Abstract
The main objective of this study was to provide an overview of the current practice for transverse mandibular and maxillary discrepancies in the Netherlands using a web-based survey. Orthodontists (ORTHO) and Oral and Maxillofacial Surgeons (OMFS) in the Netherlands were invited to the web-based survey via their professional association. Three cases were presented which could be treated non-surgically and surgically. Participants were asked what treatment they preferred: no treatment, orthodontic treatment with optional extractions or surgically assisted orthodontic treatment. The web-based survey ended with questions on various technical aspects and any experienced complication. Invitation was sent to all 303 members of professional association for ORTHO and to all 379 members of professional association for OMFS. Overall response number was 276 (response rate of 40.5%), including 127 incomplete responses. Generally, ORTHO prefer orthodontic treatment with optional extractions and OMFS lean towards surgically assisted orthodontic treatment. Mandibular Midline Distraction appears to be less preferred, possibly due to lack of clinical experience or knowledge by both professions despite being proven clinical stable surgical technique with stable long-term outcomes. There seems to be consensus on technical aspects by both professions, however, there are various thoughts on duration of consolidation period. Complications are mostly minor and manageable.
Introduction
Historically, transverse mandibular and maxillary discrepancies were managed with orthodontic dental expansion and/or dental extraction therapy. Changes in arch dimensions by dental expansion result in unstable post-treatment results. The mandibular symphysis closes at 1 year of age,[1,2] which makes expansion without surgery impossible. The midpalatal suture can be expanded with orthodontic treatment until approximately the age of 15.[3] With the introduction of distraction osteogenesis for the facial skeleton in 1990, new treatment options became possible.[4,5] Both osteogenesis and histogenesis are induced with this technique.
Mandibular midline distraction (MMD) is a proven surgical technique to widen the mandible in order to solve transverse mandibular discrepancies with stable long-term outcomes.[6,7] In conjunction with an osteotomy in the midline of the mandible a distractor is attached on both sides of the osteotomy, after which the skeletal dental base can be expanded by distraction osteogenesis. General indications for MMD are V-shape of the mandible, anterior or posterior crowding, uni- and bilateral crossbite and impacted anterior teeth with inadequate space and tipped teeth.[5,8,9,10] For maxillary transverse discrepancies, surgically assisted rapid maxillary expansion (SARME) is a widely applied stable technique.[11,12] Clinically, indications for SARME include anterior or posterior crowding, uni- and bilateral crossbite, black buccal corridors, buccal tipping of the maxillary molars and lingual tipping of the mandibular molars.[11,12,13]
There are various types of distractors available such as tooth-borne, bone-borne or a combination of both (hybrid). Following surgery, generally a latency period is respected to create soft callus formation before starting with distraction. In contrast to distraction technique for the long bones,[14] there is no standardized protocol for MMD and SARME. In the literature, there are many variable factors like the clinical indication, anesthesia technique, osteotomy technique (MMD: vertical or step, SARME: surgical transections), latency period, distractor type, distraction rate, overcorrection and consolidation period.
The main objective of this study was to provide an overview of the current practice for transverse mandibular and maxillary discrepancies in the Netherlands using a webbased survey. Orthodontists and Oral and Maxillofacial Surgeons can use this information to align and improve the treatment modalities for transverse mandibular and maxillary discrepancies and inform their patients better about the possible treatment options.
Materials and Methods
Orthodontists and Oral and Maxillofacial surgeons in the Netherlands were invited per mail to participate anonymously in this web-based survey after approval had been obtained from the Medical Ethics Committee of Erasmus MC, University Medical Center Rotterdam, the Netherlands (approval number: MEC-2020-0459). This was provided by using the professional associations for Orthodontists (“Nederlandse Vereniging van Orthodontisten,” NVvO) and for Oral and Maxillofacial Surgeons (“Nederlandse Vereniging voor Mondziekten, Kaak- en Aangezichtschirurgie,” NVMKA). To maximize the response rate, the invitation to participate was sent twice to the same mail list by both professional associations and the web-based survey was built with tick box answers.
In this web-based survey participants were asked what specialism they practice, what their place of training was, how many years of experience they have and if they are practicing in a training clinic.
Three cases were presented clinical and radiographic with transverse mandibular and maxillary discrepancies that can be treated both non-surgically and surgically (Online Supplemental Appendices I, II, and III).
Case 1 was a 16-years old woman, case 2 a 44-years old man and case 3 a 43-years old man. The patients’ chief complaint was explicitly not mentioned in order to disclose an unbiased treatment planning decision.
All 3 presented patients had given prior written consent for the use of their visual material for this web-based survey and publication in a scientific journal.
Participants were asked what treatment they prefer with the following answer options:
- -
- No treatment.
- -
- Orthodontic treatment with optional extractions:Without premolar extractions in the lower and upper jaw, only orthodontic alignment of both dental arches.
- ○
- With premolar extractions only in the lower jaw, followed by orthodontic alignment of both dental arches.
- ○
- With premolar extractions only in the upper jaw, followed by orthodontic alignment of both dental arches.
- ○
- With premolar extractions in both the lower and upper jaw, followed by orthodontic alignment of both dental arches.
- -
- Surgically assisted orthodontic treatment:
- ○
- Surgically assisted expansion of the lower jaw only with distraction osteogenesis, followed by orthodontic alignment of both dental arches.
- ○
- Surgically assisted expansion of the maxilla only with distraction osteogenesis, followed by orthodontic alignment of both dental arches.
- ○
- Surgically assisted expansion of both the lower and upper jaw with distraction osteogenesis followed by orthodontic alignment of both dental arches.
After giving the preference of treatment, our applied treatment(s) were shown for each case separately. Case 1 was treated with surgically assisted orthodontic treatment: with MMD using a bone-borne (Rotterdam Mandibular) distractor and with SARME using a Hyrax distractor. Case 2 was treated with surgically assisted orthodontic treatment: with MMD using a tooth-borne distractor and with SARME using a Haas distractor. Case 3 was treated with orthodontic treatment with premolar extractions in both the lower and upper jaw followed by orthodontic alignment of both dental arches.
In addition, participants were asked if they were satisfied with our applied treatment by using a score scale (1 = very dissatisfied and 5 = very satisfied) and whether they will recommend (again) the applied treatment in the future for the same indication.
The web-based survey ended with questions on various technical aspects concerning the number of surgically assisted orthodontic treatment performed, preference of distractor type, latency period, distraction rate, overcorrection, consolidation period, orofacial soft tissue effects and any experienced complication.
All the obtained data were stored automatically and anonymously in LimeSurvey GmbH, version 2.06lts Build 160524, which is provided by the local Erasmus MC server.
Statistical Analysis
Descriptive statistics are used to characterize the study population. Means are presented for data that followed a normal distribution and medians if the data followed a nonnormal distribution. The presented proportions are based on the number of valid cases.
For data handling and analyses, the Statistical Package of Social Sciences version 25.0 for Windows (IBM Corp, Armonk, NY, USA) was used. The graphical figures were made by exporting the data to Microsoft Excel 2016 for Windows version 16.0 (Microsoft, Redmond, WA, USA). In reporting of this study the STROBE guidelines were followed.[15]
Results
This web-based survey was sent per mail twice to all 303 members of the NVvO (Orthodontists, ORTHO) and to all 379 members of the NVMKA (Oral and Maxillofacial Surgeons, OMFS). There was an overall response number of 276 (response rate of 40.5%), including 127 incomplete responses. See Table 1 and Figure 1, Figure 2, and Figure 3 for a complete overview of the responses and results per case.

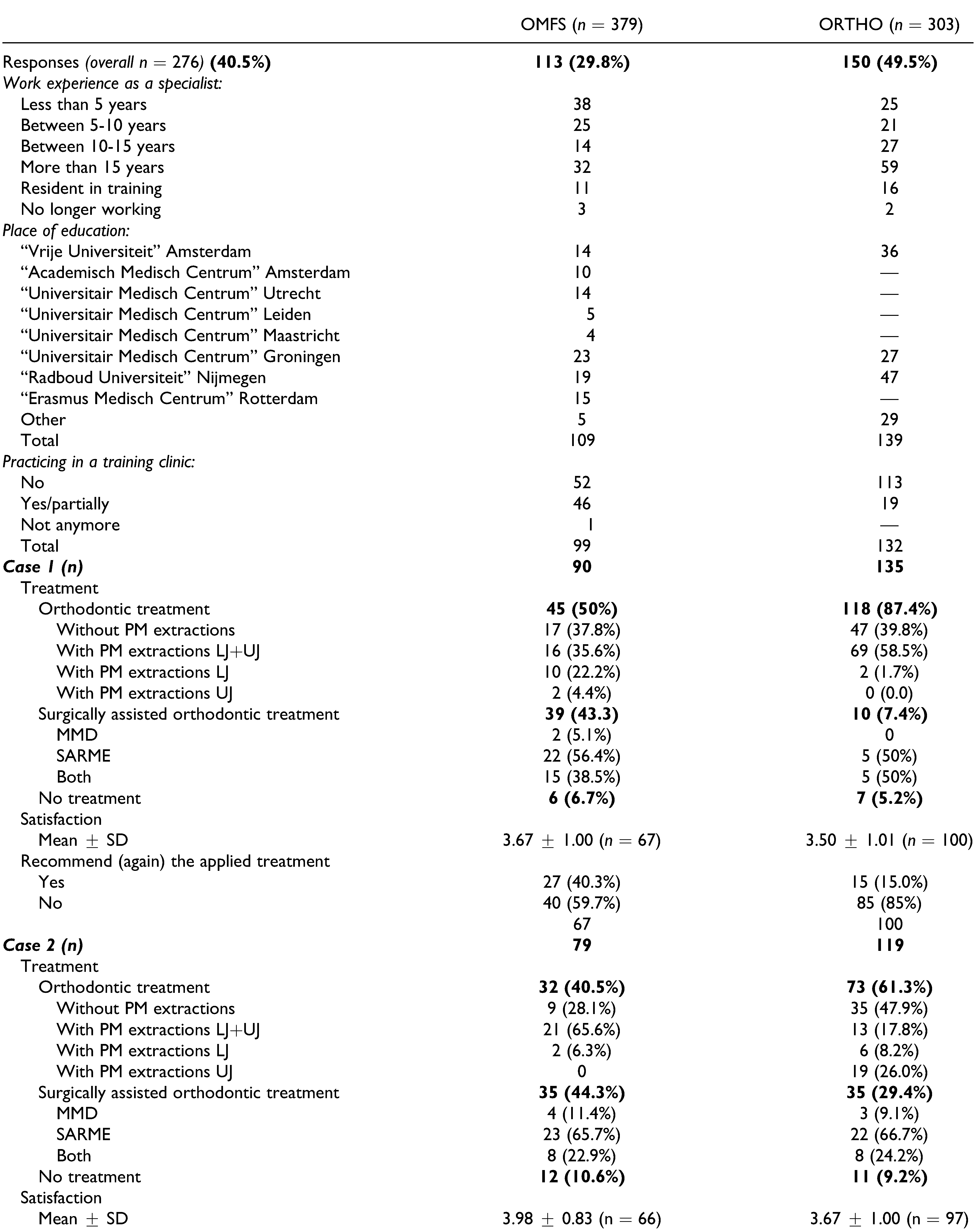
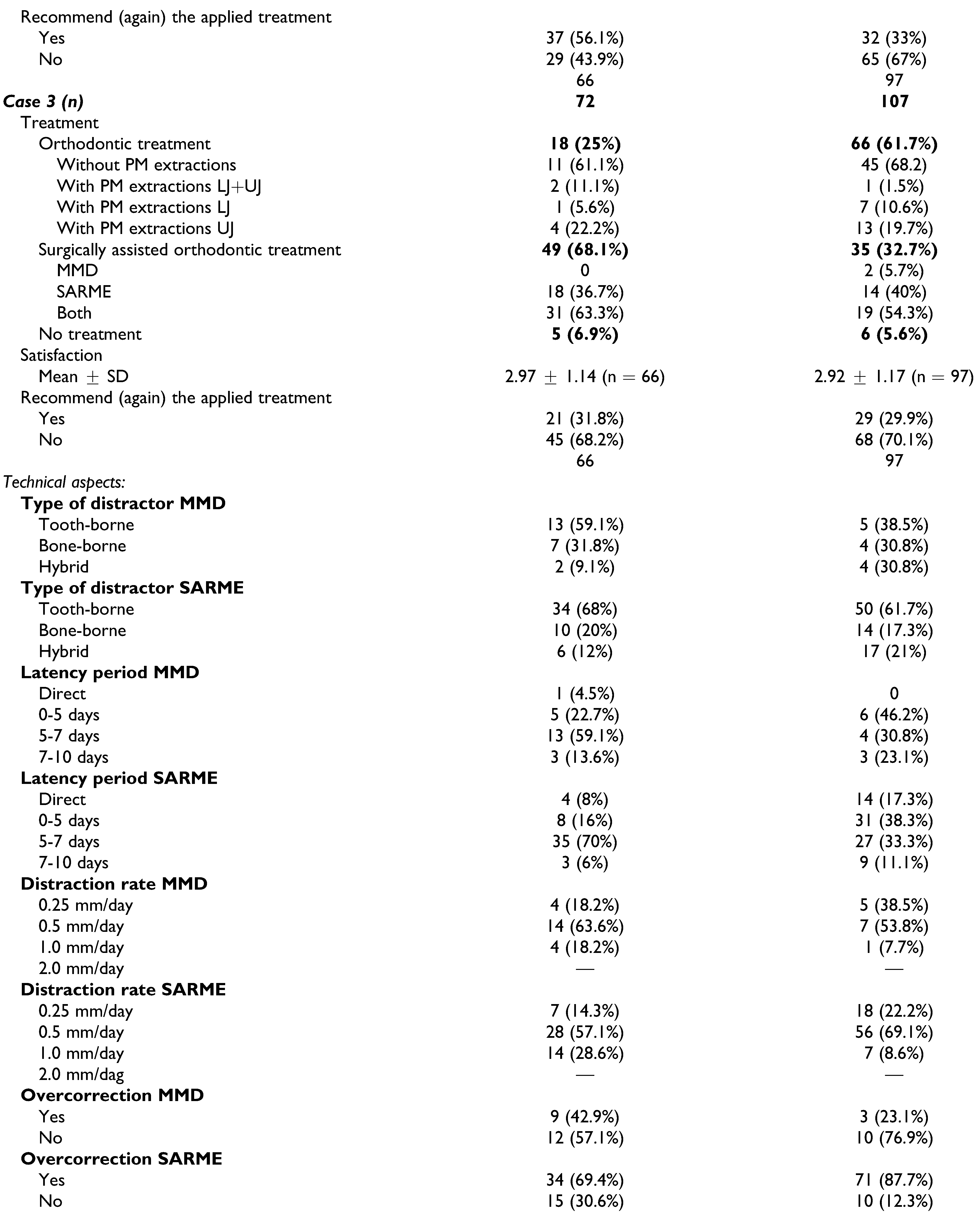
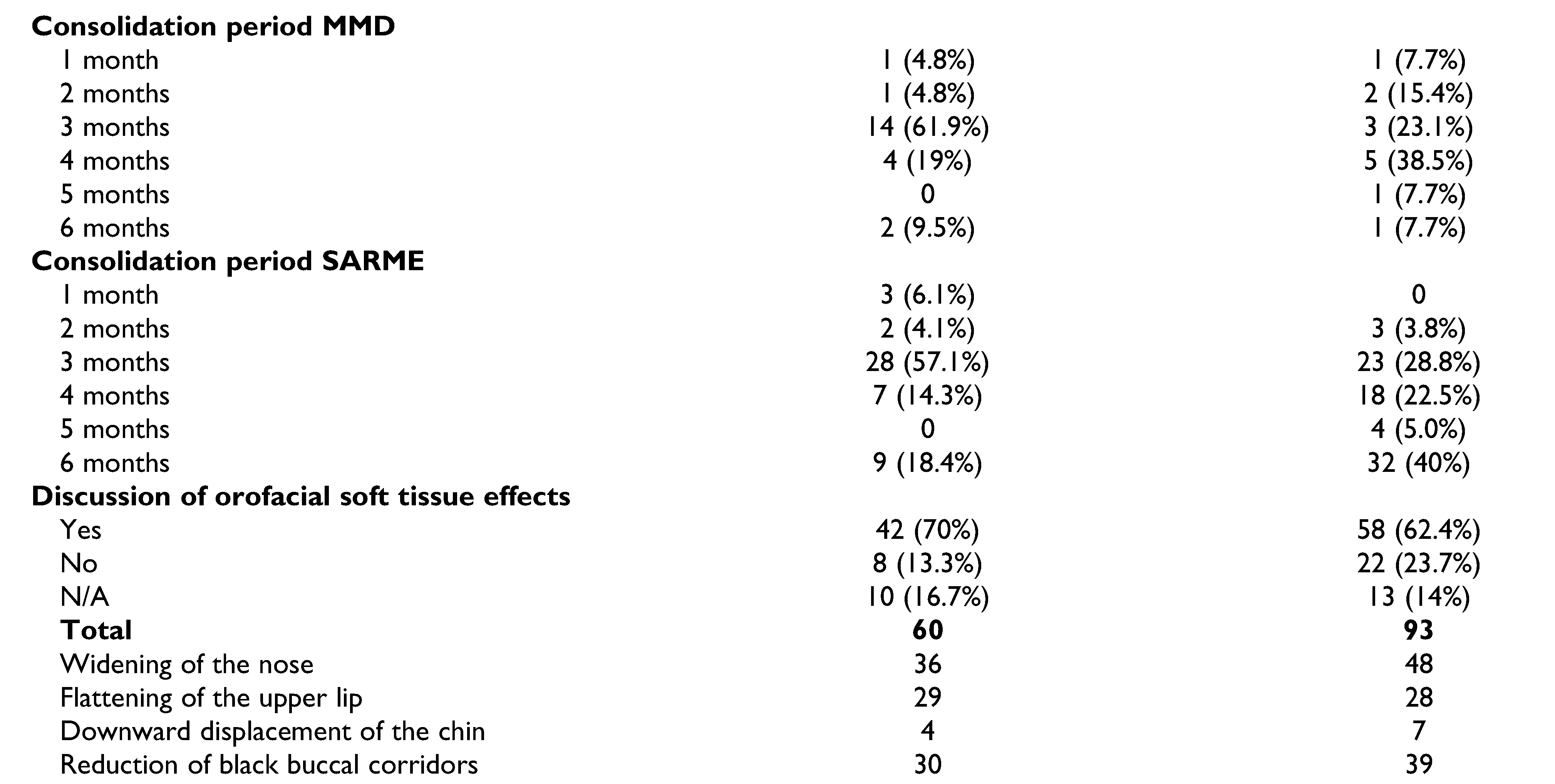
Table 1.
Complete Overview of the Responses and Results Per Case.
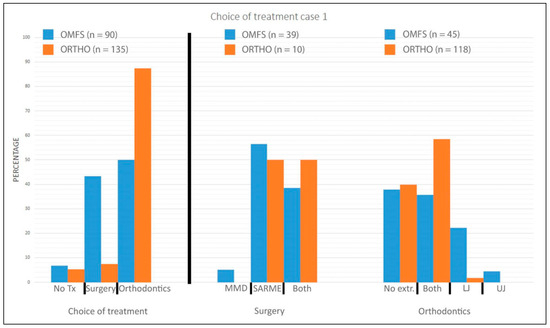
Figure 1.
Choice of treatment case 1. LJ indicates premolar extractions in lower jaw; MMD, mandibular midline distraction; OMFS, oral and maxillofacial surgeons; ORTHO, orthodontists; SARME, surgically assisted rapid maxillary expansion; Tx, treatment; UJ, premolar extractions in upper jaw.
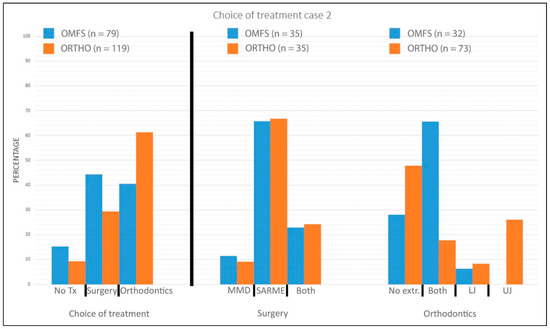
Figure 2.
Choice of treatment case 2. LJ indicates premolar extractions in lower jaw; MMD, mandibular midline distraction; OMFS, oral and maxillofacial surgeons; ORTHO, orthodontists; SARME, surgically assisted rapid maxillary expansion; Tx, treatment; UJ, premolar extractions in upper jaw.
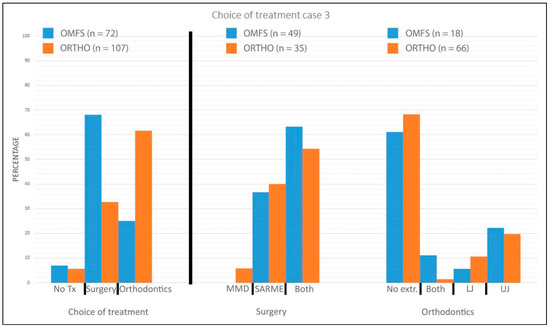
Figure 3.
Choice of treatment case 3. LJ indicates premolar extractions in lower jaw; MMD, mandibular midline distraction; OMFS, oral and maxillofacial surgeons; ORTHO, orthodontists; SARME, surgically assisted rapid maxillary expansion; Tx, treatment; UJ, premolar extractions in upper jaw.
Case 1
Case 1 was filled out completely by 135 ORTHO members (response rate of 44.6%), of which 118 members had chosen for orthodontic treatment with optional extractions, 10 members for surgically assisted orthodontic treatment (MMD, 0; SARME, 5; MMD and SARME, 5) and 7 members for no treatment. The mean score scale of satisfaction for our applied treatment was 3.5 ± 1.01 (n = 100), of which only 15 members (15.0%) would choose our applied treatment again.
On the other hand, 90 OMFS members (response rate of 23.7%) filled out completely, of which 45 members had chosen for orthodontic treatment with optional extractions, 39 members for surgically assisted orthodontic treatment (MMD, 2; SARME, 22; MMD and SARME, 15) and 6 members for no treatment. The mean score scale of satisfaction for our applied treatment was 3.67 ± 1.00 (n = 67), of which 27 members (40.3%) would choose our applied treatment again.
Case 2
Case 2 was filled out completely by 119 ORTHO members (response rate of 39.3%), of which 73 members had chosen for orthodontic treatment with optional extractions, 35 members for surgically assisted orthodontic treatment (MMD, 3; SARME, 22; MMD and SARME, 8) and 11 members for no treatment. The mean score scale of satisfaction for our applied treatment was 3.67 ± 1.00 (n = 97), of which 32 members (33%) would choose our applied treatment again.
Seventy-nine OMFS members (response rate of 20.8%) filled out completely the same case. Out of this 32 members had chosen for orthodontic treatment with optional extractions, 35 members for surgically assisted orthodontic treatment (MMD, 4; SARME, 23; MMD and SARME, 8) and 12 members for no treatment. The mean score scale of satisfaction for our applied treatment was 3.98 ± 0.83 (n = 66), of which 37 members (56.1%) would choose our applied treatment again.
Case 3
Case 3 was filled out completely by 107 ORTHO members (response rate of 35.3%), of which 66 members had chosen for orthodontic treatment with optional extractions, 35 members for surgically assisted orthodontic treatment (MMD, 2; SARME, 14; MMD and SARME, 19) and 6 members for no treatment. The mean score scale of satisfaction for our applied treatment was 2.92 ± 1.17 (n = 97), of which 29 members (29.9%) would choose our applied treatment again.
Finally, 72 OMFS members (response rate of 19%) filled out the same case completely, of which 18 members had chosen for orthodontic treatment with optional extractions, 49 members for surgically assisted orthodontic treatment (MMD, 0; SARME, 18; MMD and SARME, 31) and 5 members for no treatment. The mean score scale of satisfaction for our applied treatment was 2.97 ± 1.14 (n = 66), of which 21 members (31.8%) would choose our applied treatment again.
Technical Aspects
See Table 1 for a complete overview of the results per technical aspect. Ninety-three ORTHO members (response rate of 30.7%) have performed at least 1 MMD and/or SARME annually. The general preference of distractor type was the tooth-borne distractor combined with a latency period of 0-5 days where after a distraction rate of 0.5 mm/day was applied generally for both MMD and SARME. In contrast to SARME, generally no overcorrection of distraction is preferred for the MMD. Generally, after active distraction, a consolidation period of 4 months for MMD and 6 months for SARME is preferred. In general, before start of MMD and/or SARME possible orofacial soft tissue effects (widening of the nose, flattening of the upper lip, downward displacement of the chin and reduction of black buccal corridors) are discussed with the patients by 62.4% of the same 93 ORTHO members.
On the other hand, 60 OMFS members (response rate of 15.8%) have performed at least 1 MMD and/or SARME annually. The general preference of distractor type was the tooth-borne distractor combined with a latency period of 5-7 days where after a distraction rate of 0.5 mm/day was applied generally for both MMD and SARME. During distraction generally no overcorrection is preferred for the MMD, but for SARME it is. After distraction generally a consolidation period of 3 months for both MMD and SARME is preferred. In general, before start of MMD and/or SARME possible orofacial soft tissue effects (widening of the nose, flattening of the upper lip, downward displacement of the chin and reduction of black buccal corridors) are discussed with the patients by 70.0% of the same 60 OMFS members.
Complications
Regarding complications, by the same 93 ORTHO and 60 OMFS members, 13 complications were reported for MMD (loose distractor, 2; discomfort, 3; non-union, 2; loss of tooth, 2; loss of vitality, 2; infection, 1 and severe laceration of soft tissue, 1) and 74 complications for SARME (bleeding, 5; loss of vitality, 5; loose distractor, 5; asymmetric expansion, 33; loss of tooth, 1; deviation of nasal septum, 1; gingival and periodontal recession and/or pockets, 6; necrosis of gingiva, 1; undesired expansion, 4; broken distractor, 2; floating maxilla, 1; bad split through periodontal ligament of central incisor, 1; severe relapse, 1; damage of central incisor apex, 1; too much resistance during distraction, 1; temporary change of incisor color, 1; temporary loose incisor, 1; sinusitis, 1; discomfort, 1; ankyloses of incisor, 1 and sensibility disturbance of the upper lip, 1).
Discussion
In the orthodontic and oral and maxillofacial surgery literature, there are still a lot of controversies and a lack of consensus regarding indication for MMD and SARME, distractor type, latency period, distraction rate, overcorrection, and consolidation period for MMD and SARME. The main objective of this study was to provide an overview of the current practice for transverse mandibular and maxillary discrepancies in the Netherlands using a web-based survey about 3 specific cases. The results show that generally ORTHO prefer orthodontic treatment with optional extractions and OMFS lean towards surgically assisted orthodontic treatment. The choice for no treatment was for both specialisms broadly the same. Although the average satisfaction score per case for our applied treatments ranged between neutral and satisfied, our applied treatments seemed generally not to be preferred in the future by both specialisms. This might be related to the clinic where the clinicians were trained, but in the current survey the numbers were too low to draw any conclusions.
To our knowledge, in the literature this is the first survey regarding transverse mandibular and maxillary discrepancies with comparison from the view of ORTHO and OMFS.
MacLaine et al. has previously conducted a nationwide survey in the United Kingdom for OMFS, however this was only focused on SARME.[16] MacLaine et al. showed a general preference for a tooth-borne distractor (78%) and a general preference of 5-7 days for latency period (roughly 50%).[16] These preferences are in line with our results. However, the preference of distraction rate was 1 mm/day with a preference of overcorrection by only 23%. These preferences are not in line with our general preference of distraction rate of 0.5 mm/day and a strong preference for overcorrection.
In this study, there seems to be consensus on the technical aspects by both professions. The general preference of distractor type is the tooth-borne distractor with a distraction rate of 0.5 mm/day for both MMD and SARME by both professions. ORTHO prefer a latency period of 0-5 days where OMFS prefer 5-7 days for both MMD and SARME. Finally, the consolidation period seems to be preferred 4 months for MMD and 6 months for SARME by ORTHO, where OMFS prefer 3 months for both MMD and SARME.
Regarding complications for MMD discomfort was mentioned most often. This could be related to the design of the distractor. Bone-borne distractors are positioned in the lower mucobuccal fold close to the mucosa of the lower lip, which could lead to pressure ulcers and discomfort. Due to the position of the bone-borne distractor and saliva with food accumulation, wound healing issues could occur. A second procedure, under local anesthesia or general anesthesia, is needed to remove the distractor. Moreover, tooth-borne distractors are positioned sublingual which could interfere with the tongue position and lead to discomfort. In this web-based survey, the mentioned complications are generally in line with our previous study on complications in MMD.[17] However, the reported 2 nonunion cases are remarkable in this web-based survey.
Regarding complications for SARME, the most frequently mentioned complication was asymmetric expansion. A possible explanation for this could be the minimal invasive trend of surgery with transection of only the piriform aperture, the zygomatic buttress and the mid-palatinal suture without transection of the pterygomaxillary junction. This theory is also supported with the outcomes of Carvalho et al. in the systematic review of complications for SARME. When transection of the pterygomaxillary junction was not performed there was an increased rate of asymmetric or incorrect and undesired expansion.[18] Due to the anatomic relation, the transection between the piriform aperture and the zygomatic buttress is never completely horizontal on both sides of the median osteotomy. Due to this, expanding the maxilla may result in an asymmetric position in vertical direction. Other factors that could lead to an asymmetric expansion are broken or malfunctioning distractors.
The most cited comment on the survey itself by the participants was the lack of patients’ chief complaint per presented case. Only general information was given in order to make a clinical unbiased decision for treatment possible. However, in a clinical setting the preferences of the patient are essential to gain successful and satisfied outcomes within shared decision making. Another common cited comment was the lack of experiences with MMD and its clinical stability in the long-term. This lack of knowledge may have led to the non-surgical choice of orthodontic treatment for transverse mandibular discrepancies despite MMD is a proven surgical technique to widen the mandible with stable long-term outcomes.[6,7]
Conclusions
In the Netherlands, generally, Orthodontists prefer orthodontic treatment with optional extractions and Oral and Maxillofacial Surgeons prefer surgically assisted orthodontic treatment for transverse mandibular and maxillary discrepancies. Regarding surgically assisted orthodontic treatment, MMD seems less preferred most likely due to lack of clinical experience or knowledge by both professions despite being a proven clinical surgical technique with stable long-term outcomes. Overall, there seems to be consensus on the technical aspects by both professions, except for the duration of the consolidation period. Regarding complications, encountered in daily practice in the Netherlands, for MMD and SARME these are mostly minor and manageable. Clinicians should be aware of a possible asymmetric or incorrect and undesired expansion following SARME and communicate this prior the treatment with their patients.
Supplementary Materials
Supplemental material for this article is available online.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Acknowledgments
The authors acknowledge the NVvO, NVMKA and the 3 presented patients for the participation in this study.
Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
Ethical approval had been obtained from the Medical Ethics Committee of Erasmus MC, University Medical Center Rotterdam, the Netherlands (approval number: MEC-2020-0459).
Patient Consent
All 3 presented patients had given prior written consent for the use of their visual material for this web-based survey and publication in a scientific journal.
References
- Sperber, G.H.; Sperber, G.H.; Wald, J.; Gutterman, G.D.; Sperber, S.M. Craniofacial Development; B C Decker, 2001. [Google Scholar]
- Little, R.M. Stability and relapse of dental arch alignment. Br J Orthod. 1990, 17, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Wehrbein, H.; Yildizhan, F. The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod. 2001, 23, 105–114. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, J.G.; Schreiber, J.; Karp, N.; Thorne, C.H.; Grayson, B.H. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992, 89, 1–8, discussion 9–10. [Google Scholar] [PubMed]
- Guerrero, C.A.; Bell, W.H.; Contasti, G.I.; Rodriguez, A.M. Mandibular widening by intraoral distraction osteogenesis. Br J Oral Maxillofac Surg. 1997, 35, 383–392. [Google Scholar] [PubMed]
- King, J.W.; Wallace, J.C.; Winter, D.L.; Niculescu, J.A. Long-term skeletal and dental stability of mandibular symphyseal distraction osteogenesis with a hybrid distractor. Am J Orthod Dentofacial Orthop. 2012, 141, 60–70. [Google Scholar] [PubMed]
- de Gijt, J.P.; Gul, A.; Sutedja, H.; Wolvius, E.B.; van der Wal, K.G.; Koudstaal, M.J. Long-term (6.5 years) follow-up of mandibular midline distraction. J Craniomaxillofac Surg. 2016, 44, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Alkan, A.; Ozer, M.; Bas, B.; et al. Mandibular symphyseal distraction osteogenesis: review of three techniques. Int J Oral Maxillofac Surg. 2007, 36, 111–117. [Google Scholar] [PubMed]
- Mommaerts, M.Y. Bone anchored intraoral device for transmandibular distraction. Br J Oral Maxillofac Surg. 2001, 39, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Mommaerts, M.Y.; Polsbroek, R.; Santler, G.; Correia, P.E.; Abeloos, J.V.; Ali, N. Anterior transmandibular osteodistraction: clinical and model observations. J Craniomaxillofac Surg. 2005, 33, 318–325. [Google Scholar] [PubMed]
- de Gijt, J.P.; Gul, A.; Tjoa, S.T.; Wolvius, E.B.; van der Wal, K.G.; Koudstaal, M.J. Follow up of surgically-assisted rapid maxillary expansion after 6.5 years: skeletal and dental effects. Br J Oral Maxillofac Surg. 2017, 55, 56–60. [Google Scholar] [PubMed]
- Koudstaal, M.J.; Wolvius, E.B.; Schulten, A.J.; Hop, W.C.; van der Wal, K.G. Stability, tipping and relapse of bone-borne versus tooth-borne surgically assisted rapid maxillary expansion; a prospective randomized patient trial. Int J Oral Maxillofac Surg. 2009, 38, 308–315. [Google Scholar]
- Koudstaal, M.J.; Poort, L.J.; van der Wal, K.G.; Wolvius, E.B.; Prahl-Andersen, B.; Schulten, A.J. Surgically assisted rapid maxillary expansion (SARME): a review of the literature. Int J Oral Maxillofac Surg. 2005, 34, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Ilizarov, G.A.; Green, S.A. Transosseous Osteosynthesis: Theoretical and Clinical Aspects of the Regeneration and Growth of Tissue; Springer: Berlin/Heidelberg, 2012. [Google Scholar]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007, 147, 573–577. [Google Scholar] [CrossRef] [PubMed]
- MacLaine, J.K.; Thickett, E.M.; Power, S.M. Nationwide survey of surgically assisted rapid maxillary expansion. Br J Oral Maxillofac Surg. 2013, 51, 841–844. [Google Scholar] [PubMed]
- de Gijt, J.P.; Gul, A.; Wolvius, E.B.; van der Wal, K.G.H.; Koudstaal, M.J. Complications in mandibular midline distraction. Craniomaxillofac Trauma Reconstr. 2017, 10, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, P.H.A.; Moura, L.B.; Trento, G.S.; et al. Surgically assisted rapid maxillary expansion: a systematic review of complications. Int J Oral Maxillofac Surg. 2020, 49, 325–332. [Google Scholar] [CrossRef] [PubMed]
© 2021 by the author. The Author(s) 2021.