In conjunction with the development of civilizations and human society, accidents become more frequent. Mandibular fractures are common human bone fractures. The rate and the etiology of mandibular fractures differ in various studies regarding research conditions and societal specifications. Despite huge controversies, the principal causes of mandibular fractures are motor vehicle accidents and battle, mostly occurring in the body, condyle, and angle [
1]. Bone thickness in the angle region and third molar presence are influential in angle fracture prevalence [
2,
3,
4,
5,
6,
7]. Treatment of mandibular fractures has gradually evolved. In our day, various techniques have been studied and introduced supporting treatment of mandibular fractures. These methods range from intermaxillary fixation (IMF) alone to wire osteosynthesis, fixation screws, lag screws, plates, and so on [
8,
9,
10,
11,
12].
Deciding what algorithm to use for treatment of a mandibular fracture has complexities. The first consideration is whether any treatment is required. Subsequently, one must decide if reduction has to be performed in an open or closed approach, then one must consider intraoral versus extraoral approach, fracture immobilization versus rigid fixation, compression versus noncompression plate, and monocortical versus bicortical plate and lag screws [
10]. This is important to notice because if the presence of the angle fracture is distal to the dentition, IMF is not effective enough solely. Today, the rigid internal fixation method, using compression and in particular noncompression plating systems, has gained wide- spread popularity. Advantages of rigid internal fixation include avoidance or decreased time of IMF, early functioning of the mandible, increased patient’s satisfaction, shorter periods of hospitalization, and earlier return to work.
Using noncompression/monocortical miniplate fixation for osteosynthesis of mandibular fractures was first introduced by Michelet et al and further advanced by Champy et al. [
5,
6].
Main advantages of osteosynthesis monocortical miniplates compared with other rigid fixation methods are:
Intraoral and extraoral incision is very small.
The risk of inferior alveolar nerve and marginal mandibular nerve injuries is decreased.
The risk of tooth root injury is decreased.
It leads to simple adaptation to the bone [
13,
14,
15,
16].
Although using bicortical plates results in more stability in the fracture site, monocortical plates are mostly utilized today, because of the reduction in nerve and vessel injury risk [
1,
2].
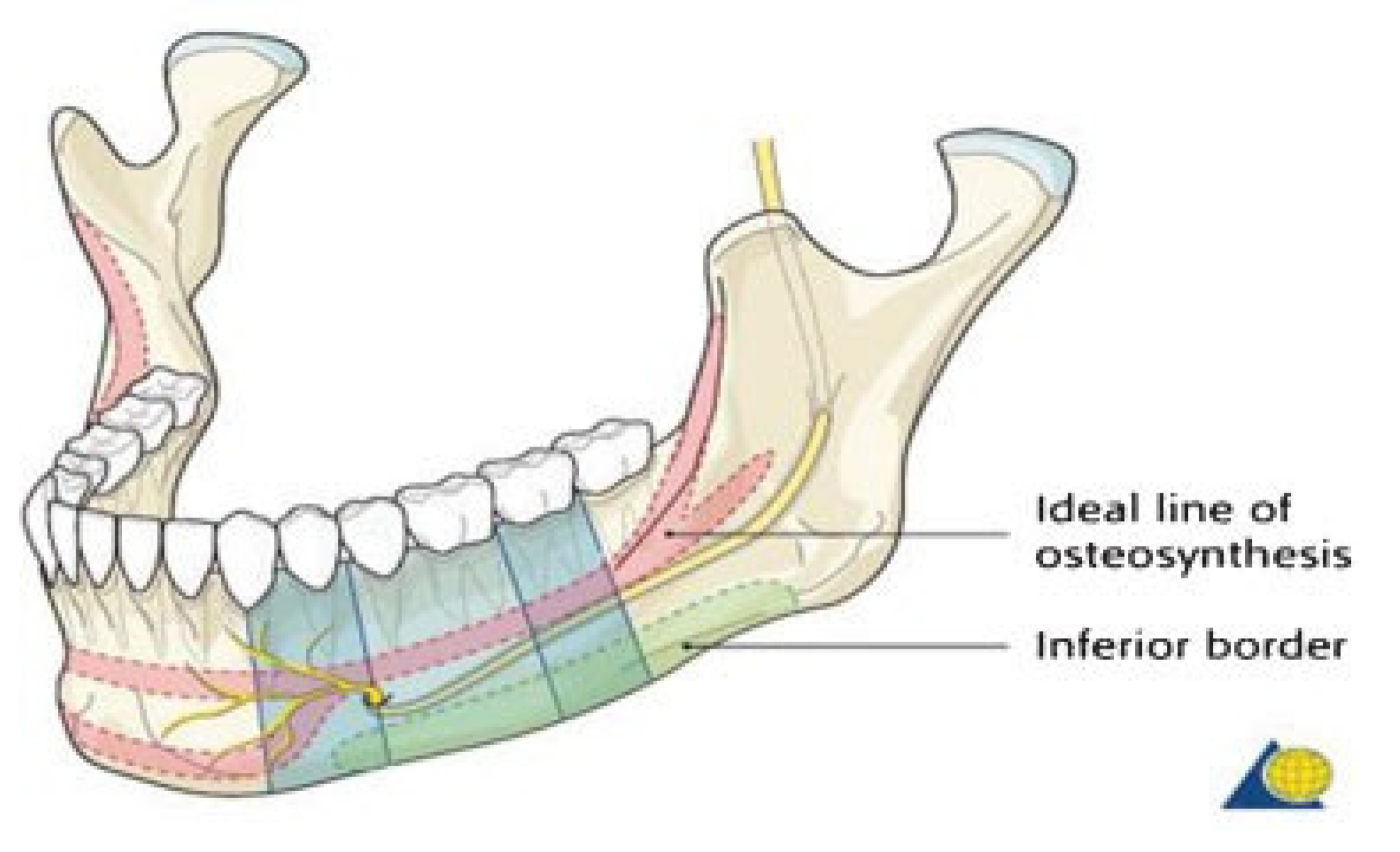
Champy and colleagues expressed that osteosynthesis will be more effective with miniplates inserted along the line called the “ideal line of osteosynthesis,” thereby counteracting the distraction forces that occur along the fracture line during mandibular function (
Figure 1). In the mandibular angle region, this line indicates that a plate might be placed either along or just below the external oblique line of the mandible [
6,
17,
18].
There are controversies in the number of miniplates used in angle fixation. Champy and colleagues showed that using one miniplate along the external oblique ridge is sufficient [
5,
6], whereas Kroon et al demonstrated that the mandibular inferior border needs one more plate to counteract inferior distraction of the lower mandibular margin caused by loading forces near the fracture line. This distraction cannot be prevented by one miniplate placed along the ideal line [
19]. The same conclusions were noted by Choi et al and Levy et al. [
13,
20]. On the other hand, some clinicians believe that rigid fixation with miniplates is not reliable, and they advise contribution of IMF [
1].
Regarding controversies about the number of miniplates, necessity of maxillomandibular fixation (MMF), and the absence of proper randomized clinical studies in treatment modalities, we decided to perform a randomized clinical study. The purpose of the present study was to compare effectiveness and complications of using one miniplate with and without MMF in mandibular angle fractures.
Patients and Methods
Forty patients with facial trauma with mandibular angle fractures referring to the maxillofacial department of Ahwaz Jundishapur University of Medical Sciences in 2008 and 2009 were categorized into two groups, each consisting of 20 individuals with sequential random entrance. The required factors to enter this study regarding to our previous experience include:
Patient could refer with more than one mandibular fracture but with no condylar and maxillary fractures.
Patients with comminuted, greenstick, or long oblique angle fractures were excluded.
Patients who were more than 2 weeks removed from trauma could not enter this study.
Patients with infected fractures were excluded.
The amount of segment displacement and whether favorable or unfavorable did not affect the entrance condition.
All patients were dentulous so maxillary and mandibular arch bars could be set.
All patients were given a sufficient explanation about entering the study, treatment method, and their follow-up.
The same surgeon in two medical centers performed intraoral treatment of patients without trocar. Monocortical noncompression miniplates (2.0 mm) all from the same commercial factory (Synthes company, Switzerland) were used.
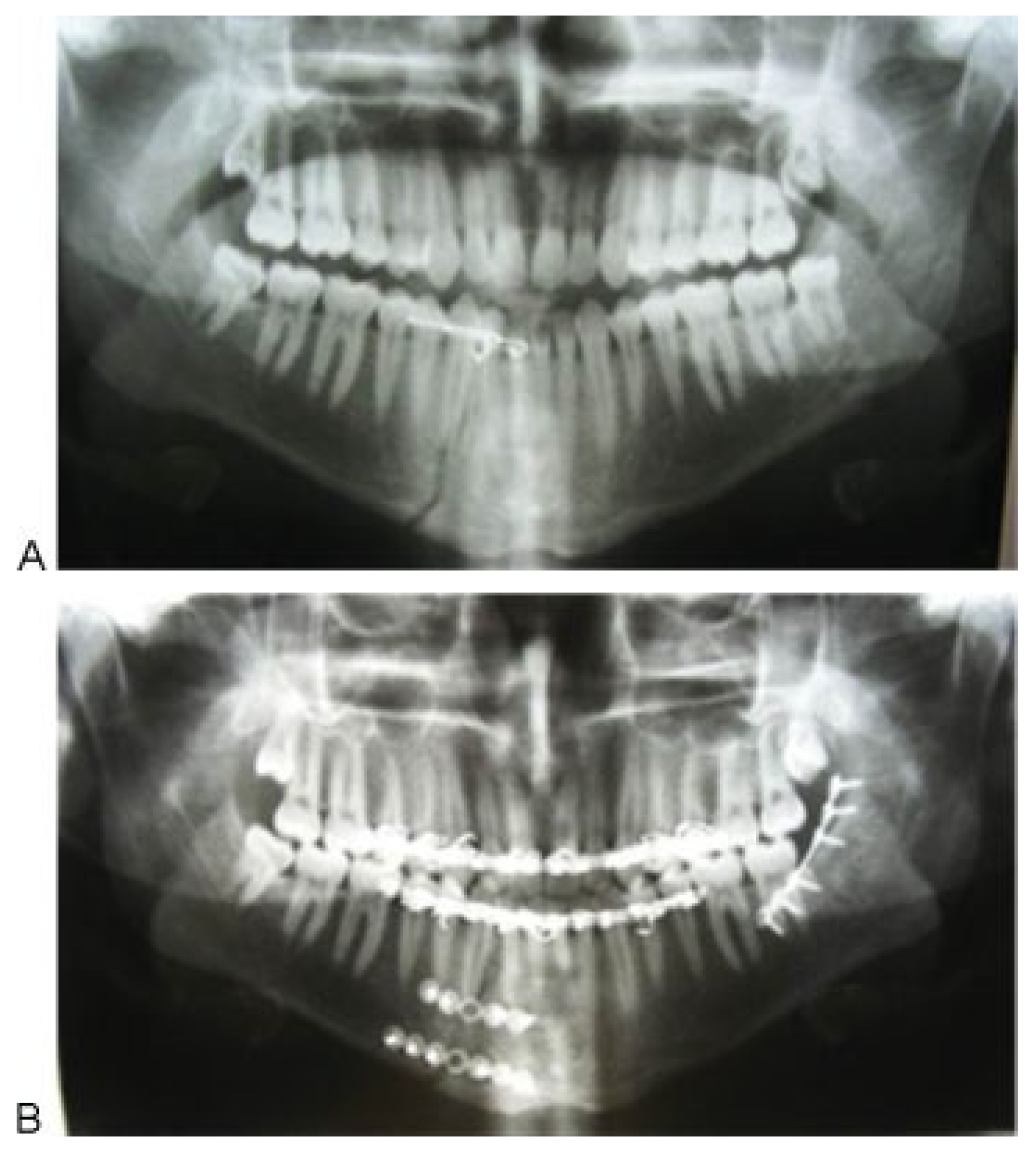
In the first group, one miniplate was placed on the external oblique ridge region (
Figure 2). Then guiding elastic bands were laid between the maxilla and mandible (two light elastic bands for each patient in the anterior dentition). These patients were not treated by rigid IMF and elastic therapy was continued for 4 weeks.
In the second group, a miniplate was fixed in the external oblique ridge. Then a rigid IMF was established for 2 weeks followed by 2 weeks of elastic therapy. All third molars, which were suspected to be infected in the fracture line, were extracted in both groups.
Follow-up examinations were performed for at least 12 weeks (maximum of 24 weeks; mean ¼ 20.25 3.95). Postoperative complications including infection, disturbed occlusion, nonunion, inadequate fixation, dehiscence, fracture of plate, and nerve injury due to surgical manipulation were evaluated.
Preoperative and postoperative radiographs (panoramic) were obtained in the same conditions. All patients received oral antibiotics and a 0.2% chlorhexidine mouthwash at the time of their presence in the maxillofacial department.
Intravenous antibiotics (Amp Cefazolin 1000 milligrams/ stat and Amp Dexamethasone 8 milligrams/stat) were administered to all patients 30 minutes before surgery and continued up to 1 day after surgery (cefazolin four times a day and dexamethasone three times a day). Then, oral antibiotics were continued for 1 week (Suspension solution Cephalexin 250 milligrams 6 hours). Chlorhexidine was used during this period.
General anesthesia was administered via nasal intubation, and then Erich arch bars were set to the maxilla and mandible. Premorbid occlusion was reestablished with bimanual manipulation. IMF was then achieved. The mucosa was infiltrated with 1% lidocaine hydrochloride with 1:100,000 epinephrine. An incision was made beginning with the first mandibular molar and was carried over the external oblique line and up the ascending ramus on the buccal side; the periosteum was then elevated, exposing the fracture. Screw holes were created using copious irrigation. Next, the miniplate was secured by screws in the fracture region(
Figure 3). According to the presence of a third molar in the fracture line, at least two screws were placed on each side of the fracture line.
Frequently in cases with third molar extraction, based on clinical evaluation of extraction socket size, three screws are placed on each side of the fracture. However, the angle fracture was the last site, and when other fractures were present, the order of fracture fixation was individualized in each case.
The statistical evaluation of the findings was performed with the help of the Statistical Package for Social Sciences software. Nonparametric tests (Mann-Whitney, Wilcoxon, and Kruskal-Wallis) were used to have a statistical comparison of demographic indicators in the two treatment groups. The Wilcoxon and Mann-Whitney tests were also used to compare treatment efficacy and complications between the two groups. Statistical significance was set at 0.05.
Results
In this study, the most common cause of mandibular angle fractures was motor vehicle crash (
n ¼ 27/40 [67.5%]), followed by assault (
n ¼ 11/40 [27.5%]), and then sports injuries (
n ¼ 2/40 [5%];
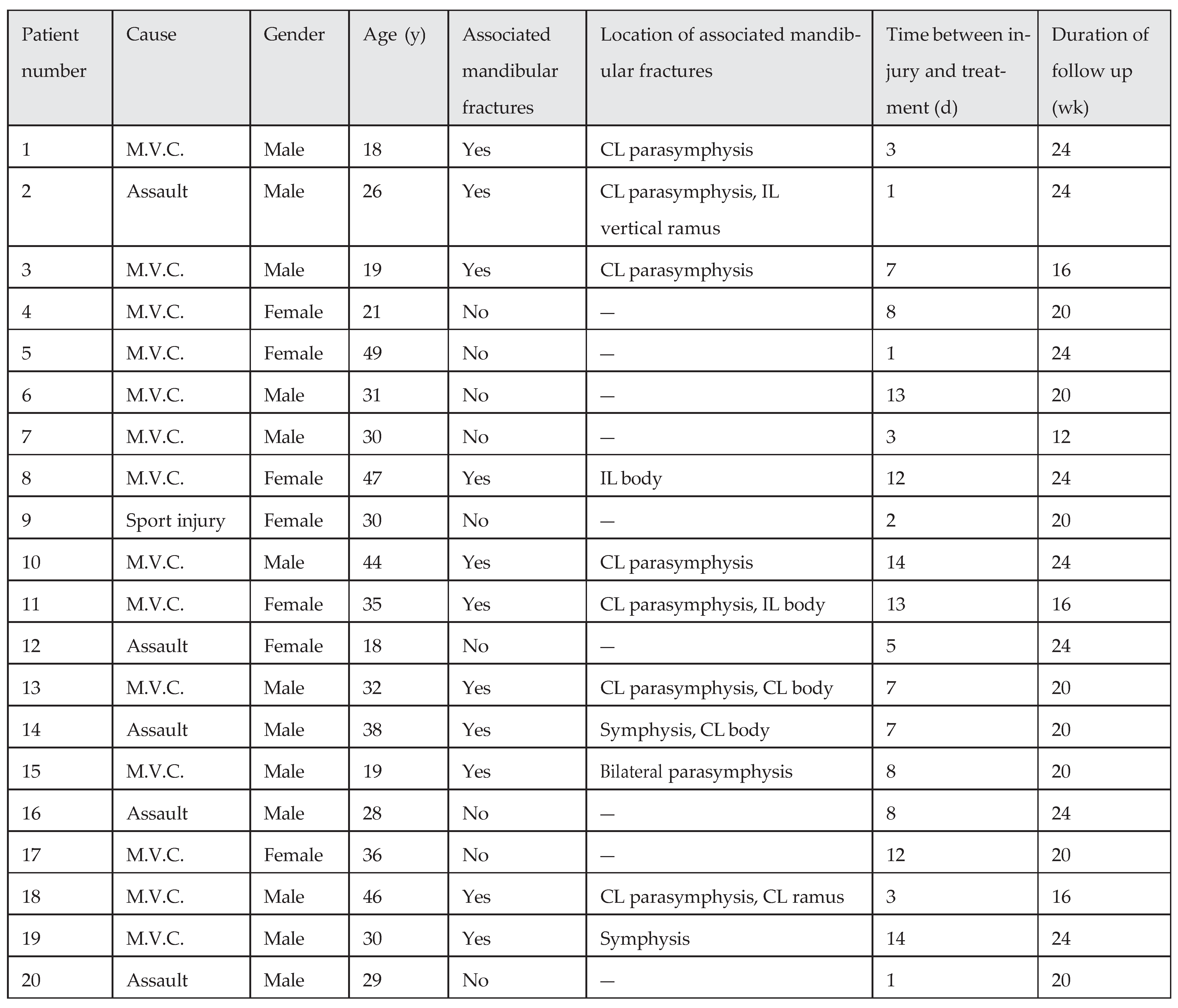
Table 1 and
Table 2). Twelve patients were women and 28 patients were men, with ages ranging from 18 to 51 years (mean ¼ 29.75 10.62). In both treatment groups (with or without MMF), the most associated fracture was parasymphysis fracture in the contralateral side (
n ¼ 18/40 [45%]). The interval of time between injury and surgical operation ranged from less than 24 hours to 14 days (mean ¼ 7.20 4.73). All patients were dentulous, so we could place Erich arch bars for MMF or elastic therapy.
Based on statistical evaluation between the two treatment groups, we found that these groups were similar in demo- graphics. Age, gender, cause, associated mandibular fractures, location of associated mandibular fractures, time between injury and treatment, and duration of follow-up were compared. The results revealed a p value of 0.255, 0.496, 0.757, 0.524, 0.624, 0.924, and 0.711, respectively, so differences are not statistically significance (p > 0.05).
First Treatment Group (without MMF) Results
Seven patients were woman and 13 patients were men, with ages ranging from 18 to 49 years (mean 31.30 9.81;
Table 1). Nine patients (45%) had isolated mandibular angle fractures and 11 patients (55%) had associated fractures. Four patients (20%) had a tooth in the mandibular angle fracture line. The mean time between injury and surgical operation and mean follow-up period were 7.10 4.63 days and 20.60 3.50 weeks, respectively.
In the follow-up period of the 20 patients, 3 (15%) were identified as having at least one postoperative complication. The first patient in this group had two concurrent complications (occlusal disturbance and nerve injury due to surgical manipulation), and the second patient had occlusal disturbance only. The first one had a tooth in the angle fracture line that was extracted surgically, and both had other fractures (the first one with an ipsilateral body fracture and the second one with contralateral parasymphysis fracture).
Malocclusions were identified a week after operation and were successfully treated by elastic therapy. Sensation was recovered within about 2 months after surgery. The third patient had wound dehiscence 3 months after surgery. This complication resolved with an intraoral incision, and the plate was successfully removed under local anesthesia. No other complications were noted in patients of this group.
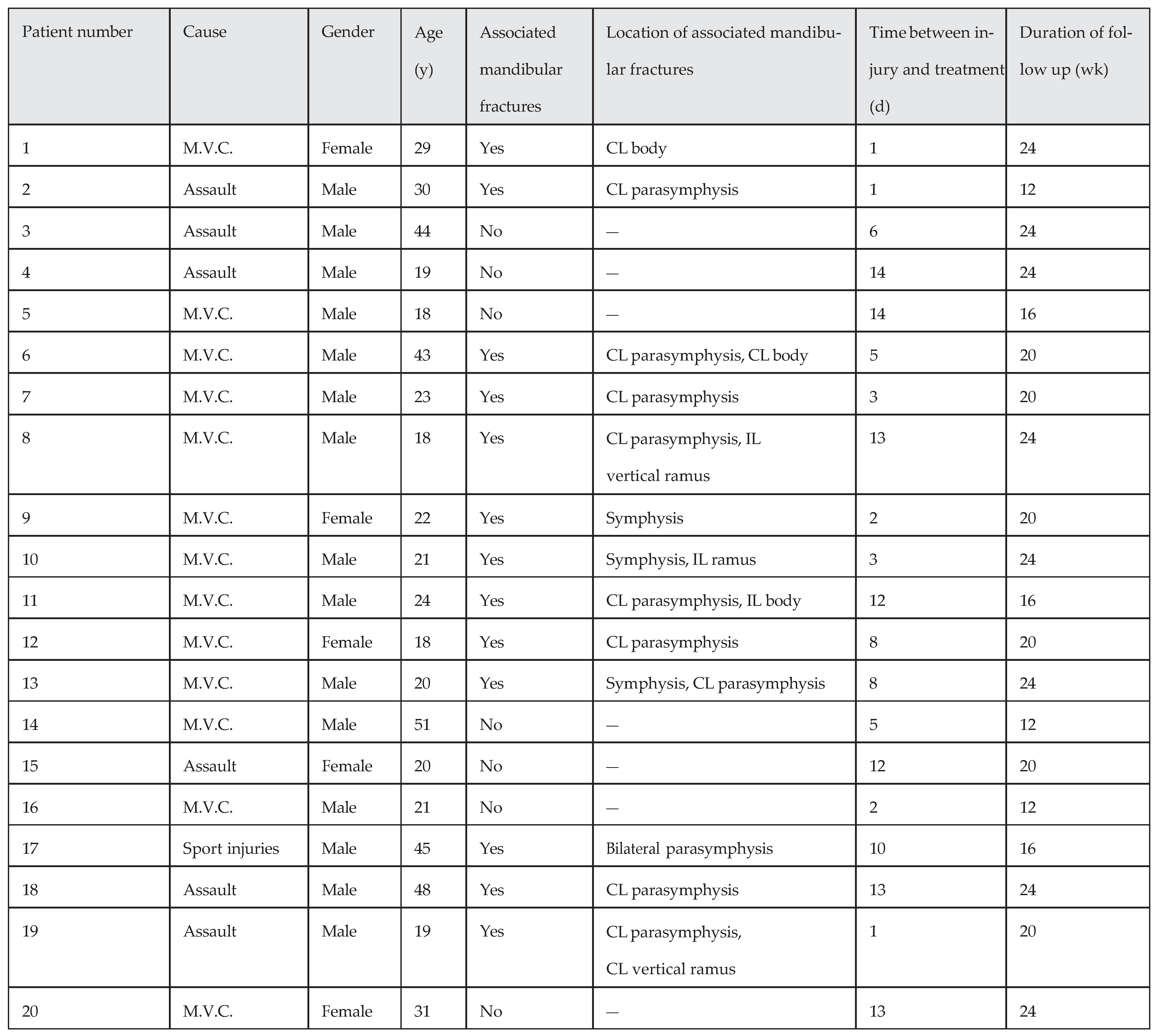
Second Treatment Group (with Rigid IMF) Results
Five patients were women and 15 patients were male, with ages ranging from 18 to 51 years (mean ¼ 28.2 11.41;
Table 2). Seven patients (35%) had an isolated mandibular angle fracture and 13 patients (65%) had associated fractures. Six patients (30%) had a tooth in the mandibular angle fracture line. The mean follow-up period in this group was 19.90 4.42 weeks, and the mean time between injury and surgical operation was 7.30 4.94 days. In the follow-up period, two patients (10%) were noted with one postoperative complication each. One patient showed infection identified 10 weeks after the operation. The patient’s symptoms were swelling and tenderness at the surgery region. The miniplate was removed subsequently under local anesthesia; the mandible was stable at the time of the plate removal and the wound healed without further event. This patient had a tooth at the angle fracture line, which was removed at operation time.
One patient had malocclusion postoperatively, which was treated by elastic therapy successfully after IMF removal. This patient had no teeth at the angle fracture line but had other fractures in the mandible (contralateral body fracture).
Results were analyzed by means of nonparametric statistical tests. The incidence of complications was analyzed between the two treatment groups by the Mann-Whitney test (p ¼ 0.79 for the first treatment group and p ¼ 0.72 for the second treatment group, not significant).
In the two groups, the incidence of complications was analyzed with the presence of the third molar and other mandibular fractures separately. This analysis, performed by Wilcoxon test gave p values of 0.56 and 0.83 (for the first group), and 0.2 and 0.10 (for the second group), respectively (not significant).
Discussion
Mandibular angle fractures are common. Reasons for this may include a thin cross-sectional area relative to the body, symphysis, and parasymphysis areas and the presence of the third molars [
2,
3,
4,
21]. This is noticeable despite developed treatment techniques; no consensus exists regarding optimal treatment [
10,
22]. Traditional treatment protocols for angle fractures involved rigid fixation in conjunction with intraoperative MMF to produce absolute stability with primary bone union and immediate postoperative function [
8].
Unfortunately, few prospective randomized studies on operative techniques have been performed and most studies are retrospective, thus we planned a randomized clinical trial study. Open reduction and internal fixation of the mandible with bone plates was first described by Schede in 1888, who used steel plates and screws [
1]. The evolution of internal fixation was aided by the discovery of biocompatible materials. Champy et al showed that the superior mandibular border was subject to tension and splaying and that the inferior border was subject to compression [
23]. Based on the biomechanical findings, Champy recommended a single noncompression miniplate on the superior border of mandibular angle fractures (Champy technique). The stability of single miniplate fixation of angle fractures was challenged by several biomechanical studies based on 3-D models, but more recent 3-D models have shown that the rotational or torsional forces at the angle are relatively weak [
24].
In the present study, we placed a single noncompression monocortical miniplate as a functionally stable fixation at the angle fracture line using the Champy technique. In our opinion and experience, because compression present in the inferior border and anatomic reduction at the angle region have a low effect on occlusion, the Champy technique in all angle fractures that are not comminuted or extended obliquely (from angle to first molar region) is quite stable and reliable. The main difference between our study and others is that we decided to treat all angle fractures—both displaced and nondisplaced, favorable and unfavorable (except comminuted and long oblique fractures)—by single miniplate fixation. In addition, because with this technique the incision is intraoral and relatively small and no trocar or extraoral incisions are used, we expected a lower complication rate. We wanted to know if a single miniplate causes more complication or instability when it is used without rigid MMF. The main two reasons we used rigid MMF in the second group are that there is no general agreement to use MMF adjunct to the Champy technique and fear of instability with one miniplate, especially when applied to most types of angle fractures.
The first thing we noted immediately after surgery was the presence of a radiographic gap in the inferior border in some cases in both groups, but these had no effect on occlusion and esthetic outcomes. Angle fractures generate the highest frequency of complications relative to other mandibular fractures, ranging from 0 to 32% in various studies [
8,
25,
26]. Biomechanical forces that occur during mastication in the angle region contribute to a greater incidence of complications. Several studies suggest that two miniplates should be used, one at the base and another at the superior border [
13,
19,
20]. All biomechanical tests in which a second miniplate has been fixed to the mandibular inferior border revealed less mobile fracture ends [
27]. Nevertheless, Ellis and Walker showed the increased rate of possible infections with this technique [
28].
Thus, the rate of infection is not only determined by the mobility of the fracture ends, but also, to a considerable degree, by the surgical trauma and the extent of bone exposure required. From this point of view, osteosynthesis with a single miniplate (Champy technique) minimizes intraoperative trauma [
29].
The complication incidence is one of the criteria for evaluation of the treatment efficacy. In our study, complications occurred in 5 (12.5%) persons including malocclusion (three cases, 7.5%), nerve injury due to surgical manipulation (one case, 2.5%), wound dehiscence (one case, 2.5%), and local infection (one case, 2.5%). In cases of mandibular angle fractures, the incidence of complications varies: Lamphier et al stated that healing complications occur in 13.3% of cases; according to Atanasov, the percentage is 25.2%, but others have reported different percentages [
29,
30]. Complications evaluated in Fox and Kellmans study included infection (2.9%), dehiscence (5.9%), and inferior alveolar nerve injury (4.4%) [
2].
Such huge differences between the findings presented by various authors depend on surgeon skill, preoperative and postoperative care, surgical techniques, surgical traumas, and so on. It is noteworthy to mention that the population of our study was relatively uneducated and had poor oral hygiene, and that the most common cause of fractures were motor bike accident. On the other hand, the fracture sites often involved open oral wounds and time of trauma to treatment was relatively long, so all of these expressed factors may increase the rate of complications. All our patients were treated with antibiotic and chlorhexidine 0.2% rinses from the time of presentation to approximately 1 week after surgery.
Several authors have suggested that extraction of a tooth in the fracture line may lead to postoperative infection [
28,
30]. In this study, we extracted all third molars in the fracture line that had fractured roots, extra mobility, or signs of infection risk.
We compared complications between two treatment groups and the difference was not statistically significant (p > 0.05). The management approach of our study, including strict oral hygiene care preoperatively and postoperatively, conservative fracture area exposure, active follow-up, and removal of third molars with infection risk, may have contributed to the low infection rates.
Regarding our study, the use of a single miniplate in the external oblique ridge is a functionally stable treatment and is as effective alone as with MMF, although in the first group (without rigid MMF) patients had to be more careful (i.e., softer diet, light elastic therapy, more follow-up sessions, etc.) than the second group (with rigid MMF).
Because of many disadvantages, we prefer not to use rigid MMF. Lack of use MMF has the advantages include a quick return to functionality in patients and higher patient satisfaction, generally. In addition, the correction of the complications encountered in our study dictated no major procedures or general anesthesia, and all were retreated ambulatory by local anesthesia and elastic therapy, which shows the low severity of our complications. The presence of one miniplate creating semirigid fixation in the fracture line gives the surgeon the chance of correcting disturbed occlusion by elastic therapy. Gear et al in their article reviewed the past articles and mentioned that the “level of experience appears to correlate with use of Champy technique [
10]. Surgeons who treat more than 10 mandible fractures a year clearly favor this technique.” This is ironic because most surgeons find the Champy technique faster and easier in comparison to other techniques.
Finally we advocate treatment with a single miniplate without IMF for all types of angle fractures (including displaced and unfavorable fractures) except comminuted and long oblique fractures, which based on our previous experience we did not encounter in our study.