Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice
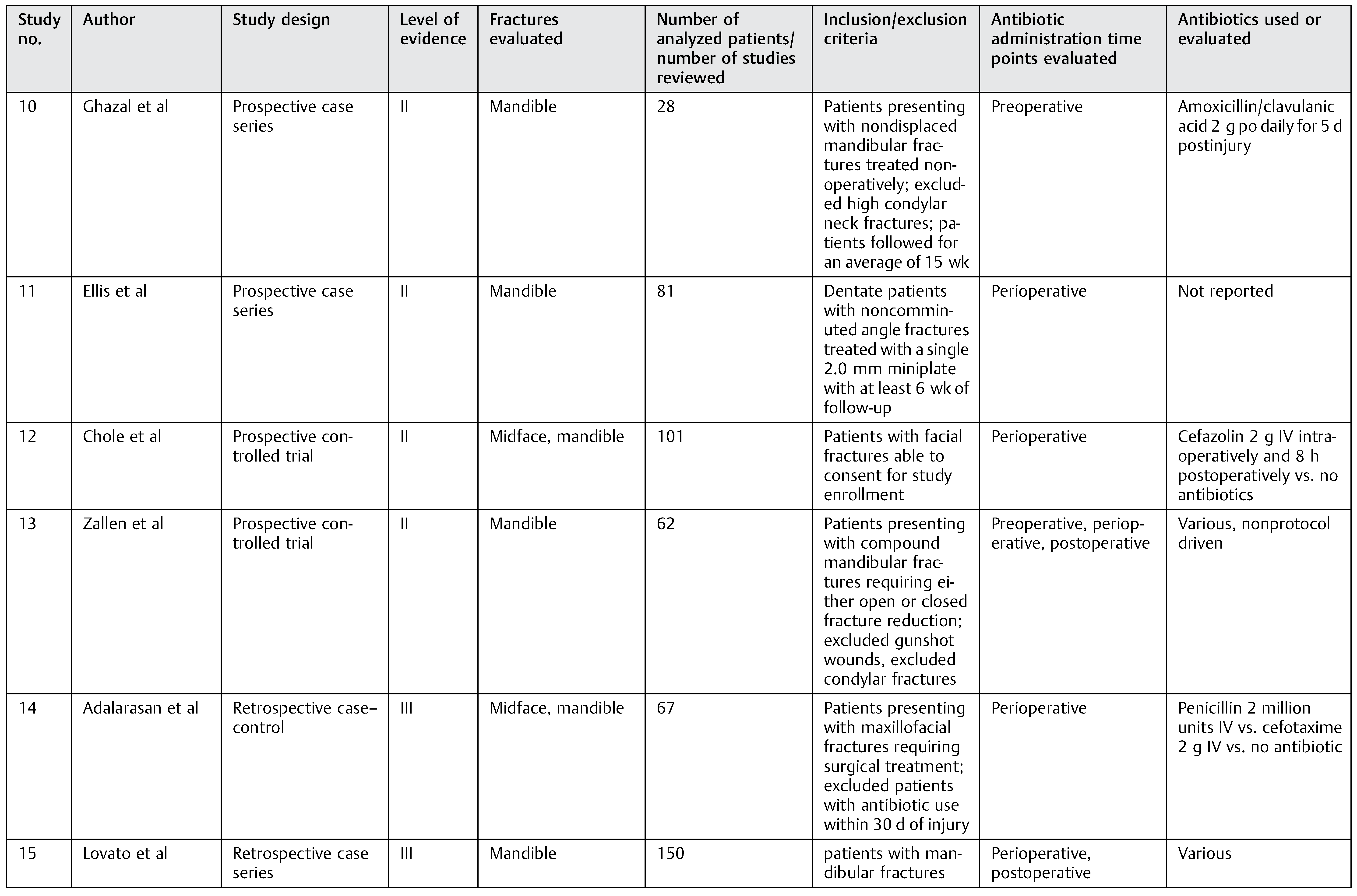
Abstract
:Methods
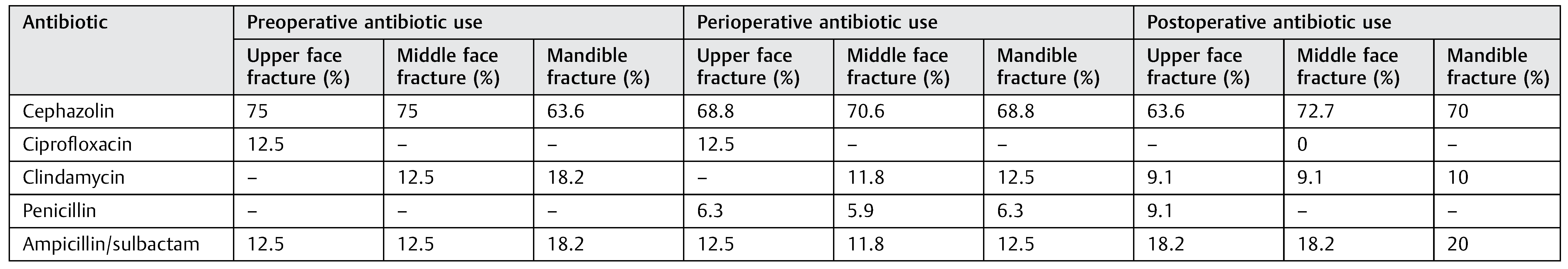
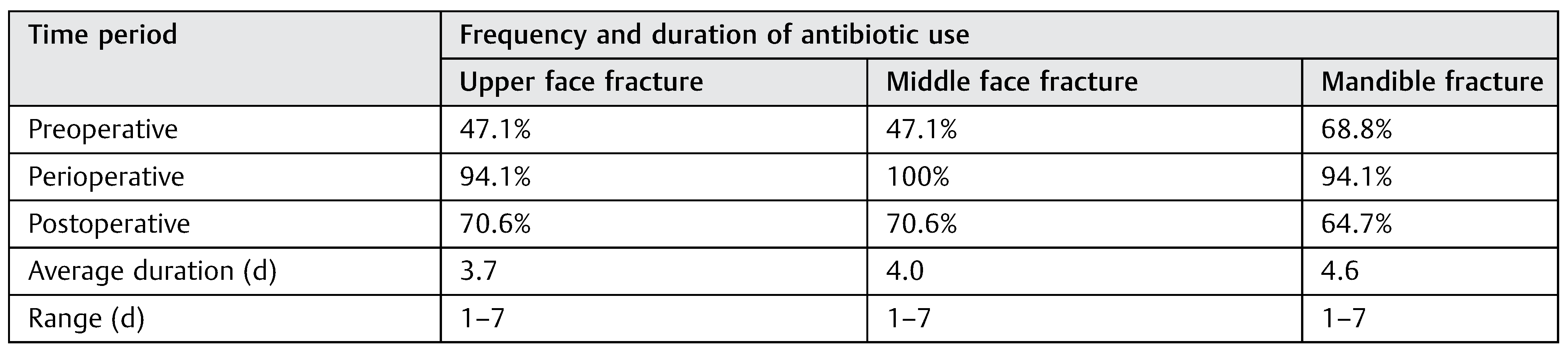
Results
Discussion
Conclusion
This study was presented, in part, as a poster at the 92nd Annual Meeting of The American Association of Plastic Surgeons, April 21, 2013, New Orleans, LA. Abstract #P34. No author has any financial disclosures relevant to this article, or conflict of interest to declare. |
References
- Lauder, A.; Jalisi, S.; Spiegel, J.; Stram, J.; Devaiah, A. Antibiotic prophylaxis in the management of complex midface and frontal sinus trauma. Laryngoscope 2010, 120, 1940–1945. [Google Scholar] [PubMed]
- Bagheri, S.C.; Dimassi, M.; Shahriari, A.; Khan, H.A.; Jo, C.; Steed, M.B. Facial trauma coverage among level-1 trauma centers of the United States. J Oral Maxillofac Surg 2008, 66, 963–967. [Google Scholar] [PubMed]
- Allareddy, V.; Allareddy, V.; Nalliah, R.P. Epidemiology of facial fracture injuries. J Oral Maxillofac Surg 2011, 69, 2613–2618. [Google Scholar]
- Imahara, S.D.; Hopper, R.A.; Wang, J.; Rivara, F.P.; Klein, M.B. Patterns and outcomes of pediatric facial fractures in the United States: a survey of the National Trauma Data Bank. J Am Coll Surg 2008, 207, 710–716. [Google Scholar] [PubMed]
- Dillon, J.K.; Christensen, B.; McDonald, T.; Huang, S.; Gauger, P.; Gomez, P. The financial burden of mandibular trauma. J Oral Maxillofac Surg 2012, 70, 2124–2134. [Google Scholar] [CrossRef]
- Singer, A.J.; Hollander, J.E.; Quinn, J.V. Evaluation and management of traumatic lacerations. N Engl J Med 1997, 337, 1142–1148. [Google Scholar]
- Bratzler, D.W.; Hunt, D.R. The surgical infection prevention and surgical care improvement projects: national initiatives to improve outcomes for patients having surgery. Clin Infect Dis 2006, 43, 322–330. [Google Scholar] [CrossRef]
- Classen, D.C.; Evans, R.S.; Pestotnik, S.L.; Horn, S.D.; Menlove, R.L.; Burke, J.P. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med 1992, 326, 281–286. [Google Scholar]
- Namias, N.; Meizoso, J.P.; Livingston, D.H. ; SOSICK Investigators Group. Survey of surgical infections currently known (SOSICK): a multicenter examination of antimicrobial use from the surgical infection society scientific studies committee. Surg Infect (Larchmt) 2008, 9, 509–514. [Google Scholar]
- Debbia, E.A.; Schito, G.C.; Gualco, L.; Tonoli, E.; Dolcino, M.; Marchese, A. Microbial epidemiology patterns of surgical infection pathogens. J Chemother 2001, 13, 84–88. [Google Scholar]
- Stulberg, J.J.; Delaney, C.P.; Neuhauser, D.V.; Aron, D.C.; Fu, P.; Koroukian, S.M. Adherence to surgical care improvement project measures and the association with postoperative infections. JAMA 2010, 303, 2479–2485. [Google Scholar] [PubMed]
- Hawn, M.T.; Richman, J.S.; Vick, C.C.; et al. Timing of surgical antibiotic prophylaxis and the risk of surgical site infection. JAMA Surg 2013, 148, 649–657. [Google Scholar]
- Antimicrobial prophylaxis for surgery. Treat Guidel Med Lett 2012, 10, 73–78, quiz 79–80.
- American Society of Plastic Surgeons Evidence Rating Scales. Available online: http://www.plasticsurgery.org/for-medical-profes- sionals/legislation-and-advocacy/health-policy-resources/evidence- based-guidelinespractice-parameters/description-and-development- of-evidence-based-practice-guidelines.html (accessed on 19 May 2013).
- Hentz, V.R. Making the case for case reports: open and shut, or case dismissed? J Hand Surg Am 2013, 38, 433–434. [Google Scholar]
- American Society of Plastic Surgeons Scale for Grading Recommendations. Available online: http://www.plasticsurgery.org/for-medical- professionals/legislation-and-advocacy/health-policy-resources/ evidence-based-guidelinespractice-parameters/description-and- development-of-evidence-based-practice-guidelines.html (accessed on 19 May 2013).
- Shuttleworth, G.N.; David, D.B.; Potts, M.J.; Bell, C.N.; Guest, P.G. Lesson of the week: orbital trauma. Do not blow your nose. BMJ 1999, 318, 1054–1055. [Google Scholar]
- Courtney, D.J.; Thomas, S.; Whitfield, P.H. Isolated orbital blowout fractures: survey and review. Br J Oral Maxillofac Surg 2000, 38, 496–504. [Google Scholar]
- Bui, P.; Demian, N.; Beetar, P. Infection rate in mandibular angle fractures treated with a 2.0-mm 8-hole curved strut plate. J Oral Maxillofac Surg 2009, 67, 804–808. [Google Scholar] [PubMed]
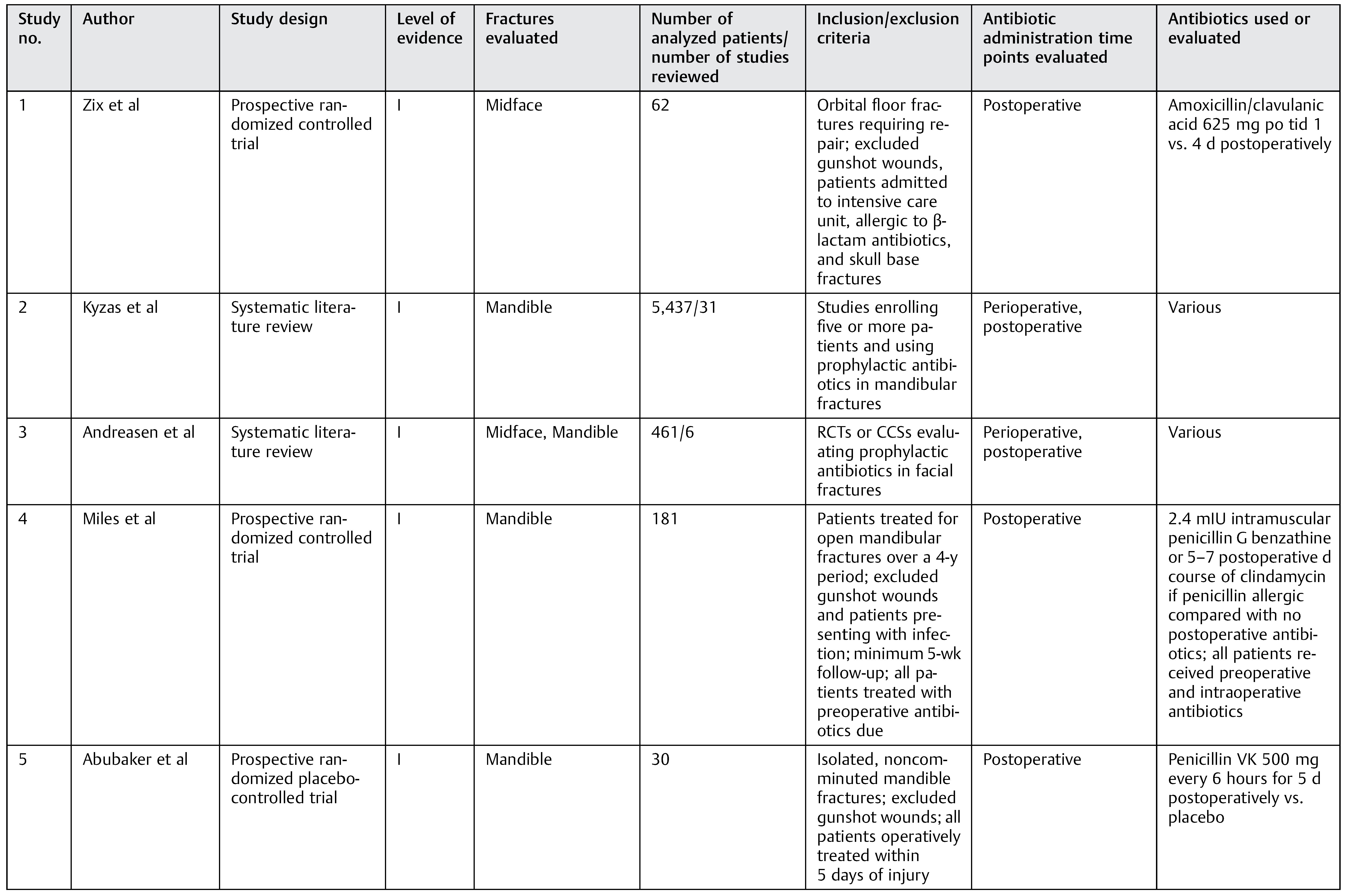
- Zix, J.; Schaller, B.; Iizuka, T.; Lieger, O. The role of postoperative prophylactic antibiotics in the treatment of facial fractures: a randomised, double-blind, placebo-controlled pilot clinical study. Part 1: orbital fractures in 62 patients. Br J Oral Maxillofac Surg 2013, 51, 332–336. [Google Scholar]
- Kyzas, P.A. Use of antibiotics in the treatment of mandible fractures: a systematic review. J Oral Maxillofac Surg 2011, 69, 1129–1145. [Google Scholar]
- Andreasen, J.O.; Jensen, S.S.; Schwartz, O.; Hillerup, Y. A systematic review of prophylactic antibiotics in the surgical treatment of maxillofacial fractures. J Oral Maxillofac Surg 2006, 64, 1664–1668. [Google Scholar]
- Miles, B.A.; Potter, J.K.; Ellis, E., III. The efficacy of postoperative antibiotic regimens in the open treatment of mandibular fractures: a prospective randomized trial. J Oral Maxillofac Surg 2006, 64, 576–582. [Google Scholar]
- Abubaker, A.O.; Rollert, M.K. Postoperative antibiotic prophylaxis in mandibular fractures: A preliminary randomized, double-blind, and placebo-controlled clinical study. J Oral Maxillofac Surg 2001, 59, 1415–1419. [Google Scholar]
- Heit, J.M.; Stevens, M.R.; Jeffords, K. Comparison of ceftriaxone with penicillin for antibiotic prophylaxis for compound mandible fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1997, 83, 423–426. [Google Scholar] [PubMed]
- Gerlach, K.; Pape, H. Perioperative antibiotic prophylaxis in mandibular fracture treatment. Chemioterapia 1987, 6 (Suppl 2), 568. [Google Scholar] [PubMed]
- Bellamy, J.L.; Molendijk, J.; Reddy, S.K.; et al. Severe infectious complications following frontal sinus fracture: the impact of operative delay and perioperative antibiotic use. Plast Reconstr Surg 2013, 132, 154–162. [Google Scholar]
- Knepil, G.J.; Loukota, R.A. Outcomes of prophylactic antibiotics following surgery for zygomatic bone fractures. J Craniomaxillofac Surg 2010, 38, 131–133. [Google Scholar] [CrossRef] [PubMed]
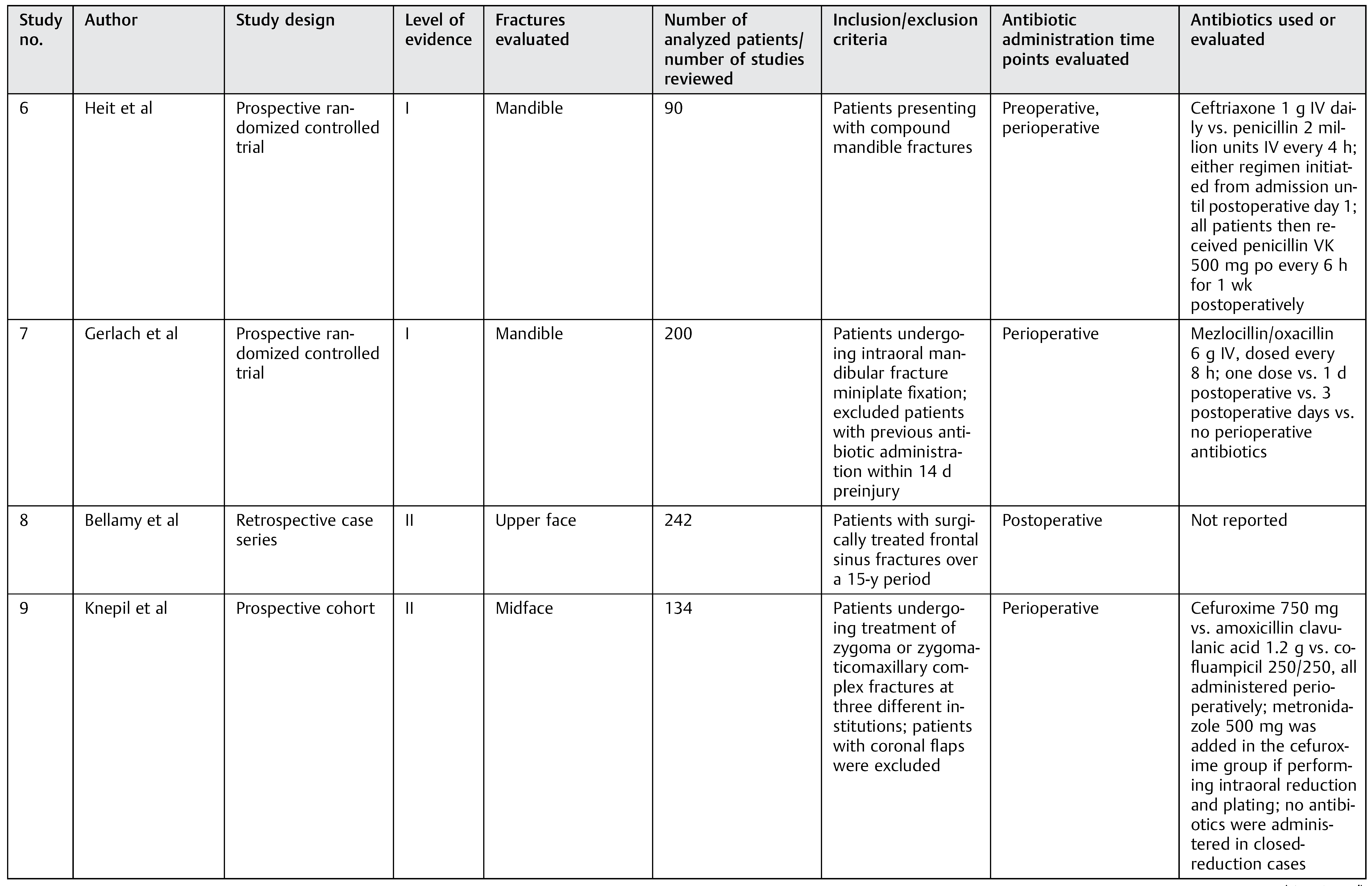
- Ghazal, G.; Jaquiéry, C.; Hammer, B. Non-surgical treatment of mandibular fractures—survey of 28 patients. Int J Oral Maxillofac Surg 2004, 33, 141–145. [Google Scholar]
- Ellis, E., III; Walker, L.R. Treatment of mandibular angle fractures using one noncompression miniplate. J Oral Maxillofac Surg 1996, 54, 864–871, discussion 871–872. [Google Scholar]
- Chole, R.A.; Yee, J. Antibiotic prophylaxis for facial fractures. A prospective, randomized clinical trial. Arch Otolaryngol Head Neck Surg 1987, 113, 1055–1057. [Google Scholar]
- Zallen, R.D.; Curry, J.T. A study of antibiotic usage in compound mandibular fractures. J Oral Surg 1975, 33, 431–434. [Google Scholar]
- Adalarasan, S.; Mohan, A.; Pasupathy, S. Prophylactic antibiotics in maxillofacial fractures: a requisite? J Craniofac, S.urg 2010, 21, 1009–1011. [Google Scholar]
- Lovato, C.; Wagner, J.D. Infection rates following perioperative prophylactic antibiotics versus postoperative extended regimen prophylactic antibiotics in surgical management of mandibular fractures. J Oral Maxillofac Surg 2009, 67, 827–832. [Google Scholar] [PubMed]
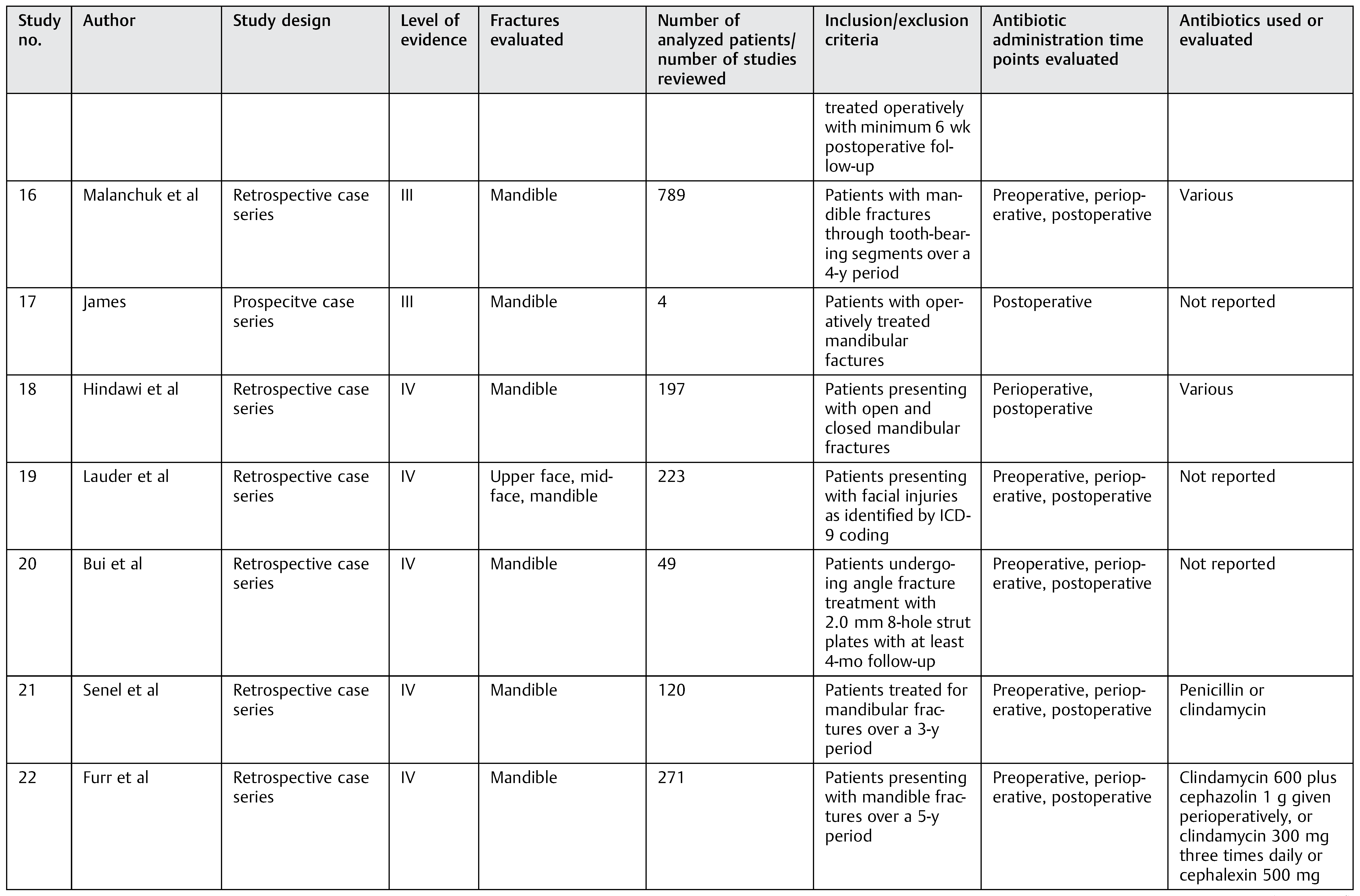
- Malanchuk, V.O.; Kopchak, A.V. Risk factors for development of infection in patients with mandibular fractures located in the tooth-bearing area. J Craniomaxillofac Surg 2007, 35, 57–62. [Google Scholar]
- James, R.B.; Fredrickson, C.; Kent, J.N. Prospective study of mandibular fractures. J Oral Surg 1981, 39, 275–281. [Google Scholar] [PubMed]
- Hindawi, Y.H.; Oakley, G.M.; Kinsella, C.R., Jr; Lindsay, K.; Scifres, A.M. Antibiotic duration and postoperative infection rates in mandibular fractures. J Craniofac Surg 2011, 22, 1375–1377. [Google Scholar]
- Senel, F.C.; Jessen, G.S.; Melo, M.D.; Obeid, G. Infection following treatment of mandible fractures: the role of immunosuppression and polysubstance abuse. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007, 103, 38–42. [Google Scholar] [PubMed]
- Furr, A.M.; Schweinfurth, J.M.; May, W.L. Factors associated with longterm complications after repair of mandibular fractures. Laryngoscope 2006, 116, 427–430. [Google Scholar]
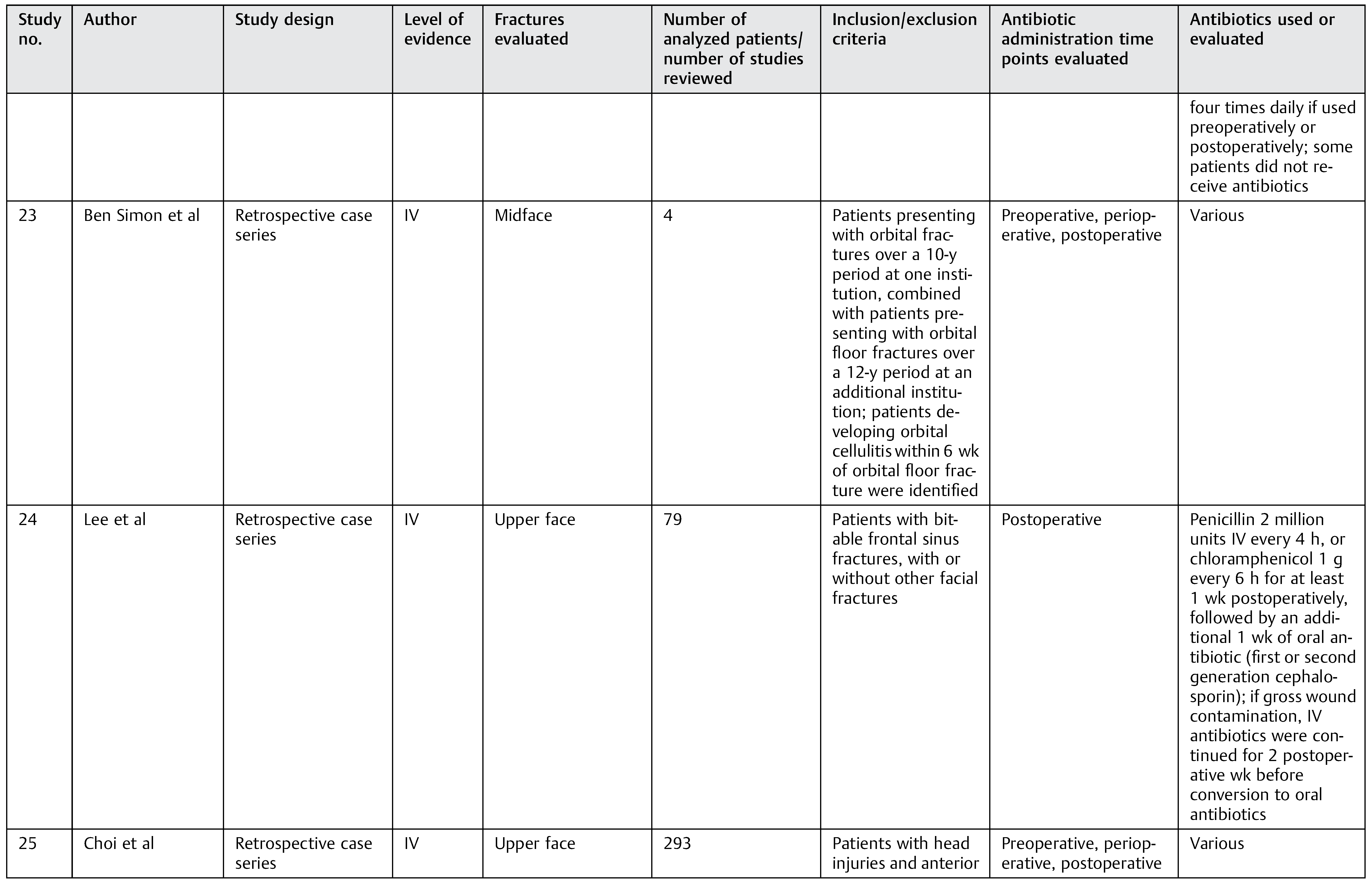
- Ben Simon, G.J.; Bush, S.; Selva, D.; McNab, A.A. Orbital cellulitis: a rare complication after orbital blowout fracture. Ophthalmology 2005, 112, 2030–2034. [Google Scholar]
- Lee, T.T.; Ratzker, P.A.; Galarza, M.; Villanueva, P.A. Early combined management of frontal sinus and orbital and facial fractures. J Trauma 1998, 44, 665–669. [Google Scholar]
- Choi, D.; Spann, R. Traumatic cerebrospinal fluid leakage: risk factors and the use of prophylactic antibiotics. Br J Neurosurg 1996, 10, 571–575. [Google Scholar]
- Silver, H.S.; Fucci, M.J.; Flanagan, J.C.; Lowry, L.D. Severe orbital infection as a complication of orbital fracture. Arch Otolaryngol Head Neck Surg 1992, 118, 845–848, discussion 882. [Google Scholar]
- Hall, S.C.; Ofodile, F.A. Mandibular fractures in an American inner city: the Harlem Hospital Center experience. J Natl Med Assoc 1991, 83, 421–423. [Google Scholar] [PubMed]
- Goldfarb, M.S.; Hoffman, D.S.; Rosenberg, S. Orbital cellulitis and orbital fractures. Ann Ophthalmol 1987, 19, 97–99. [Google Scholar]
- Adkins, W.Y.; Cassone, R.D.; Putney, F.J. Solitary frontal sinus fracture. Laryngoscope 1979, 89 Pt 1, 1099–1104. [Google Scholar]
- Larsen, O.D.; Nielsen, A. Mandibular fractures. II. A follow-up study of 229 patients. Scand J Plast Reconstr Surg 1976, 10, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Kerr, N.W. Some observations on infection in maxillo-facial fractures. Br J Oral Surg 1966, 4, 132–136. [Google Scholar] [PubMed]
- Abubaker, A.O. Use of prophylactic antibiotics in preventing infection of traumatic injuries. Dent Clin North Am 2009, 53, 707–715. [Google Scholar]
- Ellis, E., III; Miles, B.A. Fractures of the mandible: a technical perspective. Plast Reconstr Surg 2007, 120 (Suppl 2), 76S–89S. [Google Scholar]
- Srinivasan, D.; Whear, N.; Shetty, S. Antibiotics for patients with zygomatic fractures into the maxillary antrum. Br J Oral Maxillofac Surg 2006, 44, 424–425. [Google Scholar]
- Stacey, D.H.; Doyle, J.F.; Mount, D.L.; Snyder, M.C.; Gutowski, K.A. Management of mandible fractures. Plast Reconstr Surg 2006, 117, 48e–60e. [Google Scholar]
- Martin, B.; Ghosh, A. Antibiotics in orbital floor fractures. Emerg Med J 2003, 20, 66. [Google Scholar] [CrossRef] [PubMed]
- Newlands, C.; Baggs, P.R.; Kendrick, R. Orbital trauma. Antibiotic prophylaxis needs to be given only in certain circumstances. BMJ 1999, 319, 516–517. [Google Scholar] [CrossRef] [PubMed]
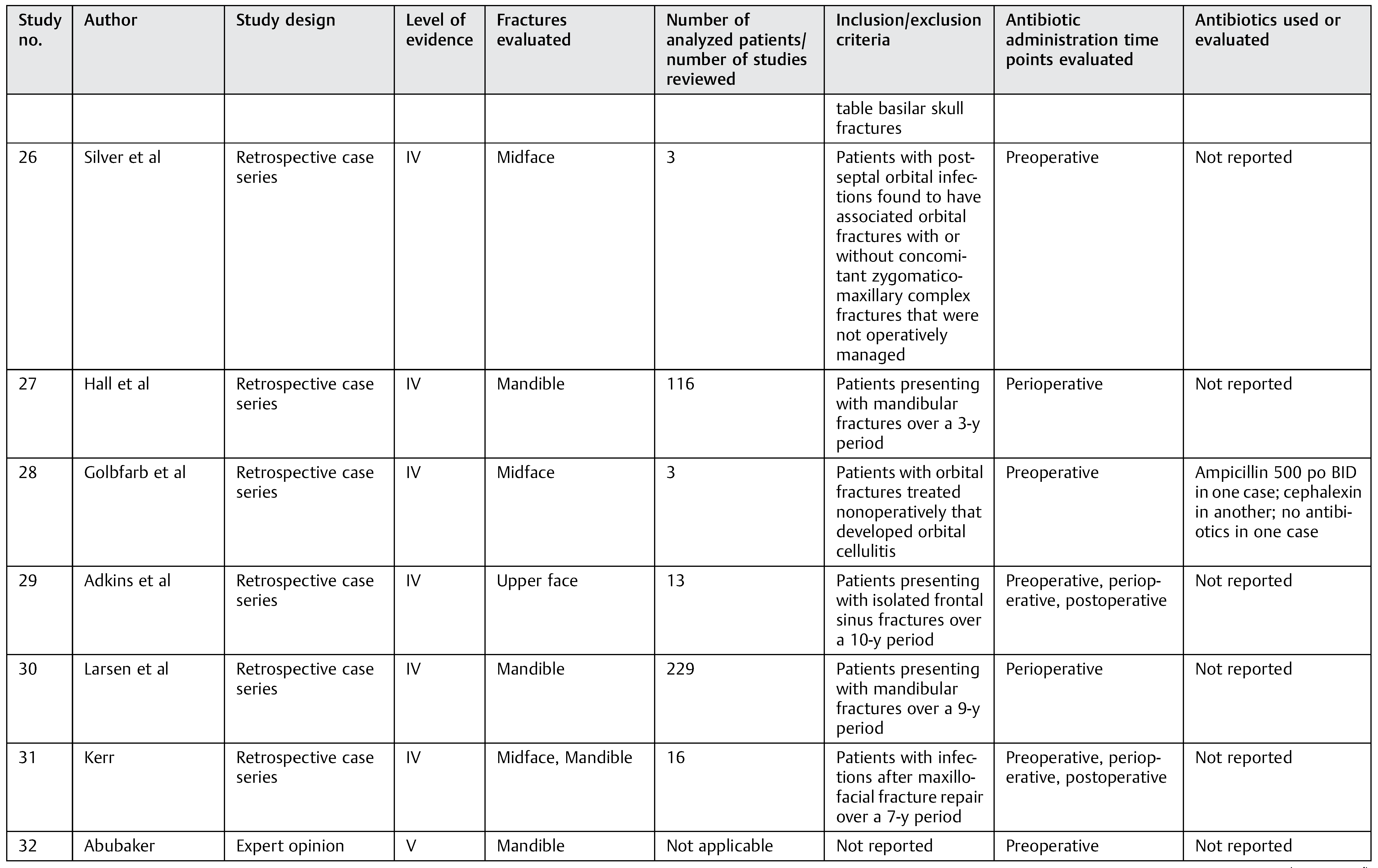
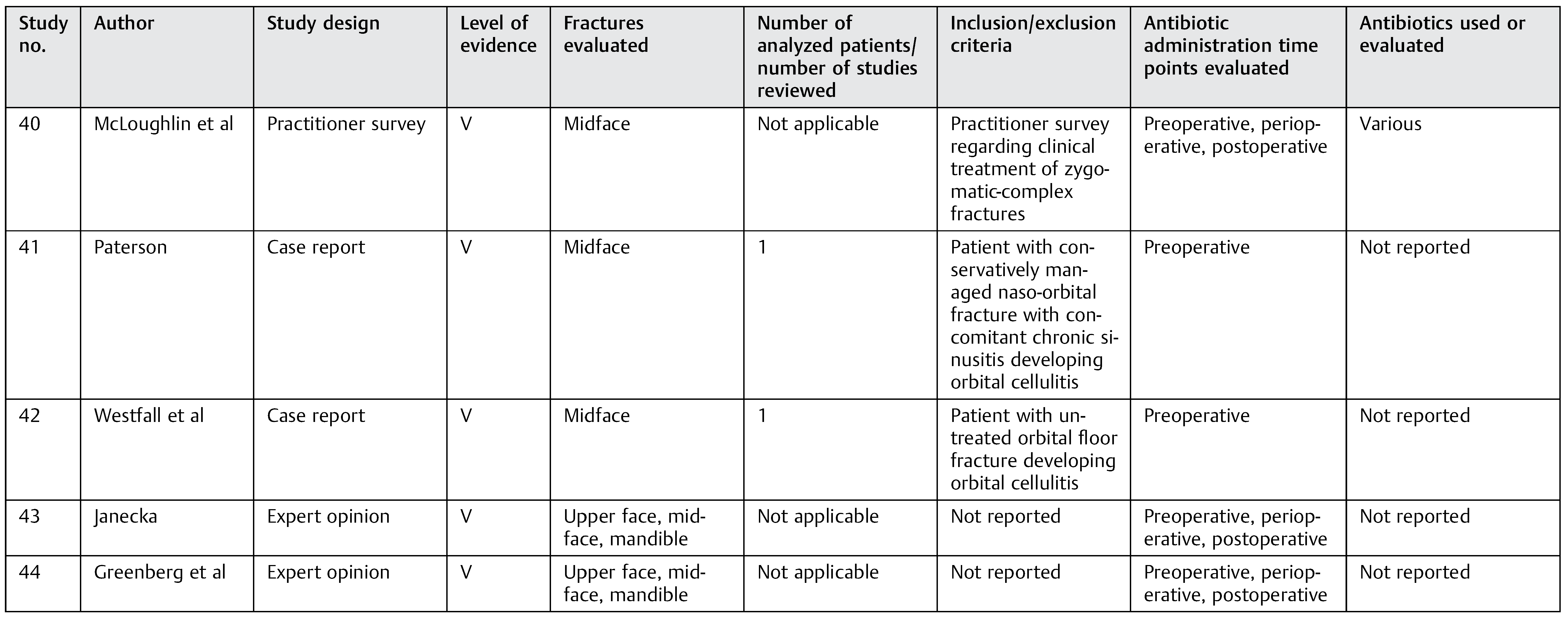
- McLoughlin, P.; Gilhooly, M.; Wood, G. The management of zygomatic complex fractures—results of a survey. Br J Oral Maxillofac Surg 1994, 32, 284–288. [Google Scholar] [CrossRef]
- Paterson, A.W.; Barnard, N.A.; Irvine, G.H. Naso-orbital fracture leading to orbital cellulitis, and visual loss as a complication of chronic sinusitis. Br J Oral Maxillofac Surg 1994, 32, 80–82. [Google Scholar] [CrossRef]
- Westfall, C.T.; Shore, J.W. Isolated fractures of the orbital floor: risk of infection and the role of antibiotic prophylaxis. Ophthalmic Surg 1991, 22, 409–411. [Google Scholar] [CrossRef] [PubMed]
- Janecka, I.P. Maxillofacial infections. Clin Plast Surg 1979, 6, 553–573. [Google Scholar] [CrossRef]
- Greenberg, R.N.; James, R.B.; Marier, R.L.; Wood, W.H.; Sanders, C.V.; Kent, J.N. Microbiologic and antibiotic aspects of infections in the oral and maxillofacial region. J Oral Surg 1979, 37, 873–884. [Google Scholar]
- Bratzler, D.W.; Houck, P.M. Surgical Infection Prevention Guideline Writers Workgroup. Antimicrobial prophylaxis for surgery: an advisory statement from the National Surgical Infection Prevention Project. Am J Surg 2005, 189, 395–404. [Google Scholar] [CrossRef]
- Mithani, S.K.; Kelamis, J.A.; Mundinger, G.S.; et al. The prevalence of cervical spine injury, head injury, or both with isolated and multiple craniomaxillofacial fractures. Plast Reconstr Surg 2012, 129, 163e, author reply 163e–164e. [Google Scholar] [CrossRef]
- Mulligan, R.P.; Mahabir, R.C. The prevalence of cervical spine injury, head injury, or both with isolated and multiple craniomaxillofacial fractures. Plast Reconstr Surg 2010, 126, 1647–1651. [Google Scholar] [CrossRef]
- Bellamy, J.L.; Mundinger, G.S.; Reddy, S.K.; Flores, J.M.; Rodriguez, E.D.; Dorafshar, A.H.; Le Fort, I.I. fractures are associated with death: a comparison of simple and complex midface fractures. J Oral Maxillofac Surg 2013, 71, 1556–1562. [Google Scholar] [PubMed]
- Vaca, E.E.; Mundinger, G.S.; Kelamis, J.A.; et al. Facial fractures with concomitant open globe injury: mechanisms and fracture patterns associated with blindness. Plast Reconstr Surg 2013, 131, 1317–1328. [Google Scholar] [PubMed]

        |
 |
 |
© 2014 by the author. The Author(s) 2014.
Share and Cite
Mundinger, G.S.; Borsuk, D.E.; Okhah, Z.; Christy, M.R.; Bojovic, B.; Dorafshar, A.H.; Rodriguez, E.D. Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice. Craniomaxillofac. Trauma Reconstr. 2015, 8, 64-78. https://doi.org/10.1055/s-0034-1378187
Mundinger GS, Borsuk DE, Okhah Z, Christy MR, Bojovic B, Dorafshar AH, Rodriguez ED. Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice. Craniomaxillofacial Trauma & Reconstruction. 2015; 8(1):64-78. https://doi.org/10.1055/s-0034-1378187
Chicago/Turabian StyleMundinger, Gerhard S., Daniel E. Borsuk, Zachary Okhah, Michael R. Christy, Branko Bojovic, Amir H. Dorafshar, and Eduardo D. Rodriguez. 2015. "Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice" Craniomaxillofacial Trauma & Reconstruction 8, no. 1: 64-78. https://doi.org/10.1055/s-0034-1378187
APA StyleMundinger, G. S., Borsuk, D. E., Okhah, Z., Christy, M. R., Bojovic, B., Dorafshar, A. H., & Rodriguez, E. D. (2015). Antibiotics and Facial Fractures: Evidence-Based Recommendations Compared with Experience-Based Practice. Craniomaxillofacial Trauma & Reconstruction, 8(1), 64-78. https://doi.org/10.1055/s-0034-1378187



