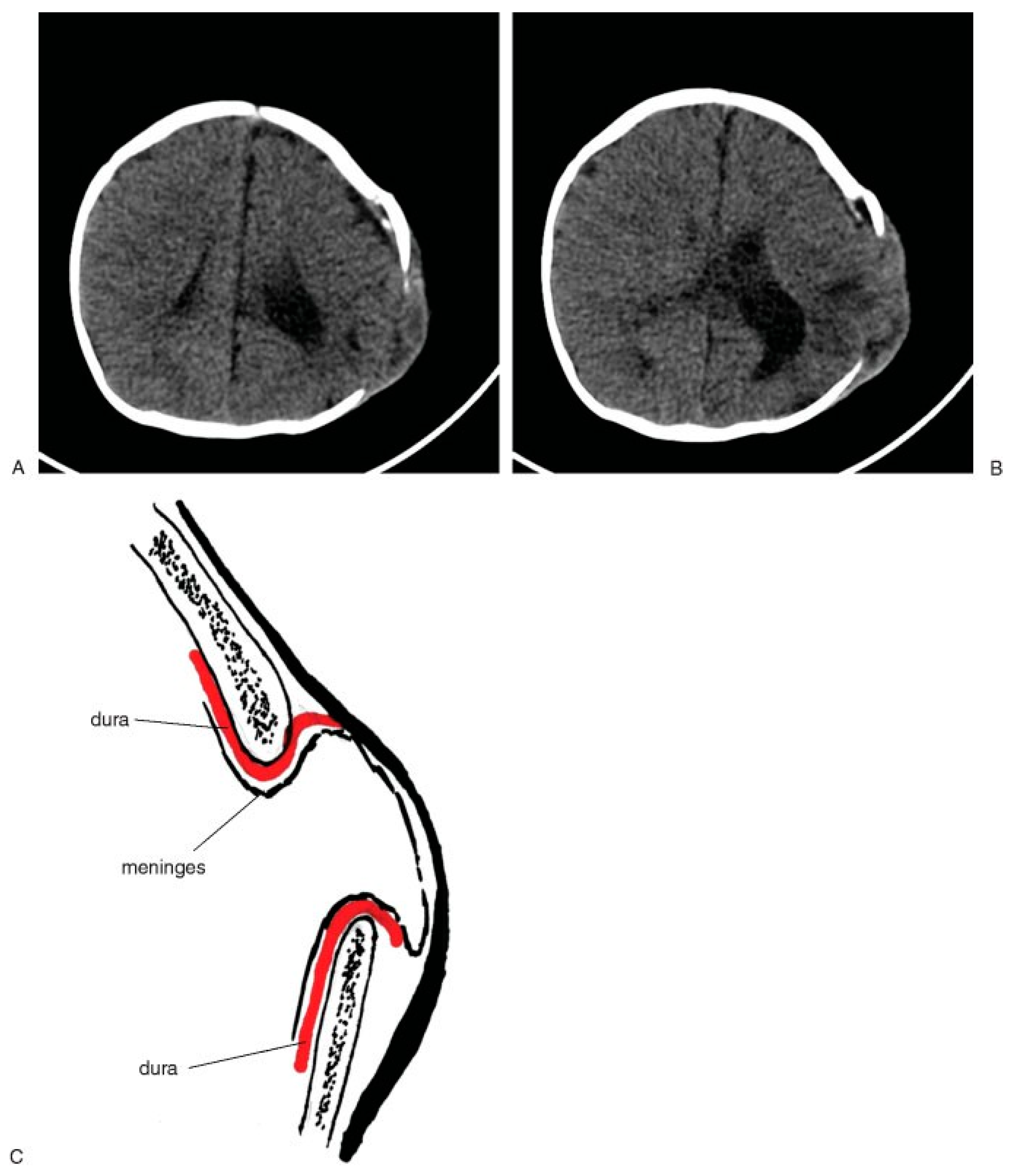
Prenatal and birth injuries to the cranium are rare, but do occur. They can be due to intrauterine compression, prolonged difficult delivery as the infant passes through the birth canal, or obstetric forceps or suction-assisted delivery techniques. All have been implicated as the cause of some postnatal deformities, but usually the injuries are minimal and recovery takes place without residual deformity. When the injuries are more extensive or do not resolve, the patients who have residual contour deformities are sent to the craniofacial surgeon for evaluation. Many of these contour deformities are the result of subgaleal or subperiosteal hematomas that are not resorbed and ossify. On computed tomography (CT), there can appear to be a duplicated cranial vault. They often take years to remodel and some have to be recontoured if they persist as aesthetic deformity (
Figure 1A–C).
When the delivery is a particularly traumatic one, cranial fractures can occur. As a potential consequence, an unusual phenomenon called ‘‘pseudo-growth’’ of the skull fracture may occur in some children. This skull fracture radiologically and clinically seems to enlarge slowly over a period of 1 to 6 months after the fracture has occurred. A palpable bone defect with protrusion of the meninges develops as the dura separates. In some patients, the defect is large enough to require bone grafting. In other patients, the pseudo-growth of the skull can be seen on radiological studies (
Figure 2A,B). In other cases, the defect is small or very limited and may not always be identifiable clinically but can be noted by palpation. Radiographic appearances, however, are not always a guide to treatment. It is the clinical examination of the integrity of the skull that dictates the need for calvarial reconstruction. Some deformity is due to a dural laceration with expansion of the remainder of the meninges and brain through the dural defect with pressure causing bone resorption. Surgical repair requires at least dural repair and possibly bone reconstruction depending upon the age of the patient. [
1,
2] Once the patient is over a year old, the efficiency of periosteal reformation of the bone is less predictable. In these cases, bone grafting is required. The use of absorbable plates and screws allows less negative influence on the healing of the reconstructed site and less potential deformity. [
3,
4] Some authors recommend routine radiological follow-up 1 year after any skull fracture to document the appearance of the pseudogrowth defect. [
1,
2]
Havlik et al. reviewed their experience and found an incidence of 0.6 to 2% of skull fractures. [
1] The contributing factors were a craniofacial bone defect, a dural tear, and expanding extracranial process, which could be either growth or a condition, such as hydrocephalus. All of the children seen in their series with this problem were 2 years of age or younger. [
1,
2,
5]
Supraorbital Fractures
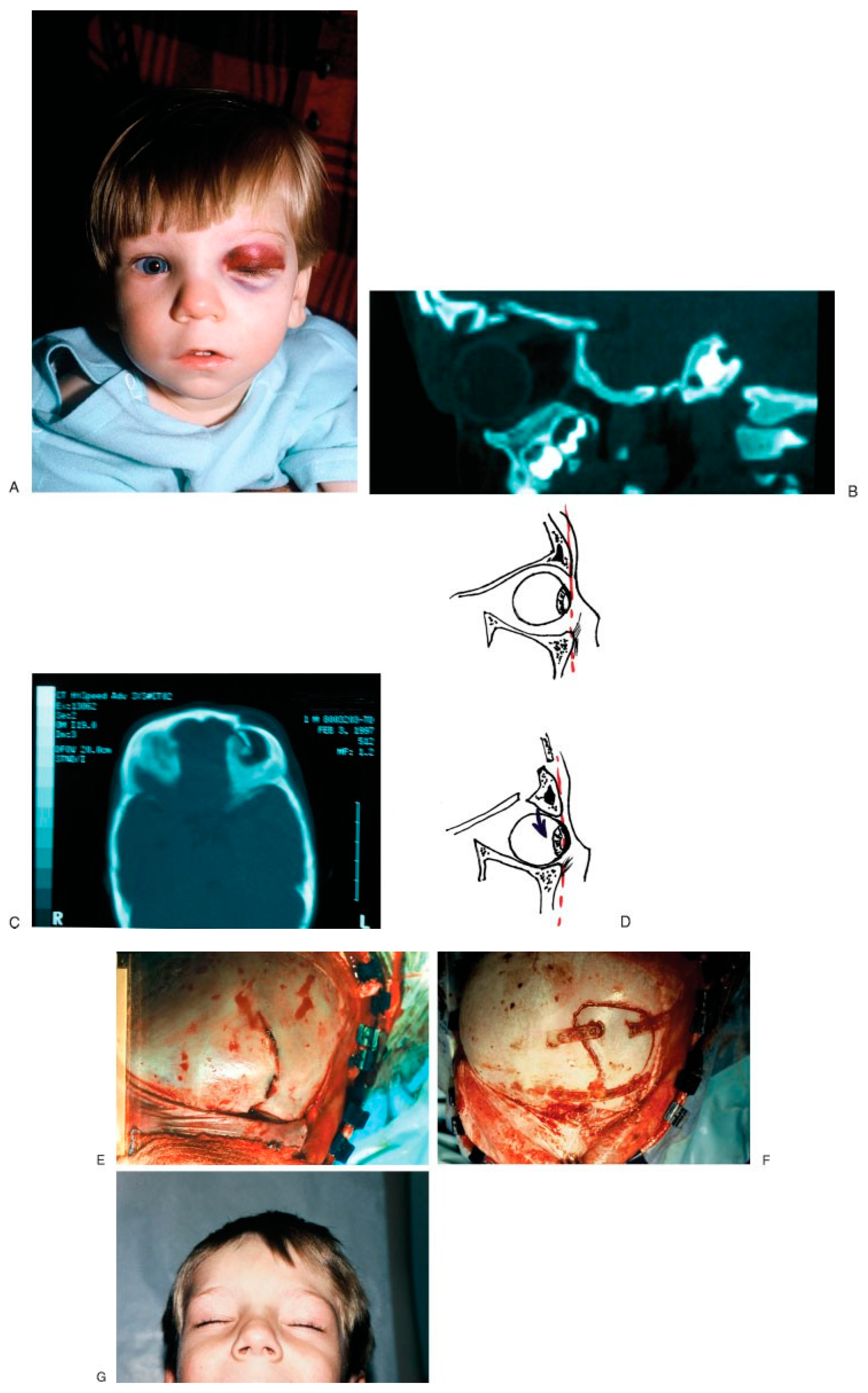
Supraorbital fractures are those that involve the superior portion of the orbital rim and orbital roof. These range from small fragments that are localized to the orbital rim to more extensive fractures that can simultaneously involve the lateral frontal bone and temporal bone. The diagnosis of supraorbital fracture is made by identifying a depression, step-off, or discrepancy in the contour of the supraorbital rim. The depression of the roof pushes the orbital globe both inferiorly and anteriorly, creating an exophthalmos and inferior globe displacement. If there is paralysis of the levator muscle, a partial or complete ptosis may be created (
Figure 3). If the patient is unable to rotate the eye upward, it may be due to direct muscle contusion or involvement of the motor nerves in the superior orbital fissure. [
6,
7] A severe fracture that extends into the superior orbital fissure may produce superior orbital fissure syndrome. The syndrome produces paralysis of all the extraocular muscles, complete ptosis, and anesthesia in the ophthalmic division of the trigeminal nerve. If the fractures extend to the optic foramen, then orbital apex syndrome results in the superior orbital fissure syndrome and blindness. [
5,
6,
7,
8]
A craniofacial CT scan is used to evaluate the brain and orbital region for the exact determination of the frontal and orbital fracture pattern and the displacements. Treatment is performed through an open reduction and fixation, often through a coronal incision, but if the fracture pattern is limited, then it might be done through an existing laceration. A more open exposure is more often needed to evacuate for epidural hematomas, repair fracture segments, brain injury, or dural lacerations.
A thorough visual screening examination should be performed whenever an orbital fracture or globe injury is suspected. The basis screening consists of evaluation of the visual acuity, confrontation fields, extraocular motion, pupil size and reactivity, evaluation of diplopia, and examination of the anterior and posterior chambers. [
5,
6]
Naso-Orbital-Ethmoidal Fractures
Another area where significant challenging problems occur is at the frontal cranial region involving the naso-orbital-ethmoidal (NOE) areas of the skull. The portions of the face change markedly during the period of postnatal growth. The skull at birth represents relatively large cranial portion and a small facial component compared with that of an adult skull. The cranial to facial proportions are 8:1 at birth, but they fall to 4:1 by 5 years of age and 2:1 in the adult. These changes are due to two factors: the natural actual growth of the face and a modification of proportions, which brings forth characteristics distinguishing the adult faces of men and women from the younger persons to establish adult individual features. [
9,
10]
The children’s craniofacial skeleton is distinguished from adults in that the nose and sinuses are essentially a single structure with the sinuses being small or absent. The ethmoid and maxillary sinuses begin to invaginate from the nasal cavity during the second trimester. They first present as separate recesses, with the ethmoid sinuses later growing into a honeycomb cluster of cells. The growth of the maxillary sinus parallels that of the face. The maxillary sinuses are narrow in the newborn and not sufficiently developed in the area beneath the orbit. The sinuses grow slowly and increase in size and become large after the age of 5 years. [
1,
5]
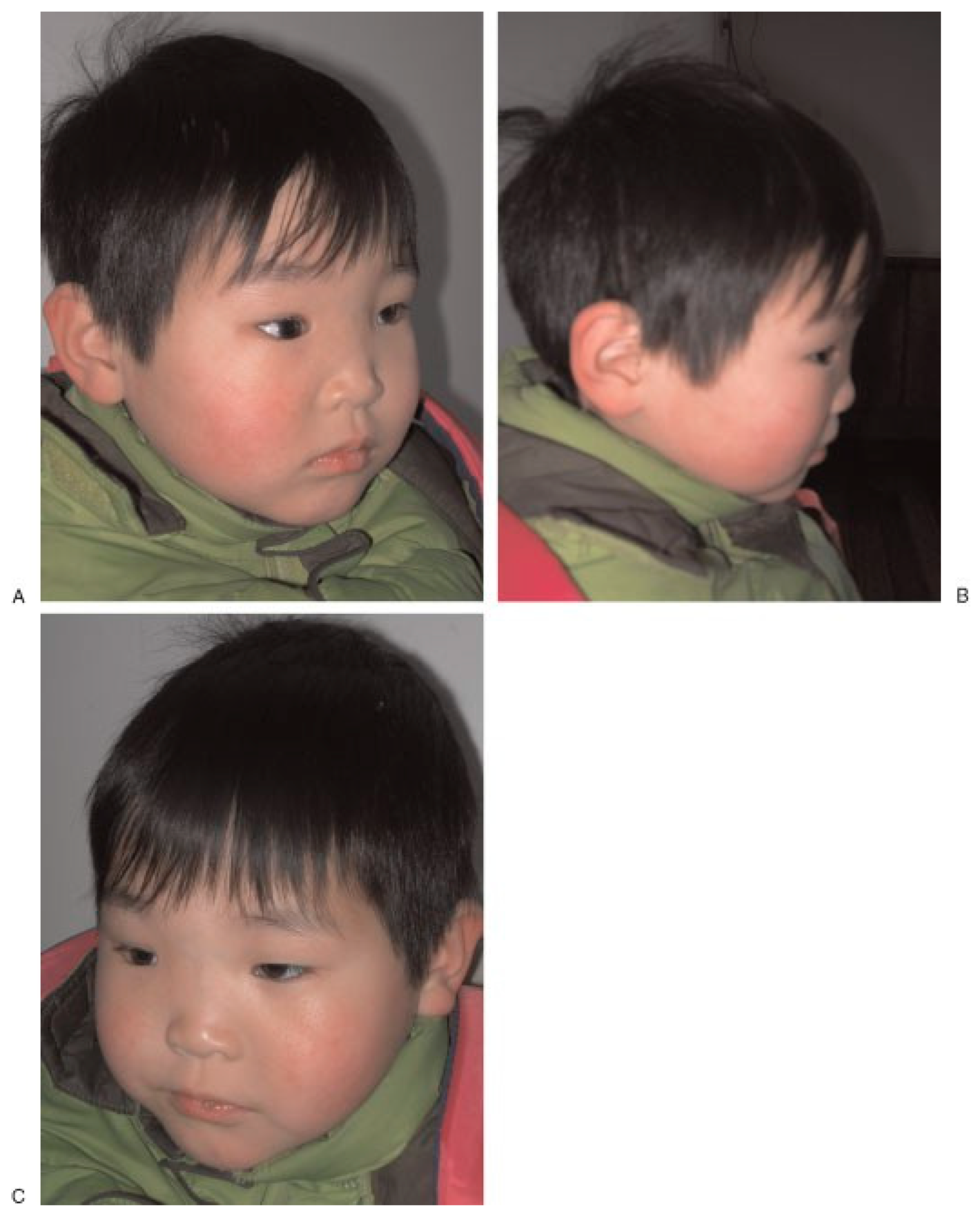
Following an injury to the upper facial area, clinical examination of the child is often difficult. Pediatric patients are frequently unable or unwilling to provide a history and the parents may or may not be present to provide additional detailed information. The children are often uncooperative and become easily frightened and apprehensive. In some cases, there may not be a history of trauma to the child, but one can see telltale signs of a significant previous injury on physical examination and CT scans (
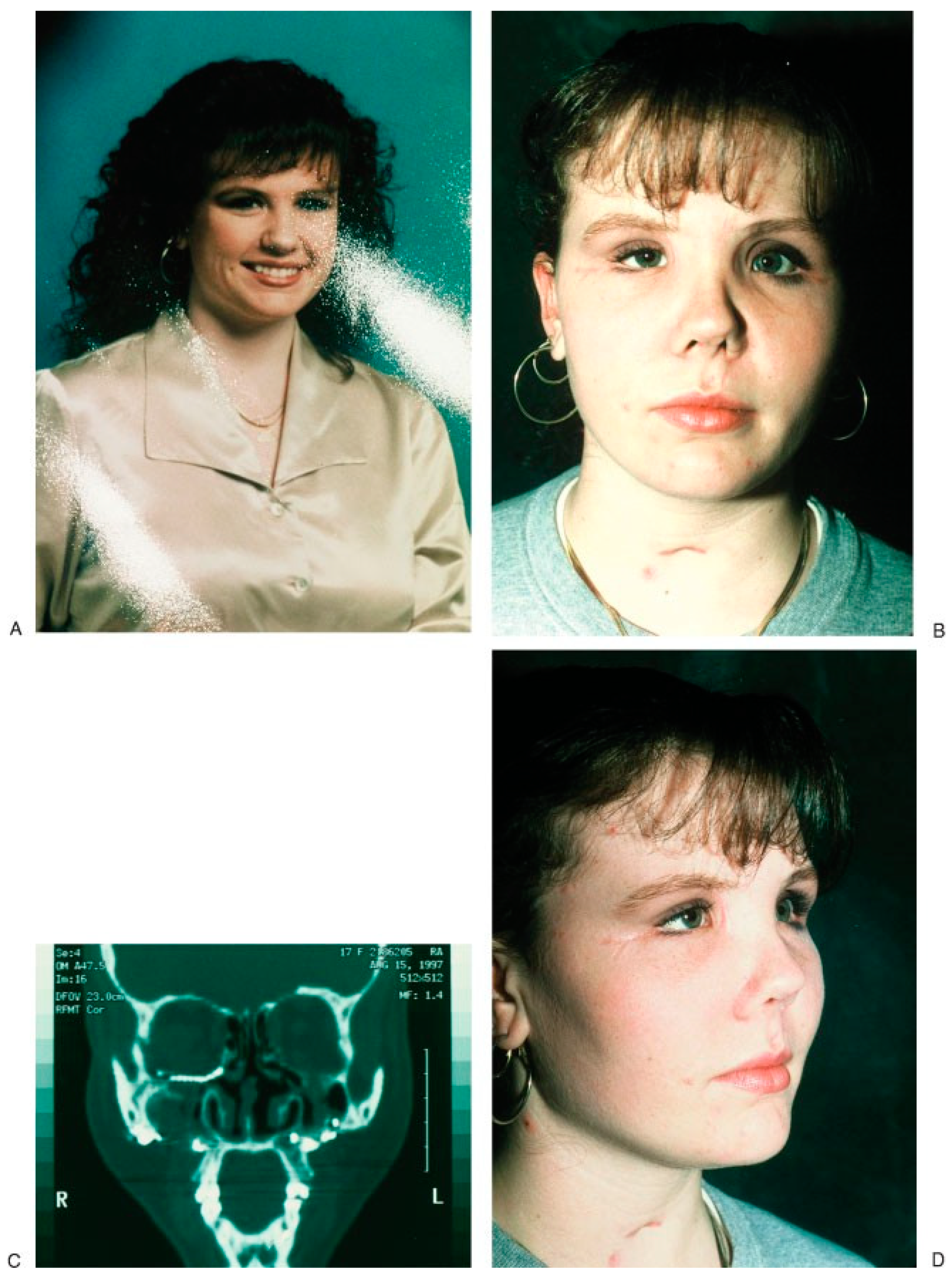
Figure 4 and
Figure 5).
The clinical examination consists of an orderly inspection of all facial areas, including observation, palpation, and a functional examination. Areas in which lacerations or bruises are present are identified. The specific areas are inspected. Frequently, an underlying fracture is present. An orderly palpation of all bone surfaces should be performed by beginning in the skull and forehead areas; the rims of the orbits and nose are palpated to identify any evidence of tenderness, irregularity, ‘‘step’’ or ‘‘level’’ discrepancies in the surface bone structure. Crepitus may be present particularly over nasal or orbital rim fractures. The examination is continued over the zygomatic arches, the cheeks, and the surface of the mandible. An intraoral examination is performed to demonstrate loose teeth and to identify intraoral lacerations or hematomas. Lateral pressure on the mandible and maxillary dental arches is necessary to determine the instability or pain in fractures involving the midline of the mandible and/or maxilla.
The clarity of imaging on computerized CT has improved the radiological diagnosis of midand upperfacial fractures and has replaced the use of plain films. Fractures of the frontal area, orbit, and maxilla are precisely demonstrated, although the examination may require sedation in young children. In addition, concomitant brain injury can be evaluated by combining facial and cranial CT scans in a single examination. However, ‘‘greenstick’’ and nondisplaced fractures are not as easily identified in CT scans.
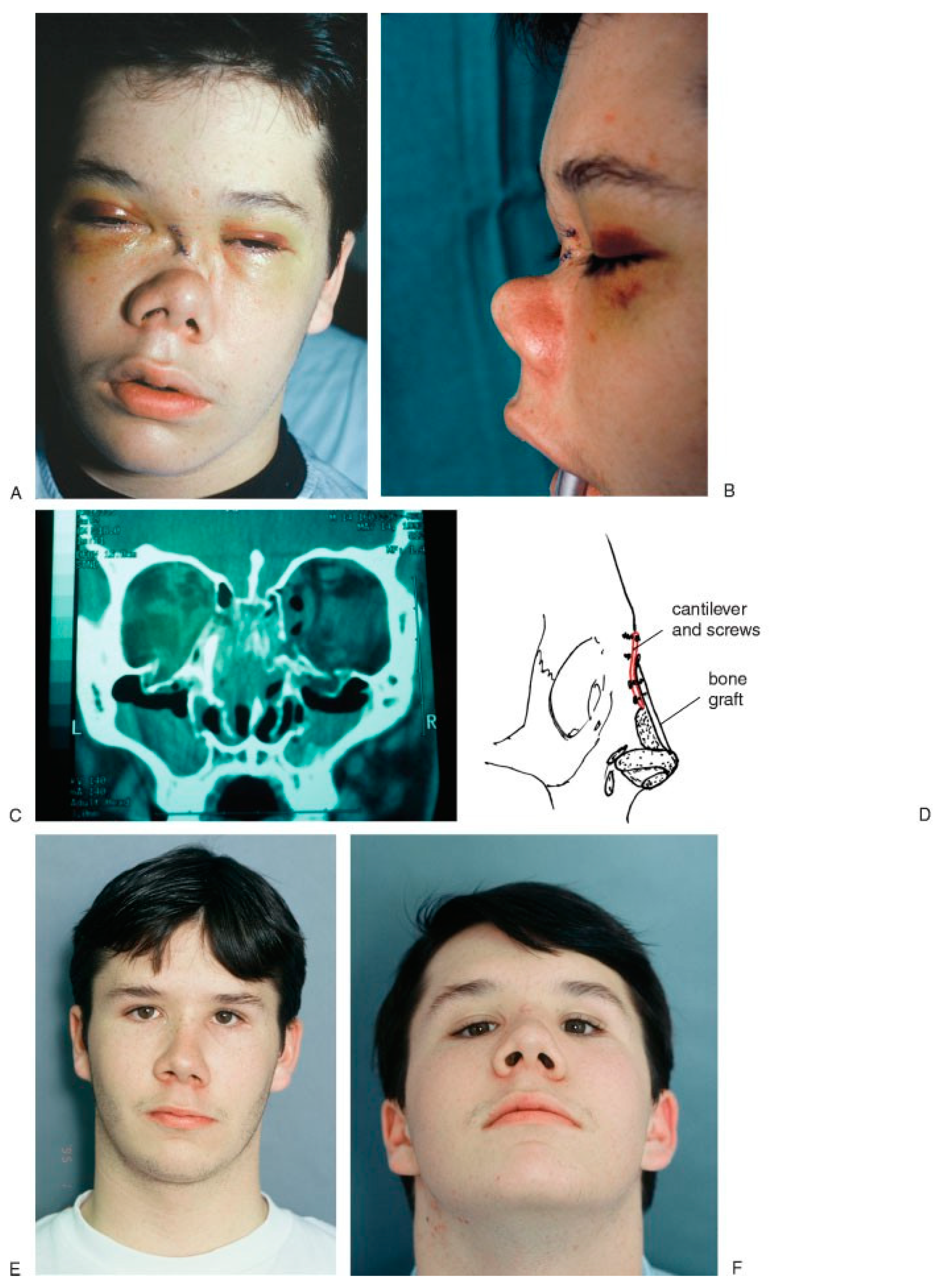
NOE fractures often result from a severe direct blow to the frontal, glabellar, or upper-nasal region or accompany frontal bone or high Le Fort II or III fractures. The nasal components of NOE fracture are pushed backward posteriorly into the interorbital space along the medial orbital rims and walls. NOE fractures are characterized by retrusion and flattening of the nasal pyramid and increased columella-lip angle with loss of distal septal nasal support. Telecanthus also exists because the fractures also involve the medial portion of the orbital rims and extend into the ethmoid sinuses, orbital floors, and medial portions of the infraorbital rims on one or both sides (
Figure 6A–D). [
11,
12,
13]
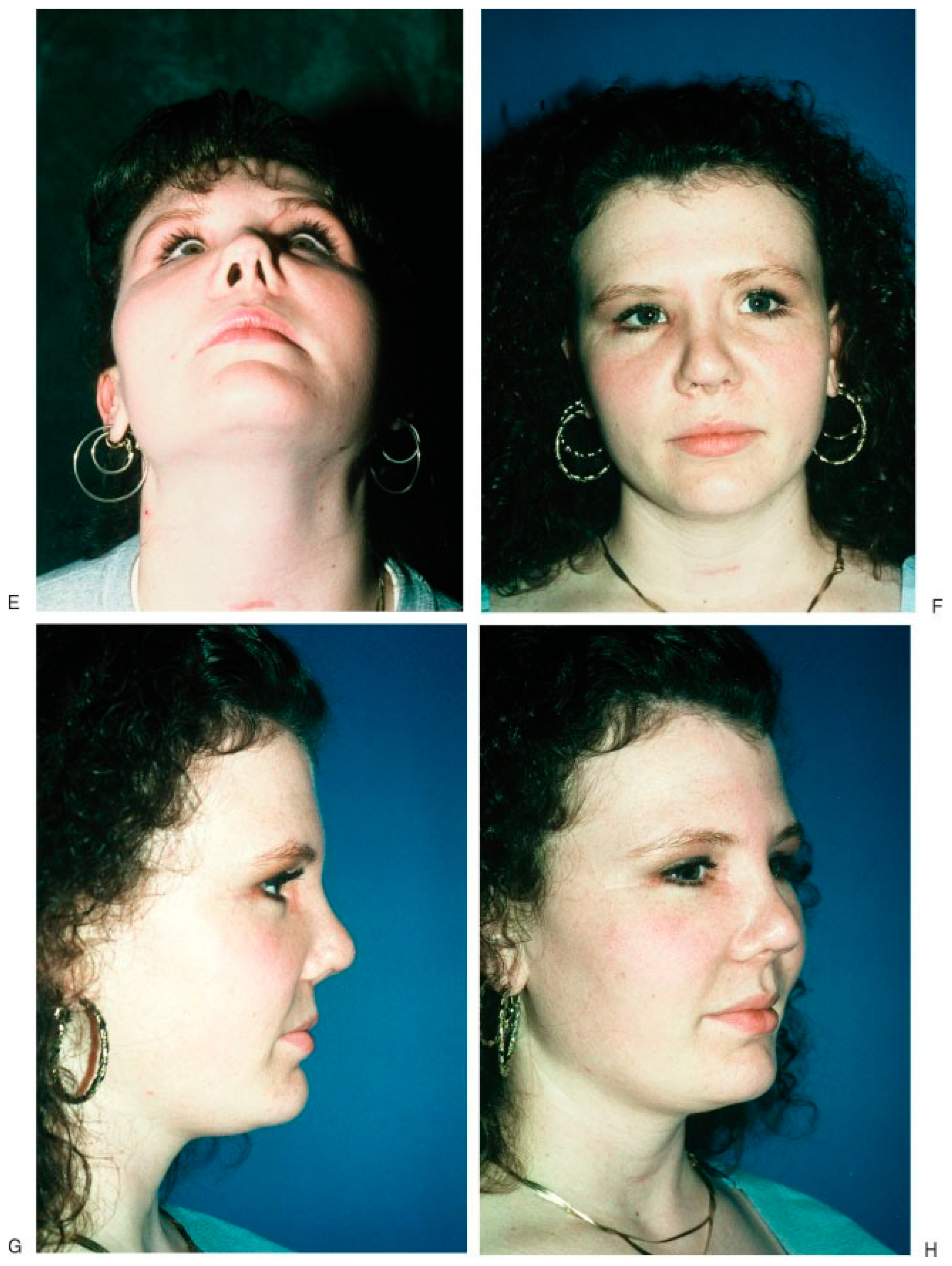
The most important principles in the treatment of NOE fractures are to restore proper projection, width, and height of the affected structures both in the acute setting as well as in the secondary reconstructions. The key initial step is to restore the proper intercanthal distance by a transnasal reduction of the medial orbital rims. The transnasal wires are placed through bone behind the canthal ligament on the posterior edge of the medial orbital rim fragments above and behind the lacrimal fossa and led to the other side so that the distance between the medial orbital rims is limited by the tightening of the two wires. Bone grafts are often used to reconstitute the nasal height, improve the aesthetic appearance, and support the distal septal structures. These are fixed to the frontal bone in a cantilever fashion. [
5,
11,
12,
13]
In secondary procedures, the same principles apply; however, they are often more challenging. Often, soft tissue contraction, loss of bony support, and failure to obtain adequate correction will result in an unsatisfactory result. Additional bone grafting around the orbital and nasal region is required to obtain the necessary support and contour correction to restore facial harmony (
Figure 7).
Conclusion
As we develop a better understanding of the treatment of these unique injuries, we can develop management protocols that permit the best outcome and at the same time prevent or avoid the potential for further deformity or secondary growth disturbances.