthod. 2017, 87, 3–10. [Google Scholar] [CrossRef]
- Al-Qawasmi, R.; Hartsfield, J.; Everett, E.; Flury, L.; Liu, L.; Foroud, T.; Macri, J.; Roberts, W. Genetic predisposition to external apical root resorption in orthodontic patients: Linkage of chromosome-18 marker. J. Dent. Res. 2003, 82, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Brin, I.; Tulloch, J.; Koroluk, L.; Philips, C. External apical root resorption in Class II malocclusion: A retrospective review of 1- versus 2-phase treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 151–156. [Google Scholar] [CrossRef]
- Han, G.; Huang, S.; Hoff, J.W.V.D.; Zeng, X.; Kuijpers-Jagtman, A.M. Root resorption after orthodontic intrusion and extrusion: An intraindividual study. Angle Orthod. 2005, 75, 912–918. [Google Scholar] [PubMed]
- Harris, D.A.; Jones, A.S.; Darendeliler, M.A. Physical properties of root cementum: Part 8. Volumetric analysis of root resorption craters after application of controlled intrusive light and heavy orthodontic forces: A microcomputed tomography scan study. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Raja, T.A.; Littlewood, S.J.; Munyombwe, T.; Bubb, N.L. Wear resistance of four types of vacuum-formed retainer materials: A laboratory study. Angle Orthod. 2014, 84, 656–664. [Google Scholar] [CrossRef] [PubMed]
- Gardner, G.D.; Dunn, W.J.; Taloumis, L. Wear comparison of thermoplastic materials used for orthodontic retainers. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 294–297. [Google Scholar] [CrossRef]
- Eliades, T.; Bourauel, C. Intraoral aging of orthodontic materials: The picture we miss and its clinical relevance. Am. J. Orthod. Dentofac. Orthop. 2005, 127, 403–412. [Google Scholar] [CrossRef]
- ISO 10993-5:2009. Biological Evaluation of Medical Devices—Part 5: Tests for In Vitro Cytotoxicity; International Organization for Standardization: Chiswik, London, UK, 2009. [Google Scholar]
- ISO 10993-10:2010. Biological Evaluation of Medical Devices—Part 10: Tests for Irritation and Skin Sensitization; International Organization for Standardization: Chiswik, London, UK, 2010. [Google Scholar]







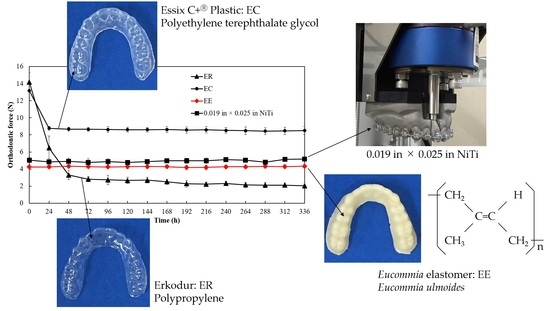
| Product | Code | Manufacturer | Composition |
|---|---|---|---|
| Erkodur | ER | Erkodent Erich Kopp GmbH | Polyethylene terephthalate glycol (PETG) |
| Essix C+® Plastic | EC | DENTSPLY Raintree Essix | Polypropylene (PP) |
| Eucommia elastomer | EE | Hitachi Zosen | Eucommia ulmoides |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inoue, S.; Yamaguchi, S.; Uyama, H.; Yamashiro, T.; Imazato, S. Orthodontic Aligner Incorporating Eucommia ulmoides Exerts Low Continuous Force: In Vitro Study. Materials 2020, 13, 4085. https://doi.org/10.3390/ma13184085
Inoue S, Yamaguchi S, Uyama H, Yamashiro T, Imazato S. Orthodontic Aligner Incorporating Eucommia ulmoides Exerts Low Continuous Force: In Vitro Study. Materials. 2020; 13(18):4085. https://doi.org/10.3390/ma13184085
Chicago/Turabian StyleInoue, Sayuri, Satoshi Yamaguchi, Hiroshi Uyama, Takashi Yamashiro, and Satoshi Imazato. 2020. "Orthodontic Aligner Incorporating Eucommia ulmoides Exerts Low Continuous Force: In Vitro Study" Materials 13, no. 18: 4085. https://doi.org/10.3390/ma13184085
APA StyleInoue, S., Yamaguchi, S., Uyama, H., Yamashiro, T., & Imazato, S. (2020). Orthodontic Aligner Incorporating Eucommia ulmoides Exerts Low Continuous Force: In Vitro Study. Materials, 13(18), 4085. https://doi.org/10.3390/ma13184085