Biodegradable plates have become a routine method in maxillofacial, craniofacial, and orthopedic reconstruction. These materials provide rigid fixation for bone healing, and degrade as the fractured bone regains strength. These characteristics may prove particularly ideal for the pediatric population, in which bone growth and turnover create potential problems for metallic plates.
Recently, there have been reports of aseptic foreignbody reactions, leading to sterile abscesses at implant fixation sites, sometimes years after the original placement of an implant [
1]. Previous literature postulated inadequate polymer degradation and debris accumulation as the primary causes [
1,
2]. The main components of biodegradable plates, polylactic isomers, and/or polyglycolic acids (PGA), demonstrate differing inherent degradation properties and rates. The current generation of commercial biodegradable plates is formulated to balance degradation and stability by altering the ratio of these polymeric components. The polymer’s ratio determines the mechanism and ultimate rate of degradation. These features may mediate the body’s immunological response to this material [
2,
3]. The purpose of this in vivo study is to compare the biocompatibility of two commonly used fixation plates, in an animal model, through the assessment of local foreign-body reactions. Given previous reports of delayed foreign-body reactions with poly-L-lactide materials [
4,
5], we hypothesize that the poly-lactide-glycolic acid (PLGA) plate, which has the higher ratio of L-lactide, will exhibit more significant foreign-body reactions than the poly(D/L)lactic acid (PDLLA) plates.
Materials and Methods
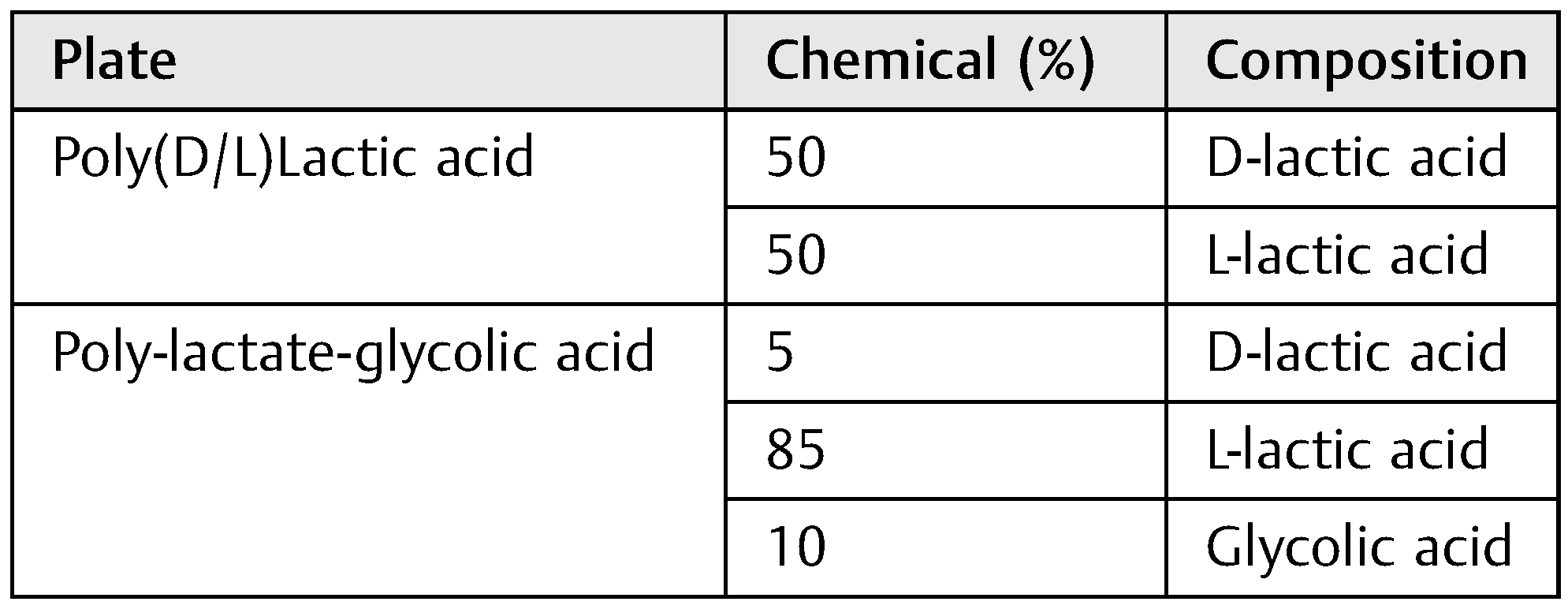
Two types of bone plates were used for implantation (
Table 1). The PLGA plate is a copolymer composed of poly-L-lactide, D-lactide and glycolide in an 85/5/10 molecular ratio (Delta System, Stryker Osteosynthesis, Freiburg, Germany). The PDLLA plate is a copolymer of D and L isomers of lactide, in a 1:1 molecular ratio (Resorb-X System, KLS-Martin, Jacksonville, FL). Both plates were 1.5 × 1.5 cm in width and length. The PDLLA plate had a thickness of 2.0 mm and the PLGA plate had a thickness of 1.4 mm.
Animal Study
A total of 15 mature male rabbits were used in this in vivo study. All research was performed in accordance with guidelines detailed by and with approval from the Institutional Animal Care and Use Committee. All procedures were performed under sterile conditions.
The rabbits were anesthetized with inhaled 1% isoflurane in conjunction with intramuscular drug enforcement administration (DEA) Schedule III medications (ketamine 42.8 mg, xylazine 8.2 mg, acepromazine 0.7 mg) at dosage of 0.5 to 0.7 mL/kg. After adequate anesthesia, the dorsum of head was shaved and prepared using chlorhexidine gluconate. Two 1-cm transverse skin incisions were made, one at the anterior aspect of the dorsal head, and one at the posterior aspect of the dorsal head. Tissue was dissected down to the calvarial periosteum, and a periosteal pocket, measuring 1.5 × 1.5 cm, was created at each incision site. A sterile PLGA plate was placed in the anterior pocket, and a sterile PDLLA plate was placed in the posterior pocket. The subcutaneous tissue and skin were then closed using 3–0 Monocryl (Ethicon, Somerville, NJ). At the conclusion of the procedure, 0.5cc of 1% bupivacaine was infused at the surgery site.
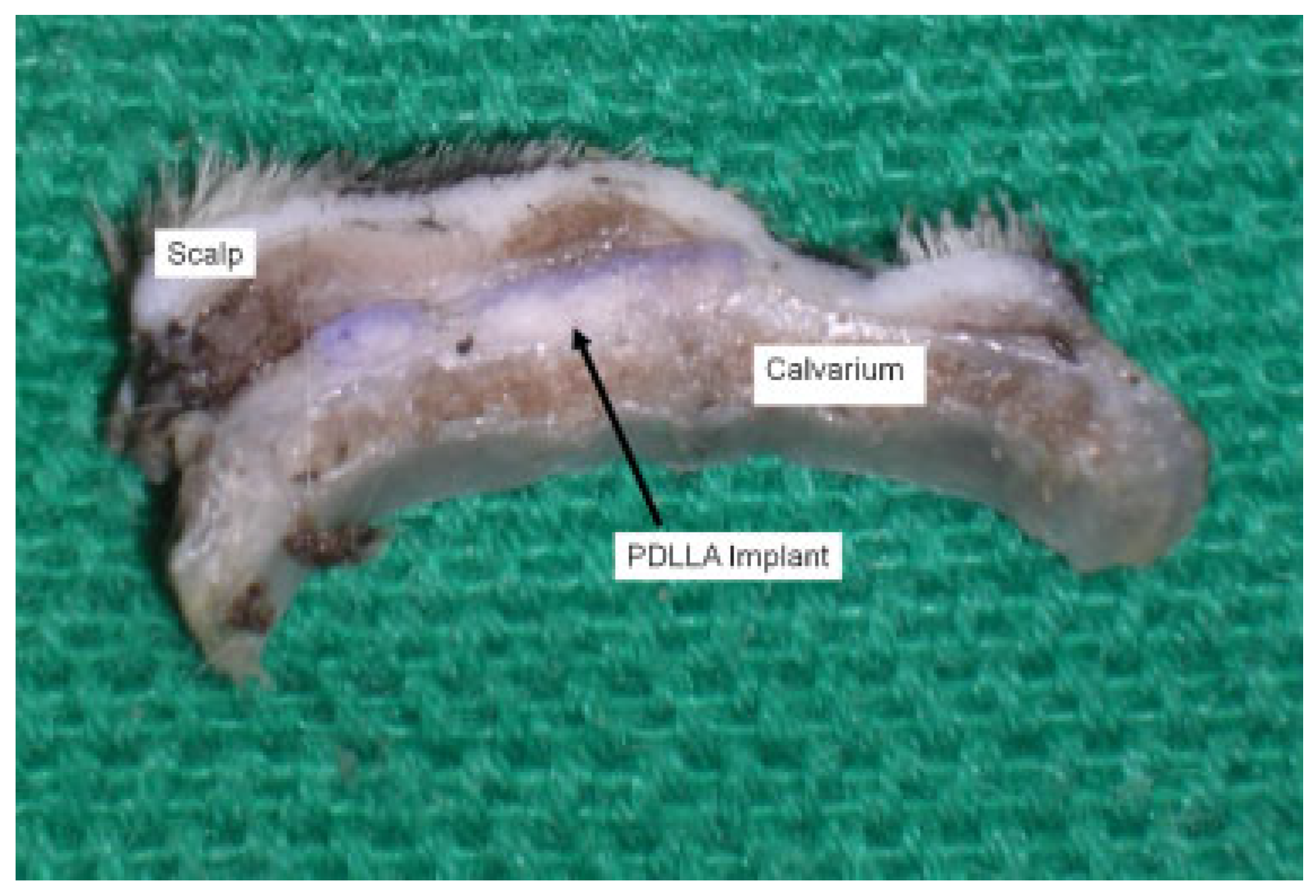
Of the 15 animals, 5 animals were humanely killed at each of the three time points—3, 6, and 12 months postoperatively. All animals were euthanized via overdose of beuthanasia (1 mL/4.55 kg, intravenous) under general anesthesia. The hair over the dorsal scalp was then shaved. The two regions of the skull implanted with plates were excised en bloc with overlying soft tissue and skin. The samples were fixed in 4% formaldehyde/1% glutaraldehyde.
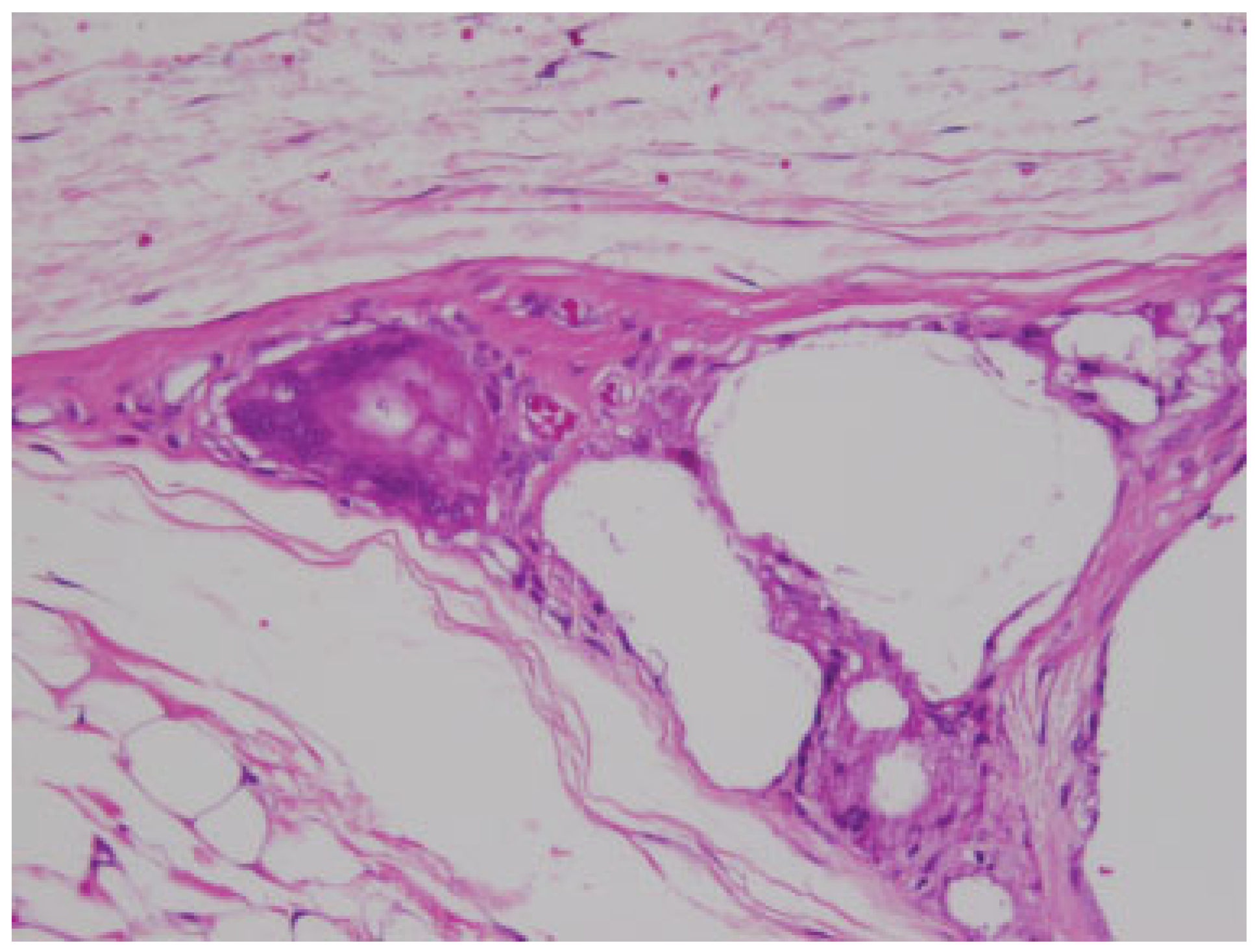
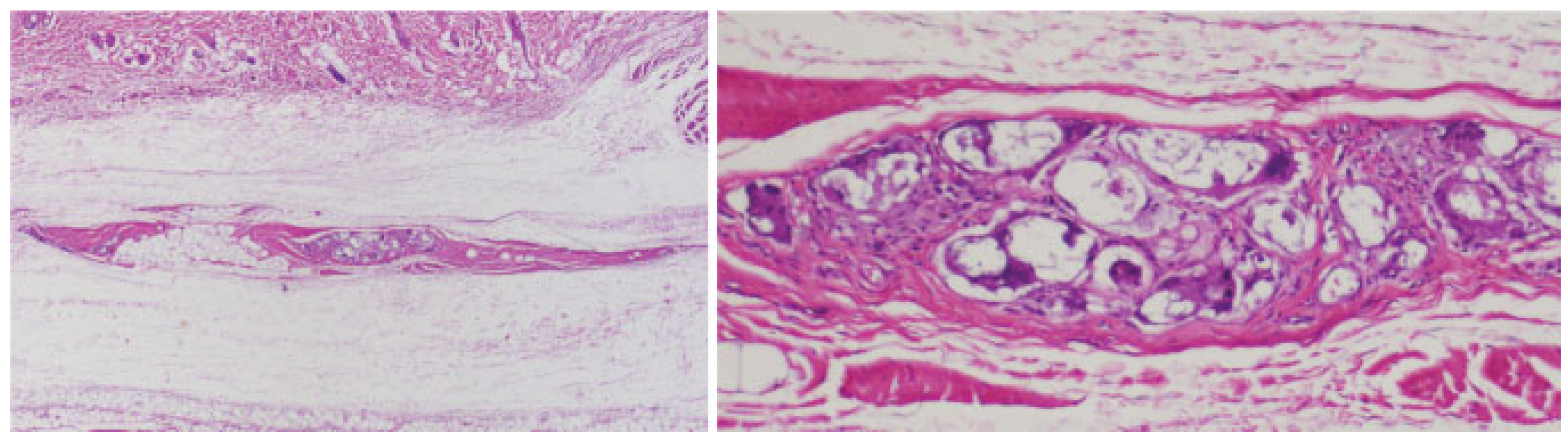
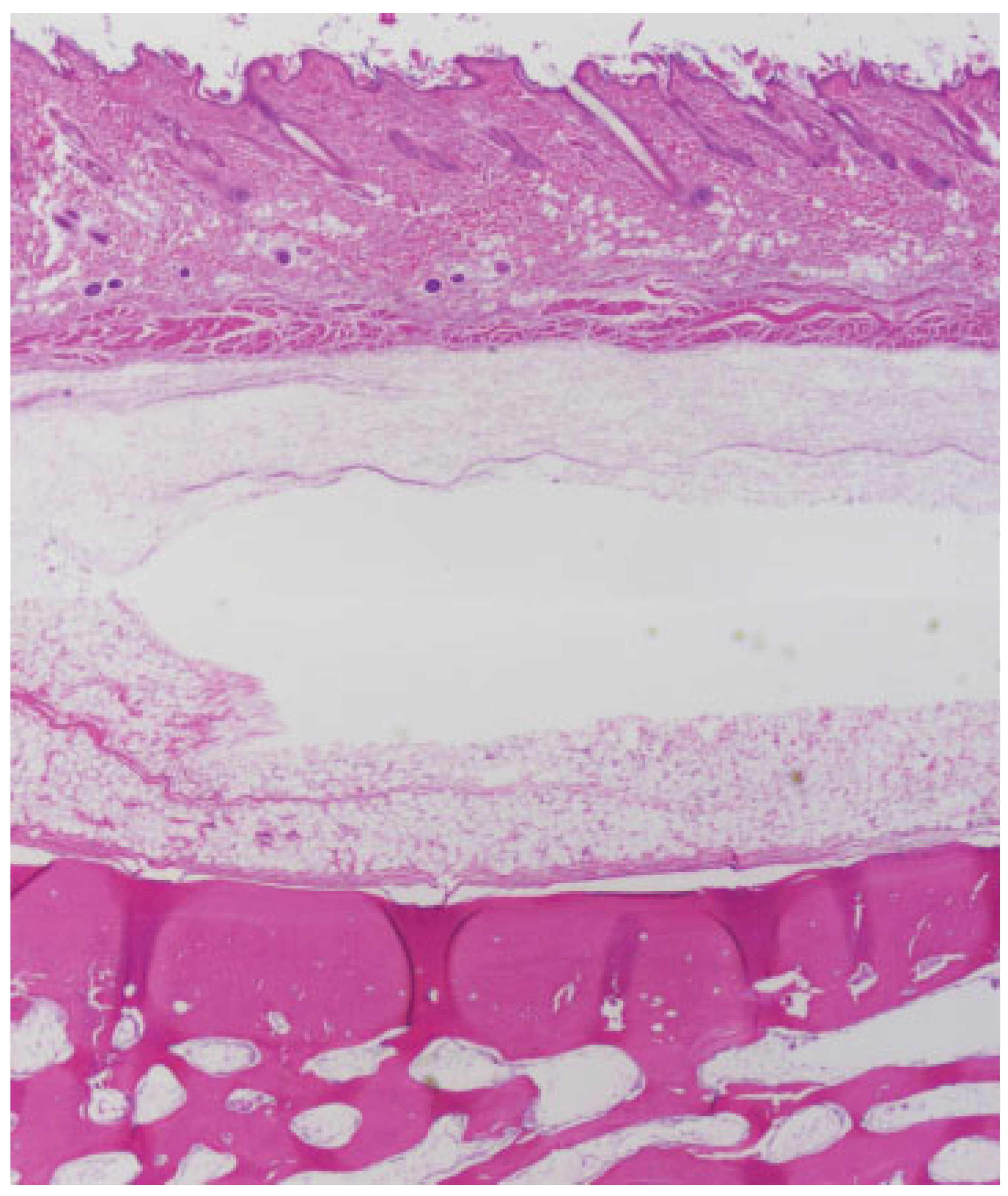
Tissue sections were obtained from decalcified, formalinfixed, paraffin-embedded tissue blocks following standardized tissue processing. The resultant tissue sections were stained with hematoxylin and eosin using a standardized automated system. Digital images were captured and compared among the treatment groups with original magnifications of ×40, ×100, ×200, and ×400. Qualitative assessment of cellular infiltration and plate resorption were based upon previously published criteria (
Table 2) [
6].
Discussion
The development of biodegradable plates was prompted from multiple publications citing concerns over migration, need for removal, and growth restriction as a result of metallic plate used in children. Skin irritation, infection, palpability, and pain were cited as the most common reasons for plate removal [
7,
8]. Intracranial migration of metallic plates poses a significant problem as well [
9]. Less clear are the effects of metallic plates on bone growth. Some animal models have suggested minimal and isolated restriction at the site of fixation, but its effect on humans is difficult to discern [
8,
10]. These potential complications would be mitigated with the use of biodegradable plates.
The ideal biodegradable plate is mechanically strong, adaptable to allow healing, and undergoes resorption in a predictable time frame. In addition, the plate material needs to be biocompatible with the recipient environment, and causes minimal local inflammatory reactions. There are multiple factors influencing the occurrence of local foreignbody inflammatory reactions (
Table 4). Among these, chemical composition has been studied the most.
Polylactic acid (PLA) and PGAs are the primary components of most biodegradable plates. The biomechanical and resorptive properties of these plates vary depending on the ratio of lactic acid isomers and/or glycolic acid [
11]. PLA degradation is biphasic. Early degradation occurs via hydrolysis of ester bonds [
3,
11]. The resulting degradation product crystallizes and undergoes a secondary hydrolysis, which is the ratelimiting step [
3]. The final end products, CO
2 and H
2O, are ultimately metabolized by the liver [
11]. The rate of degradation depends upon the crystallinity and hydrophobicity of the early by-products. L-isomers form crystalline lattices that are highly hydrophobic and more resistant to degradation than the D-isomers [
3,
12]. Different ratios of the two determine their polymer chain organization and orientation. Poly L-lactic acid crystalline particles have been identified within the cytoplasm of local phagocytic cells years after implantation [
2].
More amorphous polymers, such as PGA, are inherently less hydrophobic, undergo more rapid breakdown and are susceptible to bulk degradation or fragmentation of the material. PGA is more hydrophilic and undergoes resorption more quickly. PGA is typically used in conjunction with PLA to improve the structural integrity of an implant, as pure PGA does not offer the necessary strength for fracture fixation. These semicrystalline polymers typically exhibit degradation at the outer surface of the material, and are less likely to fragment or undergo bulk degradation.
Previous clinical studies have demonstrated that polylactic/glycolic acid implants are associated with up to a 22% prevalence of developing a local foreign-body inflammatory reaction, or “sterile abscess” [
1,
2,
4,
13]. Bergsma et al. reported that remnants from poly-L-lactide implants could lead to accumulation of localized sterile fluid up to 5.7 years after implantation, necessitating surgical drainage [
4]. These types of reactions result when the implant is either incompletely degraded or when there is a large volume of debris from degradation overwhelming metabolic clearance [
1]. Long-term follow-up studies suggest that poly-L-lactide implants are particularly prone to developing delayed foreign-body reactions even years after implantation; while poly-L-lactidecoglycolic acid implants demonstrate reactions significantly earlier, at 3 to 6 months following implantation depending on the polymeric ratios [
2,
11]. In addition, delayed foreign-body reactions were encountered with ultrasound activated polyD/L-lactide resorbable pins [
5]. These findings may suggest that the inherent properties of the materials may be altered by external factors, such as ultrasound [
5].
Our findings demonstrated that the PDLLA implant (50:50, D:L-lactide) fragmented and resorbed more quickly on visual inspection than PLGA material, with only microscopically visualized residual material at 6 and 12 months postimplantation. There was a large amount of inflammatory cell infiltrate during degradation; however, this reaction was contained within the implant capsule. There was no case of clinically obvious local induration or infection requiring intervention. We postulate that the higher ratio of D-lactide to L-lactide increased the degradability of the implant without overwhelming the clearance metabolism of the local tissue. Further investigation will be necessary to see if the microscopic residues persist in long-term follow-up after the 12-month-study period.
In contrast, the PLGA implant material studied (85:5:10, Llactide:D-lactide:glycolic acid), on visual inspection, showed minimal signs of resorption at 3, 6, and 12 months. Previously published data by Landes et al. report that PLGA implants (82:18 LactoSorb, Lorenz Surgical, Jacksonville, FL, and 85:15 PolyMax RAPID, Synthes, Oberdorf, Switzerland) fully degrade between 12 and 18 months in humans for maxillary and mandibular fracture fixation [
2]. This same study demonstrated a 5% prevalence of clinically significant local tissue reactions at 3 months [
2]. However, our study did not find any local tissue reactions beyond fibrous capsule formation. Histologically, the PLGA implants in this study were highly inert and stable with no evidence of inflammatory infiltration in the surrounding soft tissues or bone. Host species, the recipient environment, and differing chemical compositions may explain the differences in these studies. The face is typically better vascularized than the pericranium, and may respond more readily to a foreign body, leading to earlier and more robust responses. In the Landes et al. study, the faster resorbing of the two plates demonstrated a significantly earlier local soft tissue reaction [
2]. This trend was seen in our study as well.
There are several limitations to our qualitative study. Although the primary goal of this study is to evaluate the foreign-body reaction, quantification of plate resorption using biomechanical testing would be beneficial for our data analysis. Within the setting of this study, the validity of our hypothesis could not be fully evaluated, as our study perimeters did not capture any local reactions to the PLGA implants, most likely because of lack of plate integration and resorption. A follow-up study with longer time span, beyond 12 months, is necessary. In addition, as the use of biodegradable plates increases, further studies will be required to determine how these models will extrapolate to humans.