Current Evidence for the Management of Edentulous Atrophic Mandible Fractures: A PRISMA-SWiM Guided Review
Abstract
:Introduction
Background
- Provide consistent evidence regarding the management of atrophic mandible fractures.
- To search, evaluate, and validate existing guidelines if any for the management.
- Provide evidence regarding specific management of condylar fractures in the atrophic mandible.
- To address the clinical applicability of bone grafts
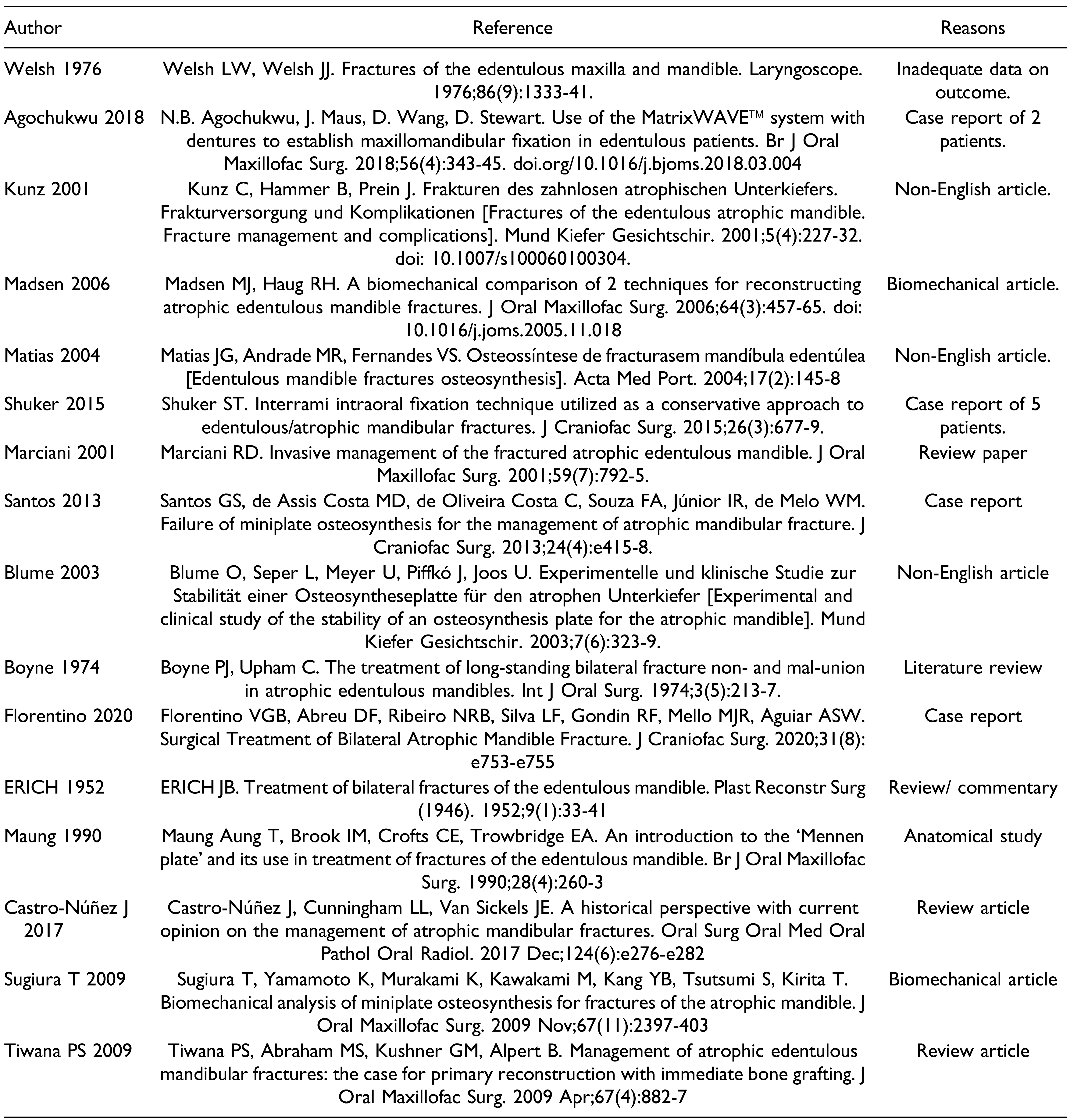
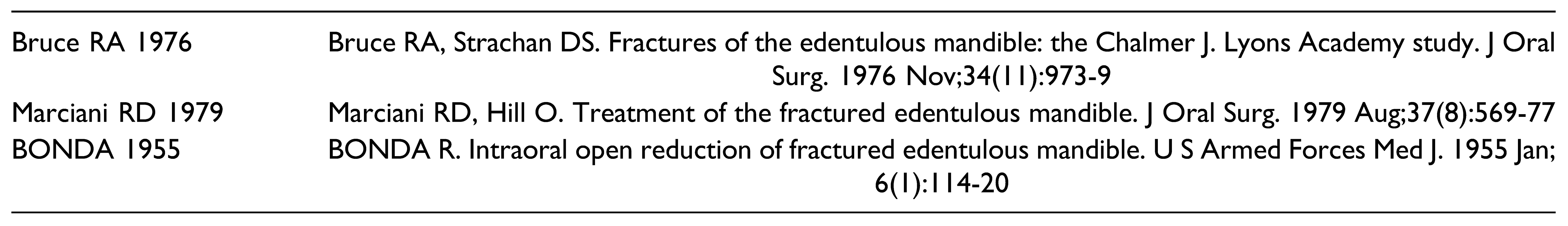
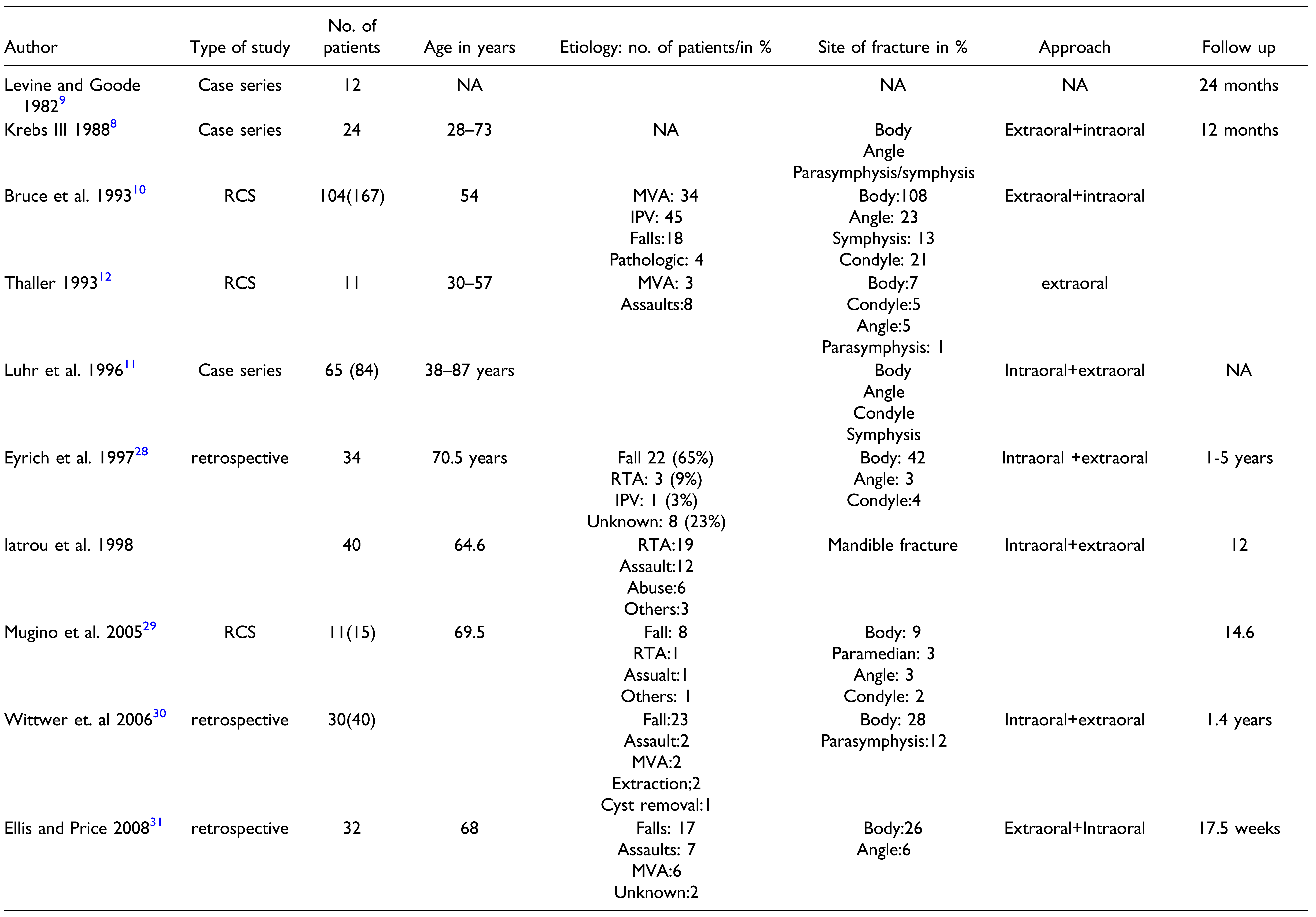
Methods
Protocol and Registration
- Clinical trials, interventional and observational studies on the management of atrophic mandible fractures.
- Case reports with >10 cases.
- Language Filter: English
- Studies with data on at least one of the post operative outcomes described above.
Quality Assessment
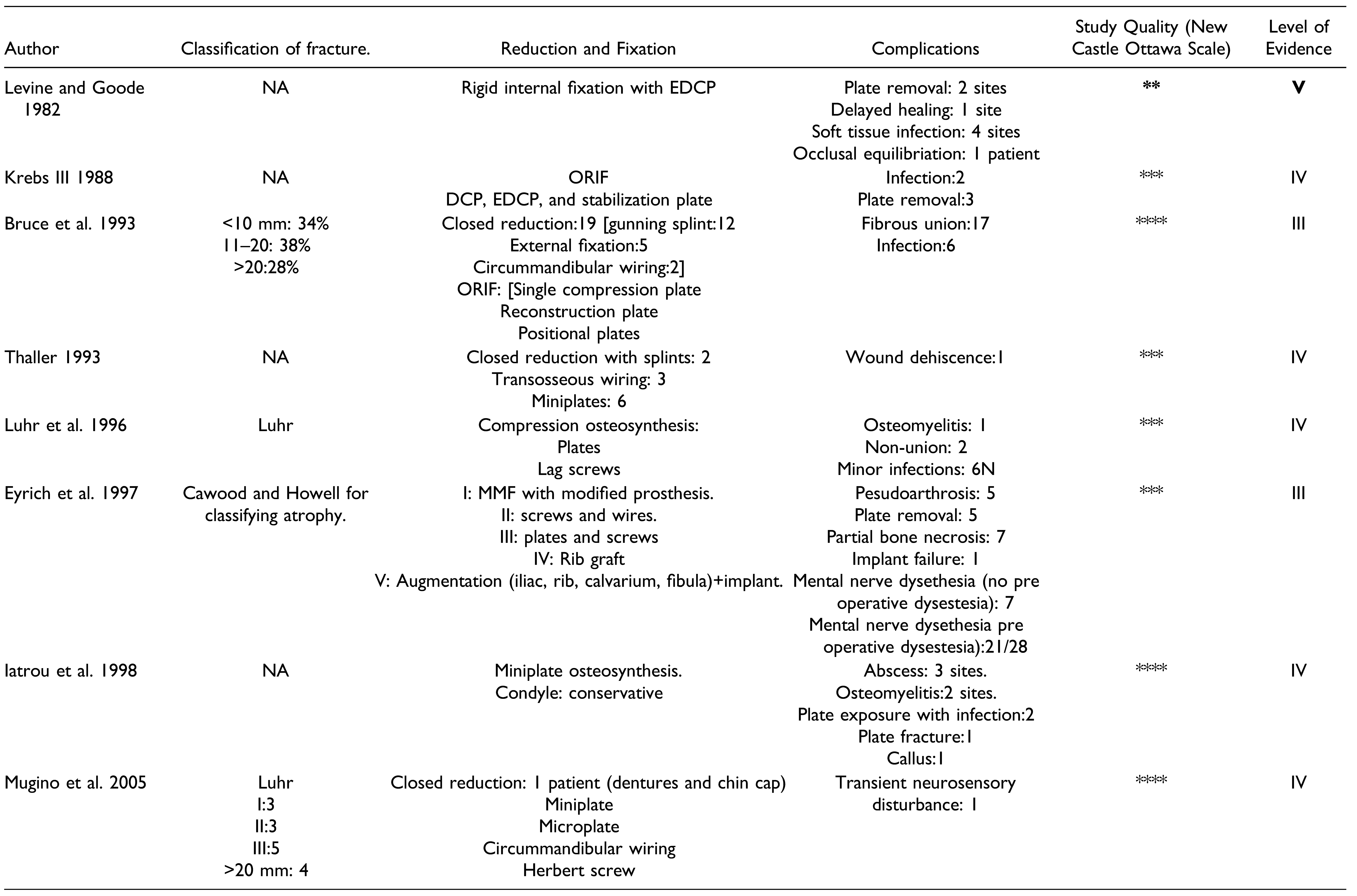
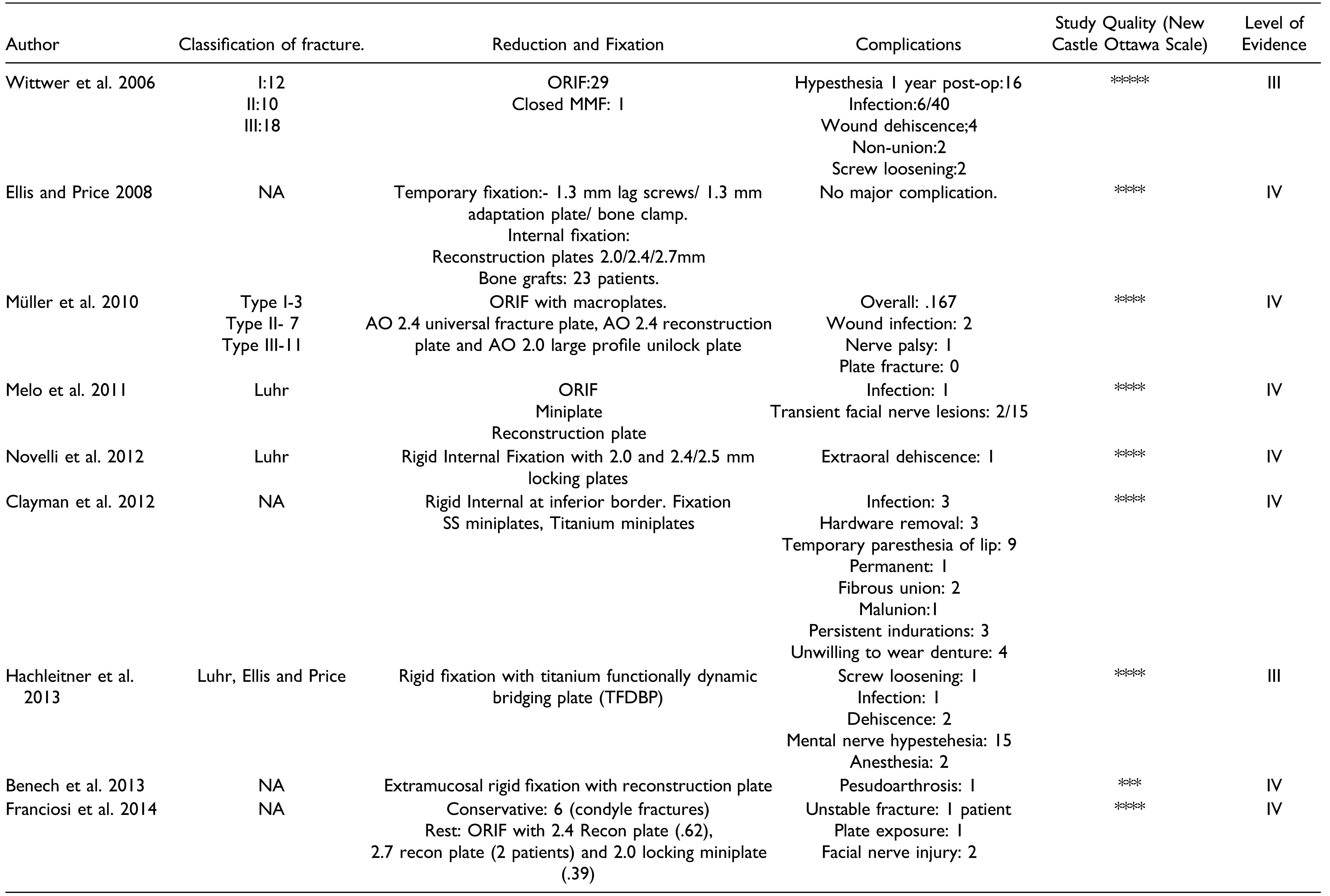
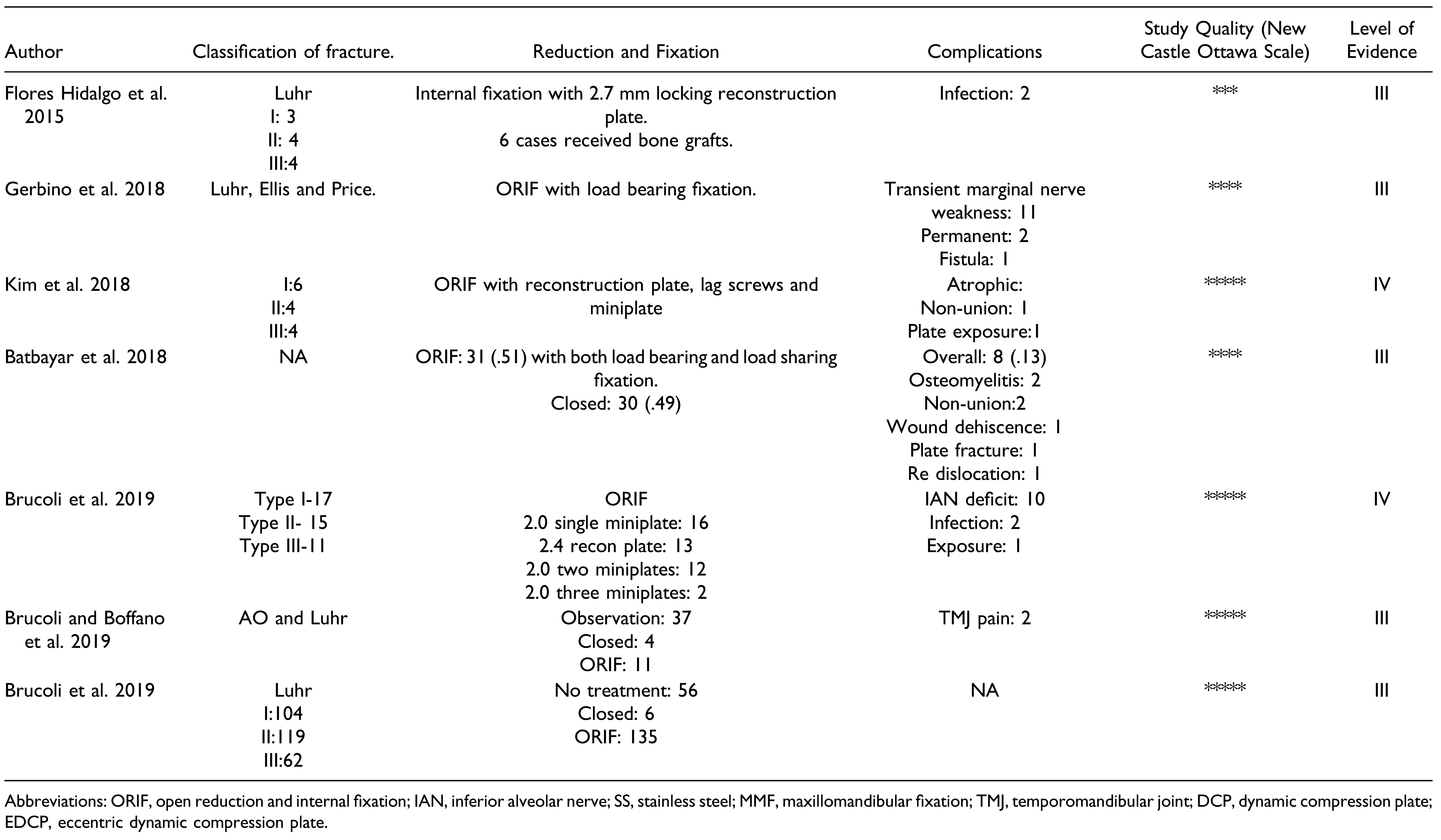
Results
Discussion
Key Results
Limitations
- None of the studies are clinical trials and hence the level of evidence is poor to suggest any definitive treatment.
- Except one study by Kim et al., all are non-comparative studies. A true comparison of outcome could not be drawn in relation to fractures of the dentate mandible.
- There is poor evidence regarding the management of condylar fractures.
- None of the studies have actually measured neurosensory outcomes. The measurements are subjective and may have bias.
- There is a lack of proper guideline or protocol to manage these fractures as being considered as a limitation in a number of included studies.
- Very limited data on the influence of age, sex, and systemic illness on outcomes.
- Inadequate data on management of post operative complications and its relationship with study variables.
Interpretation
- Bone loss/bone defects (continuity defects) [Mugino et al., Melo et al., Franciosi et al., Hidalgo et al., and Gerbino et al.).
- Comminuted and complicated fractures [Müller et al., Eyrich et al., Melo et al., and Franciosi et al.].
- Severe atrophy (Luhr III, Cawood and Howell class VI) [Eyrich et al., Mugino et al., Luhr et al., Wittwer et al., and Müller et al.]
- Partial bony defect resulting from removal of impacted teeth [Luhr et al.]
- Treatment of non-consolidated fractures [Melo et al.].
- Pathological Fractures [Eyrich et al.]
- Dental Implant based rehabilitation [Melo et al., Franciosi et al., and Hidalgo et al.]
- “What is the ideal modality of treatment for the edentulous fractured mandible?”
- No treatment is absolute as conclusive data from clinical trials are lacking. In general, the trend has shifted towards ORIF with load bearing as well as load sharing fixation. With miniplates at least two miniplates are required. Greater the atrophy, larger should be the plate. Most of the authors, however, preferred reconstruction plates. In case of condylar fractures, high condylar fractures and undisplaced fractures can be effectively managed conservatively. Displaced fractures and low-end fractures should be managed with ORIF.
- “Do they require bone grafting?”
- Bone grafting is required in cases with severe atrophy, where the residual height is less than 1 cm. It is also required in cases with continuity defects and for vertical augmentation foe implant-based rehabilitation
- “What are the complications and what has been the trend from past to present?”
Conclusion and Clinical Relevance
Funding
Declaration of Conflicting Interests
IRB statement
Supplemental Material
References
- Brucoli, M.; Boffano, P.; Romeo, I.; et al. The epidemiology of edentulous atrophic mandibular fractures in Europe. J Cranio-Maxillo-Fac Surg. 2019, 47, 1929–1934. [Google Scholar]
- Thoma, K.H. Progressive atrophy of the mandible complicated by fractures: its reconstruction. Oral Surg Oral Med Oral Pathol. 1960, 13, 4–11. [Google Scholar] [CrossRef]
- Thoma, K.H.; Holland, D.J. Atrophy of the mandible. Oral Surg Oral Med Oral Pathol. 1951, 4, 1477–1495. [Google Scholar]
- Madsen, M.J.; Haug, R.H.; Christensen, B.S.; Aldridge, E. Management of atrophic mandible fractures. Oral Maxillofac Surg Clin North Am. 2009, 21, 175–183. [Google Scholar]
- Welsh, L.W.; Welsh, J.J. Fractures of the edentulous maxilla and mandible. Laryngoscope. 1976, 86, 1333–1341. [Google Scholar]
- Marciani, R.D. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001, 59, 792–795. [Google Scholar]
- Nasser, M.; Fedorowicz, Z.; Ebadifar, A. Management of the fractured edentulous atrophic mandible. Cochrane Database Syst Rev. 2007, 1, CD006087 Update in: Cochrane Database Syst Rev 2013, 7:CD006087. [Google Scholar]
- Krebs, F.J. , 3rd. Dynamic compression plating in treatment of the fractured, edentulous mandible. Laryngoscope. 1988, 98, 198–201. [Google Scholar]
- Levine, P.A.; Goode, R.L. Treatment of fractures of the edentulous mandible. Arch Otolaryngol. 1982, 108, 167–173. [Google Scholar]
- Bruce, R.A.; Ellis E 3rd The second Chalmers, J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993, 51, 904–911. [Google Scholar] [PubMed]
- Luhr, H.G.; Reidick, T.; Merten, H.A. Results of treatment of fractures of the atrophic edentulous mandible by compression plating: a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996, 54, 250–254; discussion 254. [Google Scholar]
- Thaller, S.R. Fractures of the edentulous mandible: a retrospective review. J Craniofac Surg. 1993, 4, 91–94. [Google Scholar]
- Gerbino, G.; Cocis, S.; Roccia, F.; et al. Management of atrophic mandibular fractures: an Italian multicentric retrospective study. J Cranio-Maxillo-Fac Surg. 2018, 46, 2176–2181. [Google Scholar]
- Melo, A.R.; de Aguiar Soares Carneiro, S.C.; Leal, J.L.; Vasconcelos, B.C. Fracture of the atrophic mandible: case series and critical review. J Oral Maxillofac Surg. 2011, 69, 1430–1435. [Google Scholar]
- Novelli, G.; Sconza, C.; Ardito, E.; Bozzetti, A. Surgical treatment of the atrophic mandibular fractures by locked plates systems: our experience and a literature review. Craniomaxillofac Trauma Reconstr. 2012, 5, 65–74. [Google Scholar]
- Clayman, L.; Rossi, E. Fixation of atrophic edentulous mandible fractures by bone plating at the inferior border. J Oral Maxillofac Surg. 2012, 70, 883–889. [Google Scholar]
- Franciosi, E.; Mazzaro, E.; Larranaga, J.; et al. Treatment of edentulous mandibular fractures with rigid internal fixation: case series and literature review. Craniomaxillofac Trauma Reconstr. 2014, 7, 35–42. [Google Scholar]
- Kim, T.G.; Chung, K.J.; Lee, J.H.; Kim, Y.H.; Lee, J.H. Clinical outcomes between atrophic and nonatrophic mandibular fracture in elderly patients. J Craniofac Surg. 2018, 29, e815–e818. [Google Scholar]
- Brucoli, M.; Boffano, P.; Romeo, I.; et al. Surgical management of unilateral body fractures of the edentulous atrophic mandible. Oral Maxillofac Surg. 2020, 24, 65–71. [Google Scholar]
- Brucoli, M.; Boffano, P.; Romeo, I.; et, al. Management of mandibular condylar fractures in patients with atrophic edentulous mandibles. J Stomatol Oral Maxillofac Surg. 2020, 121, 226–232. [Google Scholar]
- Batbayar, E.O.; Bos, R.R.M.; van Minnen, B. A treatment protocol for fractures of the edentulous mandible. J Oral Maxillofac Surg. 2018, 76, 2151–2160. [Google Scholar] [CrossRef] [PubMed]
- Tiwana, P.S.; Abraham, M.S.; Kushner, G.M.; Alpert, B. Management of atrophic edentulous mandibular fractures: the case for primary reconstruction with immediate bone grafting. J Oral Maxillofac Surg. 2009, 67, 882–887. [Google Scholar] [CrossRef]
- Nasser, M.; Pandis, N.; Fleming, P.S.; et al. Interventions for the management of mandibular fractures. Cochrane Database Syst Rev 2013, 7, CD006087. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020, 368, l6890. [Google Scholar] [CrossRef]
- Eriksen, M.B.; Frandsen, T.F. The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J Med Libr Assoc. 2018, 106, 420–431. [Google Scholar] [CrossRef]
- OCEBM Levels of Evidence Working Group. Oxford Centre for Evidence-Based Medicine. The Oxford 2011 levels of evidence. 2011. Revised. http://www.cebm.net/ocebm-levelsof-evidence/ (Accessed 1 May 2016).
- Howick, J.; Chalmers, I.; Glasziou, P.; et al. “Explanation of the 2011 Oxford Centre for Evidence-Based Medicine (OCEBM) Levels of Evidence (Background Document)”. Available from: https://www.cebm.ox.ac.uk/resources/levels-ofevidence/ocebm-levels-of-evidence.
- Eyrich, G.K.; Gra¨tz, K.W.; Sailer, H.F. Surgical treatment of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1997, 55, 1081–1087, discussion 1087-8. [Google Scholar] [CrossRef]
- Mugino, H.; Takagi, S.; Oya, R.; Nakamura, S.; Ikemura, K. Miniplate osteosynthesis of fractures of the edentulous mandible. Clin Oral Investig. 2005, 9, 266–270. [Google Scholar] [CrossRef]
- Wittwer, G.; Adeyemo, W.L.; Turhani, D.; Ploder, O. Treatment of atrophic mandibular fractures based on the degree of atrophy--experience with different plating systems: a retrospective study. J Oral Maxillofac Surg. 2006, 64, 230–234. [Google Scholar] [CrossRef]
- Ellis, E., 3rd; Price, C. Treatment protocol for fractures of the atrophic mandible. J Oral Maxillofac Surg. 2008, 66, 421–435. [Google Scholar]
- Müller, S.; Bürgers, R.; Ehrenfeld, M.; Gosau, M. Macroplate fixation of fractures of the edentulous atrophic mandible: immediate function and masticatory rehabilitation. Clin Oral Investig. 2011, 15, 151–156. [Google Scholar] [CrossRef]
- Hachleitner, J.; Enzinger, S.; Brandtner, C.; Gaggl, A. The role of the titanium functionally dynamic bridging plate for the treatment of the atrophic mandible fractures. J CranioMaxillo-Fac Surg. 2014, 42, 438–442. [Google Scholar]
- Benech, A.; Nicolotti, M.; Brucoli, M.; Arcuri, F. Intraoral extramucosal fixation of fractures in the atrophic edentulous mandible. Int J Oral Maxillofac Surg. 2013, 42, 460–463. [Google Scholar] [CrossRef]
- Flores-Hidalgo, A.; Altay, M.A.; Atencio, I.C.; et al. Management of fractures of the atrophic mandible: a case series. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015, 119, 619–627. [Google Scholar]
- Madsen, M.J.; Haug, R.H. A biomechanical comparison of 2 techniques for reconstructing atrophic edentulous mandible fractures. J Oral Maxillofac Surg. 2006, 64, 457–465. [Google Scholar]

 |
 |
 |
 |
 |
 |
 |
 |
© 2025 by the authors. Published by MDPI on behalf of the AO Foundation. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bera, R.N.; Tiwari, P. Current Evidence for the Management of Edentulous Atrophic Mandible Fractures: A PRISMA-SWiM Guided Review. Craniomaxillofac. Trauma Reconstr. 2023, 16, 317-332. https://doi.org/10.1177/19433875221115585
Bera RN, Tiwari P. Current Evidence for the Management of Edentulous Atrophic Mandible Fractures: A PRISMA-SWiM Guided Review. Craniomaxillofacial Trauma & Reconstruction. 2023; 16(4):317-332. https://doi.org/10.1177/19433875221115585
Chicago/Turabian StyleBera, Rathindra N., and Preeti Tiwari. 2023. "Current Evidence for the Management of Edentulous Atrophic Mandible Fractures: A PRISMA-SWiM Guided Review" Craniomaxillofacial Trauma & Reconstruction 16, no. 4: 317-332. https://doi.org/10.1177/19433875221115585
APA StyleBera, R. N., & Tiwari, P. (2023). Current Evidence for the Management of Edentulous Atrophic Mandible Fractures: A PRISMA-SWiM Guided Review. Craniomaxillofacial Trauma & Reconstruction, 16(4), 317-332. https://doi.org/10.1177/19433875221115585




