Tomographic Evaluation of Mandibular Thickness on Premolar and Molar Regions Related to Monocortical Screws
Abstract
:Materials and Methods
Patients, Sample, and Imaging Acquisition
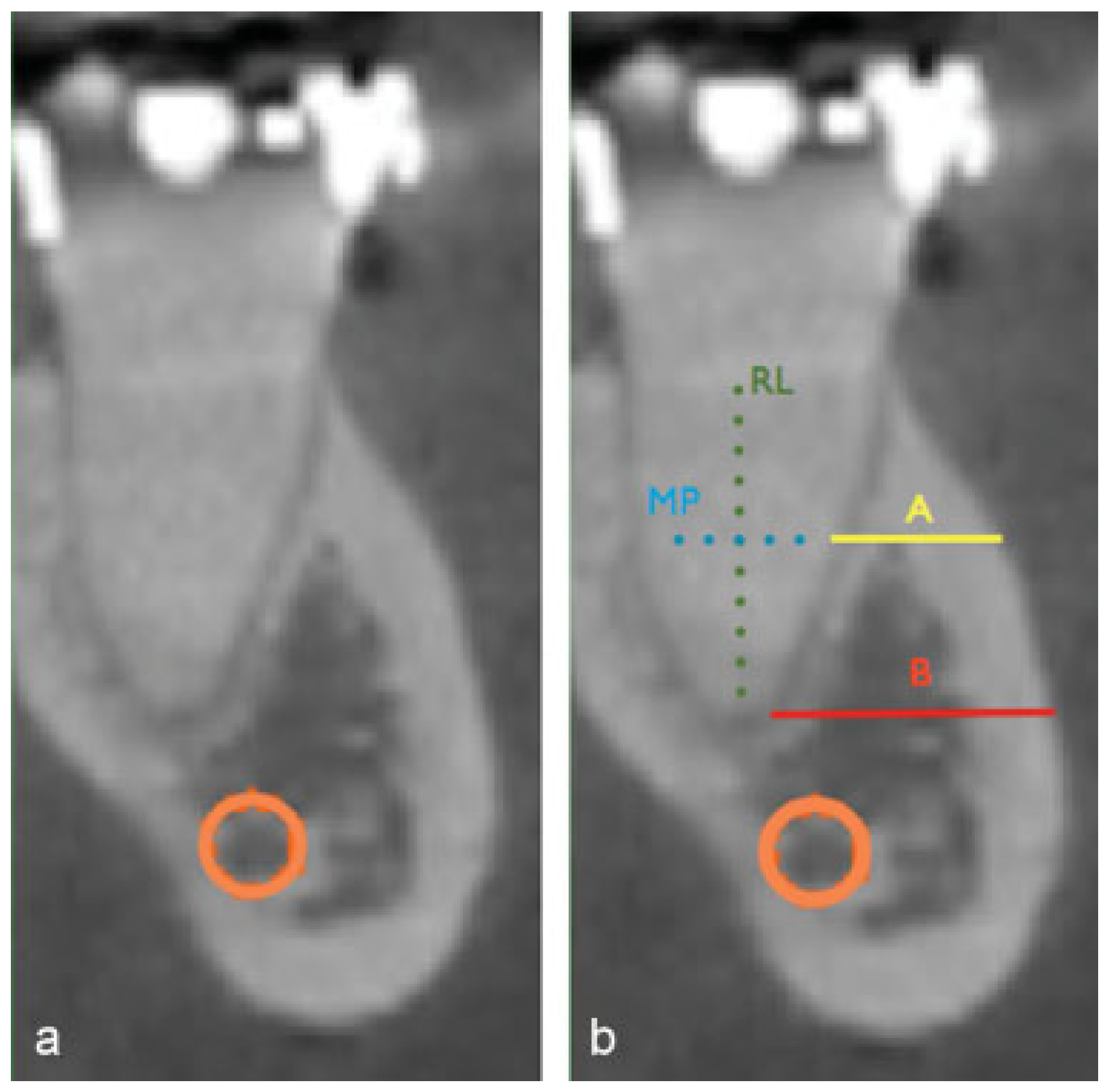
Measuring Protocol
- •
- Root length (RL): vertical distance between bone crest and the end of root
- •
- Mean point (MP): the mean distance of RL.
- •
- Distance A (A): horizontal distance from the external cortical plate to the root surface measured at the MP point.
- •
- Distance B (B): horizontal distance from the external cortical plate to the root surface measured at the root apex.
Statistical Analysis
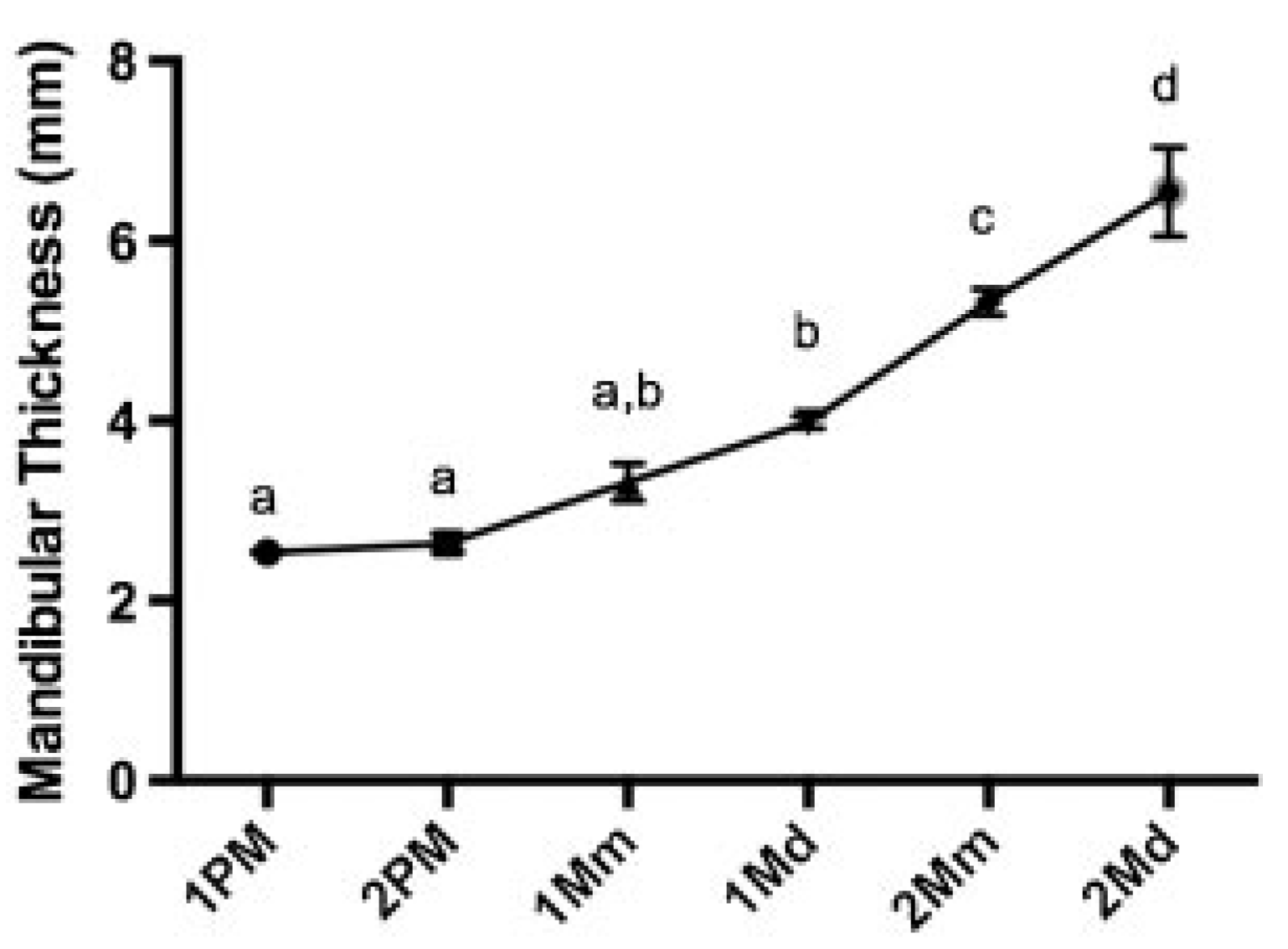
Results
Discussion
References
- Bhatnagar, A.; Bansal, V.; Kumar, S.; Mowar, A. Comparative analysis of osteosynthesis of mandibular anterior fractures following open reduction using ‘stainless steel lag screws and mini plates’. J. Maxillofac. Oral. Surg. 2013, 12, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Gadre, K.S.; Halli, R.; Joshi, S.; et al. Incidence and pattern of craniomaxillofacial injuries: A 22 year retrospective analysis of cases operated at major trauma hospitals/centres in Pune, India. J. Maxillofac. Oral. Surg. 2013, 12, 372–378. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III. Rigid skeletal fixation of fractures. J. Oral. Maxillofac. Surg. 1993, 51, 163–173. [Google Scholar] [CrossRef]
- Goyal, M.; Jhamb, A.; Chawla, S.; Marya, K.; Dua, J.S.; Yadav, S. A comparative evaluation of fixation techniques in anterior mandibular fractures using 2.0 mm monocortical titanium miniplates versus 2.4 mm cortical titanium lag screws. J. Maxillofac. Oral. Surg. 2012, 11, 442–450. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Chen, S.; Threadgill, J.M. Small and large titanium plates are equally effective for treating mandible fractures. J Oral Maxillofac Surg 2012, 70, 1613–1621. [Google Scholar] [CrossRef]
- Sato, F.R.; Asprino, L.; Noritomi, P.Y.; da Silva, J.V.; de Moraes, M. Comparison of five different fixation techniques of sagittal split ramus osteotomy using three-dimensional finite elements analysis. Int J Oral Maxillofac Surg 2012, 41, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Taub, D.; Tursun, R.; Gold, L.; Jamal, B.T. Nonunion of mandibular midline osteotomy after tumor surgery and radiation repaired by endosseous implants. J Oral Maxillofac Surg 2010, 68, 833–836. [Google Scholar] [CrossRef]
- Wang, W.H.; Deng, J.Y.; Zhu, J.; Li, M.; Xia, B.; Xu, B. Computer-assisted virtual technology in intracapsular condylar fracture with two resorbable long-screws. Br. J. Oral. Maxillofac. Surg. 2013, 51, 138–143. [Google Scholar] [CrossRef]
- Seemann, R.; Schicho, K.; Wutzl, A.; et al. Complication rates in the operative treatment of mandibular angle fractures: A 10-year retrospective. J. Oral. Maxillofac. Surg. 2010, 68, 647–650. [Google Scholar] [CrossRef] [PubMed]
- Martins, M.M.; Homsi, N.; Pereira, C.C.; Jardim, E.C.; Garcia, I.R., Jr. Epidemiologic evaluation of mandibular fractures in the Rio de Janeiro high-complexity hospital. J. Craniofac. Surg. 2011, 22, 2026–2030. [Google Scholar] [CrossRef]
- Oliver, R. Lag screw fixation of mandibular symphysis fractures is associated with fewer post-operative complications compared to plates and screws. J. Evid. Based Dent. Pract. 2013, 13, 20–21. [Google Scholar] [CrossRef] [PubMed]
- Paeng, J.Y.; Hong, J.; Kim, C.S.; Kim, M.J. Comparative study of skeletal stability between bicortical resorbable and titanium screw fixation after sagittal split ramus osteotomy for mandibular prognathism. J. Craniomaxillofac. Surg. 2012, 40, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Otsuka, T.; Shigematsu, M.; Goto, M. A long-term comparative study of two rigid internal fixation techniques in terms of masticatory function and neurosensory disturbance after mandibular correction by bilateral sagittal split ramus osteotomy. Int. J. Oral. Maxillofac. Surg. 2011, 40, 360–365. [Google Scholar] [CrossRef]
- Olivera, L.B.; Sant’ Ana, E.; Manzato, A.J.; Guerra, F.L.; Arnett, G.W. Biomechanical in vitro evaluation of three stable internal fixation techniques used in sagittal osteotomy of the mandibular ramus: A study in sheep mandibles. J. Appl. Oral. Sci. 2012, 20, 419–426. [Google Scholar] [CrossRef]
- Goyal, M.; Marya, K.; Chawla, S.; Pandey, R. Mandibular osteosynthesis: A comparative evaluation of two different fixation systems using 2.0 mm titanium miniplates & 3-D locking plates. J. Maxillofac. Oral. Surg. 2011, 10, 316–320. [Google Scholar] [PubMed]
- Pohlenz, P.; Blessmann, M.; Blake, F.; Gbara, A.; Schmelzle, R.; Heiland, M. Major mandibular surgical procedures as an indication for intraoperative imaging. J. Oral. Maxillofac. Surg. 2008, 66, 324–329. [Google Scholar] [CrossRef]
- Singh, G.; Mohammad, S.; Chak, R.K.; Lepcha, N.; Singh, N.; Malkunje, L.R. Bio-resorbable plates as effective implant in paediatric mandibular fracture. J. Maxillofac. Oral. Surg. 2012, 11, 400–406. [Google Scholar] [CrossRef]
- Kocaelli, H.A.; Kaptan, F.; Kayahan, B.; Haznedaroğlu, F. Management of the perforations due to miniplate application. J. Endod. 2006, 32, 482–485. [Google Scholar]
- Leite, G.M.; Lana, J.P.; de Carvalho Machado, V.; Manzi, F.R.; Souza, P.E.; Horta, M.C. Anatomic variations and lesions of the mandibular canal detected by cone beam computed tomography. Surg. Radiol. Anat. 2014, 36, 795–804. [Google Scholar] [CrossRef]
- Cutright, B.; Quillopa, N.; Schubert, W. An anthropometric analysis of the key foramina for maxillofacial surgery. J. Oral. Maxillofac. Surg. 2003, 61, 354–357. [Google Scholar] [CrossRef]
- Mensink, G.; Gooris, P.J.; Bergsma, E.J.; Frank, M.H.; van Gemert, J.T.; van Merkesteyn, J.P. Is the lingual fracture line influenced by the mandibular canal or the mylohyoid groove during a bilateral sagittal split osteotomy? A human cadaveric study. J. Oral. Maxillofac. Surg. 2014, 72, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Tsunori, M.; Mashita, M.; Kasai, K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. Angle Orthod. 1998, 68, 557–562. [Google Scholar] [PubMed]
- Rangel, F.A.; Maal, T.J.; Bronkhorst, E.M.; et al. Accuracy and reliability of a novel method for fusion of digital dental casts and cone beam computed tomography scans. PLoS ONE 2013, 8, e59130. [Google Scholar] [CrossRef] [PubMed]
- Monnerat, C.; Restle, L.; Mucha, J.N. Tomographic mapping of mandibular interradicular spaces for placement of orthodontic miniimplants. Am. J. Orthod. Dentofacial Orthop. 2009, 135, 428.e1–428.e9. [Google Scholar] [CrossRef]
- Ehrenfeld, M.; Manson, P.N.; Prein, J. Principles of Internal Fixation of Cramomaxillofacial Skeleton, 1st ed.; Thieme Medical Publishers/Maple Press, 2012; Volume 412. [Google Scholar]
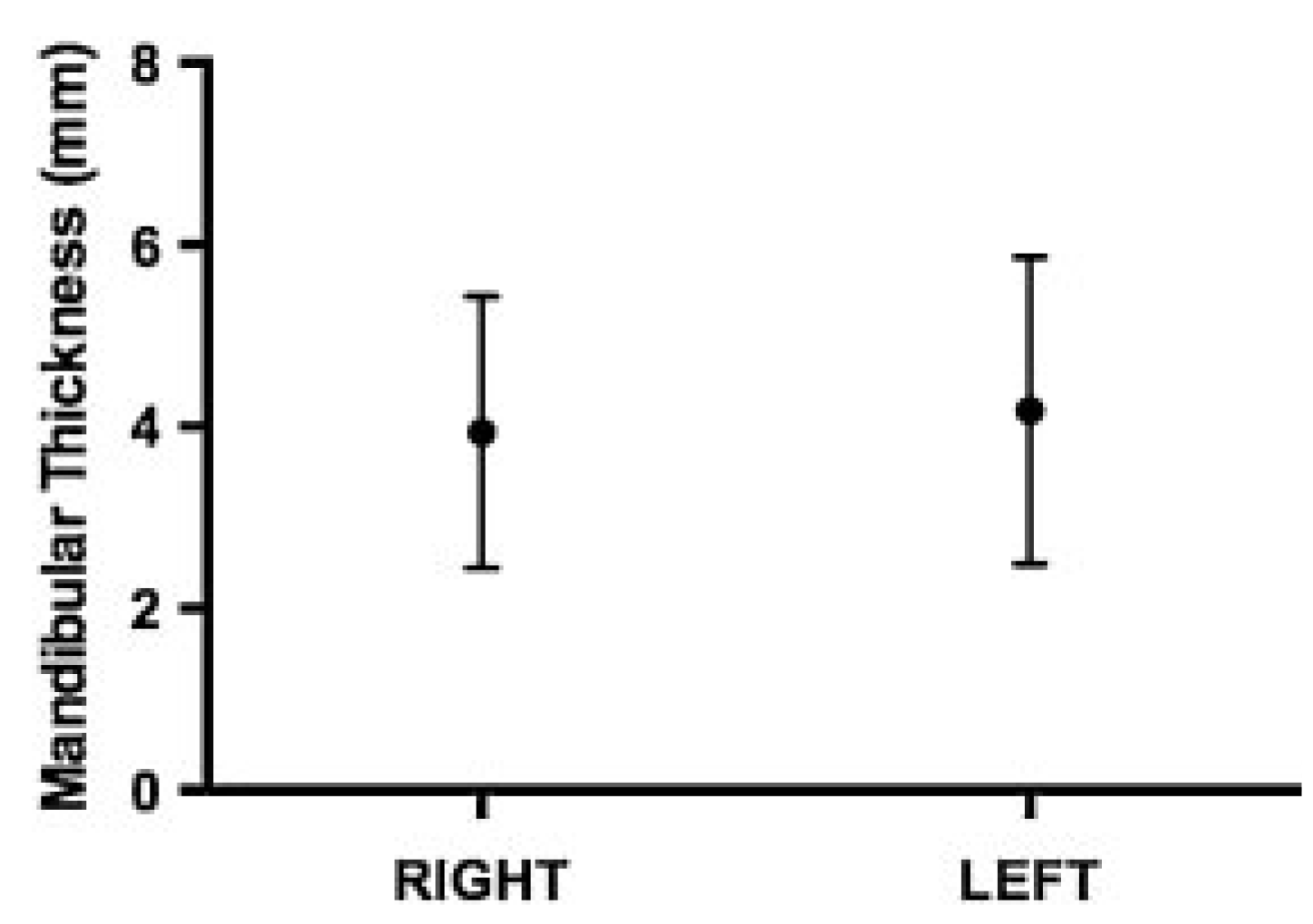
| Left | ||||||
| 1 PM | 2 PM | 1 Mm | 1 Md | 2 Mm | 2 Md | |
| Mean | 2.53 | 2.57 | 3.17 | 3.94 | 5.22 | 6.96 |
| Standard deviation | 1.05 | 1.33 | 1.65 | 1.87 | 2.34 | 2.18 |
| Upper | 5.12 | 4.67 | 6.23 | 8.00 | 10.80 | 10.65 |
| Lower | 1.09 | 0.96 | 1.05 | 1.33 | 1.25 | 1.08 |
| Median | 2.38 | 2.41 | 2.82 | 3.95 | 4.44 | 5.98 |
| Right | ||||||
| 1 PM | 2 PM | 1 Mm | 1 Md | 2 Mm | 2 Md | |
| Mean | 2.55 | 2.71 | 3.46 | 4.03 | 5.42 | 6.89 |
| Standard deviation | 1.07 | 1.25 | 1.66 | 1.55 | 1.94 | 1.88 |
| Upper | 4.79 | 6.23 | 6.71 | 6.80 | 9.75 | 11.78 |
| Lower | 0.84 | 0.63 | 1.11 | 1.68 | 1.93 | 3.66 |
| Median | 2.35 | 2.29 | 3.08 | 3.87 | 5.12 | 7.06 |
© 2015 by the author. The Author(s) 2015.
Share and Cite
Ribeiro, J.; Marin, C.; Homsi, N.; Rocha Junior, H.; Magacho, L.; Fidalgo, G.; Zanela, M. Tomographic Evaluation of Mandibular Thickness on Premolar and Molar Regions Related to Monocortical Screws. Craniomaxillofac. Trauma Reconstr. 2016, 9, 105-108. https://doi.org/10.1055/s-0035-1566162
Ribeiro J, Marin C, Homsi N, Rocha Junior H, Magacho L, Fidalgo G, Zanela M. Tomographic Evaluation of Mandibular Thickness on Premolar and Molar Regions Related to Monocortical Screws. Craniomaxillofacial Trauma & Reconstruction. 2016; 9(2):105-108. https://doi.org/10.1055/s-0035-1566162
Chicago/Turabian StyleRibeiro, Jonathan, Charles Marin, Nicolas Homsi, Hernando Rocha Junior, Luiz Magacho, Guto Fidalgo, and Manuella Zanela. 2016. "Tomographic Evaluation of Mandibular Thickness on Premolar and Molar Regions Related to Monocortical Screws" Craniomaxillofacial Trauma & Reconstruction 9, no. 2: 105-108. https://doi.org/10.1055/s-0035-1566162
APA StyleRibeiro, J., Marin, C., Homsi, N., Rocha Junior, H., Magacho, L., Fidalgo, G., & Zanela, M. (2016). Tomographic Evaluation of Mandibular Thickness on Premolar and Molar Regions Related to Monocortical Screws. Craniomaxillofacial Trauma & Reconstruction, 9(2), 105-108. https://doi.org/10.1055/s-0035-1566162



