Abstract
Extensive defects of the scalp and forehead associated with calvarial bone resections demand complex reconstructions. Free flaps offer vascularized tissue of excellent quality and quantity. We report six patients with extensive scalp and forehead defects associated with calvarial bone resections reconstructed with free flaps. Five patients also required a cranioplasty. The flaps used were two anterolateral thigh flaps, one vastus lateralis flap, one myocutaneous latissimus dorsi flap, one latissimus dorsi flap, and one radial forearm flap. All flaps survived with no partial necrosis. There were no donor site complications. One patient presented an exposure of the alloplastic material used for cranioplasty. We strongly recommend the use of free flaps for this kind of reconstruction.
The reconstruction of extensive defects of the scalp and forehead associated with calvarial bone resections remains a challenge for the reconstructive surgeon. This kind of defect may be secondary to trauma, oncological resections, infections, or radiotherapy. They can be superficial with only outer cortical bone involvement or full thickness with dural or cerebral exposure [1,2,3].
The success of this type of reconstruction depends on the correct preoperative evaluation of the patient and the potential defect, considering location, size, and depth [3,4,5].
The type of reconstruction must be tailored to the extension and depth of the defect. Superficial defects smaller than 3 cm wide can be easily resolved with direct closure or local flaps [4,5,6]; however, local repair may be conditioned by adverse factors such as radiotherapy or scars derived from previous surgeries or infections, making free tissue transplantation a more reliable option. Free flaps are considered the first choice for larger and more complex defects of the region [7,8].
The flaps most commonly used for scalp and forehead reconstruction are the anterolateral thigh (ALT) flap, the latissimus dorsi muscle flap, the myocutaneous rectus abdominis flap, and the radial forearm flap. This is due to the length of their vascular pedicles and the amount of soft tissue they provide [9].
Materials and Methods
Between June 2007 and November 2010, six patients with extensive scalp and forehead defects associated with calvarial bone resections requiring free flap reconstruction were operated at the Hospital Italiano de Buenos Aires, Argentina. Data were collected regarding epidemiological details, cause and location of the defect, type of flap used for the repair, recipient vessels for anastomosis, type of cranioplasty, and postoperative complications.
Results
Patient and Defect Details
The mean age of the patients was 54 years (range 31 to 70), and mean follow-up was 30.3 months (range 12 to 60). Five patients were male and one female. The defects were due to oncological resections in three cases, osteoradionecrosis in one, skin necrosis with secondary alloplastic material exposure in one, and scalp and calvarial necrosis derived from electrocution in another (Table 1).

Table 1.
Characteristics of Patients.
The mean size of the soft tissue defects was 101 cm2 (range 4 to 225), and all the patients had an associated full-thickness craniectomy. The mean size of bony defects was 35 cm2 (range 9 to 100). Only one patient had an associated 4 × 4-cm dura resection (Table 1).
Reconstructive Procedures
The bony defects were reconstructed primarily in three cases, secondarily in two, and one defect was not repaired because it was less than 3 cm in diameter. In three cases, a titanium mesh was used for the cranioplasty and a prefabricated polyetheretherketone (PEEK) implant in two.
For the soft tissue repair, we used two ALT flaps, one vastus lateralis flap with a 2 × 2-cm perforator-based skin paddle, one myocutaneous latissimus dorsi flap, one skin grafted latissimus dorsi flap, and one radial forearm flap. The temporal vessels were used as recipients in four cases, the vessels of a previous radial forearm flap in one case, and saphenous vein grafts for both vein and artery were required to reach the thyroid artery and the external jugular vein in one case. One patient required a synthetic dural repair.
Complications
We only had one mayor complication in an obese patient (body mass index 44) who suffered a pulmonary embolism on postoperative day 20 that was successfully treated by endovascular aspiration. All flaps survived with no partial necrosis. There were no donor site complications. One of the PEEK implants had to be removed due to extrusion 3 months after surgery.
Discussion
Many options have been proposed for the treatment of large soft tissue defects of the scalp. Split-thickness skin grafts are a choice when there is no osseous compromise and the periosteum is healthy. Another option are local flaps, which can be simple rotation flaps with skin grafting of the donor site or complex flaps like the four-flap technique described by Orticochea [10]. This kind of flap offers the advantage of easy performance and the replacement of hair-bearing defects with hair-bearing scalp. On the other hand, they usually leave sections of scalp to be grafted and they have a limited vascularity at the flap tips when sutured under tension, which makes them less reliable.
Tissue expansion is a very good alternative when treating a benign lesion or in a noninfected secondary setting that gives you the time to complete the expansion process. This kind of reconstruction also has its drawbacks like implant exposure, flap necrosis, or alopecia that can be as high as 39% in some series [11,12].
Distant musculocutaneous flaps like the vertical trapezius, pectoralis mayor, or latissimus dorsi flaps were used when microvascular surgery was not available [13,14]. These flaps present mayor disadvantages like random vascularization at the flap tip and important donor site morbidity; they are usually bulky and none of them can reach the vertex.
Free flaps offer the best solution for extremely large soft tissue defects of the scalp because they have a robust vascularization, there is a great variety of flaps to choose from, they can be tailored to fit the defect, and they can be positioned freely. Furthermore, the high survival rate makes them extremely reliable. We also recommend this kind of flaps in special situations such as previous radiotherapy or when using alloplastic materials for cranioplasty, multiple previous surgeries, or infections.
We believe there is no ideal flap for any of these situations, and we have to choose the most suitable one for each particular case, also taking into account the association with other reconstructive options like tissues expanders or local flaps [15,16,17,18,19,20,21,22].
The key features when choosing a flap for this kind of problem are: (1) the size and thickness, so it can replace the full extent of the resection without being too bulky, resembling more precisely the shape of the skull; (2) the length of the vascular pedicle, taking into account that the temporal vessels may be of poor quality or have been injured by previous procedures; (3) the need for muscle to seal a dura defect or deal with a contaminated environment.
In our series, we used five types of free flaps. In case 1, we used an ALT because we were going to replace a complete aesthetic subunit of the forehead. For this purpose, we needed a thin fasciocutaneous flap. In our patient population, with the exception of obese patients, ALT flaps are usually thin in male subjects and do not need any debulking procedure; this is not the situation when treating female subjects, who usually have thicker flaps. The ALT flap provides a long pedicle that can reach the mandibular border if needed and can be designed to have an independent muscle cuff to seal any dural defect.
In case 3, we chose a free latissimus dorsi flap because the patient was obese and any flap with a fasciocutaneous component would have been too bulky. We skin-grafted this flap 1 week after the initial surgery when we were certain about the vascular success. During this time, we protected the flap with a nonadherent dressing.
In case 2, the patient suffered bone necrosis due to electrocution and was secondarily infected with Pseudomona aeruginosa, so he was a candidate for multiple reexplorations and debridement procedures. We chose to use a musculocutaneous latissimus dorsi free flap instead of a skin-grafted muscle flap that would have been thinner and more aesthetic because in our experience resuturing several times the borders of skin-grafted muscle flaps can lead to dehiscence.
In case 6, we needed a thin flap to replace forehead skin in a discretely obese subject (body mass index 27) who had a possible previous injury of the temporal vessels, so we used the only thin flap with a long pedicle that this patient had, a radial forearm flap. This flap has the disadvantage of donor site morbidity.
One patient received a vastus lateralis flap, because we needed to provide a great amount of soft tissue to fill an anterior skull base defect and very little skin. We chose this flap because both latissimus dorsi muscles were compromised by previous surgeries and hoped to use as recipient vessels the distal end of the pedicle of a previous ALT flap transferred 4 weeks earlier to reconstruct the orbit. This was not possible, and being that this flap has a short pedicle and the patient had no temporal vessels, we used vein grafts to reach the neck.
In Table 2 we compare the different types of flaps used.

Table 2.
Comparison of Flaps Used.
The need to perform the cranioplasty during the same procedure is another controversial point. We recommend doing it simultaneously with the soft tissue repair when we are completely certain there is no contamination. If we have any doubt about this, we should defer it for a secondary setting [4]. The material used to perform the cranioplasty should be chosen according to the defect. Very small defects can even be left unrepaired [23].
For the cranioplasty, we chose synthetic materials in all cases because the size of the defects would have required a very large amount of bone grafts, and we consider the donor site morbidity unacceptable. We did not use methyl methacrylate because in our experience, and as other authors have also pointed out, it is prone to late infections [4]. Titanium meshes were used if we had no dead space between mesh and the dura and only in the primary setting. PEEK implants can only be used in a secondary setting because they have to be computer designed to match the defect. Of all the patients who received the cranioplasty, we had only one exposure, a PEEK implant placed 6 months after the initial surgery and secondary to wound dehiscence. We have limited experience with this kind of implant and cannot be objective about long-term results.
Case Reports
Case 1
A 70-year-old man had previous cranial base and nasal dorsum resection due to squamous cell carcinoma reconstructed with bone grafts and an ALT flap. Three years postoperatively, he presented a new skin tumor on the forehead with calvarial bone compromise detected after Mohs resection. The right forehead subunit was completely resected and the corresponding craniectomy performed. The dura had to be replaced with a purified polyester urethane microporous fleece and biologic glue due to adhesions from the previous cranial base surgery. The defect was repaired with a titanium mesh and an ALT flap transferred to the temporal vessels (Figure 1, Figure 2 and Figure 3).
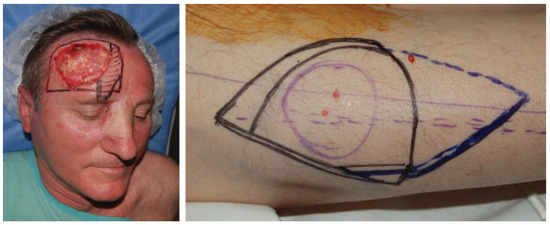
Figure 1.
Case 1: flap design.
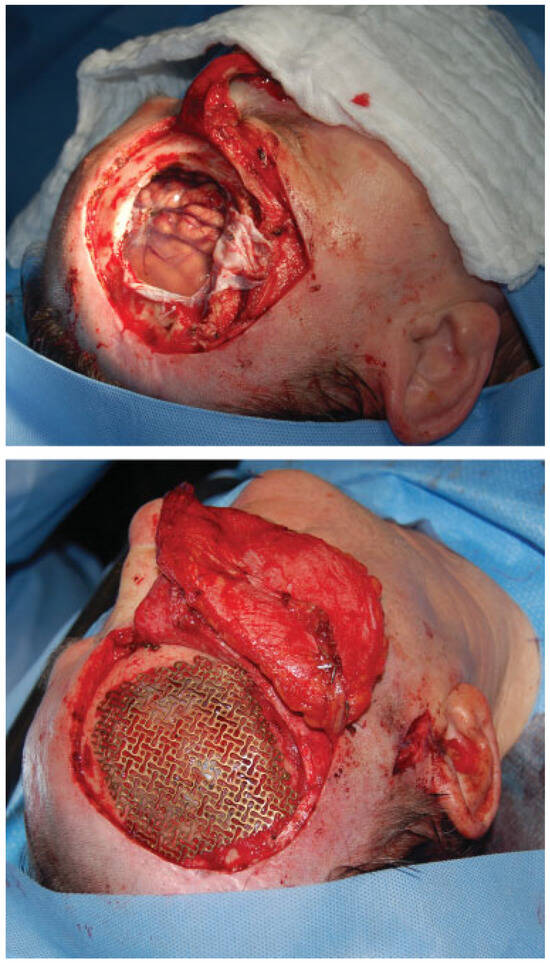
Figure 2.
Case 1: surgical defect and cranioplasty.

Figure 3.
Case 1: postoperative result.
Case 2
A 31-year-old patient suffered a high-voltage electrocution with occipital scalp loss and secondary osteomyelitis of the cranial bone. Multiple debridements were performed and the final defect was reconstructed with a latissimus dorsi myocutaneous flap anastomosed to the temporal vessels. The cranioplasty with a peek implant was performed 1 year later once the infectious process was under control (Figure 4, Figure 5 and Figure 6).

Figure 4.
Case 2: preoperative defect and craniectomy.

Figure 5.
Case 2: latissimus dorsi free flap insetting and vascular anastomosis to temporal vessels.
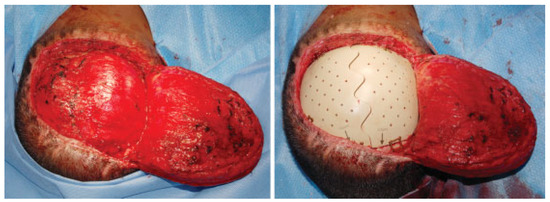
Figure 6.
Case 2: cranioplasty with polyetheretherketone implant in a second surgery.
Case 3
A 41-year-old severely obese woman had pleomorphic sarcoma of the occipital scalp. A complete resection was performed including a small craniectomy. The defect was reconstructed with a latissimus dorsi flap transferred to the temporal vessels that was skin-grafted 2 weeks postoperatively. The craniectomy defect was not repaired (Figure 7 and Figure 8).

Figure 7.
Case 3: scalp sarcoma before and after resection.

Figure 8.
Case 3: latissimus dorsi free flap insetting and postoperative defect after skin grafting.
Case 4
A 64-year-old man had multiple surgeries due to a dermatofibrosarcoma protuberans of the scalp and a previous radial forearm free flap reconstruction. Complete resection was performed including an extensive craniectomy. The resulting defect was reconstructed with an ALT flap, and a secondary cranioplasty was performed 3 months later with a peek implant. In this case, the implant had to be extracted due to infection 3 months after placement (Figure 9, Figure 10 and Figure 11).

Figure 9.
Case 4: scalp dermatofibrosarcoma before and after resection.

Figure 10.
Case 4: defect reconstruction with anterolateral thigh flap.
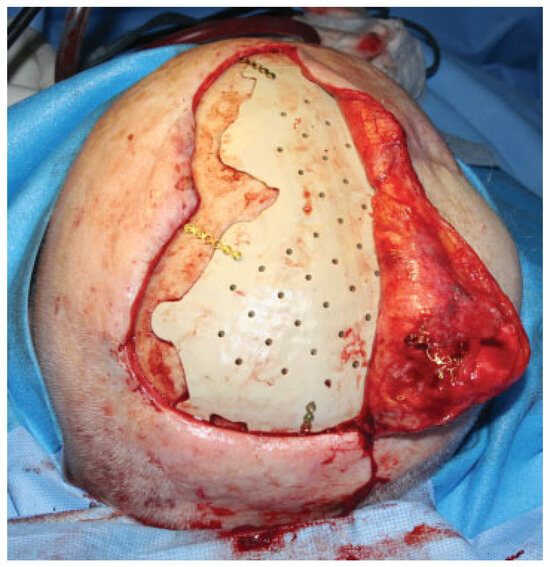
Figure 11.
Case 4: secondary cranioplasty with polyetheretherketone implant.
Conclusions
Scalp reconstruction is still a demanding procedure due to the special characteristics of the tissue to be replaced, the few local flap options, and the lack of adequate recipient vessels except for the temporal artery and vein. For the treatment of complex and extensive scalp defects including calvarial resections, free flaps are our first choice. We believe the cranioplasty should only be performed under optimal conditions and not necessarily at the same time of the soft tissue repair.
References
- Lutz, B.S.; Wei, F.C.; Chen, H.C.; Lin, C.H.; Wei, C.Y. Reconstruction of scalp defects with free flaps in 30 cases. Br J Plast Surg 1998, 51, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.; Bickel, K.; Levin, S. Microsurgical reconstruction of extensive scalp defects. J Reconstr Microsurg 1999, 15, 255–262; discussion 263–264. [Google Scholar] [CrossRef] [PubMed]
- TerKonda, R.P.; Sykes, J.M. Concepts in scalp and forehead reconstruction. Otolaryngol Clin N Am 1997, 30, 519–539. [Google Scholar] [CrossRef]
- Afifi, A.; Djohan, R.S.; Hammert, W.; Papay, F.A.; Barnett, A.E.; Zins, J.E. Lessons learned reconstructing complex scalp defects using free flaps and a cranioplasty in one stage. J Craniofac Surg 2010, 21, 1205–1209. [Google Scholar] [CrossRef]
- van Driel, A.A.; Mureau, M.A.; Goldstein, D.P.; et al. Aesthetic and oncologic outcome after microsurgical reconstruction of complex scalp and forehead defects after malignant tumor resection: An algorithm for treatment. Plast Reconstr Surg 2010, 126, 460–470. [Google Scholar] [CrossRef]
- Iblher, N.; Ziegler, M.C.; Penna, V.; Eisenhardt, S.U.; Stark, G.B.; Bannasch, H. An algorithm for oncologic scalp reconstruction. Plast Reconstr Surg 2010, 126, 450–459. [Google Scholar] [CrossRef]
- Komorowska-Timek, E.; Gabriel, A.; Bennett, D.C.; et al. Artificial dermis as an alternative for coverage of complex scalp defects following excision of malignant tumors. Plast Reconstr Surg 2005, 115, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.P.; Lai, C.H.; Chang, C.H.; Lin, C.L.; Lai, C.S.; Lin, S.D. Free flap options for reconstruction of complicated scalp and calvarial defects: Report of a series of cases and literature review. Microsurgery 2010, 30, 13–18. [Google Scholar] [CrossRef]
- Beasley, N.J.; Gilbert, R.W.; Gullane, P.J.; Brown, D.H.; Irish, J.C.; Neligan, P.C. Scalp and forehead reconstruction using free revascularized tissue transfer. Arch Facial Plast Surg 2004, 6, 16–20. [Google Scholar] [CrossRef]
- Orticochea, M. Four flap scalp reconstruction technique. Br J Plast Surg 1967, 20, 159–171. [Google Scholar] [CrossRef]
- Antonyshyn, O.; Gruss, J.S.; Mackinnon, S.E.; Zuker, R. Complications of soft tissue expansion. Br J Plast Surg 1988, 41, 239–250. [Google Scholar] [PubMed]
- Newman, M.I.; Hanasono, M.M.; Disa, J.J.; Cordeiro, P.G.; Mehrara, B.J. Scalp reconstruction: A 15-year experience. Ann Plast Surg 2004, 52, 501–506; discussion 506. [Google Scholar] [PubMed]
- Liu, R.; Gullane, P.; Brown, D.; Irish, J. Pectoralis major myocutaneous pedicled flap in head and neck reconstruction: Retrospective review of indications and results in 244 consecutive cases at the Toronto General Hospital. J Otolaryngol 2001, 30, 34–40. [Google Scholar] [CrossRef]
- Virós Porcuna, D.; León Vintró, X.; López Vilas, M.; Pujol Olmo, A.; Masià Ayala, J.; Quer Agustí, M. [Pectoralis major flaps. Evolution of their use in the age of microvascularized flaps]. Acta Otorrinolaringol Esp 2008, 59, 263–268. [Google Scholar] [CrossRef]
- Hoffman, J.F. Management of scalp defects. Otolaryngol Clin N Am 2001, 34, 571–582. [Google Scholar]
- Nordström, R.E.; Devine, J.W. Scalp stretching with a tissue expander for closure of scalp defects. Plast Reconstr Surg 1985, 75, 578–581. [Google Scholar]
- Wieslander, J.B. Repeated tissue expansion in reconstruction of a huge combined scalp-forehead avulsion injury. Ann Plast Surg 1988, 20, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, J.L. Use of pericranial flap in scalp wounds with exposed bone. Plast Reconstr Surg 1983, 72, 786–790. [Google Scholar]
- Terranova, W. The use of periosteal flaps in scalp and forehead reconstruction. Ann Plast Surg 1990, 25, 450–456. [Google Scholar] [CrossRef]
- Guerrissi, J.O. Reconstruction of large defects in the scalp with fasciocutaneous flaps. Scand J Plast Reconstr Surg Hand Surg 1999, 33, 217–224. [Google Scholar]
- Lesavoy, M.A.; Dubrow, T.J.; Schwartz, R.J.; Wackym, P.A.; Eisenhauer, D.M.; McGuire, M. Management of large scalp defects with local pedicle flaps. Plast Reconstr Surg 1993, 91, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Orticochea, M. New three-flap reconstruction technique. Br J Plast Surg 1971, 24, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Shonka, D.C., Jr.; Potash, A.E.; Jameson, M.J.; Funk, G.F. Successful reconstruction of scalp and skull defects: Lessons learned from a large series. Laryngoscope 2011, 121, 2305–2312. [Google Scholar] [CrossRef] [PubMed]
© 2012 by the author. The Author(s) 2012.