Abstract
Major causes of facial combat injuries include blasts, high-velocity/high-energy missiles, and low-velocity missiles. High-velocity bullets fired from assault rifles encompass special ballistic properties, creating a transient cavitation space with a small entrance wound and a much larger exit wound. There is no dispute regarding the fact that primary emergency treatment of ballistic injuries to the face commences in accordance with the current advanced trauma life support (ATLS) recommendations; the main areas in which disputes do exist concern the question of the timing, sequence, and modes of surgical treatment. The aim of the present study is to present the treatment outcome of high-velocity/high-energy gunshot injuries to the face, using a protocol based on the experience of a single level I trauma center. A group of 23 injured combat soldiers who sustained bullet and shrapnel injuries to the maxillofacial region during a 3-week regional military conflict were evaluated in this study. Nine patients met the inclusion criteria (high-velocity/high-energy injuries) and were included in the study. According to our protocol, upon arrival patients underwent endotracheal intubation and were hemodynamically stabilized in the shock-trauma unit and underwent total-body computed tomography with 3-D reconstruction of the head and neck and computed tomography angiography. All patients underwent maxillofacial surgery upon the day of arrival according to the protocol we present. In view of our treatment outcomes, results, and low complication rates, we conclude that strict adherence to a well-founded and structured treatment protocol based on clinical experience is mandatory in providing efficient, appropriate, and successful treatment to a relatively large group of patients who sustain various degrees of maxillofacial injuries during a short period of time.
Major causes of facial combat injuries include blasts, high-velocity/high-energy missiles, and low-velocity missiles. Blasts caused by high explosives often contain metal fragments, such as Claymore charges, which contain hundreds of metal pellets. Victims who are close to the center of the explosion barely survive such fatal injuries.
The severity of a ballistic injury is directly related to the shape and size of the projectile and to its contended kinetic energy at impact, which depends on the distance it traveled [1,2]. High-velocity bullets fired from assault rifles encompass special ballistic properties, including high-impact kinetic energy of around 3250 ft/s, which creates a transient cavitation space with a small entrance wound and a much larger exit wound. This type of perforating injury is usually avulsive and causes enormous damage to soft and hard tissues, with severe comminution of the facial skeleton. Low-velocity missile injuries are quite different, due to the fact that the projectiles possesses only about one-third of the kinetic energy compared with high-velocity projectiles. Such missiles generally cause penetrating injuries, which inflict multiple fractures and skin lacerations and rarely involve tissue avulsion [3,4,5].
The hallmark of high-velocity ballistic injuries to the face is highly comminuted fractures of the facial skeleton and avulsion injuries of facial as well as intraoral soft tissue along the main trajectory of the offending missile. Concomitant injuries often include secondary distant fractures, caused by the propagation of the shock wave. Other secondary injuries may include avascular necrosis caused by damage to the intimal lining of blood vessels resulting in intimal flaps and tears, often distant from the main trajectory [6].
Other factors that influence the clinical presentation are the bullet caliber or projectile size and shape, the traveling distance, the initial muzzle velocity, and the ballistic properties of the missile, and of course the anatomic nature of the injury site. Injury sites may vary anatomically and may consist of strong bony structures (such as the mandible), weak bony structures (the midface, for example), and soft tissue structures such as the neck [7].
There is no dispute regarding the fact that primary emergency treatment of ballistic injuries to the face commence in accordance with the current advanced trauma life support (ATLS) recommendations, with airway management and control of bleeding [8]. The importance of early evacuation of the injured patient to a level I trauma center specializing and experienced in multidisciplinary treatment of ballistic trauma patients as soon as the patient's condition stabilizes is also widely recognized. The main areas in which disputes do exist concern the question of the timing, sequence, and modes of surgical treatment.
When the patient is hemodynamically stabilized, full multidisciplinary evaluation of the patient's condition and appropriate imaging leading toward a comprehensive treatment plan may commence [9]. The patient is then transferred to the operating theater for a prioritized surgical intervention sequence. Surgical treatment commences with lifesaving and organ-saving procedures such as hemostasis, craniotomy, vascular surgery, reduction of open fractures, and so on. Maxillofacial surgery (other than that involving airway maintenance, hemostasis, and management of retrobulbar hematoma) should be performed immediately following emergency surgical interventions.
If second-stage reconstruction of the midfacial skeleton or soft tissue is necessary, it is usually performed during the first week. Distant hard tissue flaps (split-thickness calvarial bone graft, for example) and microvascular soft tissue combined tissue flaps (radial forearm flap, fibula flap, etc.) may be used, as the patient's overall condition has improved and he or she will therefore successfully and safely tolerate extensive surgical interventions with minimal risk [10,11]. Secondary reconstruction of the mandible is generally executed later during the first month, to allow proper healing of the soft tissue bed surrounding the mandible prior to free microvascular bone grafting to replace lost bone, or in case of late complications such as osteomyelitis [12,13].
In summary, over the past 25 years of vast experience in treatment of ballistic injuries to the face, we have developed a structured and time-proven treatment sequence that enables us to provide efficient and proper treatment to a relatively large number of ballistic injury patients in a relatively short period of time. We present our experience-based protocol used in treatment of high-velocity and high-energy ballistic injuries to the face at our medical center in an eight-step simplified manner and describe the implementation of the protocol on combat soldiers injured during a recent military conflict. An example of the protocol implementation is presented in Figure 1.
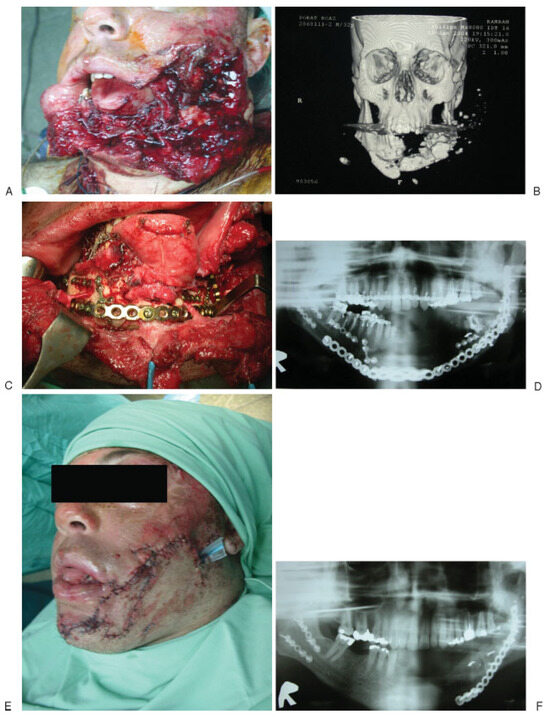

Figure 1.
(A) Photograph of a soldier with severe shrapnel injury from an antitank missile. (B) 3-D reconstruction of the computed tomography scan for injury evaluation and 3-D surgical planning. (C) Photograph of the reconstruction performed in the primary surgical care; notice preservation of bilateral mental nerves and reconstruction using both monocortical semirigid fixation for fracture simplification and bicortical rigid fixation with load-bearing reconstruction plate. (D) Panoramic postoperative X-ray. (E) Photograph of the patient at the end of the primary surgery; notice that no skin graft or free flap was needed for primary closure. (F) Panoramic X-ray at the end of the iliac crest bone graft second surgery. (G) Functional rehabilitation using dental implants. (H) Photograph of the final result 1 year after injury.
Patients and Methods
Patients
Twenty-three combat soldiers who sustained maxillofacial ballistic injuries during a recent military conflict were admitted to our medical center between July 20 and August 14, 2006. We included only patients who sustained high-velocity/high-energy injuries. One patient suffered from facial fractures following a helicopter collision and was excluded from the study. The remaining 22 patients had sustained maxillofacial ballistic injuries, 13 of which were superficial, soft tissue, low-energy shrapnel wounds, which were also excluded from the study. Nine patients (age range 21 to 32, mean ¼ 25.9 years) suffered from severe high-energy/high-velocity ballistic maxillofacial injuries: three sustained high-velocity gunshot injuries inflicted by assault rifle projectiles and the remaining six were injured by high-energy antitank missile shrapnel and Claymore charges. The complete medical records are presented (Table 1 and Table 2).

Table 1.
Diagnostic Details of Patients with High-Velocity/High-Energy Maxillofacial Ballistic Injury.

Table 2.
Treatment Details of Patients with High-Velocity/High-Energy Maxillofacial Ballistic Injury.
Treatment Protocol
The following is our experience-based protocol used in treatment of high-velocity and high-energy ballistic injuries to the maxillofacial region. A practical flowchart of the protocol is also shown in Figure 2.
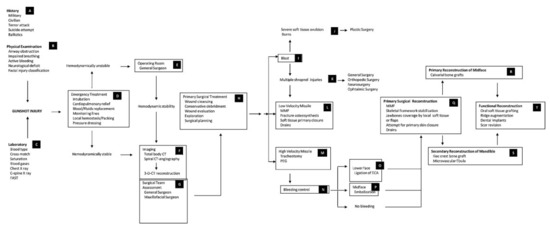
Figure 2.
Maxillofacial ballistic injuries flowchart of treatment protocol. CT, computed tomography; FAST, focused assessment with sonography for trauma; MMF, maxillo-mandibular fixation; PEG, percutaneous endoscopic gastrostomy; ECA, external carotid artery.
- Primary lifesaving and organ preservation procedures: intubation upon arrival, cervical spine radiography, direct pressure and packing for hemostasis, and hemodynamic stabilization in accordance with ATLS protocols.
- Imaging: multiplanar computed tomography (CT), 3-D CT, CT angiography in all maxillofacial ballistic injury patients, and superselective angiography in midface injuries.
- Interdisciplinary patient evaluation, registration and classification of injuries, establishment of a list of diagnoses, and formulation of a multidisciplinary prioritized treatment plan.
- Tracheotomy and percutaneous gastrostomy in the operating theater in highly avulsive and complex injuries.
- Restoration and stabilization of occlusal relations via maxillomandibular fixation. Facial bony framework stabilization and rigid fixation using load-bearing bicortical plates (2.4 mm) in the mandible and monocortical plates (2.0 mm) in the remaining facial skeleton.
- Tissue preservation: meticulous primary closure of the intraoral and extraoral soft tissue to provide full coverage of the comminuted fractures.
- Immediate bone grafting of the midface, nasal orbital, and zygomatic structures using calvarial free bone grafts, if no major head trauma is present to contraindicate calvarial bone grafting, if so anterior iliac crest bone grafting is harvested.
- Secondary reconstruction of avulsive mandibular injuries using iliac crest bone grafts during the first weeks following trauma. Implementation of vascularized free grafts only in cases of massive tissue avulsion or in cases of primary reconstruction failures.
Results
In total, 22 patients with ballistic facial injury had undergone a total of 33 surgical procedures, averaging 1.5 procedures per patient. The 13 patients with soft tissue shrapnel injury demonstrated remarkable injury patterns, which consisted of shrapnel wounds in exposed body areas, namely, the face and the upper and lower extremities, due to the fact that all other body surfaces were protected by helmets and ceramic combat jackets used by elite combat units.
Nine patients met the inclusion criteria and formed our study group. Eight patients were transported to the hospital by military helicopters and one was transported by an ambulance (this patient was the only one who had not undergone endotracheal intubation upon arrival at the shock/trauma unit, due to a Glasgow Coma Scale (GCS) of 15, which did not necessitate tracheotomy or endotracheal intubation). The protocol is presented as a flowchart in Figure 2 and an example of the implementation of the protocol is presented in Figure 1A–H. All of the patients underwentinitial hemodynamic stabilization, comprehensive assessment, and appropriate imaging. All patients had undergone total body CT except for one, who required only a head CT. CT angiography was performed on all three assault rifle injury patients and on four of the six shrapnel injury patients in which severe vascular injuries were suspected. Full clinical evaluation and radiographic imaging were followed by multidisciplinary treatment plan formation for each patient.
All injured combat soldiers underwent primary maxillofacial surgery upon the day of arrival, and five of them were simultaneously or sequentially treated by a multidisciplinary surgical team consisting of maxillofacial, general, neuro-, vascular, orthopedic, and hand surgeons, as required by each specific injury pattern.
A tracheotomy was initially performed during the primary surgical interventions in all three high-velocity sniper/assault rifle projectile injuries and in five high-energy shrapnel injuries. The main indications for the procedure were complex facial injuries involving hard and soft tissue and the anticipated requirement for additional surgical interventions in the foreseeable future.
Two of the nine patients included in the study sustained severe vascular injuries and underwent angiography and superselective embolization early upon arrival. None of the injuries in the study group required ligation of the external carotid artery. Bleeding in zone II was treated primarily by direct pressure and packing in four patients (one bullet injury and three shrapnel injuries), and hemostasis was later accomplished during surgery. One patient with shrapnel injury sustained concomitant vascular injuries in the lower extremities and was simultaneously treated surgically by a team of orthopedic and vascular surgeons.
Open reduction and internal fixation (ORIF) of all maxillofacial fractures was performed in strict adherence to AO/ASIF principles using 2.4-mm locking load-bearing reconstruction plates and bicortical screws in cases involving severe comminution and/or avulsion of mandibular bone; 2.0-/1.5-mm monocortical plates and screws were used for simplification of complex mandibular fractures and for treatment of simple fractures of the mandible. Such plates and screws were also utilized in ORIF of fractured maxillae, malar bones, and orbits. Bone grafting was performed on two patients with bullet injury and on two patients with shrapnel injury.
One patient sustained an antitank missile shrapnel injury, which penetrated intracranially and underwent craniectomy, lobectomy, and ORIF of zygoma, but he unfortunately remains in a comatose state.
The immediate complication rate in the high-velocity/high-energy group of wounded soldiers was 22% (2/9) and included one case of local wound infection and one case of flap dehiscence. Late complications were encountered in only one patient (11%, 1/9), who had late enophthalmos. The patient with immediate wound infection complication was treated by drainage and intravenous antibiotic treatment, which led to full resolution. One other patient, who had a sniper rifle injury, suffered from flap dehiscence following bone graft reconstruction of the anterior mandible and required late reconstruction of the anterior mandible with a microvascular fibula free flap during the secondary reconstruction stage according to our protocol. Three patients (one with sniper rifle injury and two with shrapnel injury) underwent ORIF of orbital fractures. Healing was uneventful except for one patient with shrapnel injury who experienced late enophthalmos and required secondary bone graft reconstruction of the orbital floor. No in-hospital mortalities were encountered. The range of hospitalization time for the remaining eight patients in the primary treatment phase (immediately following the injury) was 4 to 52 days, with a mean of 13.25 days.
Discussion
In earlier times, surgical treatment of gunshot wounds to the face was executed in two distinct stages: the primary phase, which was performed immediately after the injury and consisted mainly of debridement, hemostasis, and soft tissue closure, and open reduction of fractures, bone grafting, and complementary soft tissue repair, which were deferred to a later stage [8,12]. This approach resulted in significant scaring and contracture of the facial soft tissue, rendering proper secondary correction nearly impossible. Patients who were treated in this manner often suffered from severe esthetic and functional deficits. To minimize such unsolicited results, we encourage comprehensive surgical treatment of facial gunshot injuries as early as possible, based on our experience as well as others [9,14,15,16,17]. This approach is also advocated by Denny et al., who implement an aggressive multispecialty team approach at the Medical College of Wisconsin [9]. Their approach consists of plastic surgical techniques, ORIF and miniplate reconstruction of facial fractures, acute bone grafting, and soft tissue reconstruction at the earliest possible time when feasible; they show superior esthetic and functional results that are accomplished with a substantially lower number of hospitalizations and surgical interventions as well as shorter hospitalization periods [9]. Early aggressive comprehensive surgical intervention for hard and soft tissue reconstruction including free microvascular free flaps is also advocated by others [6]; on the other hand, our experience, as well as others' [12], led us to defer vascularized tissue reconstruction to a later stage.
The presented experience-based protocol for treatment of ballistic high-velocity injuries to the maxillofacial region consists of immediate primary lifesaving procedures, implementing a full array of modern imaging techniques, along with comprehensive interdisciplinary evaluation of the patient and formulation of a prioritized treatment plan, emergency life- and limb-saving surgical procedures, maxillomandibular fixation, primary stabilization and rigid fixation of the facial bony framework, primary closure of soft tissue, primary bone grafting of the midface; secondary bone grafting and reconstruction of mandible occur during the second stage of reconstruction, with free microvascular bone grafting when indicated. The protocol was formulated and progressively modified over the past 25 years of vast experience in treatment of ballistic injuries to the face at our department (Figure 2), which resides in a level I trauma center in Northern Israel. The protocol was successfully implemented during the Second Lebanon War in July 2006 on 23 wounded soldiers who sustained ballistic injuries to the face and were evacuated to and treated at our medical center during a brief 3-week period.
The relatively low rate of severe late residual complications (11%, one of nine patients) is probably related to the proximity of the trauma center to the battleground, which facilitated rapid evacuation to a level I trauma center, thus enabling efficient and structured multidisciplinary evaluation of the patients in the shock/trauma unit and surgical intervention on the day of the injury. We believe that all patients with gunshot injury should be evacuated to such a level I trauma center at the earliest possible time. Whenever possible, such an approach should be implemented, as many authors claim [18,19].
Only one patient suffered from acute infection, and initial treatment was deferred due to a skull base fracture complicated by cerebrospinal fluid leak. This example further emphasizes the importance of early surgical intervention and wound closure.
In accordance with others [20,21], we emphasize that head CT is mandatory in all patients with facial gunshot injury to rule out occult intracranial pathologic processes, which may present even in awake patients. In some cases, such occult injuries may present only at a later stage, thus increasing the risk of consequent morbidity or even mortality. Computerized angiotomography is of utmost importance in precise imaging of the location and extent of vascular injuries, as well as the 3-D structure of the bony injuries. It was therefore performed in seven of the nine patients in our study in whom severe vascular injuries were suspected, as advocated in previous studies [8,21,22]. It is our experience that in most cases of high-velocity gunshot injuries, soft tissue injuries demonstrate splaying of the facial soft tissue rather than true avulsion. In such cases, a significant and even major component of the soft tissue injury may be treated with primary closure, and free vascularized soft tissue grafts are seldom required at the acute phase. When compared with free soft tissue grafting, primary closure is usually performed at an earlier time and therefore carries the aforementioned benefits: primary closure is simpler to perform, is better tolerated by patients, and mandates relatively shorter hospitalization periods. External fixation was widely used in earlier times in treatment of extensive and/or comminuted facial fractures. In modern times, we rarely utilize true external fixation methods. Rather, patients with gunshot wounds suffering from extensive and/or comminuted facial fractures are treated nowadays using locking 2.4-mm reconstruction plates, functioning as internal/external fixation load-bearing plates, thus exploiting the beneficial properties of both methods.
In contrast to earlier times, nowadays all elite combat soldiers wear protective ceramic jackets and helmets, reducing the amount of penetrating injuries to the torso and superior part of the head and increasing the relative proportion of injuries to the exposed areas of the body [23]. Surveying the injuries sustained by the wounded soldiers admitted to our medical center during the recent conflict shows a relatively higher number of bullet and shrapnel injuries to exposed body parts—the face and the upper and lower extremities. These findings coincide with an analysis reviewing anatomic location of all penetrating injuries sustained by 164 soldiers killed during the Lebanon War [24]. The study showed that the face sustained the greatest density of penetrating injuries of all body parts. A study surveying penetrating injuries sustained by Israel Defense Forces (IDF) soldiers during the second Palestinian uprising showed similar results. The most commonly injured body parts were the head, face, and neck (54.2%) and extremities (50%), whereas protected body parts sustained fewer injuries—the trunk was injured in only 25% of all reviewed cases [25]. Kosashvili et al. analyzed the anatomic distribution of 149 penetrating injuries sustained by 26 IDF casualties in 2005 [26]. The face and neck areas sustained the highest density rate of both shrapnel and bullet injuries, and the prevalence of anterior injuries was significantly higher than posterior ones. Entry wound diameters, however, did not significantly differ between exposed and protected body parts. Our study, as well as the aforementioned reports, emphasizes the notion that the use of military personal armor systems have turned the face and neck into the most vulnerable areas of the body, in terms of bullet and shrapnel injuries.
In view of our treatment outcome, results, and low late complication rate, we conclude that strict adherence to a well-founded and structured treatment protocol based on clinical experience is mandatory in providing efficient, appropriate, and successful treatment to a relatively large group of patients who sustain various degrees of maxillofacial injuries during a short period of time.
References
- Gibbons, A.J.; Patton, D.W. Ballistic injuries of the face and mouth in war and civil conflict. Dent Update 2003, 30, 272–278. [Google Scholar] [PubMed]
- Yetiser, S.; Kahramanyol, M. High-velocity gunshot wounds to the head and neck: A review of wound ballistics. Mil Med 1998, 163, 346–351. [Google Scholar]
- Cohen, M.A.; Shakenovsky, B.N.; Smith, I. Low velocity hand-gun injuries of the maxillofacial region. J Maxillofac Surg 1986, 14, 26–33. [Google Scholar]
- Glapa, M.; Kourie, J.F.; Doll, D.; Degiannis, E. Early management of gunshot injuries to the face in civilian practice. World J Surg 2007, 31, 2104–2110. [Google Scholar] [PubMed]
- Williams, C.N.; Cohen, M.; Schultz, R.C. Immediate and long-term management of gunshot wounds to the lower face. Plast Reconstr Surg 1988, 82, 433–439. [Google Scholar] [PubMed]
- Tan, Y.H.; Zhou, S.X.; Liu, Y.Q.; Liu, B.L.; Li, Z.Y. Small-vessel pathology and anastomosis following maxillofacial firearm wounds: An experimental study. J Oral Maxillofac Surg 1991, 49, 348–352. [Google Scholar] [CrossRef]
- Rocca, A.; Paoli, J.R.; Leonetti, G.; Lenziani, E.; de Montera, A.M. [Gunshot injuries of the face. Clinical observations in 21 cases]. Ann Chir Plast Esthet 1998, 43, 125–131. [Google Scholar]
- Kihtir, T.; Ivatury, R.R.; Simon, R.J.; Nassoura, Z.; Leban, S. Early management of civilian gunshot wounds to the face. J Trauma 1993, 35, 569–575; discussion 575. [Google Scholar]
- Denny, A.D.; Sanger, J.R.; Matloub, H.S.; Yousif, N.J. Self-inflicted midline facial gunshot wounds: The case for a combined craniofacial and microvascular team approach. Ann Plast Surg 1992, 29, 564–570. [Google Scholar] [CrossRef]
- Antonyshyn, O.M.; Paletz, J.L.; Wilson, K.L. Reconstruction of composite facial defects: The combined application of multiple reconstructive modalities. Can J Surg 1993, 36, 441–452. [Google Scholar]
- Suominen, E.; Tukiainen, E. Close-range shotgun and rifle injuries to the face. Clin Plast Surg 2001, 28, 323–337. [Google Scholar] [CrossRef] [PubMed]
- Futran, N.D.; Farwell, D.G.; Smith, R.B.; Johnson, P.E.; Funk, G.F. Definitive management of severe facial trauma utilizing free tissue transfer. Otolaryngol Head Neck Surg 2005, 132, 75–85. [Google Scholar] [CrossRef]
- Ozkan, O.; Ozgentas, H.E.; Dikici, M.B. Simultaneous reconstruction of large maxillary and mandibular defects with a fibular osteocutaneous flap combined with an anterolateral thigh flap. J Reconstr Microsurg 2004, 20, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Gruss, J.S.; Antonyshyn, O.; Phillips, J.H. Early definitive bone and softtissue reconstruction of major gunshot wounds of the face. Plast Reconstr Surg 1991, 87, 436–450. [Google Scholar] [CrossRef] [PubMed]
- Motamedi, M.H. Primary management of maxillofacial hard and soft tissue gunshot and shrapnel injuries. J Oral Maxillofac Surg 2003, 61, 1390–1398. [Google Scholar]
- Siberchicot, F.; Pinsolle, J.; Majoufre, C.; Ballanger, A.; Gomez, D.; Caix, P. [Gunshot injuries of the face. Analysis of 165 cases and reevaluation of the primary treatment]. Ann Chir Plast Esthet 1998, 43, 132–140. [Google Scholar]
- Vayvada, H.; Menderes, A.; Yilmaz, M.; Mola, F.; Kzlkaya, A.; Atabey, A. Management of close-range, high-energy shotgun and rifle wounds to the face. J Craniofac Surg 2005, 16, 794–804. [Google Scholar] [CrossRef]
- Behnia, H.; Motamedi, M.H. Reconstruction and rehabilitation of short-range, high-velocity gunshot injury to the lower face: A case report. J Craniomaxillofac Surg 1997, 25, 220–227. [Google Scholar]
- McLean, J.N.; Moore, C.E.; Yellin, S.A. Gunshot wounds to the face— acute management. Facial Plast Surg 2005, 21, 191–198. [Google Scholar] [CrossRef]
- Becelli, R.; De Ponte, F.S.; Sassano, P.P.; Rinna, C. Firearm injuries in maxillofacial region reconstructive surgery. J Craniofac Surg 1995, 6, 473–476. [Google Scholar] [CrossRef]
- Dolin, J.; Scalea, T.; Mannor, L.; Sclafani, S.; Trooskin, S. The management of gunshot wounds to the face. J Trauma 1992, 33, 508–514; discussion 514–515. [Google Scholar] [PubMed]
- Demetriades, D.; Chahwan, S.; Gomez, H.; Falabella, A.; Velmahos, G.; Yamashita, D. Initial evaluation and management of gunshot wounds to the face. J Trauma 1998, 45, 39–41. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.W.; Johnson, D.D.; Jenkins, D.; Dickinson, E.; Reilly, P. Close to the vest. Body armor changes the face of penetrating injuries. JEMS 2000, 25, 32–41. [Google Scholar]
- Gofrit, O.N.; Kovalski, N.; Leibovici, D.; Shemer, J.; O'Hana, A.; Shapira, S.C. Accurate anatomical location of war injuries: Analysis of the Lebanon war fatal casualties and the proposition of new principles for the design of military personal armour system. Injury 1996, 27, 577–581. [Google Scholar] [PubMed]
- Lakstein, D.; Blumenfeld, A. Israeli Army casualties in the second Palestinian uprising. Mil Med 2005, 170, 427–430. [Google Scholar]
- Kosashvili, Y.; Hiss, J.; Davidovic, N.; et al. Influence of personal armor on distribution of entry wounds: Lessons learned from urban-setting warfare fatalities. J Trauma 2005, 58, 1236–1240. [Google Scholar]
© 2012 by the author. The Author(s) 2012.