Evaluation of the Upper Airway in Class II Patients Undergoing Maxillary Setback and Counterclockwise Rotation in Orthognatic Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
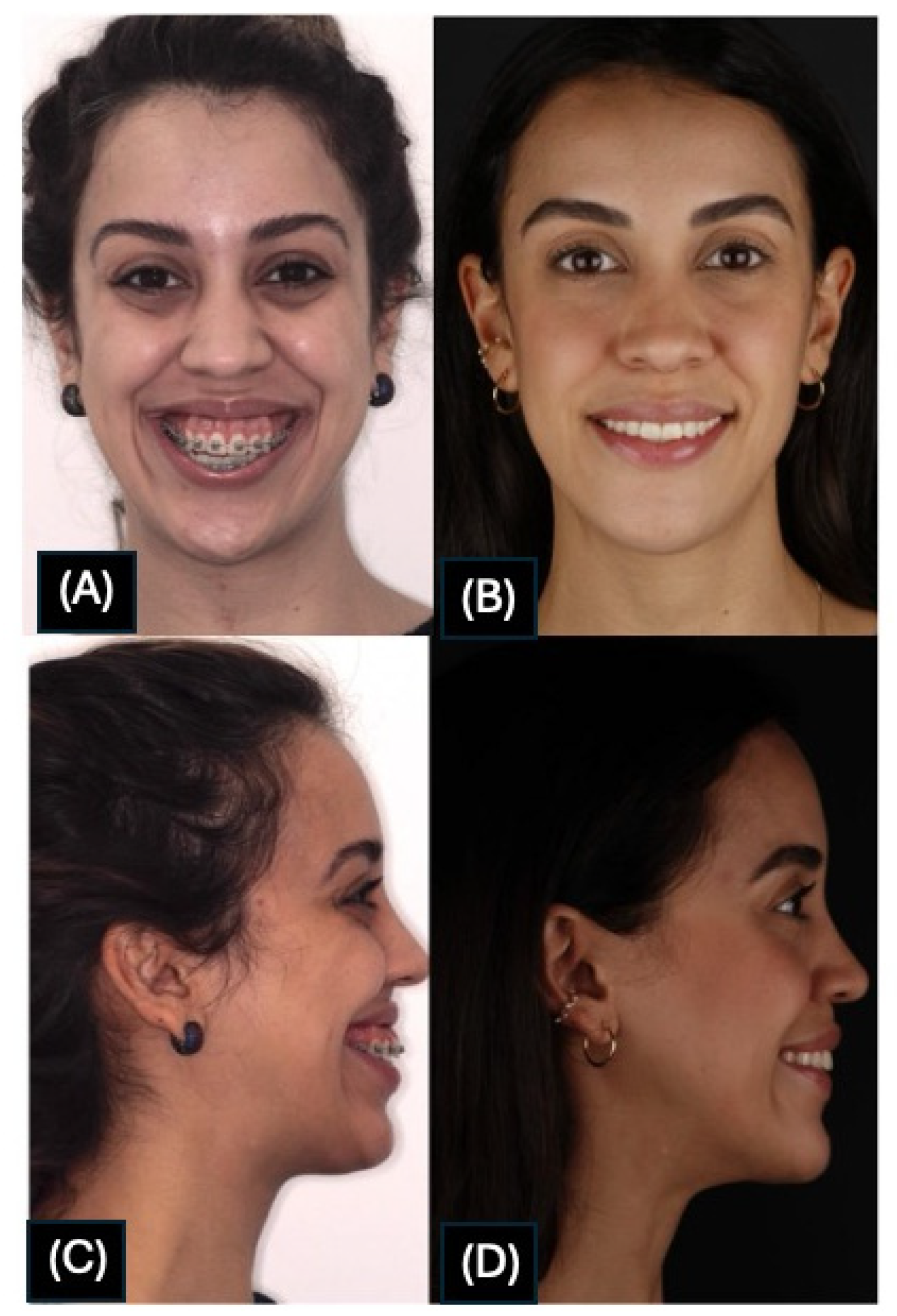
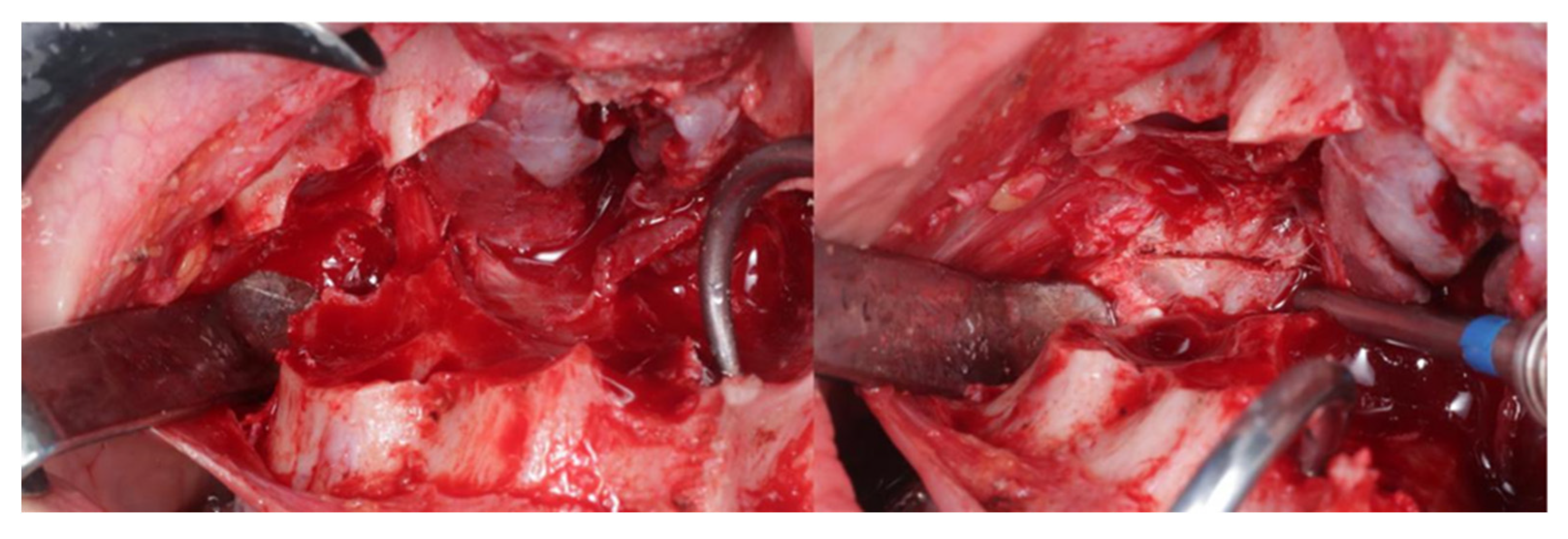
2.2. Surgical Technique
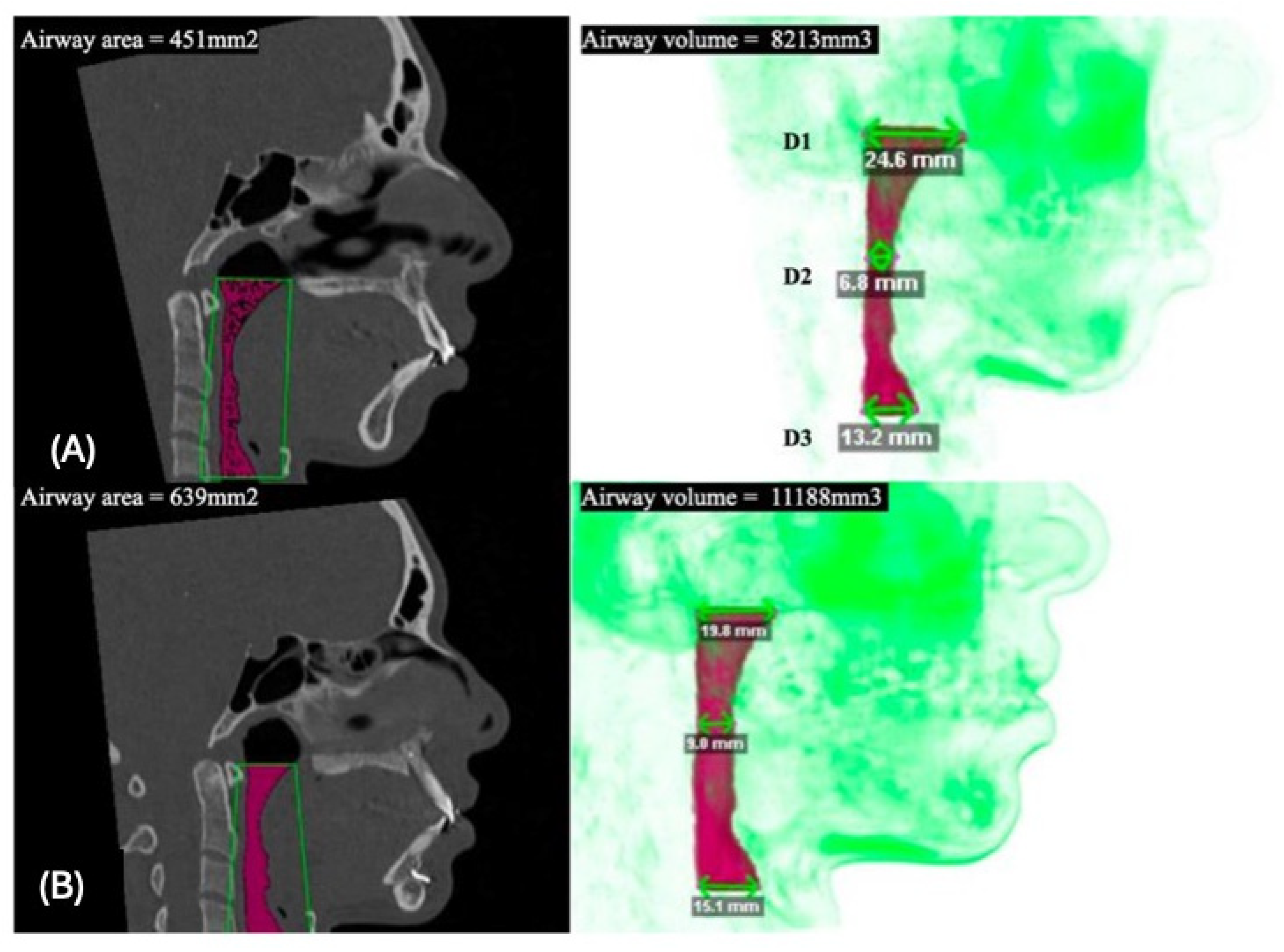
2.3. CT Scan Acquisition and Image Analysis
2.4. Statistical Analysis
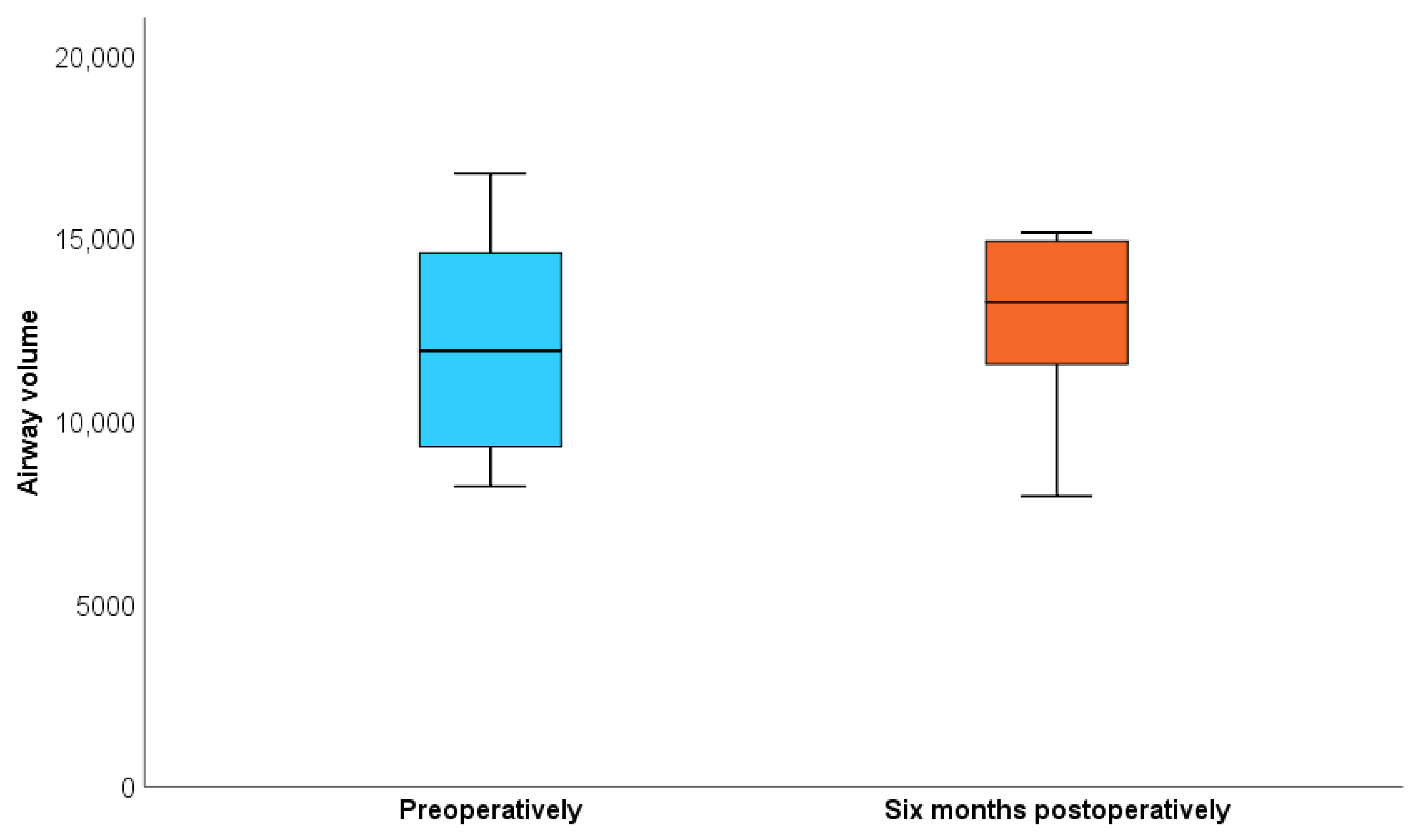
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ghoreishian, M.; Gheisari, R. The Effect of Maxillary Multidirectional Movement on Nasal Respiration. J. Oral Maxillofac. Surg. 2009, 67, 2283–2286. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, M.R.; Alcazar, N.M.P.V.; Janson, G.; de Freitas, K.M.S.; Henriques, J.F.C. Upper and Lower Pharyngeal Airways in Subjects with Class I and Class II Malocclusions and Different Growth Patterns. Am. J. Orthod. Dentofac. Orthop. 2006, 130, 742–745. [Google Scholar] [CrossRef]
- Brito, F.C.; Brunetto, D.P.; Nojima, M.C.G. Three-Dimensional Study of the Upper Airway in Different Skeletal Class II Malocclusion Patterns. Angle Orthod. 2019, 89, 93–101. [Google Scholar] [CrossRef]
- Xiang, Z.; Wang, Y.; He, Y.; Wang, Y.; Bi, R.; Li, J. Comparison of Maxillary Setback by Maxillary Tuberosity Removal or Intentional Pterygoid Plate Fracture in Le Fort I Osteotomy: A Long-Term Evaluation. Int. J. Oral. Maxillofac. Surg. 2021, 50, 487–493. [Google Scholar] [CrossRef]
- Schouman, T.; Baralle, M.-M.; Ferri, J. Facial Morphology Changes After Total Maxillary Setback Osteotomy. J. Oral Maxillofac. Surg. 2010, 68, 1504–1511. [Google Scholar] [CrossRef] [PubMed]
- Mehra, P.; Downie, M.; Pita, M.C.; Wolford, L.M. Pharyngeal Airway Space Changes after Counterclockwise Rotation of the Maxillomandibular Complex. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 154–159. [Google Scholar] [CrossRef]
- Zou, Y.; Yang, R.; Yeweng, S.; Wu, Z. MSCT 3D Analysis of Nasopharyngeal Airway After Le Fort I Maxillary Setback Surgeries. J. Craniofacial Surg. 2024, 35, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-T.; Park, J.-H.; Kwon, T.-G. Influence of Mandibular Setback Surgery on Three-Dimensional Pharyngeal Airway Changes. Int. J. Oral Maxillofac. Surg. 2019, 48, 1057–1065. [Google Scholar] [CrossRef]
- Esteves, L.S.; Ávila, C.; Medeiros, P.J. Changes in Occlusal Plane through Orthognathic Surgery. Dental Press. J. Orthod. 2012, 17, 160–173. [Google Scholar] [CrossRef]
- Lee, J.-Y.; Kim, Y.-I.; Hwang, D.-S.; Park, S.-B. Effect of Setback Le Fort I Osteotomy on Midfacial Soft-Tissue Changes as Evaluated by Cone-Beam Computed Tomography Superimposition for Cases of Skeletal Class III Malocclusion. Int. J. Oral Maxillofac. Surg. 2013, 42, 790–795. [Google Scholar] [CrossRef]
- Kaygısız, E.; Tuncer, B.B.; Yüksel, S.; Tuncer, C.; Yıldız, C. Effects of Maxillary Protraction and Fixed Appliance Therapy on the Pharyngeal Airway. Angle Orthod. 2009, 79, 660–667. [Google Scholar] [CrossRef]
- Ward, J.L.; Garri, J.I.; Wolfe, S.A. Posterior Movements of the Maxilla. J. Craniofacial Surg. 2007, 18, 882–886. [Google Scholar] [CrossRef]
- Tomita, D.; Haga, S.; Tanzawa, F.; Miyazawa, T.; Nakano, H.; Maki, K. Maxillary Protrusion with Severe Overjet Treated by Maxillary Anterior Alveolar Osteotomy. Case Rep. Dent. 2024, 2024, 3850765. [Google Scholar] [CrossRef]
- Kim, T.; Baek, S.-H.; Choi, J.-Y. Effect of Posterior Impaction and Setback of the Maxilla on Retropalatal Airway and Velopharyngeal Dimensions after Two-Jaw Surgery in Skeletal Class III Patients. Angle Orthod. 2015, 85, 625–630. [Google Scholar] [CrossRef]
- de Sousa Miranda, W.; Álvares de Castro Rocha, V.; Lara dos Santos Marques, K.; Trindade Neto, A.I.; do Prado, C.J.; Zanetta-Barbosa, D. Three-Dimensional Evaluation of Superior Airway Space after Orthognathic Surgery with Counterclockwise Rotation and Advancement of the Maxillomandibular Complex in Class II Patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 453–458. [Google Scholar] [CrossRef]
- Pereira, P.K.N.; de Castro Rocha, V.Á.; Degan, V.V.; Garib, D.G.; Vedovello, S.A.S.; de Menezes, C.C. Upper Airways after Mandibular Advancement Orthognathic Surgery: A 4-Year Follow-Up. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 743–749. [Google Scholar] [CrossRef]
- Rathi, S.; Gilani, R.; Kamble, R.; Bhandwalkar, S. Temporomandibular Joint Disorder and Airway in Class II Malocclusion: A Review. Cureus 2022, 14, e30515. [Google Scholar] [CrossRef] [PubMed]
- Steegman, R.; Hogeveen, F.; Schoeman, A.; Ren, Y. Cone Beam Computed Tomography Volumetric Airway Changes after Orthognathic Surgery: A Systematic Review. Int. J. Oral. Maxillofac. Surg. 2023, 52, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Han, J.J.; Hwang, S.J. Evaluation of Early Postoperative Healing of Pterygomaxillary Region after LeFort I Osteotomy with Total Maxillary Setback Movement. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Bertolazi, A.N.; Fagondes, S.C.; Hoff, L.S.; Dartora, E.G.; da Silva Miozzo, I.C.; de Barba, M.E.F.; Menna Barreto, S.S. Validation of the Brazilian Portuguese Version of the Pittsburgh Sleep Quality Index. Sleep Med. 2011, 12, 70–75. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | n = 8 | n (%) |
|---|---|---|
| Sex | Female | 7 (87.5) |
| Male | 1 (12.5) | |
| Age | Mean (standard deviation) | 29.4 (7.8) |
| Median (min-max) | 29 (20–45) |
| Characteristics | n = 8 | n (%) |
|---|---|---|
| Mandibular advancement | Mean (standard deviation) | 10.20 (4.17) |
| Median (min–max) | 12.15 (3.30; 13.70) | |
| Interquartile range | 7.15; 13 | |
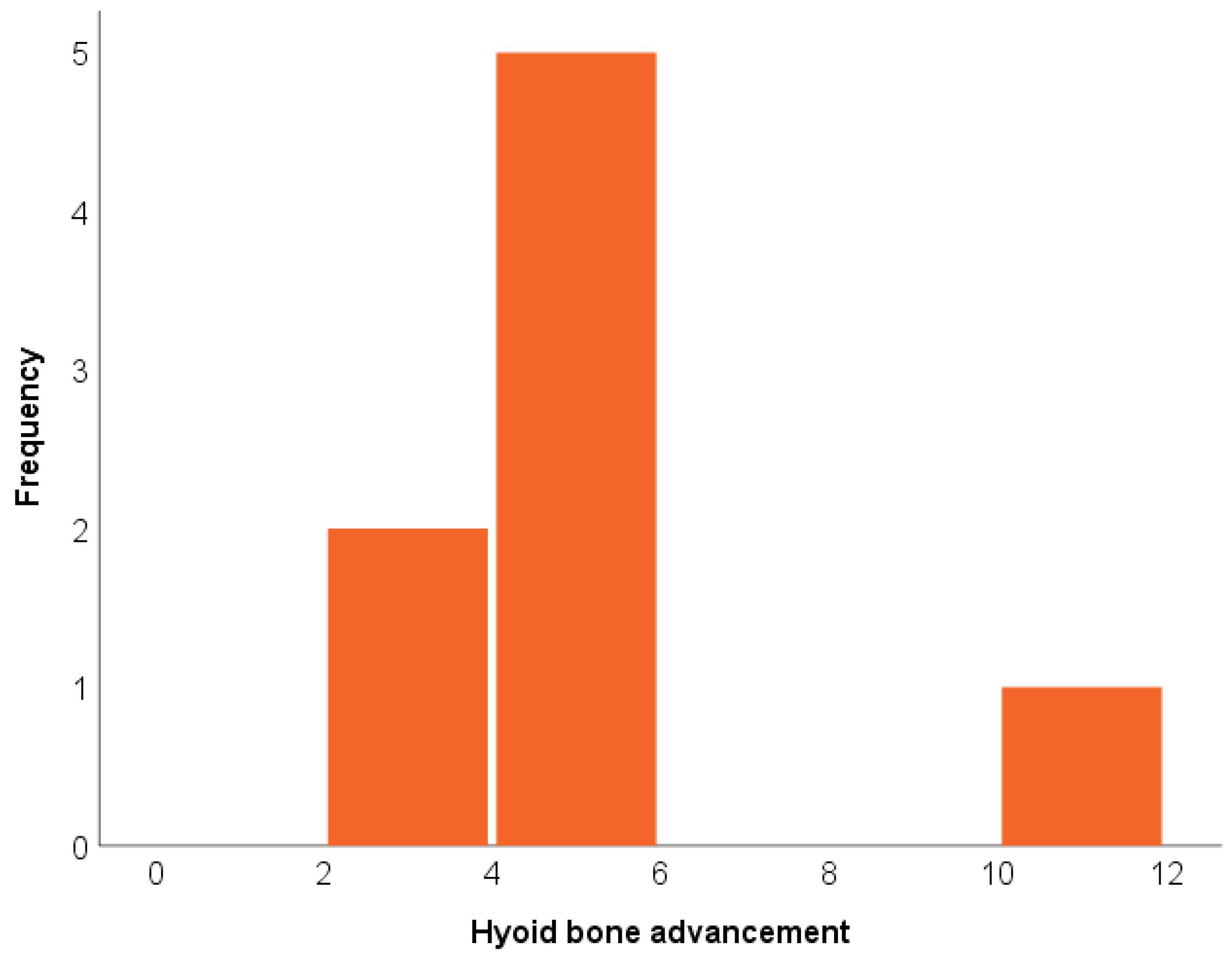
| Hyoid bone advancement | Mean (standard deviation) | 5.20 (2.79) |
| Median (min–max) | 4.70 (2.90; 11.70) | |
| Interquartile range | 3.55; 5.25 | |
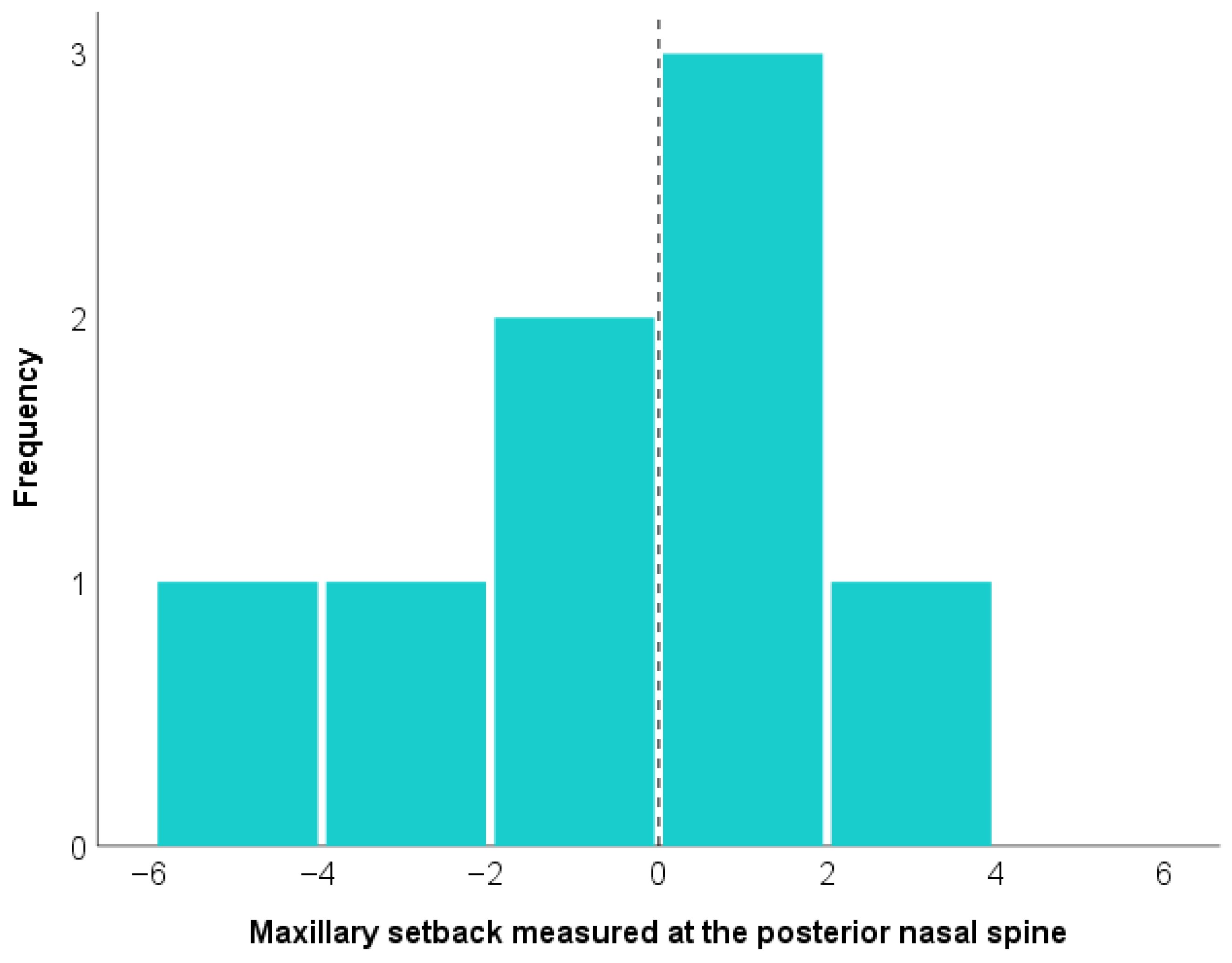
| Maxillary setback measured at the posterior nasal spine | Mean (standard deviation) | −1.25 (2.67) |
| Median (min–max) | −1.47 (−5.71; 3.46) | |
| Interquartile range | −2.63; 0.14 | |
| Maxillary setback measured at the anterior nasal spine | Mean (standard deviation) | −1.81 (2.27) |
| Median (min–max) | −0.83 (−5.93; 0.62) | |
| Interquartile range | −3.72; −0.17 | |
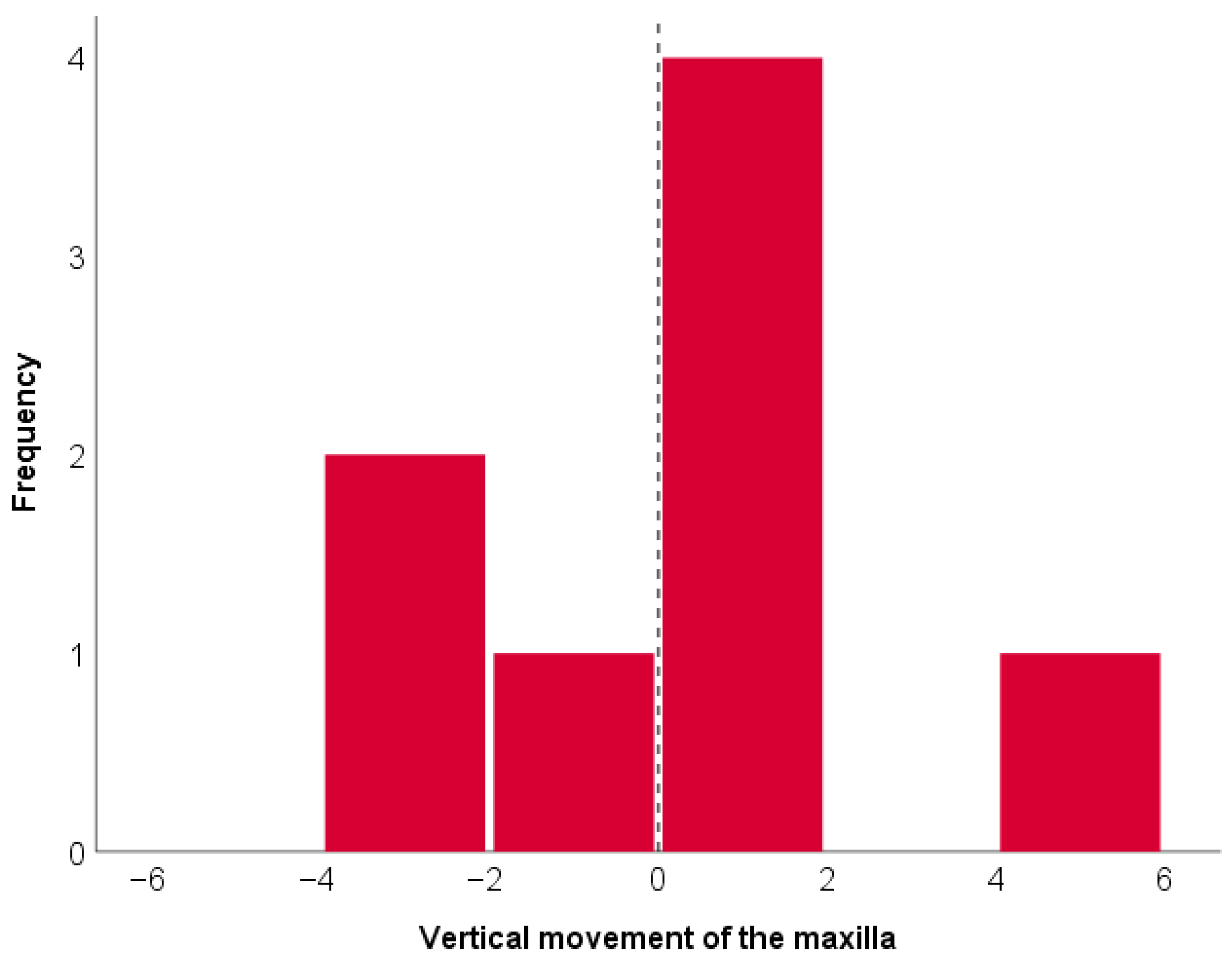
| Vertical movement of the maxilla | Mean (standard deviation) | 0.12 (2.38) |
| Median (min–max) | 0.50 (−3.26; 4.43) | |
| Interquartile range | −1.68; 1.06 | |
| Rotation of the occlusal plane | Mean (standard deviation) | 4.14 (1.90) |
| Median (min±max) | 3.99 (1.50; 7.12) | |
| Interquartile range | 2.74; 5.50 |
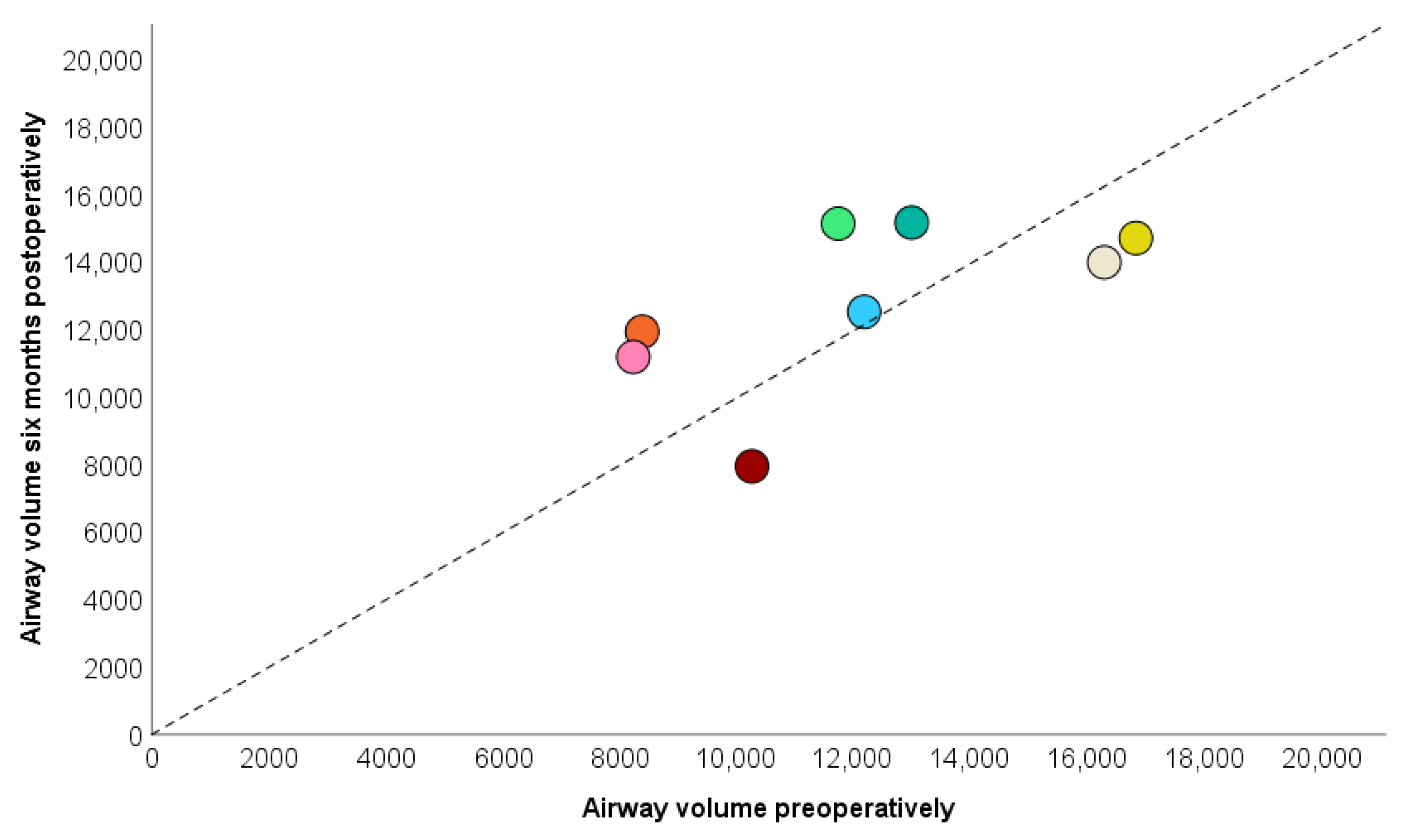
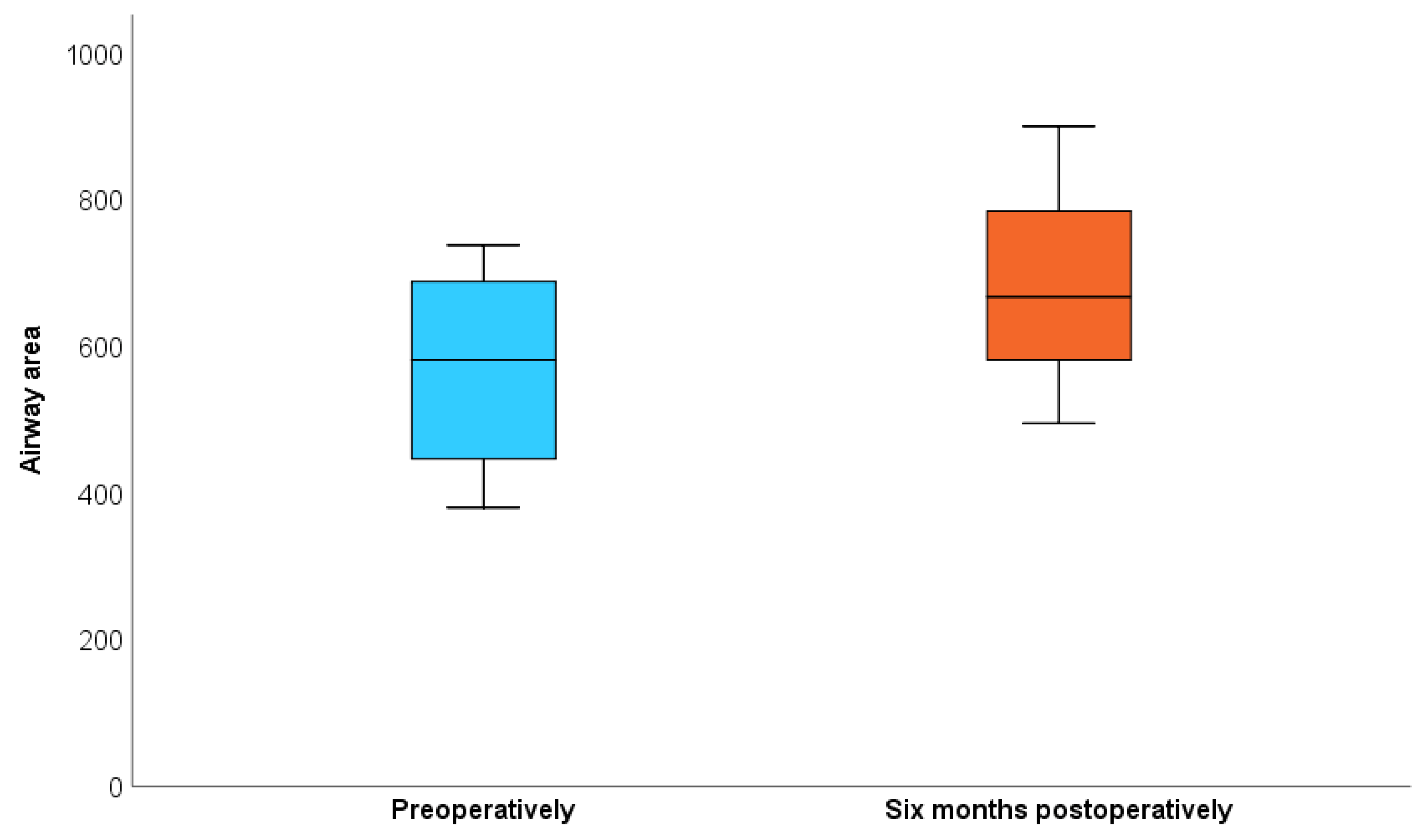
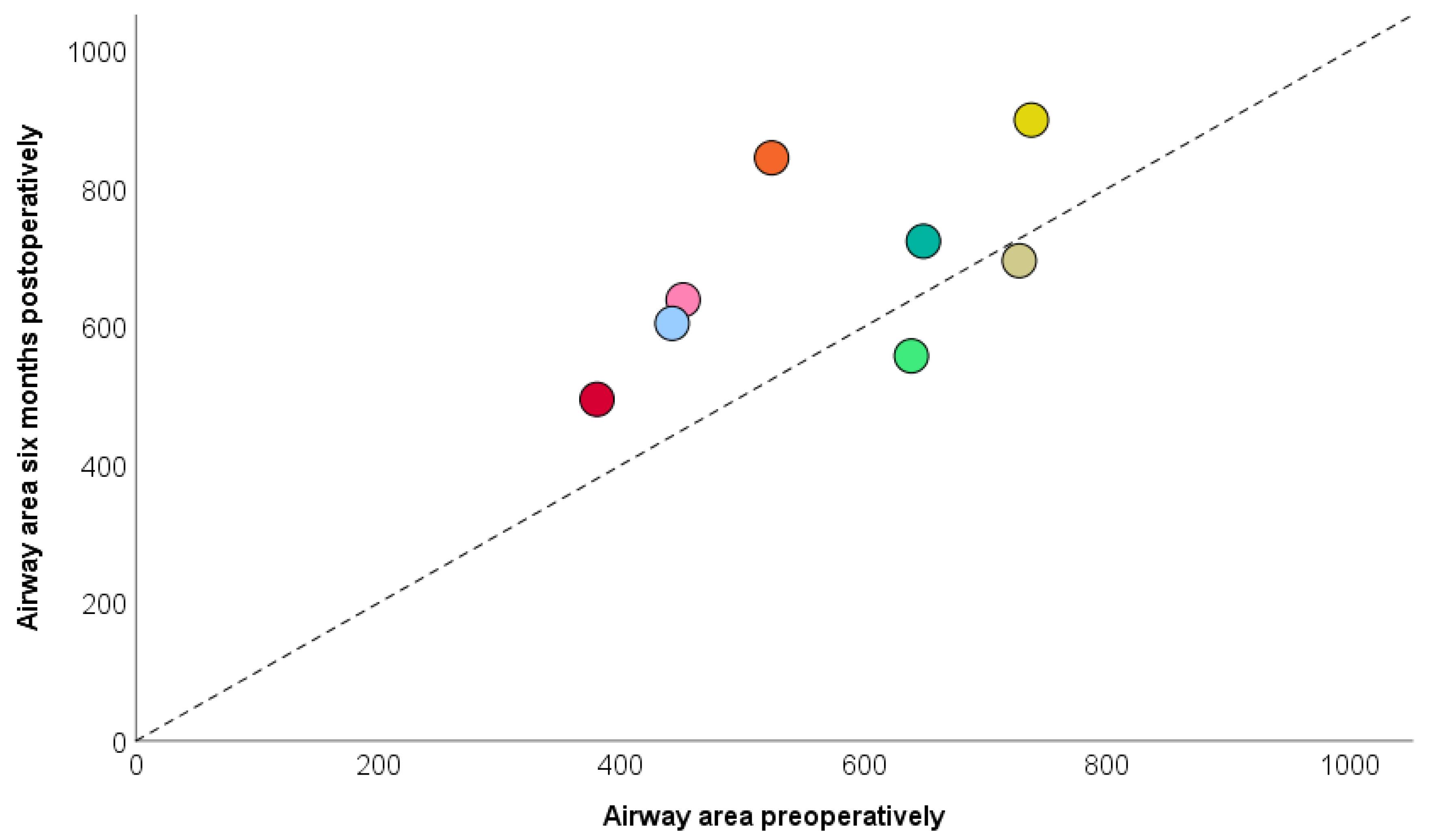
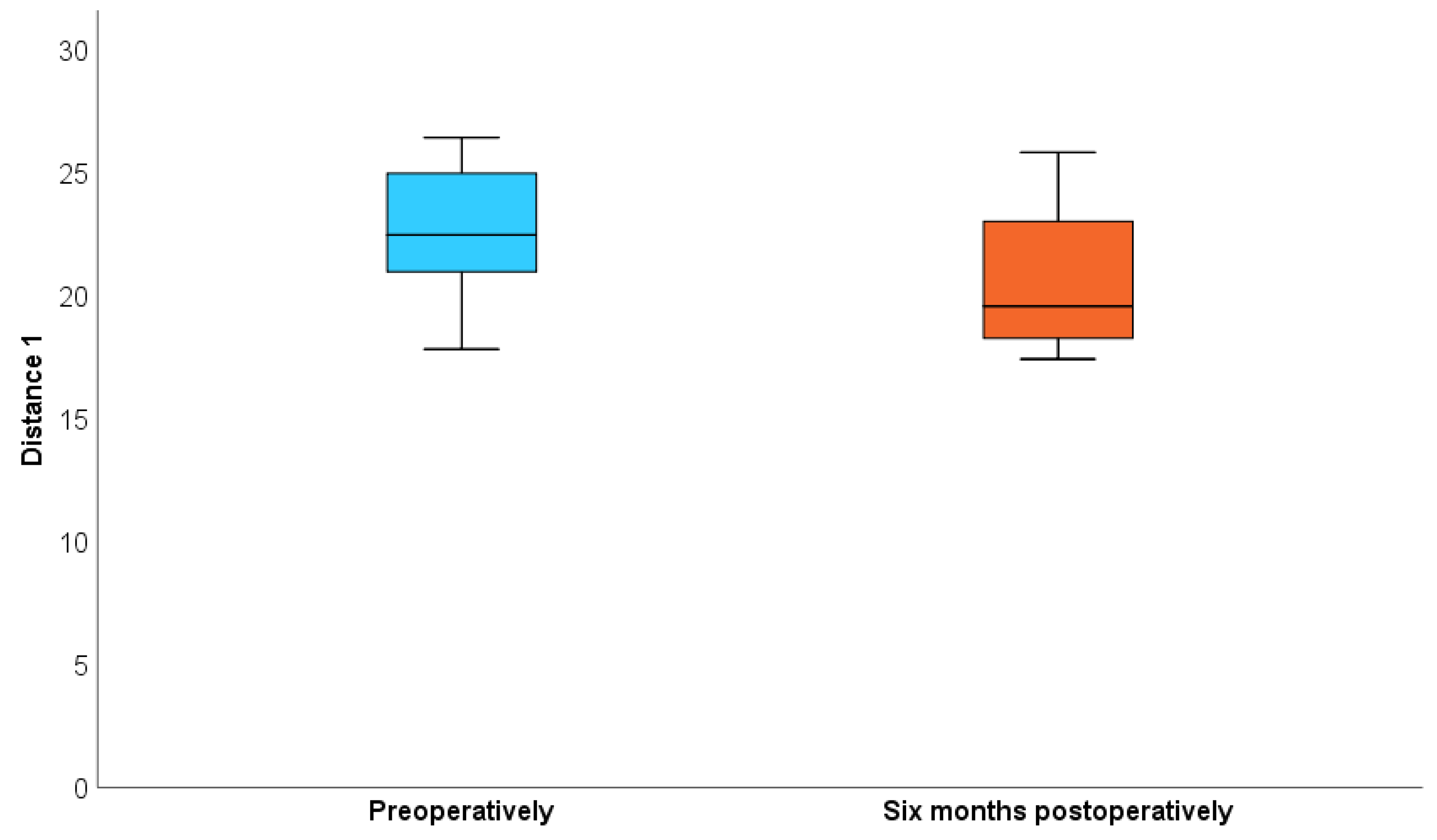
| Characteristics (n = 8) | Preoperative | Postoperative (6 Months) | p Value |
|---|---|---|---|
| Airway volume | 0.327 | ||
| Mean (DP) | 12,080.50 (3217.95) | 12,825.38 (2481.60) | |
| Median (IIQ) | 11,926 (9300–14,599) | 132,585.0 (11,562.50–14,924) | |
| Airway area | 0.050 | ||
| Mean (DP) | 568.88 (137.81) | 682.75 (138.45) | |
| Median (IIQ) | 581.50 (446.50–688.50) | 667.50 (581.50–784.50) | |
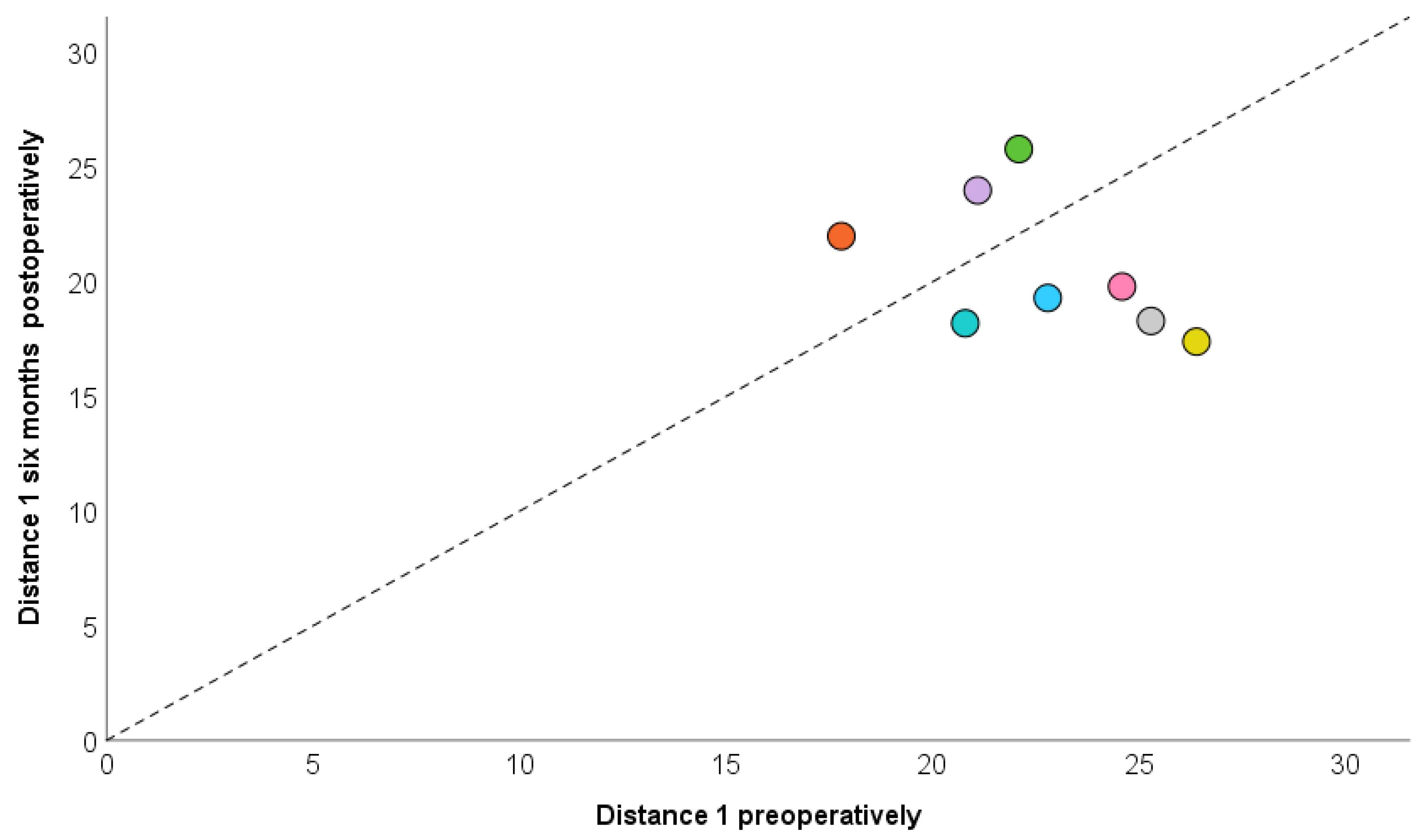
| Distance 1 | 0.327 | ||
| Mean (DP) | 22.61 (2.79) | 20.60 (3.03) | |
| Median (IIQ) | 22.45 (20.95–24.95) | 19.55 (18.25–23) | |
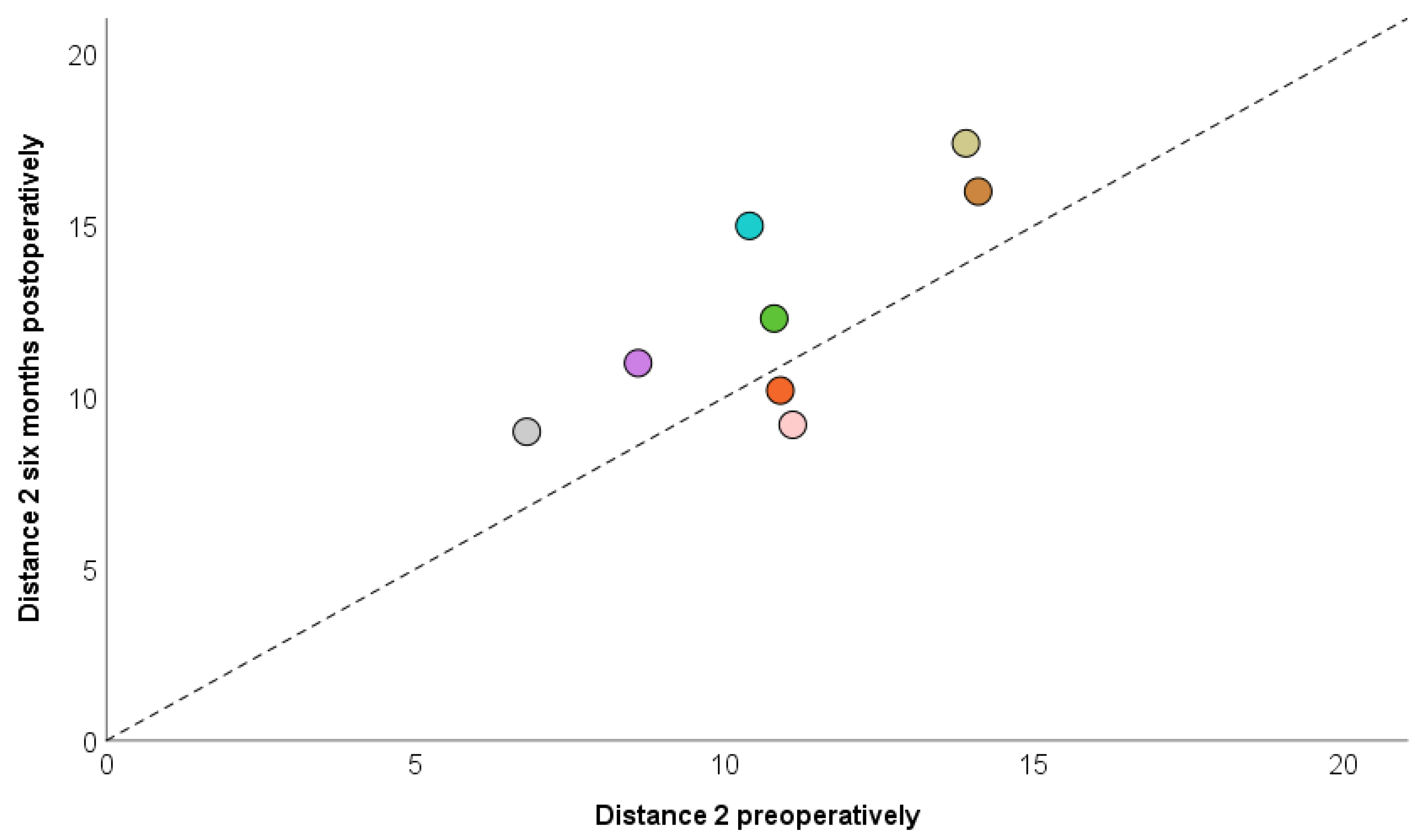
| Distance 2 | 0.058 | ||
| Mean (DP) | 10.83 (2.44) | 12.51 (3.23) | |
| Median (IIQ) | 10.85 (9.50–12.50) | 11.65 (9.70–15.50) | |
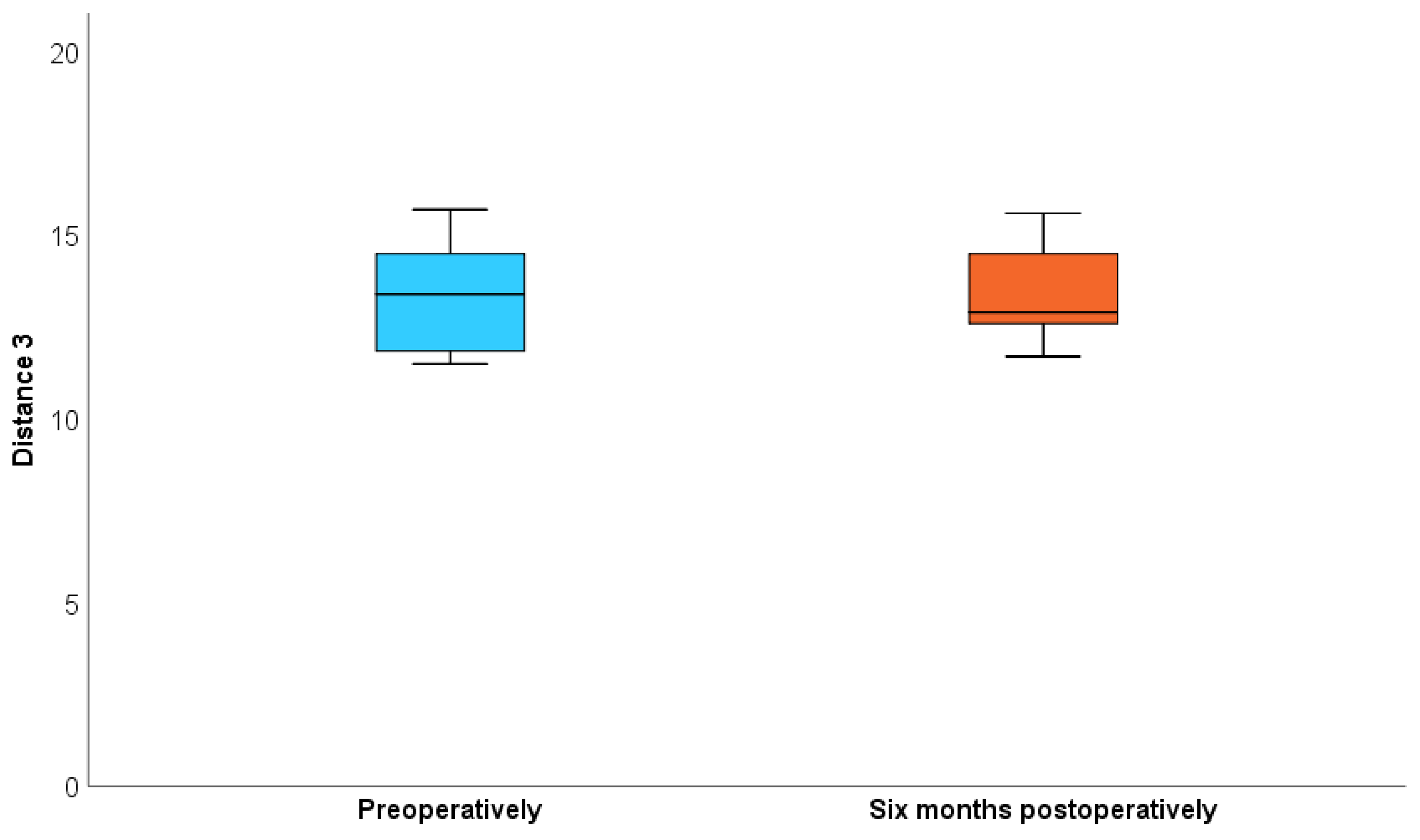
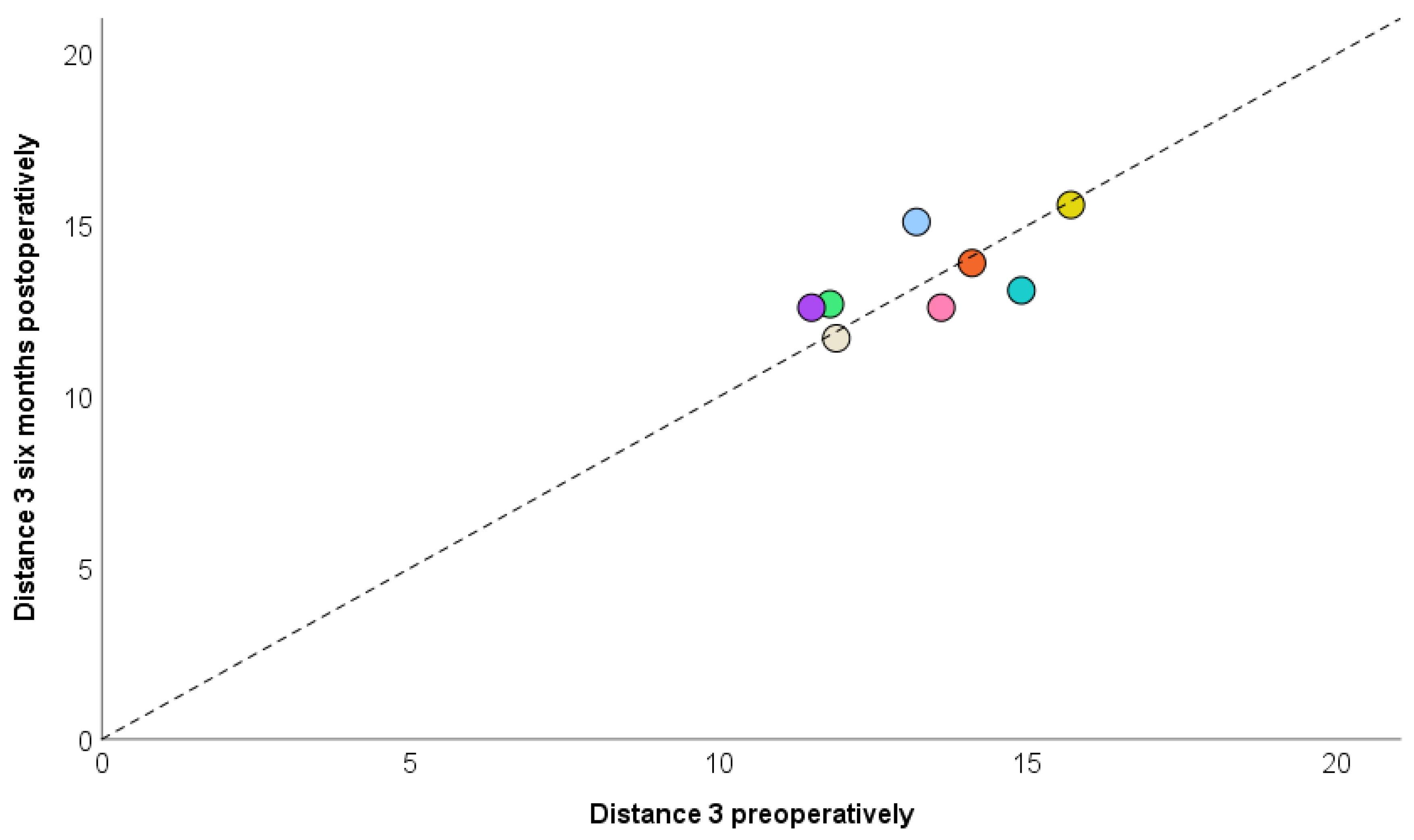
| Distance 3 | 0.999 | ||
| Mean (DP) | 13.34 (1.54) | 13.41 (1.35) | |
| Median (IIQ) | 13.40 (11.85–14.50) | 12.90 (12.60–14.50) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Lima, F.F.; De Carvalho, T.M.I.; Pulino, B.; Cerantula, C.; Correa, M.G.; Guerra, R.C. Evaluation of the Upper Airway in Class II Patients Undergoing Maxillary Setback and Counterclockwise Rotation in Orthognatic Surgery. Craniomaxillofac. Trauma Reconstr. 2025, 18, 39. https://doi.org/10.3390/cmtr18030039
de Lima FF, De Carvalho TMI, Pulino B, Cerantula C, Correa MG, Guerra RC. Evaluation of the Upper Airway in Class II Patients Undergoing Maxillary Setback and Counterclockwise Rotation in Orthognatic Surgery. Craniomaxillofacial Trauma & Reconstruction. 2025; 18(3):39. https://doi.org/10.3390/cmtr18030039
Chicago/Turabian Stylede Lima, Flávio Fidêncio, Tayná Mendes Inácio De Carvalho, Bianca Pulino, Camila Cerantula, Mônica Grazieli Correa, and Raphael Capelli Guerra. 2025. "Evaluation of the Upper Airway in Class II Patients Undergoing Maxillary Setback and Counterclockwise Rotation in Orthognatic Surgery" Craniomaxillofacial Trauma & Reconstruction 18, no. 3: 39. https://doi.org/10.3390/cmtr18030039
APA Stylede Lima, F. F., De Carvalho, T. M. I., Pulino, B., Cerantula, C., Correa, M. G., & Guerra, R. C. (2025). Evaluation of the Upper Airway in Class II Patients Undergoing Maxillary Setback and Counterclockwise Rotation in Orthognatic Surgery. Craniomaxillofacial Trauma & Reconstruction, 18(3), 39. https://doi.org/10.3390/cmtr18030039







