Application of Digital Anthropometry for Craniofacial Assessment
Abstract
:- Craniofacial anthropometry: Measurements performed on the head and face.
- Somatometry: Measurements performed on the rest of the body [2].
Historical Overview
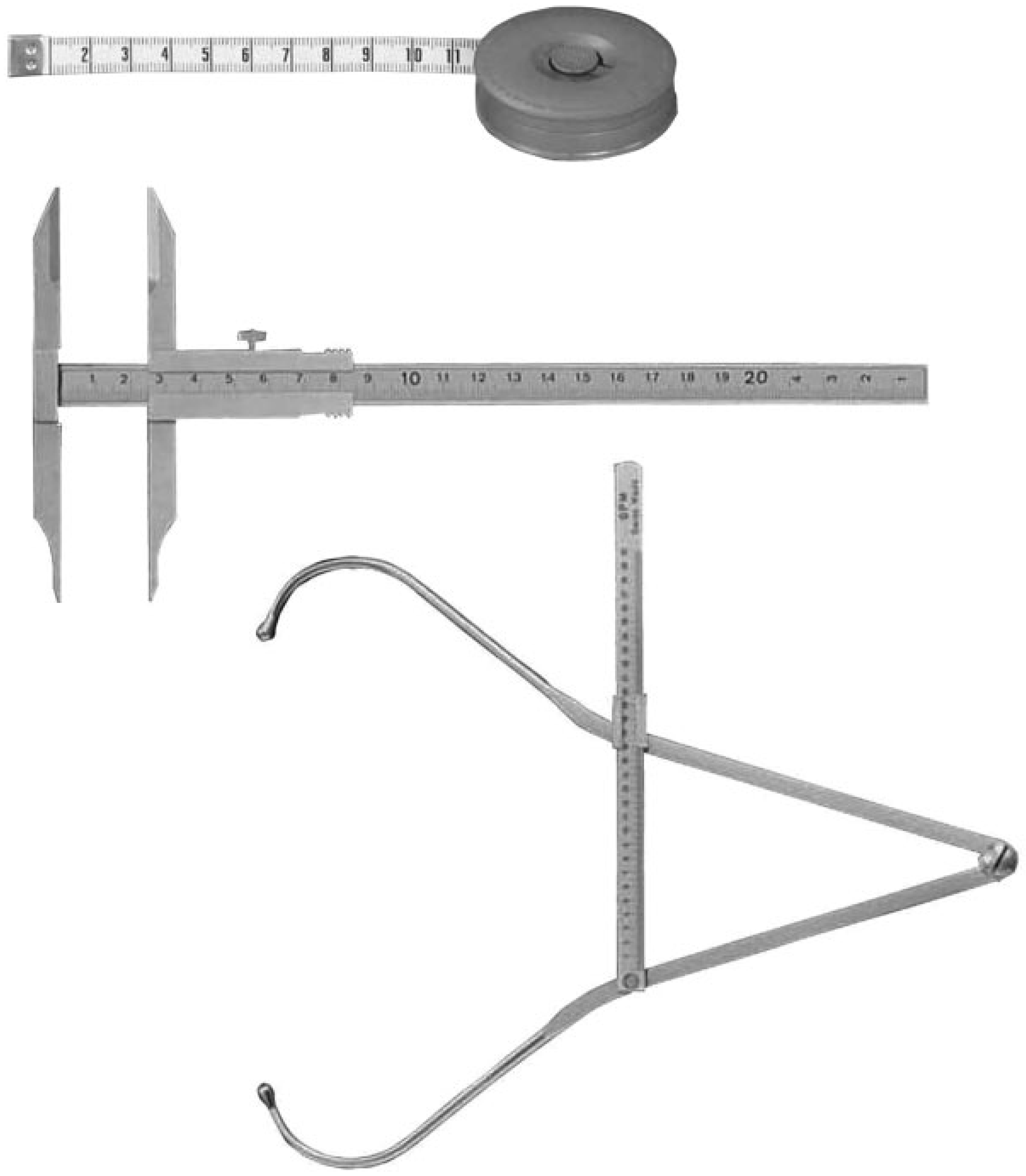
Manual Anthropometry
Anthropometric Landmarks
Digital Anthropometry
Importance of a Normative Anthropometric Database
Diagnosis
- Presence or absence of deformity
- Extent of deformity
- Location/size of the deformed region
- Most defective sites /measurements
- Other minor defects not clearly visible but potentially of significant diagnostic value [5]
Treatment Planning
Postoperative Evaluation
Z-scores (Standardized Scores)
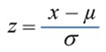
- Normal = Average Z-score 2SD
- AbnormalSubnormal = Average Z-score − 2SDSupernormal = Average Z-score + 2SD
Other Applications of Three-dimensional Anthropometry
Growth Studies
Anaplasthology
Forensics
- Soft tissues undergo changes subsequent to death.
- Destitute cadavers have been used in most of these early studies whose nutritional and health may not represent the population as a whole.
- Gravitational forces may cause false soft tissue measurements in horizontally positioned cadavers [32].
Genetics
Ergonomic Product Design
Conclusion
References
- Kenneth, L.J. Smith’s Recognizable Patterns of Human Malformation, 6th ed.; Elsevier Health Sciences: Philadelphia, PA, USA, 2005. [Google Scholar]
- Salter, E.M.; Kolar, J.C. Anthropometry. In Encyclopedia of Measurement and Statistics; Salkind, N.J., Ed.; Sage Reference: Thousand Oaks, CA, USA, 2007; Volume 1, pp. 35–38. [Google Scholar]
- Leppig, K.A.; Werler, M.M.; Cann, C.I.; Cook, C.A.; Holmes, L.B. Predictive value of minor anomalies. I. Association with major malformations. J Pediatr 1987, 110, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.; Oh, A.K.; Ohta, E.; et al. Validity and reliability of craniofacial anthropometric measurement of 3D digital photogrammetric images. Cleft Palate Craniofac J 2008, 45, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Kolar, J.C.; Salter, E.M. Craniofacial anthropometry: Practical measurement of the head and face for clinical, surgical, and research use; CC Thomas: Springfield, IL, USA, 1997. [Google Scholar]
- Hrdlička, A. Anthropometry; The Wistar Institute of Anatomy and Biology: Philadelphia, PA, USA, 1920. [Google Scholar]
- Anderson, N.K.; Habal, M. In Memoriam of Leslie Farkas, MD. J Craniofac Surg 2009, 20, 713. [Google Scholar] [CrossRef]
- Deutsch, C.K.; Shell, A.R.; Bird, B.D. The Farkas System Of Craniofacial Anthropometry: Methodology And Normative Databases. In The Handbook of Anthropometry, 1st ed.; Preedy, V., Ed.; Springer: New York, NY, USA, 2012. [Google Scholar]
- Naini, F.B.; Leslie, G. Leslie G. Farkas: pioneer of modern craniofacial anthropometry. Arch Facial Plast Surg 2010, 12, 141–142. [Google Scholar] [CrossRef] [PubMed]
- Farkas, L.; Munro, I. Anthropometric Facial Proportions in Medicine; Charles C. Thomas Publisher: Springfield, IL, USA, 1987. [Google Scholar]
- Allanson, J.E. Objective techniques for craniofacial assessment: what are the choices? Am J Med Genet 1997, 70, 1–5. [Google Scholar] [CrossRef]
- Farkas, L.G.; Hajniš, K.; Posnick, J.C. Anthropometric and anthropo-scopic findings of the nasal and facial region in cleft patients before and after primary lip and palate repair. Cleft Palate Craniofac J 1993, 30, 1–12. [Google Scholar] [CrossRef]
- Mulliken, J.B.; Burvin, R.; Farkas, L.G. Repair of bilateral complete cleft lip: intraoperative nasolabial anthropometry. Plast Reconstr Surg 2001, 107, 307–314. [Google Scholar] [CrossRef]
- Kolar, J.C.; Salter, E.M. Preoperative anthropometric dysmorphology in metopic synostosis. Am J Phys Anthropol 1997, 103, 341–351. [Google Scholar] [CrossRef]
- Kolar, J.C.; Salter, E.M.; Weinberg, S.M. Preoperative craniofacial dysmorphology in isolated sagittal synostosis: a comprehensive anthropometric evaluation. J Craniofac Surg 2010, 21, 1404–1410. [Google Scholar] [CrossRef]
- Ridgway, E.B.; Wu, J.K.; Sullivan, S.R.; et al. Craniofacial growth in patients with FGFR3Pro250Arg mutation after fronto-orbital advancement in infancy. J Craniofac Surg 2011, 22, 455–461. [Google Scholar] [CrossRef]
- Farkas, L.G. Anthropometry of the Head and Face, 2nd ed.; Raven Press: New York, NY, USA, 1994. [Google Scholar]
- Farkas, L.G.; Deutsch, C.K. Anthropometric determination of craniofacial morphology. Am J Med Genet 1996, 65, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Jayaratne, Y.S.; Zwahlen, R.A.; Lo, J.; Tam, S.C.; Cheung, L.K. Computeraided maxillofacial surgery: an update. Surg Innov 2010, 17, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Azouz, Z.B.; Rioux, M.; Shu, C.; Lepage, R. Characterizing human shape variation using 3D anthropometric data. Vis Comput 2006, 22, 302–314. [Google Scholar] [CrossRef]
- Landes, C.A.; Bitsakis, J.; Diehl, T.; Bitter, K. Introduction of a three-dimensional anthropometry of the viscerocranium. Part I: measurement of craniofacial development and establishment of standard values and growth functions. J Craniomaxillofac Surg 2002, 30, 18–24. [Google Scholar] [CrossRef]
- Bush, K.; Antonyshyn, O. Three-dimensional facial anthropometry using a laser surface scanner: validation of the technique. Plast Reconstr Surg 1996, 98, 226–235. [Google Scholar] [CrossRef]
- Farkas, L.G.; Katic, M.J.; Forrest, C.R.; et al. International anthropometric study of facial morphology in various ethnic groups/races. J Craniofac Surg 2005, 16, 615–646. [Google Scholar] [CrossRef]
- Deutsch, C.K.; D’Agostino, R.B. Statistical Appendix. In Anthropometry of the head and face, 2nd ed.; Farkas, L.G., Ed.; Raven Press: New York, NY, USA, 1994; pp. 353–359. [Google Scholar]
- Mei, Z.; Grummer-Strawn, L.M. Standard deviation of anthropometric Z-scores as a data quality assessment tool using the 2006 WHO growth standards: a cross country analysis. Bull World Health Organ 2007, 85, 441–448. [Google Scholar] [CrossRef]
- World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995, 854, 1–452. [Google Scholar]
- Ward, R.E.; Jamison, P.L.; Allanson, J.E. Quantitative approach to identifying abnormal variation in the human face exemplified by a study of 278 individuals with five craniofacial syndromes. Am J Med Genet 2000, 91, 8–17. [Google Scholar] [CrossRef]
- Kovacs, L.; Zimmermann, A.; Wawrzyn, H.; et al. Computer aided surgical reconstruction after complex facial burn injuries — opportunities and limitations. Burns 2005, 31, 85–91. [Google Scholar] [CrossRef]
- Jayaratne, Y.S.; Lo, J.; Zwahlen, R.A.; Cheung, L.K. Three-dimensional photogrammetry for surgical planning of tissue expansion in hemifacial microsomia. Head Neck 2010, 32, 1728–1735. [Google Scholar] [CrossRef] [PubMed]
- Sohail, A.S.M.; Bhattacharya, P. Detection of facial feature points using anthropometric face model. In Signal Processing for Image Enhancement and Multimedia Processing; Damiani, E., Yétongnon, K., Schelkens, P., Dipanda, A., Legrand, L., Chbeir, R., Eds.; Springer: New York, NY, USA, 2008; pp. 189–200. [Google Scholar]
- Halberstein, R.A. The application of anthropometric indices in forensic photography: three case studies. J Forensic Sci 2001, 46, 1438–1441. [Google Scholar] [CrossRef]
- Starbuck, J.M.; Ward, R.E. The affect of tissue depth variation on craniofacial reconstructions. Forensic Sci Int 2007, 172, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Wilamowska, K.; Shapiro, L.; Heike, C. Classification of 3D face shape in 22q11.2 deletion syndrome. IEEE International Symposium on Biomedical Imaging 2009, 534–553. [Google Scholar]
- Kim, H.; Han, D.H.; Roh, Y.M.; Kim, K.; Park, Y.G. Facial anthropometric dimensions of Koreans and their associations with fit of quartermask respirators. Ind Health 2003, 41, 8–18. [Google Scholar] [CrossRef]
- Tang, C.Y.; Tang, N.; Stewart, M.C. Ophthalmic anthropometry for Hong Kong Chinese adults. Optom Vis Sci 1998, 75, 293–301. [Google Scholar] [CrossRef]
- Liu, H.; Li, Z.; Zheng, L. Rapid preliminary helmet shell design based on three-dimensional anthropometric head data. J Eng Design 2008, 19, 45–54. [Google Scholar] [CrossRef]

| Region | Name | Abbreviation | Definition [5,17] |
|---|---|---|---|
| Head | Vertex | v | The highest point on the head when the head is oriented in the Frankfort horizontal plane |
| Trichion | tr | A point at on the hairline in the midline of the forehead | |
| Glabella | g | The most prominent midline between eyebrows | |
| Nose | Nasion | n | The midpoint on the soft tissue contour of the base of the nasal root at the level of the frontonasal suture |
| Sellion | se | The most posterior point of the frontonasal soft tissue contour in the midline of the base of the nasal root | |
| Pronasale | prn | The most anterior midpoint of the nasal tip | |
| Subnasale | sn | The midpoint on the nasolabial soft tissue contour between the columella crest and the upper lip | |
| Alare | al | The most lateral point on each alar contour | |
| Alar curvature (or alar crest) point | ac | The most lateral point in the curved baseline of each ala | |
| Columella apex | c′ | The most anterior, or the highest point on the columella crest at the apex of the nostril | |
| Eye | Exocanthion | ex | The soft tissue point located at the outer commissure of each eye fissure |
| Endocanthion | en | The soft tissue point located at the inner commissure of each eye fissure | |
| Palpebrale superius | ps | The highest point in the mid portion of the free margin of each upper eyelid | |
| Palpebrale inferius | pi | The lowest point in the mid portion of the free margin of each lower eyelid | |
| Lips and mouth | Labiale superius | ls | The midpoint of the vermilion line of the upper lip |
| Crista philtri | cph | The point at each elevated margin of the philtrum just above the vermilion line | |
| Cheilion | ch | The point located at each labial commissure | |
| Stomion | sto | The midpoint of the labial fissure when the lips are closed naturally | |
| Labiale inferius | li | The midpoint of the lower vermilion line | |
| Chin | Sublabiale | sl | The midpoint of the Labiomental sulcus |
| Pogonion | pg | The most anterior midpoint of the chin | |
| Gnathion | gn | The lowest median landmark on the lower border of the mandible | |
| Ears | Tragion | t | The notch at the upper margin of the tragus |
| Otobasion inferius | obi | The point of attachment of the ear lobe to the cheek | |
| Otobasion superius | obs | The point of attachment of the helix in the temporal region | |
| Postaurale | pa | The most posterior point on the free margin of the ear | |
| Preaurale | pra | The most anterior point of each ear, located just in front of the helix attachment to the head | |
| Superaurale | sa | The highest point of the free margin of the auricle | |
| Subaurale | sba | The lowest point of the free margin of the ear lobe |
© 2014 by the author. The Author(s) 2014.
Share and Cite
Jayaratne, Y.S.N.; Zwahlen, R.A. Application of Digital Anthropometry for Craniofacial Assessment. Craniomaxillofac. Trauma Reconstr. 2014, 7, 101-107. https://doi.org/10.1055/s-0034-1371540
Jayaratne YSN, Zwahlen RA. Application of Digital Anthropometry for Craniofacial Assessment. Craniomaxillofacial Trauma & Reconstruction. 2014; 7(2):101-107. https://doi.org/10.1055/s-0034-1371540
Chicago/Turabian StyleJayaratne, Yasas S. N., and Roger A. Zwahlen. 2014. "Application of Digital Anthropometry for Craniofacial Assessment" Craniomaxillofacial Trauma & Reconstruction 7, no. 2: 101-107. https://doi.org/10.1055/s-0034-1371540
APA StyleJayaratne, Y. S. N., & Zwahlen, R. A. (2014). Application of Digital Anthropometry for Craniofacial Assessment. Craniomaxillofacial Trauma & Reconstruction, 7(2), 101-107. https://doi.org/10.1055/s-0034-1371540



