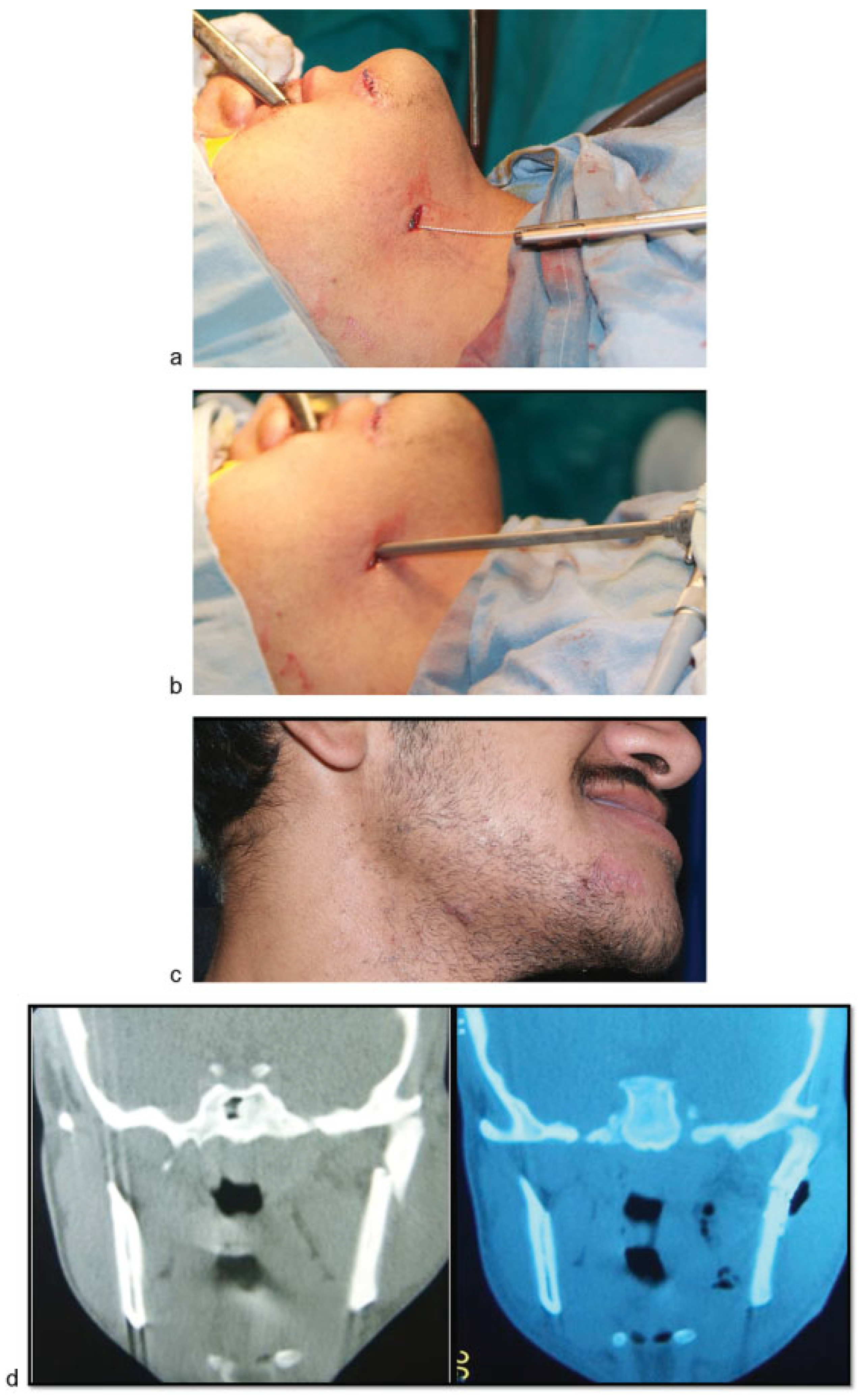
Minimizing the Submandibular Incision in Endoscopic Subcondylar Fracture Repair
Abstract
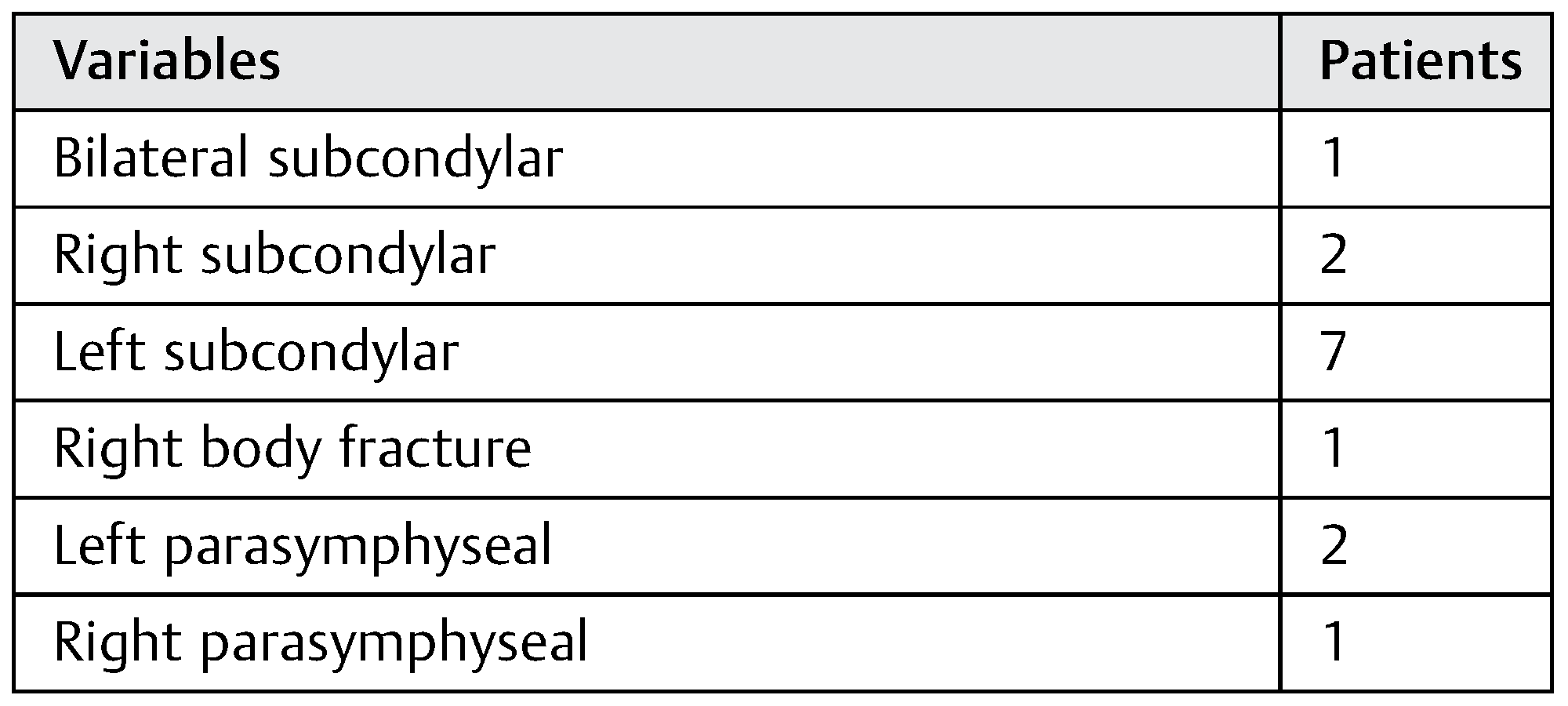
:Patients and Methods
Results
Discussion
Conclusion
References
- Schön, R.; Fakler, O.; Gellrich, N.C.; Schmelzeisen, R. Five-year experience with the transoral endoscopically assisted treatment of displaced condylar mandible fractures. Plast Reconstr Surg 2005, 116, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, D.A. A multicentre audit of unilateral fractures of the mandibular condyle. Br J Oral Maxillofac Surg 1997, 35, 230–236. [Google Scholar] [CrossRef]
- Silvennoinen, U.; Iizuka, T.; Lindqvist, C.; Oikarinen, K. Different patterns of condylar fractures: an analysis of 382 patients in a 3-year period. J Oral Maxillofac Surg 1992, 50, 1032–1037. [Google Scholar] [CrossRef] [PubMed]
- Stacey, D.H.; Doyle, J.F.; Mount, D.L.; Snyder, M.C.; Gutowski, K.A. Management of mandible fractures. Plast Reconstr Surg 2006, 117, 48e–60e. [Google Scholar] [CrossRef]
- Draaijers, L.J.; Tempelman, F.R.; Botman, Y.A.; et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg 2004, 113, 1960–1965, discussion 1966–1967. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.J.; Arora, B.; Dagum, A.; Valentine, S.; Hollander, J.E. Development and validation of a novel scar evaluation scale. Plast Reconstr Surg 2007, 120, 1892–1897. [Google Scholar] [CrossRef]
- Boutros, S.G. Closed reduction and fluoroscopically assisted percutaneous stabilization of displaced subcondylar mandible fractures. Plast Reconstr Surg 2005, 116, 971–977. [Google Scholar] [CrossRef]
- Silverman, S.L. New operation for displaced fractures at the neck of the condyle. Int J Orthod 1925, 67, 876. [Google Scholar]
- Wassmund, M. Uber Luxations frakturen des Kiefernglenkes. Dtsch Kieferchir. 1934, 1, 27. [Google Scholar]
- Haug, R.H.; Brandt, M.T. Closed reduction, open reduction, and endoscopic assistance: current thoughts on the management of mandibular condyle fractures. Plast Reconstr Surg 2007, 120 (Suppl. 2), 90S–102S. [Google Scholar] [CrossRef]
- Lauer, G.; Schmelzeisen, R. Endoscope-assisted fixation of mandibular condylar process fractures. J Oral Maxillofac Surg 1999, 57, 36–39, discussion 39–40. [Google Scholar] [CrossRef]
- Lee, C.; Stiebel, M.; Young, D.M. Cranial nerve VII region of the traumatized facial skeleton: optimizing fracture repair with the endoscope. J Trauma 2000, 48, 423–431, discussion 431–432. [Google Scholar] [CrossRef]
- Sandler, N.A.; Andreasen, K.H.; Johns, F.R. The use of endoscopy in the management of subcondylar fractures of the mandible: a cadaver study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999, 88, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Schön, R.; Schmelzeisen, R. Endoscopic fracture treatment. Ann R Australas Coll Dent Surg 2002, 16, 40–45. [Google Scholar] [PubMed]
- Mueller, R. Endoscopic treatment of facial fractures. Facial Plast Surg 2008, 24, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Schmelzeisen, R.; Lauer, G.; Wichmann, U. Endoscope-assisted fixation of condylar fractures of the mandible [in German]. Mund Kiefer Gesichtschir 1998, 2 (Suppl. 1), S168–S170. [Google Scholar] [CrossRef]
- Schön, R.; Gutwald, R.; Schramm, A.; Gellrich, N.C.; Schmelzeisen, R. Endoscopy-assisted open treatment of condylar fractures of the mandible: extraoral vs intraoral approach. Int J Oral Maxillofac Surg 2002, 31, 237–243. [Google Scholar] [CrossRef]
- Kellman, R.M. Endoscopic approach to subcondylar mandible fractures. Facial Plast Surg 2004, 20, 239–247. [Google Scholar] [CrossRef]
- Chen, C.T.; Lai, J.P.; Tung, T.C.; Chen, Y.R. Endoscopically assisted mandibular subcondylar fracture repair. Plast Reconstr Surg 1999, 103, 60–65. [Google Scholar] [CrossRef]
- Honda, T.; Nozaki, M.; Isono, N.; Sasaki, K. Endoscope-assisted facial fracture repair. World J Surg 2001, 25, 1075–1083. [Google Scholar] [CrossRef]
- Sandler, N.A. Endoscopic-assisted reduction and fixation of a mandibular subcondylar fracture: report of a case. J Oral Maxillofac Surg 2001, 59, 1479–1482. [Google Scholar] [CrossRef] [PubMed]
- Miloro, M. Endoscopic-assisted repair of subcondylar fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003, 96, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Schön, R.; Schramm, A.; Gellrich, N.C.; Schmelzeisen, R. Follow-up of condylar fractures of the mandible in 8 patients at 18 months after transoral endoscopic-assisted open treatment. J Oral Maxillofac Surg 2003, 61, 49–54. [Google Scholar] [CrossRef]
- Troulis, M.J. Endoscopic open reduction and internal rigid fixation of subcondylar fractures. J Oral Maxillofac Surg 2004, 62, 1269–1271. [Google Scholar] [CrossRef]
- Vural, E. Treatment of adult subcondylar mandibular fractures: closed vs open vs endoscopic approach. Arch Otolaryngol Head Neck Surg 2004, 130, 1228–1230. [Google Scholar] [CrossRef] [PubMed]
- Mueller, R.V.; Czerwinski, M.; Lee, C.; Kellman, R.M. Condylar fracture repair: use of the endoscope to advance traditional treatment philosophy. Facial Plast Surg Clin North Am 2006, 14, 1–9. [Google Scholar] [CrossRef]
- Aziz, S.R.; Ziccardi, V.B. Endoscopically assisted management of mandibular condylar fractures. Atlas Oral Maxillofac Surg Clin North Am 2009, 17, 71–74. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Mueller, R.V.; Lee, K.; Mathes, S.J. Endoscopic subcondylar fracture repair: functional, aesthetic, and radiographic outcomes. Plast Reconstr Surg 1998, 102, 1434–1443, discussion 1444–1445. [Google Scholar] [CrossRef] [PubMed]
- Troulis, M.J.; Kaban, L.B. Endoscopic approach to the ramus/condyle unit: clinical applications. J Oral Maxillofac Surg 2001, 59, 503–509. [Google Scholar] [CrossRef]
- Kellman, R.M. Endoscopically assisted repair of subcondylar fractures of the mandible: an evolving technique. Arch Facial Plast Surg 2003, 5, 244–250. [Google Scholar] [CrossRef]
- Martin, M.; Lee, C. Endoscopic mandibular condyle fracture repair. Atlas Oral Maxillofac Surg Clin North Am 2003, 11, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Biglioli, F.; Colletti, G. Transmasseter approach to condylar fractures by mini-retromandibular access. J Oral Maxillofac Surg 2009, 67, 2418–2424. [Google Scholar] [CrossRef] [PubMed]
- Biglioli, F.; Colletti, G. Mini-retromandibular approach to condylar fractures. J Craniomaxillofac Surg 2008, 36, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Colletti, G.; Battista, V.M.; Allevi, F.; Giovanditto, F.; Rabbiosi, D.; Biglioli, F. Extraoral approach to mandibular condylar fractures: our experience with 100 cases. J Craniomaxillofac Surg 2014, 42, e186–e194. [Google Scholar] [CrossRef]
- Nicolai, G.; Lorè, B.; De Marinis, L.; Calabrese, L. Combined surgical approach retromandibular and intraoral to subcondylar mandibular fractures. J Craniofac Surg 2011, 22, 1354–1357. [Google Scholar] [CrossRef]
- Schiel, S.; Mayer, P.; Probst, F.; Otto, S.; Cornelius, C.P. Transoral open reduction and fixation of mandibular condylar base and neck fractures in children and young teenagers—a beneficial treatment option? J Oral Maxillofac Surg 2013, 71, 1220–1230. [Google Scholar] [CrossRef]


© 2015 by the author. The Author(s) 2015.
Share and Cite
Aboelatta, Y.A.; Elbarbary, A.S.; Abdelazeem, S.; Massoud, K.S.; Safe, I.I. Minimizing the Submandibular Incision in Endoscopic Subcondylar Fracture Repair. Craniomaxillofac. Trauma Reconstr. 2015, 8, 315-320. https://doi.org/10.1055/s-0035-1549010
Aboelatta YA, Elbarbary AS, Abdelazeem S, Massoud KS, Safe II. Minimizing the Submandibular Incision in Endoscopic Subcondylar Fracture Repair. Craniomaxillofacial Trauma & Reconstruction. 2015; 8(4):315-320. https://doi.org/10.1055/s-0035-1549010
Chicago/Turabian StyleAboelatta, Yasser Abdallah, Amir S. Elbarbary, Sarah Abdelazeem, Karim S. Massoud, and Ikram I. Safe. 2015. "Minimizing the Submandibular Incision in Endoscopic Subcondylar Fracture Repair" Craniomaxillofacial Trauma & Reconstruction 8, no. 4: 315-320. https://doi.org/10.1055/s-0035-1549010
APA StyleAboelatta, Y. A., Elbarbary, A. S., Abdelazeem, S., Massoud, K. S., & Safe, I. I. (2015). Minimizing the Submandibular Incision in Endoscopic Subcondylar Fracture Repair. Craniomaxillofacial Trauma & Reconstruction, 8(4), 315-320. https://doi.org/10.1055/s-0035-1549010



