The Comprehensive AOCMF Classification System: Mandible Fractures—Level 2 Tutorial
Abstract
:Anatomical and Diagnostic Imaging Considerations
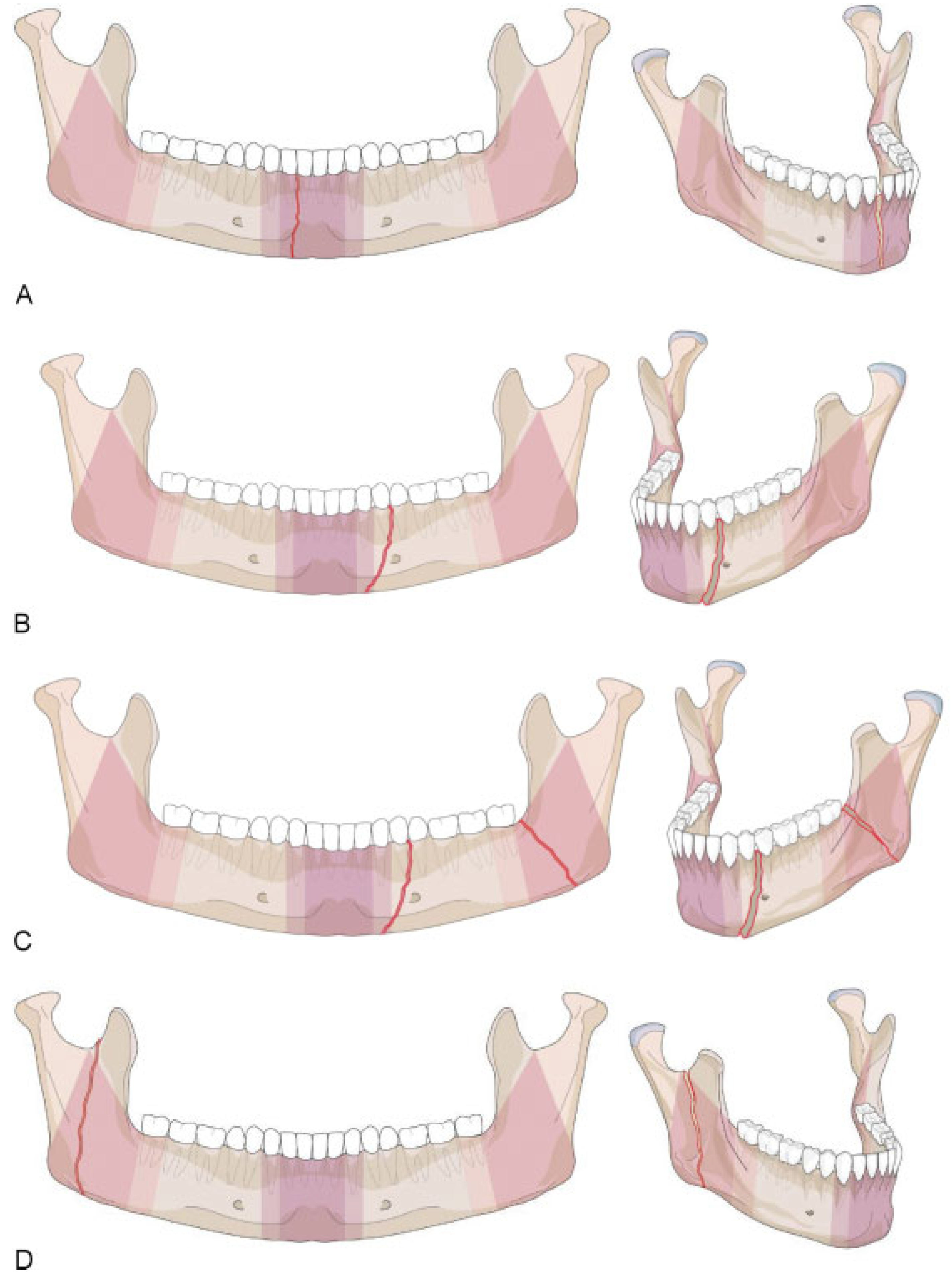
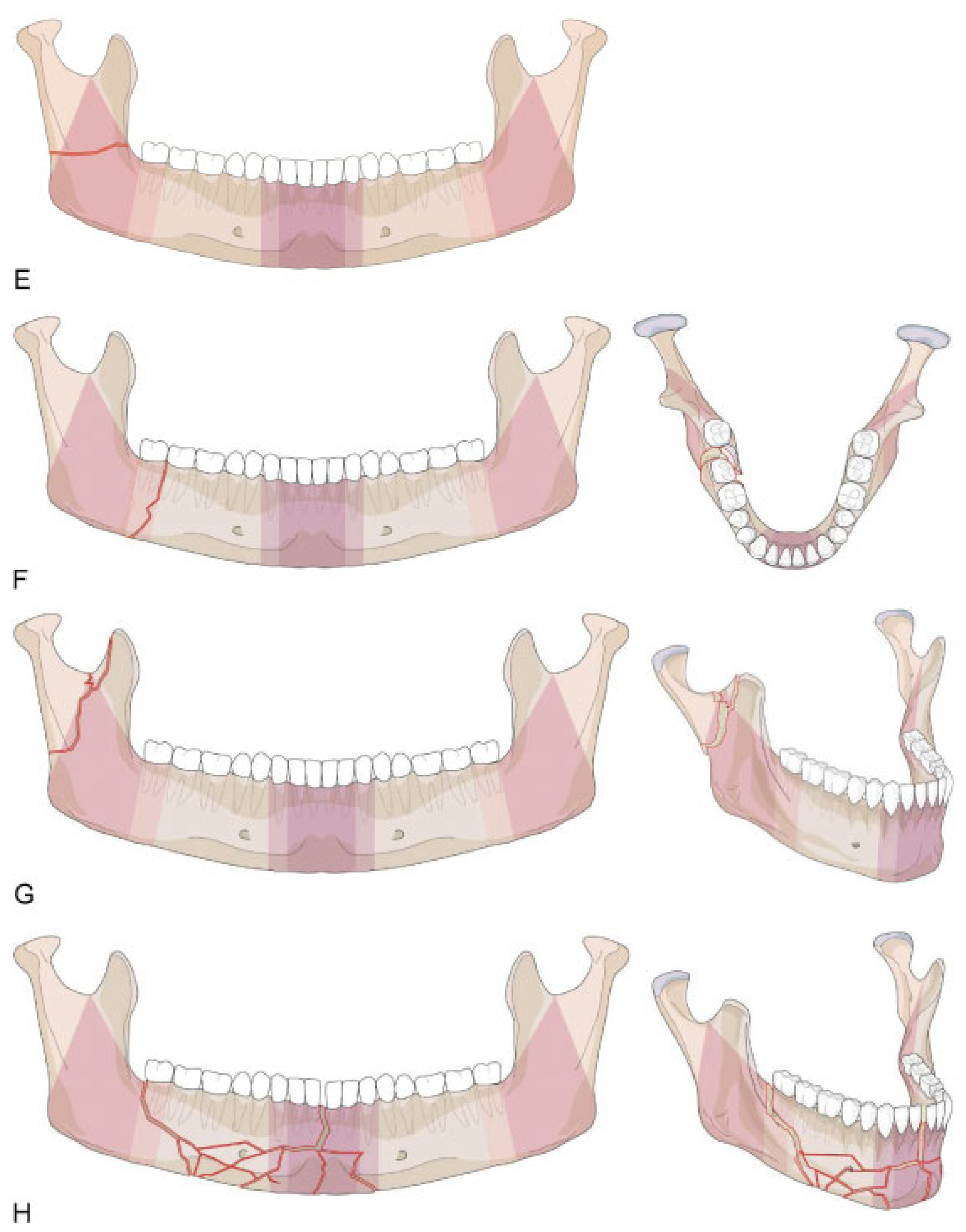
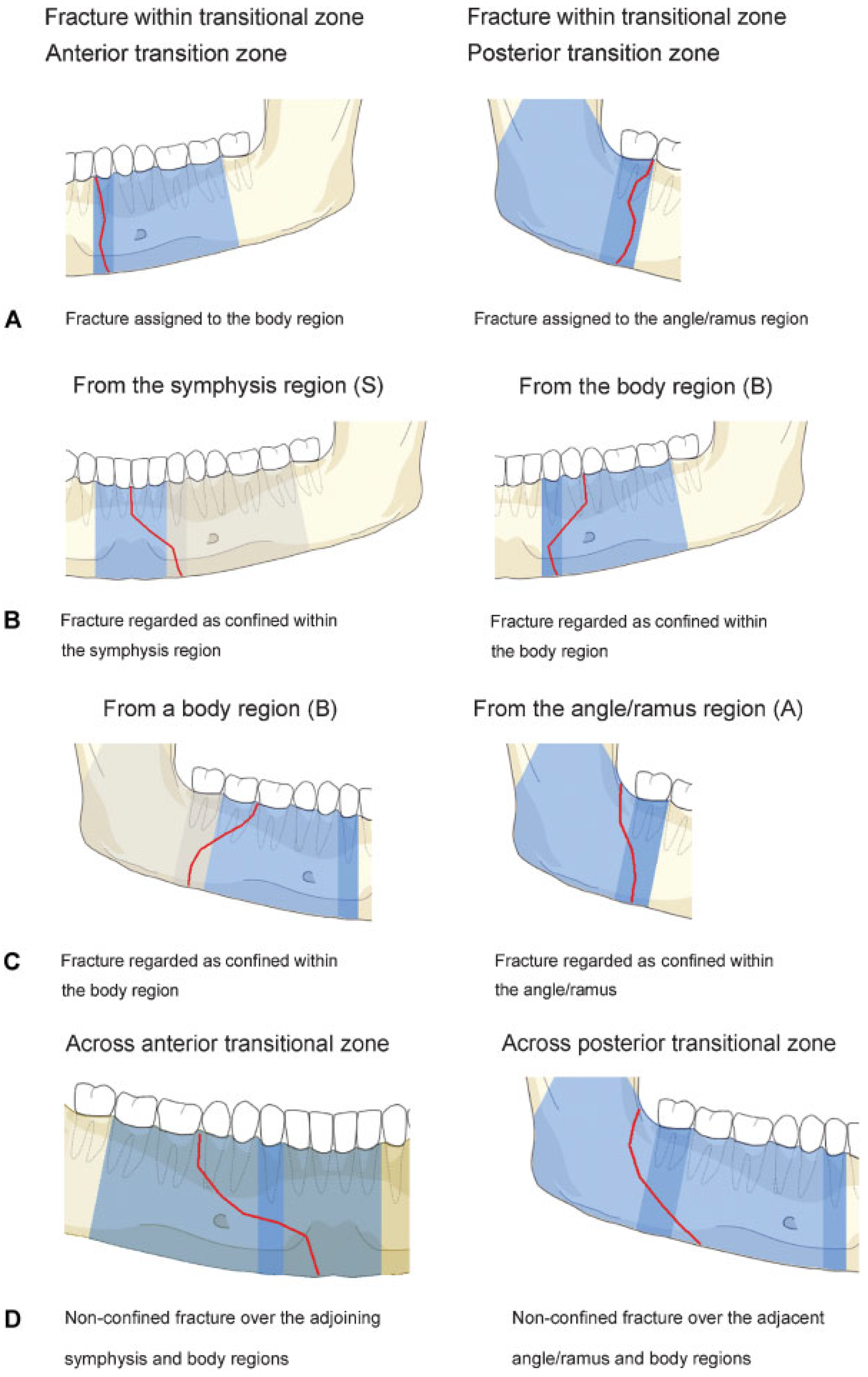
Level 2 Mandibular Fracture Classification System
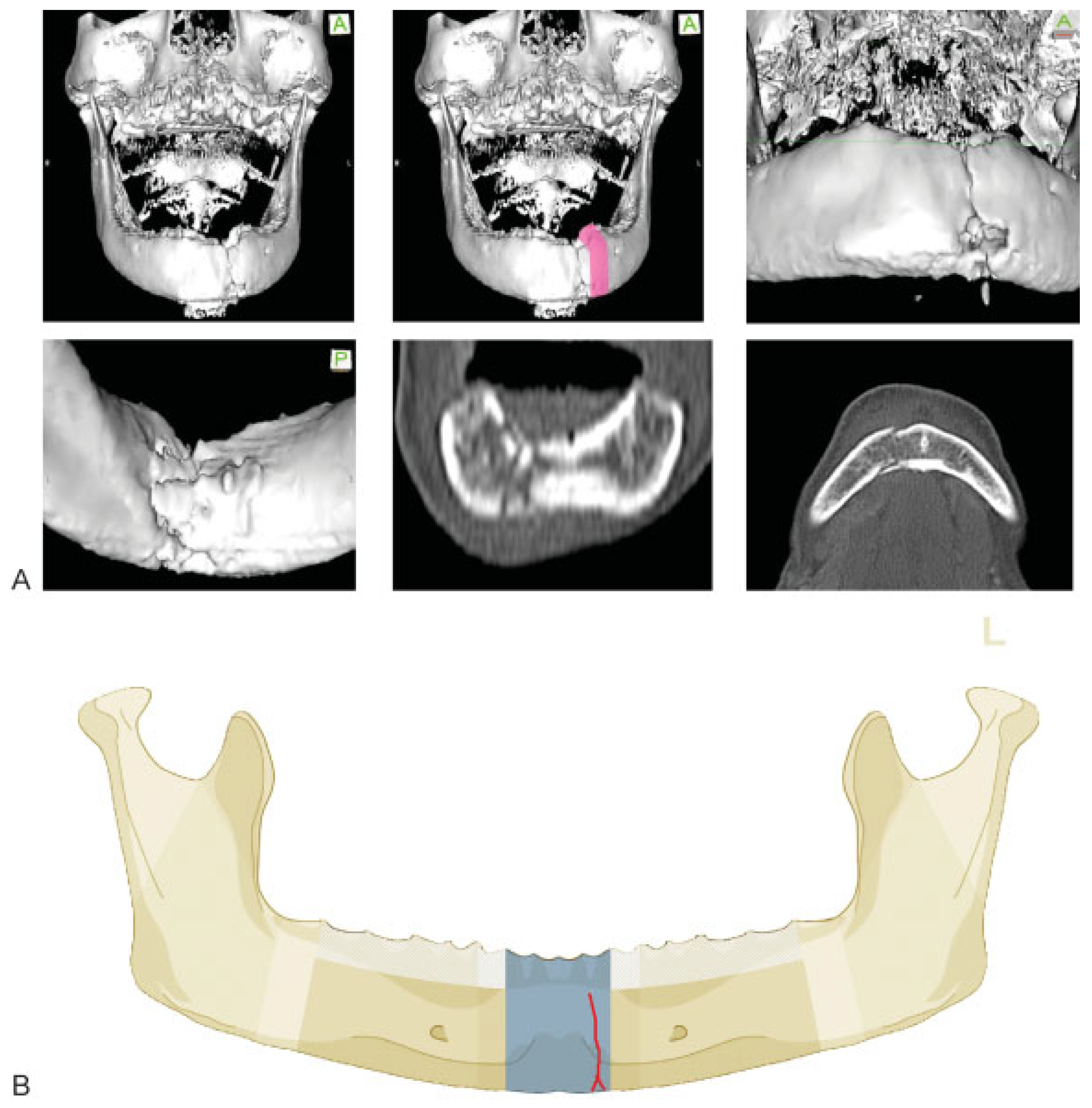
Symphysis/Parasymphysis Region
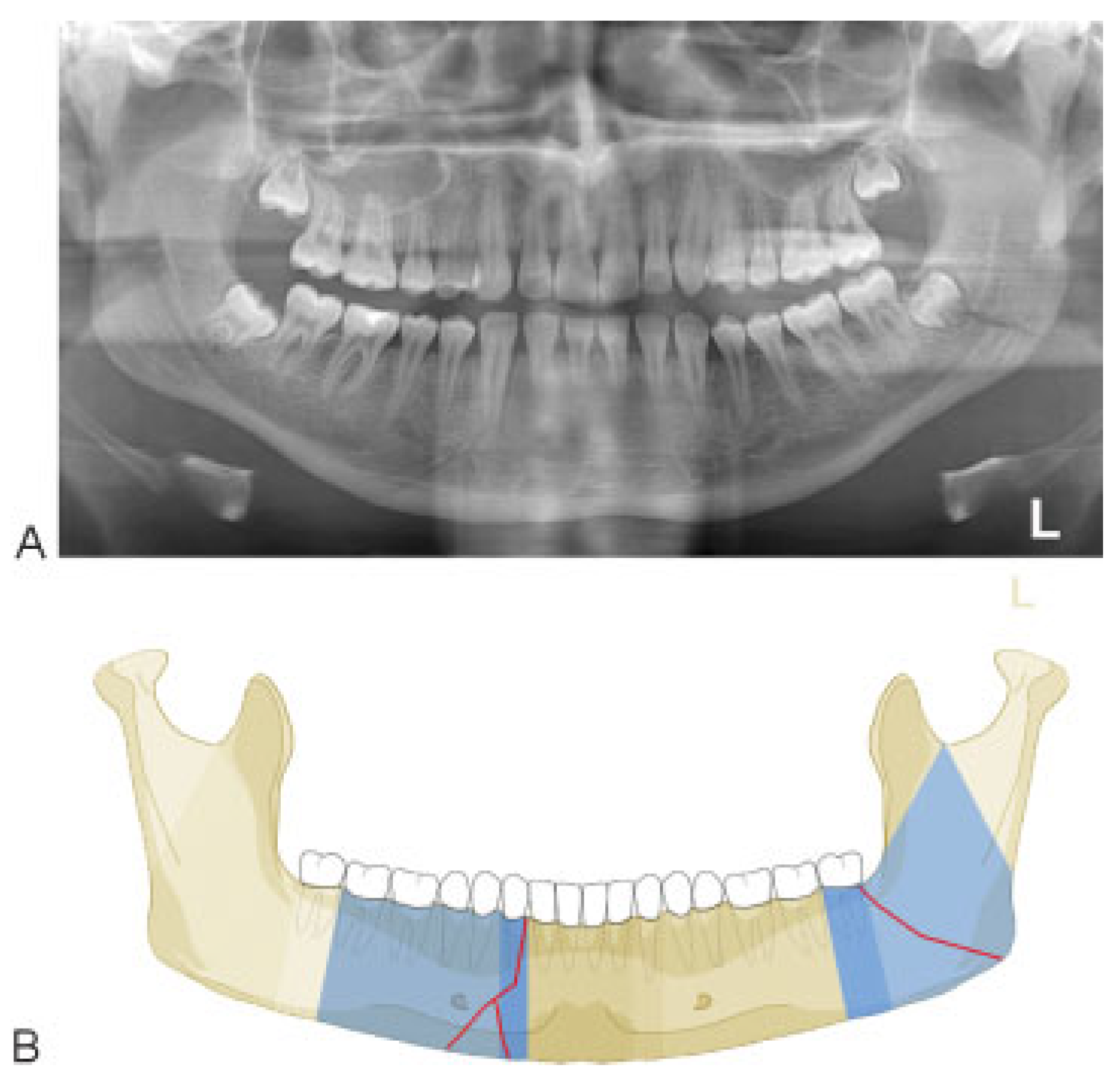
Mandibular Body Region
Angle/Ramus Region
Coronoid Process
Condylar Process
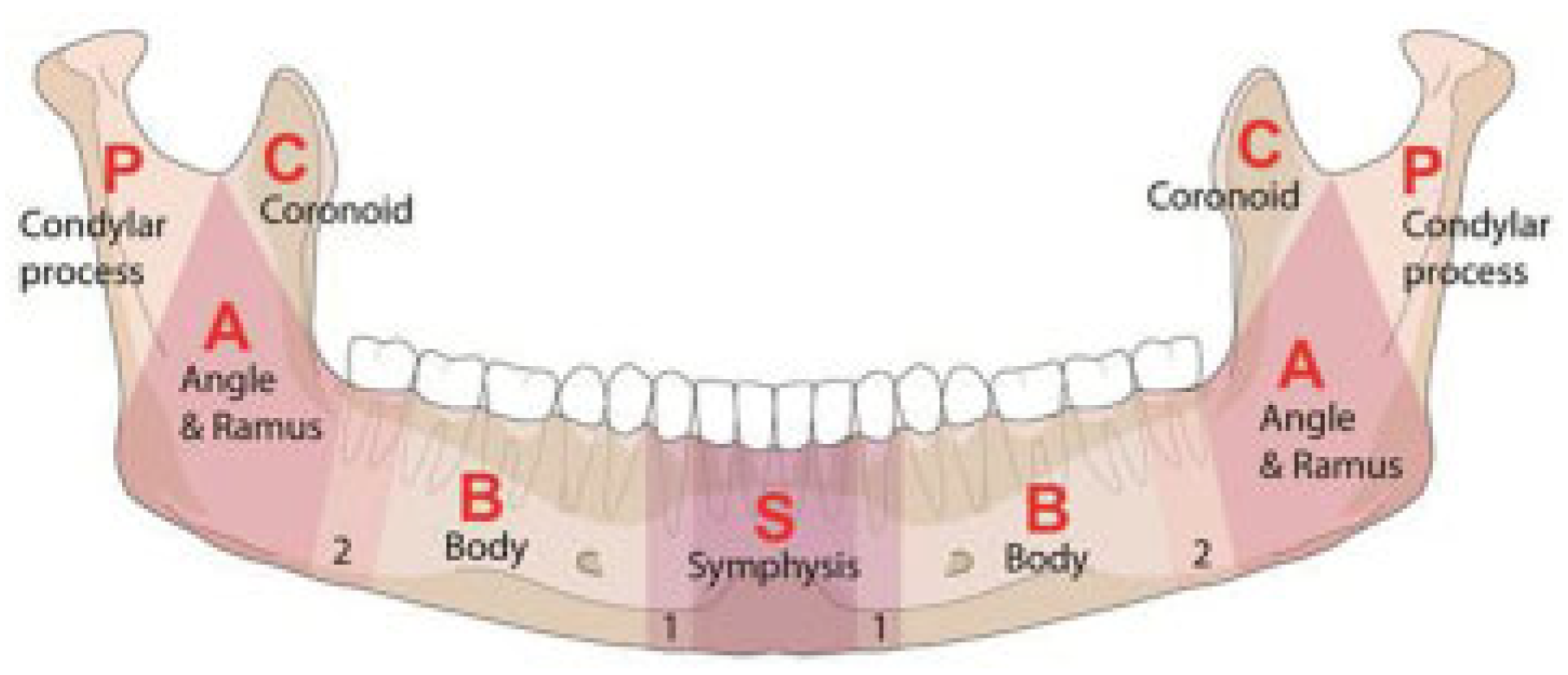
Confinement—Fractures Located within Anatomical Regions
- • “Confined” fracture pattern: the fracture, irrespective of its morphology, remains within an anatomical region (including a transition zone) and does not extend into an adjoining region across a transition zone.
- • “Nonconfined” fracture pattern: the fracture crosses at least one transition zone and may extend over one or more adjoining region.
Fracture Coding and Topographical Distribution
- S = Symphysis/parasymphysis
- B = Body
- A = Angle/ramus
- C = Coronoid process
- P = Condylar process
Case Examples
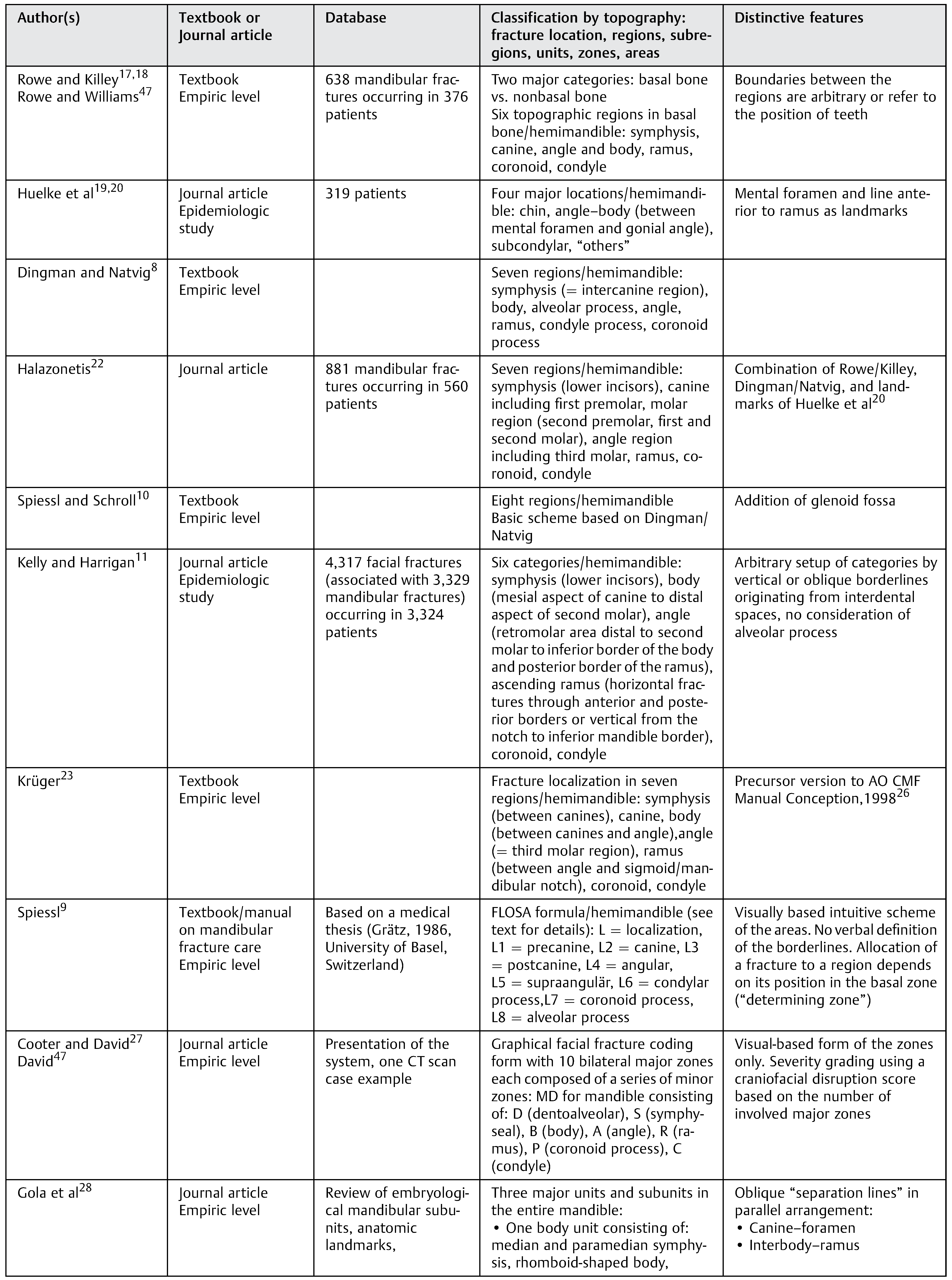
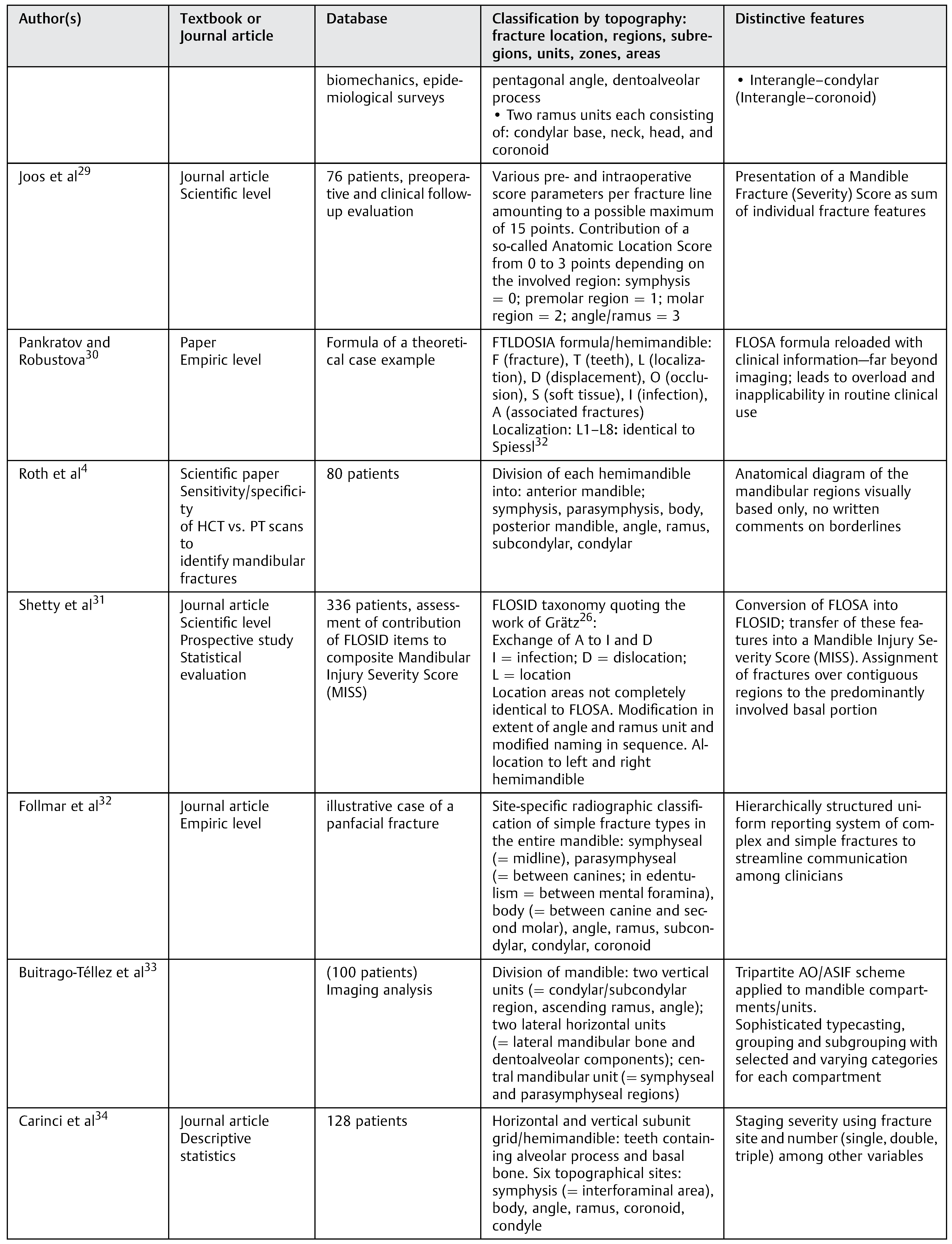
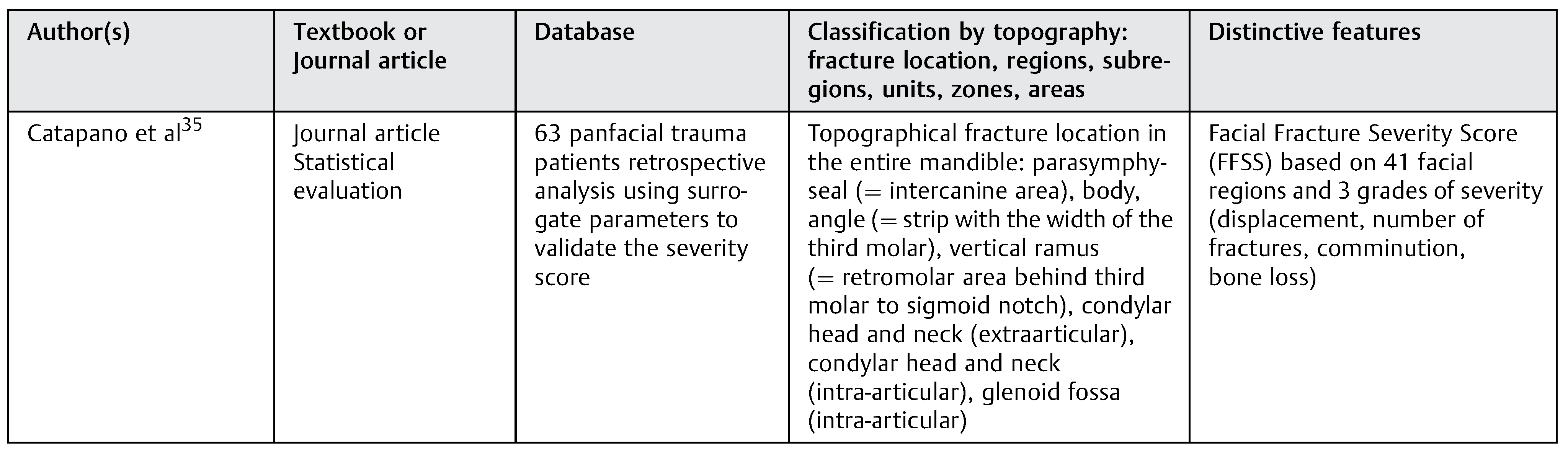
Discussion
Concluding Note
Acknowledgments
Appendix A. Additional level 2 coding examples of mandibular fractures

References
- Audigé, L.; Cornelius, C.P.; Di Ieva, A.; Prein, J.; CMF Classification Group. The first comprehensive AO classification system for fractures of the craniomaxillofaxial skeleton: rationale, methodological background, developmental process and objectives. Craniomaxillofac Trauma Reconstr 2014, 7 (Suppl 1), S6–S14. [Google Scholar]
- Cornelius, C.P.; Audigé, L.; Kunz, C.; et al. The comprehensive AOCMF classification system: mandible fractures - level 3 tutorial. Craniomaxillofac Trauma Reconstr 2014, 7 (Suppl 1), S31–S43. [Google Scholar]
- Buitrago-Téllez, C.H.; Cornelius, C.P.; Prein, J.; et al. The comprehensive AOCMF classification system: radiological issues and systematic approach. Craniomaxillofac Trauma Reconstr 2014, 7 (Suppl 1), S123–S130. [Google Scholar] [CrossRef]
- Roth, F.S.; Kokoska, M.S.; Awwad, E.E.; et al. The identification of mandible fractures by helical computed tomography and panorex tomography. J Craniofac Surg 2005, 16, 394–399. [Google Scholar] [CrossRef] [PubMed]
- Anatomica, T. International Anatomical Terminology, 1st ed.Thieme Medical Publishers: New York, NY, 1998. [Google Scholar]
- Neff, A.; Cornelius, C.P.; Rasse, M.; et al. The comprehensive AOCMF classification system: condylar process fractures - level 3 tutorial. Craniomaxillofac Trauma Reconstr 2014, 7 (Suppl 1), S44–S58. [Google Scholar]
- Marsh, J.L.; Slongo, T.F.; Agel, J.; et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007, Suppl), S1–S133. [Google Scholar]
- Dingman, R.O.; Natvig, P. Surgery of Facial Fractuers; WB Saunders: Philadelphia, PA, 1964. [Google Scholar]
- Spiessl, B. Spiessl, B., Ed.; AO classification of mandibular fractures. In Internal Fixation of the Mandible-A Manual of AO/ASIF Principles, 2nd ed.; Springer Verlag: Berlin, Heidelberg, New York, London, Paris, Tokyo, 1989. [Google Scholar]
- Spiessl, B.; Schroll, K. Nigst, H., Ed.; Unterkieferfrakturen, Vorbemerkungen. In Spezielle Frakturen-und Luxationslehre, 1st ed.; Thieme Verlag: Stuttgart New York, 1972; pp. 102–107. [Google Scholar]
- Kelly, D.E.; Harrigan, W.F. A survey of facial fractures: Bellevue Hospital, 1948-1974. J Oral Surg 1975, 33, 146–149. [Google Scholar]
- Bormann, K.H.; Wild, S.; Gellrich, N.C.; et al. Five-year retrospective study of mandibular fractures in Freiburg, Germany: incidence, etiology, treatment, and complications. J Oral Maxillofac Surg 2009, 67, 1251–1255. [Google Scholar] [CrossRef]
- Meaders, R.A.; Sullivan, S.M. The development and use of a computerized database for the evaluation of facial fractures incorporating aspects of the AAOMS Parameters of Care. J Oral Maxillofac Surg 1998, 56, 924–929. [Google Scholar]
- Olson, R.A.; Fonseca, R.J.; Zeitler, D.L.; Osbon, D.B. Fractures of the mandible: a review of 580 cases. J Oral Maxillofac Surg 1982, 40, 23–28. [Google Scholar] [CrossRef]
- Ellis, E., III; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol 1985, 59, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Abreu, M.H.; Freire-Maia, B.; Souza, LN. 1,454 mandibular fractures: a 3-year study in a hospital in Belo Horizonte, Brazil. J Craniomaxillofac Surg 2012, 40, 116–123. [Google Scholar] [PubMed]
- Rowe, N.L.; Killey, H.C. Fractures of the facial skeleton. Williams & Wilkins: Baltimore, 1968. [Google Scholar]
- Rowe, N.L.; Killey, H.C. General considerations and classification of mandibular fractures; Williams & Wilkins: Baltimore, 1955. [Google Scholar]
- Huelke, D.F.; Burdi, A.R.; Eyman, C.E. Association between mandibular fractures and site of trauma, dentition and age. J Oral Surg Anesth Hosp Dent Serv 1962, 20, 478–481. [Google Scholar] [PubMed]
- Huelke, D.F.; Burdi, A.R.; Eymen, C. Mandibular fractures as related to site of trauma and state of dentition. J Dent Res 1961, 40, 1262–1266. [Google Scholar]
- Luyk, N.H.; Ferguson, J.W. The diagnosis and initial management of the fractured mandible. Am J Emerg Med 1991, 9, 352–359. [Google Scholar] [CrossRef]
- Halazonetis, J.A. The ‘weak’ regions of the mandible. Br J Oral Surg 1968, 6, 37–48. [Google Scholar]
- Krüger, E. Krüger, E., Schilli, W., Eds.; Mandibular fractures, 1. Classification, diagnosis and fundamentals of treatment. Quintessence Publishing Company: Oral and Maxillofacial Traumatology. Chicago, 1982; pp. 211–223. [Google Scholar]
- Prein, J. Manual of Internal Fixation in the Cranio-Facial Skeleton. Springer: New York, NY, 1998. [Google Scholar]
- Schilli, W.; Stoll, P.; Bähr, W.; Prein, J. Prein, J., Ed.; Mandibular fractures. In Manual of Internal Fixation in the Cranio-Facial Skeleton; Springer: New York, NY, 1998; pp. 86–87. [Google Scholar]
- Grätz, K. Eine neue Klassifikation zur Einteilung von Unterkiefer- frakturen Universität Basel; 1986. 1986.
- Cooter, R.D.; David, D.J. Computer-based coding of fractures in the craniofacial region. Br J Plast Surg 1989, 42, 17–26. [Google Scholar] [CrossRef]
- Gola, R.; Cheynet, F.; Carreau, J.P.; Amrouche, M. Proposal of a new topographic classification of mandibular fractures [in French]. Rev Stomatol Chir Maxillofac 1996, 97, 59–71. [Google Scholar]
- Joos, U.; Meyer, U.; Tkotz, T.; Weingart, D. Use of a mandibular fracture score to predict the development of complications. J Oral Maxillofac Surg 1999, 57, 2–5, discussion 5–7. [Google Scholar] [CrossRef]
- Pankratov, A.S.; Robustova, T.G. A classification of mandibular fractions [in Russian]. Stomatologia (Mosk) 2001, 80, 29–32. [Google Scholar]
- Shetty, V.; Atchison, K.; Der-Matirosian, C.; et al. The mandible injury severity score: development and validity. J Oral Maxillofac Surg 2007, 65, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Follmar, K.E.; Baccarani, A.; Das, R.R.; et al. A clinically applicable reporting system for the diagnosis of facial fractures. Int J Oral Maxillofac Surg 2007, 36, 593–600. [Google Scholar] [CrossRef]
- Buitrago-Téllez, C.H.; Audigé, L.; Strong, B.; et al. A comprehensive classification of mandibular fractures: a preliminary agreement validation study. Int J Oral Maxillofac Surg 2008, 37, 1080–1088. [Google Scholar] [CrossRef] [PubMed]
- Carinci, F.; Arduin, L.; Pagliaro, F.; et al. Scoring mandibular fractures: a tool for staging diagnosis, planning treatment, and predicting prognosis. J Trauma 2009, 66, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Catapano, J.; Fialkov, J.A.; Binhammer, P.A.; et al. A new system for severity scoring of facial fractures: development and validation. J Craniofac Surg 2010, 21, 1098–1103. [Google Scholar] [CrossRef]
- Loukota, R.A.; Eckelt, U.; De Bont, L.; Rasse, M. Subclassification of fractures of the condylar process of the mandible. Br J Oral Maxillofac Surg 2005, 43, 72–73. [Google Scholar] [CrossRef]
- Ichim, I.; Swain, M.V.; Kieser, J.A. Mandibular stiffness in humans: numerical predictions. J Biomech 2006, 39, 1903–1913. [Google Scholar] [CrossRef]
- Craig, M.; Bir, C.; Viano, D.; Tashman, S. Biomechanical response of the human mandible to impacts of the chin. J Biomech 2008, 41, 2972–2980. [Google Scholar] [CrossRef]
- Bell, R.B.; Wilson, D.M. Is the use of arch bars or interdental wire fixation necessary for successful outcomes in the open reduction and internal fixation of mandibular angle fractures? J Oral Maxillofac Surg 2008, 66, 2116–2122. [Google Scholar] [CrossRef]
- Ellis, E., III. Management of fractures through the angle of the mandible. Oral Maxillofac Surg Clin North Am 2009, 21, 163–174. [Google Scholar] [CrossRef]
- Fox, A.J.; Kellman, R.M. Mandibular angle fractures: two-miniplate fixation and complications. Arch Facial Plast Surg 2003, 5, 464–469. [Google Scholar] [PubMed]
- Gear, A.J.; Apasova, E.; Schmitz, J.P.; Schubert, W. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 2005, 63, 655–663. [Google Scholar] [PubMed]
- Haug, R.H.; Serafin, B.L. Mandibular angle fractures: a clinical and biomechanical comparison-the works of Ellis and Haug. Craniomaxillofac Trauma Reconstr 2008, 1, 31–38. [Google Scholar]
- Haug, R.H.; Peterson, G.P.; Goltz, M. A biomechanical evaluation of mandibular condyle fracture plating techniques. J Oral Maxillofac Surg 2002, 60, 73–80, discussion 80–81. [Google Scholar]
- Schierle, H.P.; Schmelzeisen, R.; Rahn, B.; Pytlik, C. One- or two-plate fixation of mandibular angle fractures? J Craniomaxillofac Surg 1997, 25, 162–168. [Google Scholar] [CrossRef]
- Rowe, N.L.; Williams, J.L. Maxillofacial Injuries. Churchill Livingstone: Edinburgh, 1985; Volume 1. [Google Scholar]
- David, D.J. Facial fracture classification: current thoughts and applications. J Craniomaxillofac Trauma 1999, 5, 31–36, discussion 37–38. [Google Scholar]



© 2014 by the author. The Author(s) 2014.
Share and Cite
Cornelius, C.-P.; Audigé, L.; Kunz, C.; Rudderman, R.; Buitrago-Téllez, C.H.; Frodel, J.; Prein, J. The Comprehensive AOCMF Classification System: Mandible Fractures—Level 2 Tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7, 15-30. https://doi.org/10.1055/s-0034-1389557
Cornelius C-P, Audigé L, Kunz C, Rudderman R, Buitrago-Téllez CH, Frodel J, Prein J. The Comprehensive AOCMF Classification System: Mandible Fractures—Level 2 Tutorial. Craniomaxillofacial Trauma & Reconstruction. 2014; 7(s1):15-30. https://doi.org/10.1055/s-0034-1389557
Chicago/Turabian StyleCornelius, Carl-Peter, Laurent Audigé, Christoph Kunz, Randal Rudderman, Carlos H. Buitrago-Téllez, John Frodel, and Joachim Prein. 2014. "The Comprehensive AOCMF Classification System: Mandible Fractures—Level 2 Tutorial" Craniomaxillofacial Trauma & Reconstruction 7, no. s1: 15-30. https://doi.org/10.1055/s-0034-1389557
APA StyleCornelius, C.-P., Audigé, L., Kunz, C., Rudderman, R., Buitrago-Téllez, C. H., Frodel, J., & Prein, J. (2014). The Comprehensive AOCMF Classification System: Mandible Fractures—Level 2 Tutorial. Craniomaxillofacial Trauma & Reconstruction, 7(s1), 15-30. https://doi.org/10.1055/s-0034-1389557



