Autologous Fat Transfer for Esthetic Contouring of Face in Posttraumatic Nonfunctional Maxillofacial Deformities
Abstract
:Materials and Methods
Surgical Procedure
- Under general anesthesia, patients were prepared with all aseptic precautions. For infiltration of donor site (medial aspect of thigh), we prepare a mixture of 500 mL of Ringer’s lactate and 0.5 mL of 1:1000 adrenaline. This solution was infiltrated as required.
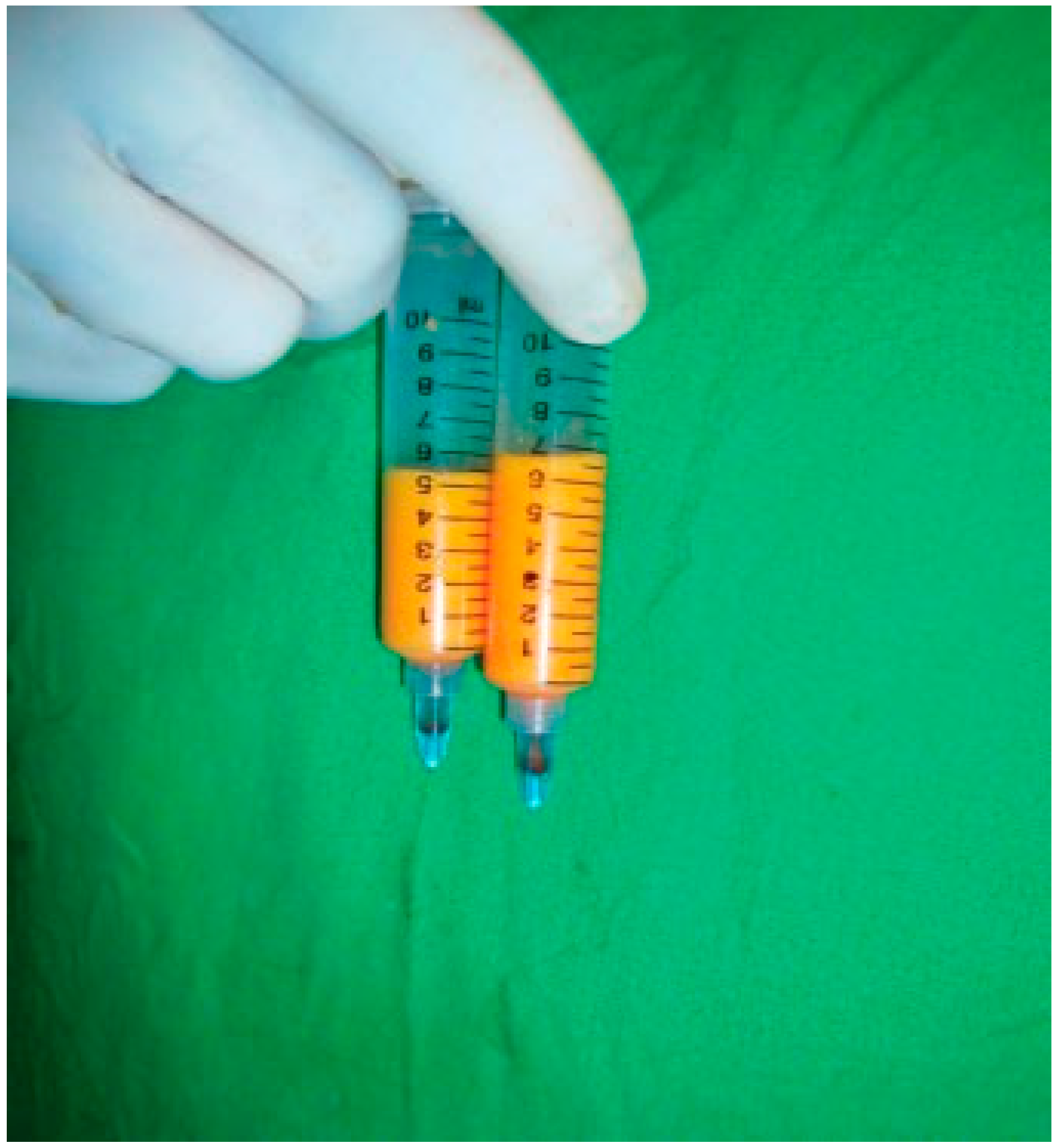
- After a waiting period of a minimum 20 min, fat harvesting was done by manual aspiration using Sydney Coleman aspiration system which consists of a 3-mm bore cannula attached to a 10-mL Luer lock syringe (Figure 1).
- Same 10-mL syringe is used for its placement in manual centrifuge apparatus (Figure 2). Speed of manual centrifuge, as measured by digital tachometer, does not exceed 500 RPM (revolutions per minute). Centrifugation was thus performed at 500 RPM for 2 min.
- The aspirate after centrifuge form three layers (Figure 3):
- The upper oily layer of fatty acids.
- The intermediate layer consists of adipocytes cell mass.
- The lower one is the dark red mass of packed red blood cells.

- Placement of the fat: A 3- or 2-mL Luer lock syringe with blunt tipped cannula of 3-mm bore attached to its nozzle is used. Through small stab incision, the cannula is used to create subcutaneous tunnels in a fan-shaped manner into which the fat cells are deposited as the cannula is withdrawn. In cases of fat grafting in scarred tissue, subcision was done using 16-gauge needle. Over correction of ~25% was done considering postoperative resorption.
- Postoperative care:
- Broad-spectrum antibiotic and anti-inflammatory drugs for 1 week.
- The patient should be in semi sitting position to decrease the amount of edema.
- Routine cold fermentation was advised to enhance resolution of ecchymosis and postoperative edema.
- Application of antibiotic cream over the incision site twice daily.
- Patient was asked to avoid pressure or massage over grafted site.
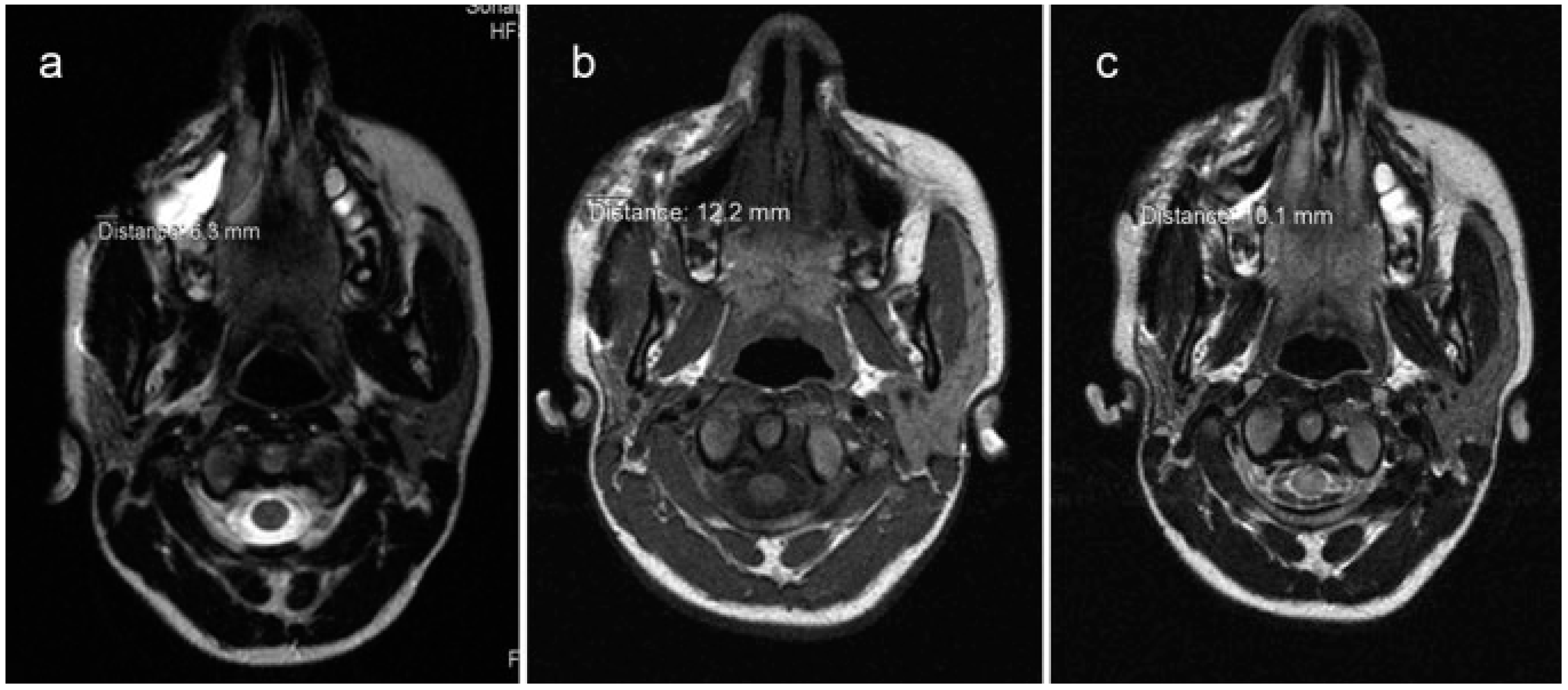
- Follow-up: Every case was subjected to postoperative photography biweekly for 3 months and subsequently at 6th month, 1 year, and 2 years postoperatively. Postoperative MRI was taken at 1st and 12th months.
- The presence of notable asymmetries in terms of volume of the treated areas (Yes/No)
- The presence of nodules, infection, thickened areas, ecchymosis, or pain on either side or any other postoperative complications (Yes/No)
- Their level of satisfaction scoring from 0 (very bad) to 10 (very good)


Results
Clinical Evaluation
Radiographic Evaluation
Discussion
| Sr. No. | Questions | Options | Answers | Remarks | |
|---|---|---|---|---|---|
| I. Subjective Evaluation | 1 | The presence of notable asymmetries in terms of volume of the treated areas after 1st surgery | Yes | 4/25 | 16% |
| No | 21/25 | 84% | |||
| 2 | Postoperative complications | Yes | 1/25 | 4% | |
| No | 24/25 | 96% | |||
| 3 | Level of satisfaction | 0 (very bad) to 10 (very good) | Mean score | Very good | |
| 9.1 | |||||
| II. | Objective assessment | 0 (very bad) to 10 (very good) | Mean score | Good | |
| 8.8 | |||||







| Sr. No. | Measurement in Preoperative Scan (mm) (A) | Measurement in 1 mo Postoperative Scan (mm) (B) | Measurement in 1 y Postoperative Scan (mm) (C) | Difference Between B and C (Expressed in %) |
|---|---|---|---|---|
| 1 | 0.5 | 6.7 | 5.2 | 22.39 |
| 2 | 3.4 | 10.0 | 7.8 | 22 |
| 3 | 1.8 | 4.5 | 2.8 | 37.77 |
| 4 | 2.9 | 6.3 | 3.9 | 38.09 |
| 5 | 6.3 | 12.2 | 10.1 | 17.21 |
| 6 | 2.4 | 6.0 | 3.9 | 35 |
| 7 | 1.3 | 7.4 | 5.8 | 21.62 |
| 8 | 2.5 | 7.5 | 4.8 | 36 |
| 9 | 3.9 | 8.0 | 6.8 | 15 |
| 10 | 6.1 | 13.0 | 11.2 | 13.84 |
| 11 | 7.2 | 13.1 | 10.6 | 19.08 |
| 12 | 2.4 | 7.2 | 6.0 | 16.67 |
| 13 | 3.1 | 7.0 | 6.7 | 18.57 |
| 14 | 6.0 | 12.0 | 10.3 | 14.16 |
| 15 | 1.3 | 8.3 | 6.3 | 24.09 |
| 16 | 2.0 | 5.1 | 5.0 | 1.96 |
| 17 | 3.0 | 7.1 | 6.0 | 15.49 |
| 18 | 2.2 | 8.1 | 5.9 | 27.16 |
| 19 | 5.2 | 12.2 | 10.1 | 17.21 |
| 20 | 1.8 | 11.2 | 9.0 | 19.64 |
| 21 | 5.0 | 12.0 | 9.3 | 22.50 |
| 22 | 4.7 | 9.4 | 7.3 | 22.34 |
| 23 | 3.9 | 6.8 | 4.9 | 27.94 |
| 24 | 7.1 | 12.6 | 11.1 | 11.90 |
| 25 | 4.2 | 11.2 | 8.0 | 28.57 |
| Mean | 21.85 | |||
Conclusions
References
- Neuber, G. Fett transplantation. Chir Kongr Verhandt Deutsche Gesellsch Chir 1893, 22, 66. [Google Scholar]
- Miller, C.G. Cannula Implants and Review of Implantation Techniques in Esthetic Surgery; Oak Press: Chicago, IL, USA, 1926. [Google Scholar]
- Peer, L.A. Loss of weight and volume in human fat grafts. Plast Reconstr Surg 1950, 5, 217–230. [Google Scholar] [CrossRef]
- Coleman, S.R. Structural fat grafting. Aesthet Surg J 1998, 18, 386–388. [Google Scholar] [CrossRef]
- Niechajev, I.; Sevćuk, O. Long-term results of fat transplantation: Clinical and histologic studies. Plast Reconstr Surg 1994, 94, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Pinski, K.S.; Roenigk, H.H., Jr. Autologous fat transplantation. Longterm follow-up. J Dermatol Surg Oncol 1992, 18, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Chajchir, A.; Benzaquen, I. Fat-grafting injection for soft-tissue augmentation. Plast Reconstr Surg 1989, 84, 921–934, discussion 935. [Google Scholar] [CrossRef]
- Illouz, Y.G. The fat cell “graft”: A new technique to fill depressions. Plast Reconstr Surg 1986, 78, 122–123. [Google Scholar] [CrossRef]
- Coleman, S.R. Structural fat grafts: The ideal filler? Clin Plast Surg 2001, 28, 111–119. [Google Scholar] [CrossRef]
- Nguyen, A.; Pasyk, K.A.; Bouvier, T.N.; Hassett, C.A.; Argenta, L.C. Comparative study of survival of autologous adipose tissue taken and transplanted by different techniques. Plast Reconstr Surg 1990, 85, 378–386, discussion 387–389. [Google Scholar] [CrossRef]
- Boyce, R.G.; Nuss, D.W.; Kluka, E.A. The use of autogenous fat, fascia, and nonvascularized muscle grafts in the head and neck. Otolaryngol Clin North Am 1994, 27, 39–68. [Google Scholar] [CrossRef]
- Matsudo, P.K.; Toledo, L.S. Experience of injected fat grafting. Aesthetic Plast Surg 1988, 12, 35–38. [Google Scholar] [CrossRef]
- Ersek, R.A. Transplantation of purified autologous fat: A 3-year follow-up is disappointing. Plast Reconstr Surg 1991, 87, 219–227, discussion 228. [Google Scholar] [CrossRef] [PubMed]
- Fournier, P.F. Fat grafting: My technique. Dermatol Surg 2000, 26, 1117–1128. [Google Scholar] [CrossRef]
- Coleman, S.R. Long-term survival of fat transplants: Controlled demonstrations. Aesthetic Plast Surg 1995, 19, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Pu, L.L.; Cui, X.; Fink, B.F.; Cibull, M.L.; Gao, D. The viability of fatty tissues within adipose aspirates after conventional liposuction: A comprehensive study. Ann Plast Surg 2005, 54, 288–292, discussion 292. [Google Scholar]
- Smith, P.; Adams, W.P., Jr.; Lipschitz, A.H.; et al. Autologous human fat grafting: Effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg 2006, 117, 1836–1844. [Google Scholar] [CrossRef] [PubMed]
- Coleman, S.R. Facial augmentation with structural fat grafting. Clin Plast Surg 2006, 33, 567–577. [Google Scholar] [CrossRef]
- Wolf, G.A.; Gallego, S.; Patrón, A.S.; et al. Magnetic resonance imaging assessment of gluteal fat grafts. Aesthetic Plast Surg 2006, 30, 460–468. [Google Scholar] [CrossRef]
- Swanson, E. Malar augmentation assessed by magnetic resonance imaging in patients after face lift and fat injection. Plast Reconstr Surg 2011, 127, 2057–2065. [Google Scholar] [CrossRef]
- Saleh, Y.; Mostafa, H. Clinical and radiological assessment of fat transplantation using centrifuge technique. Egypt J Plast Reconstr Surg 2005, 29, 129–133. [Google Scholar]
- Hörl, H.W.; Feller, A.M.; Biemer, E. Technique for liposuction fat reimplantation and long-term volume evaluation by magnetic resonance imaging. Ann Plast Surg 1991, 26, 248–258. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the author. The Author(s) 2015.
Share and Cite
Agrawal, K.S.; Bachhav, M.; Naik, C.S.; Tanwar, H.; Sankhe, S.S. Autologous Fat Transfer for Esthetic Contouring of Face in Posttraumatic Nonfunctional Maxillofacial Deformities. Craniomaxillofac. Trauma Reconstr. 2016, 9, 113-120. https://doi.org/10.1055/s-0035-1566163
Agrawal KS, Bachhav M, Naik CS, Tanwar H, Sankhe SS. Autologous Fat Transfer for Esthetic Contouring of Face in Posttraumatic Nonfunctional Maxillofacial Deformities. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(2):113-120. https://doi.org/10.1055/s-0035-1566163
Chicago/Turabian StyleAgrawal, Kapil S., Manoj Bachhav, Charudatta S. Naik, Harshwardhan Tanwar, and Shilpa S. Sankhe. 2016. "Autologous Fat Transfer for Esthetic Contouring of Face in Posttraumatic Nonfunctional Maxillofacial Deformities" Craniomaxillofacial Trauma & Reconstruction 9, no. 2: 113-120. https://doi.org/10.1055/s-0035-1566163
APA StyleAgrawal, K. S., Bachhav, M., Naik, C. S., Tanwar, H., & Sankhe, S. S. (2016). Autologous Fat Transfer for Esthetic Contouring of Face in Posttraumatic Nonfunctional Maxillofacial Deformities. Craniomaxillofacial Trauma & Reconstruction, 9(2), 113-120. https://doi.org/10.1055/s-0035-1566163



