Biomechanical Analysis of a Custom-Made Mouthguard Reinforced With Different Elastic Modulus Laminates During a Simulated Maxillofacial Trauma
Abstract
:1. Introduction
2. Methods
2.1. Finite Element Analysis (FEA) Pre-Processing
2.2. FEA Solution
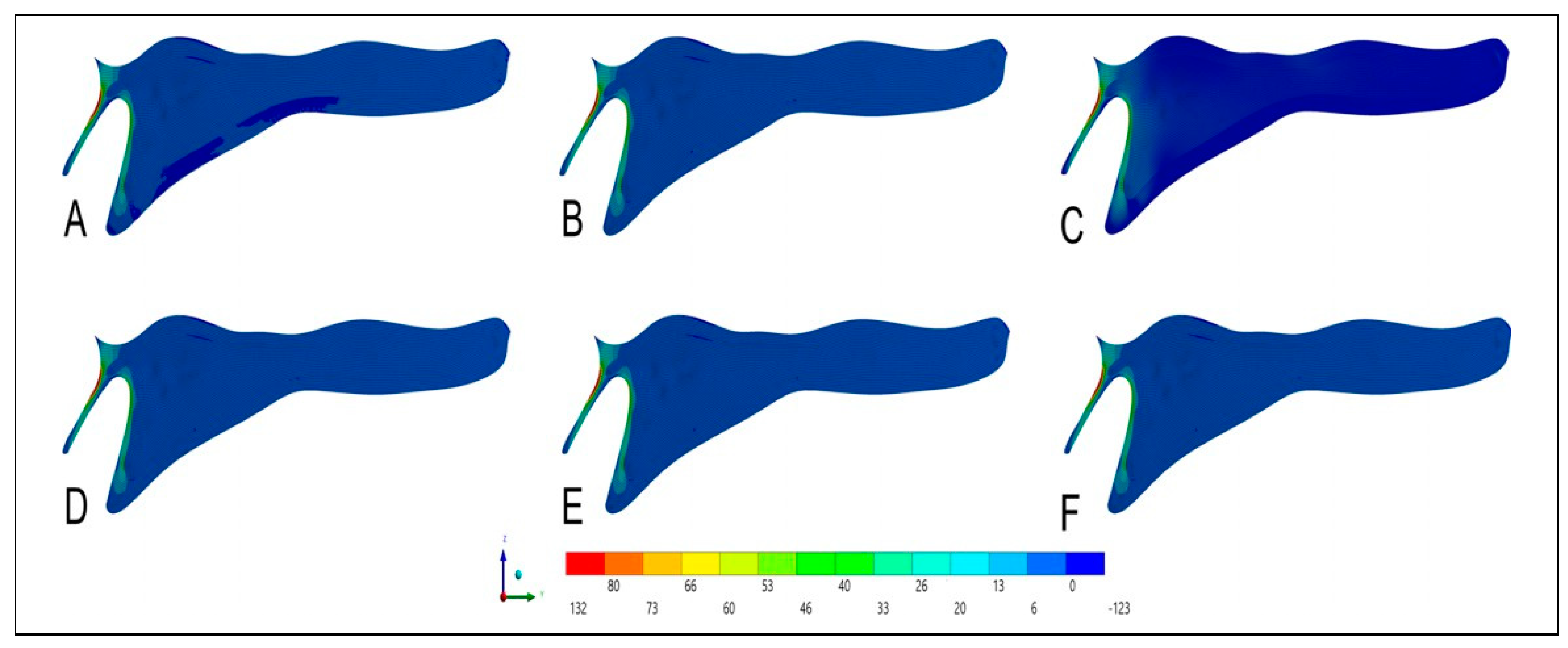
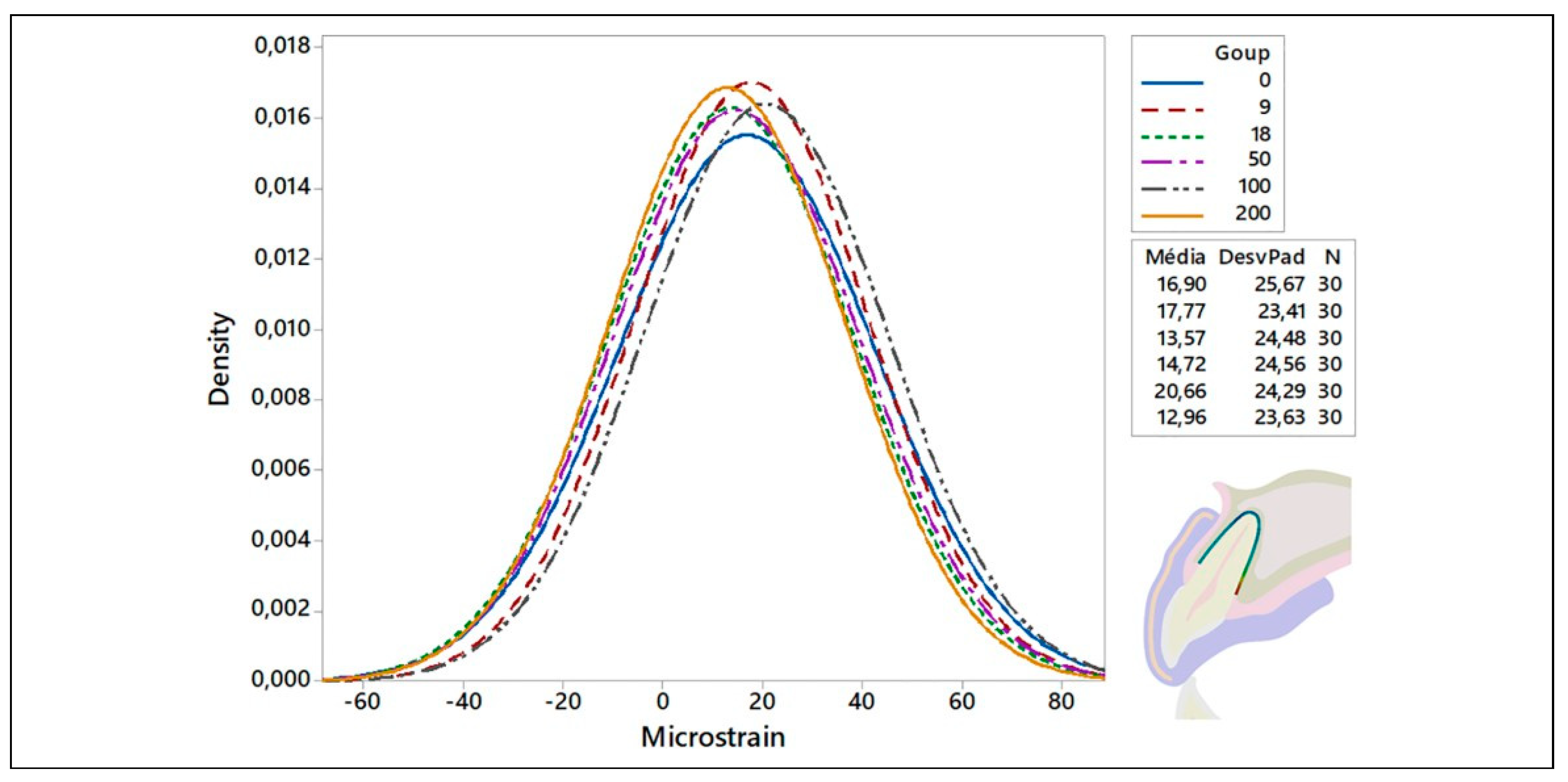
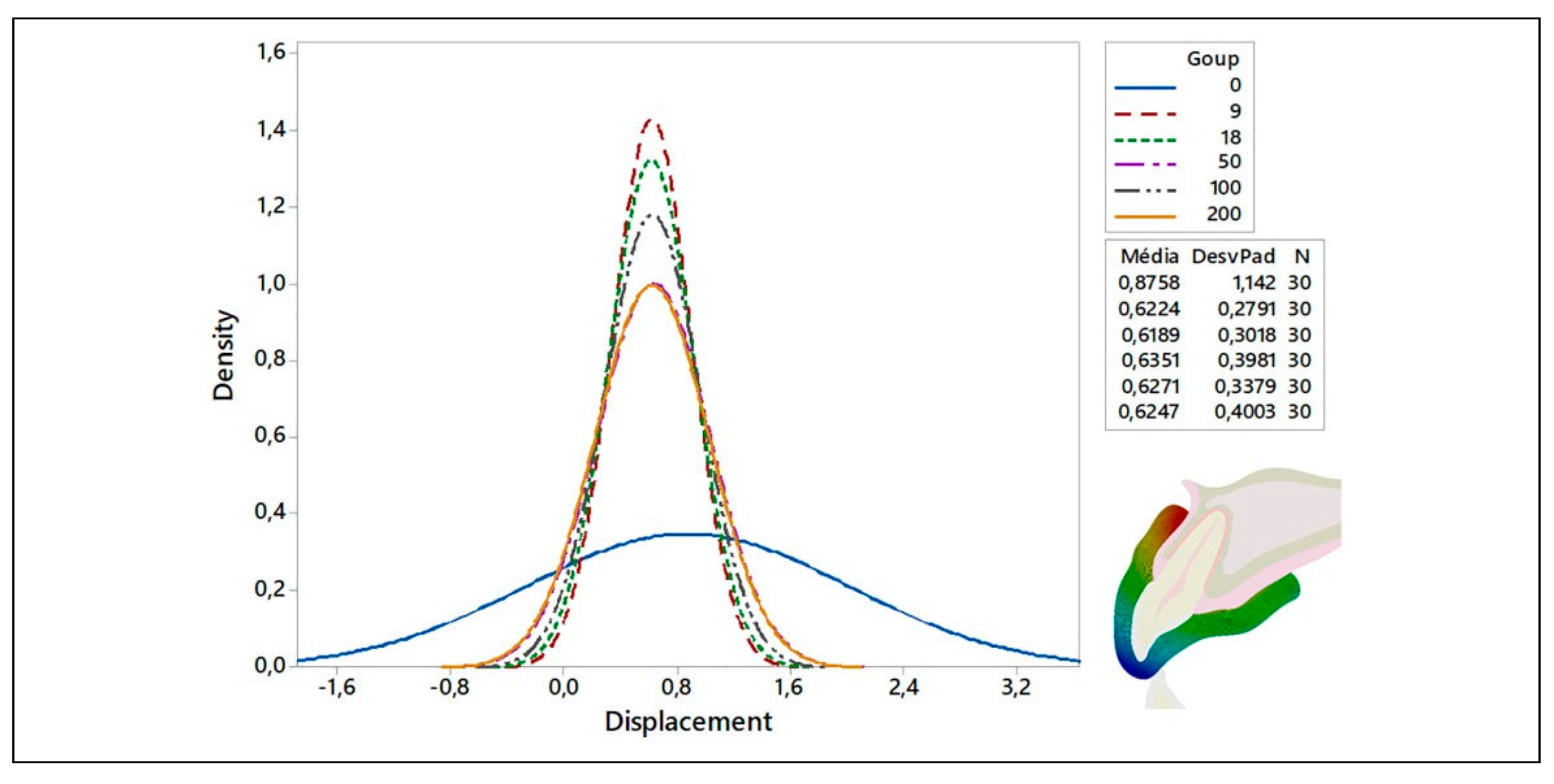
3. Results
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Bruggesser, S.; Ku¨hl, S.; Solakoglu, Ö.; Filippi, A. The prevalence of orofacial injuries in judo: A cross-sectional study. Dent. Traumatol. 2020, 36, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Allison, P.; Tamimi, F. Mouthguards should be worn in contact sports. Br. J. Sports Med. 2020, 54, 1016–1017. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Borges, A.L.S.; Bottino, M.A. Simulation of mouthguard use in preventing dental injuries caused by different impacts in sports activities. Sport. Sci. Health 2018, 15, 85–90. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; de Carvalho, P.C.K.; de Queiroz Gonc¸alves, P.H.P.; Borges, A.L.S.; de Arruda Paes-Junior, T.J. Does silica–nylon mesh improves the biomechanical response of custom-made mouthguards? Sport. Sci. Health 2019, 16, 1–10. [Google Scholar]
- DiAngelis, A.J.; Andreasen, J.O.; Ebeleseder, K.A.; Kenny, D.J.; Trope, M.; Sigurdsson, A.; Andersson, L.; Bourguignon, C.; Flores, M.T.; Hicks, M.L.; et al. International association of dental traumatology guidelines for the management of traumatic dental injuries: 1. fractures and luxations of permanent teeth. Dent. Traumatol. 2012, 28, 2–12. [Google Scholar] [PubMed]
- Tribst, J.P.M.; de Oliveira Dal Piva, A.M.; Borges, A.L.S.; Bottino, M.A. Influence of custom-made and stock mouthguard thickness on biomechanical response to a simulated impact. Dent. Traumatol. 2018, 34, 429–437. [Google Scholar]
- Takeda, T.; Ishigami, K.; Shintaro, K.; Nakajima, K.; Shimada, A.; Regner, C.W. The influence of impact object characteristics on impact force and force absorption by mouthguard material. Dent. Traumatol. 2004, 20, 12–20. [Google Scholar]
- Ver’ıssimo, C.; Bicalho, A.A.; Soares, P.B.; Tantbirojn, D.; Versluis, A.; Soares, C.J. The effect of antagonist tooth contact on the biomechanical response of custom-fitted mouthguards. Dent. Traumatol. 2017, 33, 57–63. [Google Scholar]
- Bochnig, M.S.; Oh, M.J.; Nagel, T.; Ziegler, F.; Jost-Brinkmann, P.G. Comparison of the shock absorption capacities of different mouthguards. Dent. Traumatol. 2017, 33, 205–213. [Google Scholar] [CrossRef]
- Bulsara, Y.R.; Matthew, I.R. Forces transmitted through a laminated mouthguard material with Sorbothane insert. Endod. Dent. Traumatol. 1998, 14, 45–47. [Google Scholar] [CrossRef]
- Patrick, D.; Van Noort, R.; Found, M.S. Evaluation of laminated structures for sports mouthguards. Key Eng. Mater. 2002, 221, 133–144. [Google Scholar]
- Kataoka, S.H.; Setzer, F.C.; Gondim, E., Jr.; Caldeira, C.L. Impact absorption and force dissipation of protective mouth guards with or without titanium reinforcement. J. Am. Dent. Assoc. 2014, 145, 956–959. [Google Scholar]
- Westerman, B.; Stringfellow, P.M.; Eccleston, J.A. Beneficial effects of air inclusions on the performance of ethylene vinyl acetate (EVA) mouthguard material. Br. J. Sports Med. 2002, 36, 51–53. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, Y.; Nakajima, K.; Saitou, M.; Katano, K.; Kanemitsu, A.; Takeda, T.; Fukuda, K. The effect of lightcured resin with a glass fiber net as an intermediate material for Hard & Space mouthguard. Dent. Traumatol. 2020, 36, 654–661, Epub ahead of print. [Google Scholar] [PubMed]
- Bridgman, H.; Kwong, M.T.; Bergmann, J.H.M. Mechanical safety of embedded electronics for in-body wearables: A smart mouthguard study. Ann. Biomed. Eng. 2019, 47, 1725–1737. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; Garcia-Godoy, F.; Martorelli, M.; Sorrentino, R.; Gloria, A. Stress distribution of bulk-fill resin composite in class II restorations. Am. J. Dent. 2017, 30, 227–232. [Google Scholar]
- Ausiello, P.; Ciaramella, S.; Martorelli, M.; Lanzotti, A.; Gloria, A.; Watts, D.C. CAD-FE modeling and analysis of class II restorations incorporating resin-composite, glass ionomer and glass ceramic materials. Dent. Mater. 2017, 33, 1456–1465. [Google Scholar]
- Martorelli, M.; Ausiello, P. A novel approach for a complete 3D tooth reconstruction using only 3D crown data. Int. J. Interact. Des. Manuf. 2013, 7, 125–133. [Google Scholar]
- Amarante, M.V.; Pereira, M.V.; Darwish, F.A.; Camarão, A.F. Stress prediction in a central incisor with intra-radicular restorations. Mater. Res. 2011, 14, 189–194. [Google Scholar]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Penteado, M.M.; Borges, A.L.S.; Bottino, M.A. Influence of ceramic material, thickness of restoration and cement layer on stress distribution of occlusal veneers. Braz. Oral. Res. 2018, 32, e118. [Google Scholar]
- Mu¨ller, D.D.; Bissinger, R.; Reymus, M.; Bu¨cher, K.; Hickel, R.; Ku¨hnisch, J. Survival and complication analyses of avulsed and replanted permanent teeth. Sci. Rep. 2020, 10, 2841. [Google Scholar]
- Otani, T.; Kobayashi, M.; Nozaki, K.; Gonda, T.; Maeda, Y.; Tanaka, M. Influence of mouthguards and their palatal design on the stress-state of tooth-periodontal ligament-bone complex under static loading. Dent. Traumatol. 2018, 34, 208–213. [Google Scholar] [PubMed]
- da Rocha, D.M.; Tribst, J.P.M.; Ausiello, P.; Dal Piva, A.M.D.O.; da Rocha, M.C.; Di Nicoló, R.; Borges, A.L.S. Effect of the restorative technique on load-bearing capacity, cusp deflection, and stress distribution of endodontically-treated premolars with MOD restoration. Restor. Dent. Endod. 2019, 44, e33. [Google Scholar] [PubMed]
- de Paula Barros, J.N.; de Araújo, T.A.A.; Soares, T.R.C.; Lenzi, M.M.; de Andrade Risso, P.; Fidalgo, T.K.D.S.; Maia, L.C. Profiles of trauma in primary and permanent teeth of children and adolescents. J. Clin. Pediatr. Dent. 2019, 43, 5–10. [Google Scholar]
- Gurtu, A.; Roy, S.; Chandra, P.; Bansal, R. Reattachment of complex fractures; a reality by advances in self-etch bonding systems. Indian. J. Dent. Res. 2019, 30, 135–139. [Google Scholar]
- Tribst, J.P.M.; Dal Piva, A.M.D.O.; Bottino, M.A.; Kleverlaan, C.J.; Koolstra, J.H. Mouthguard use and TMJ injury prevention at different occlusions: A three-dimensional finite element analysis. Dent. Traumatol. 2020, 00, 1–8. [Google Scholar]


| Simulated Laminate Material | Elastic Modulus (GPa) | Enamel | Dentin | Cortical Bone | Periodontal Ligament |
| Extremely Flexible | 0.0001 | 144 | 125 | 92 | 651 |
| Low modulus reinforcement | 10 | 130 | 126 | 92 | 652 |
| No Reinforcement | 18 | 126 | 126 | 92 | 652 |
| Flexible Alloy | 50 | 125 | 126 | 92 | 652 |
| Titanium Alloy | 100 | 123 | 126 | 92 | 653 |
| Hard Material | 200 | 117 | 126 | 92 | 655 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tribst, J.P.M.; Dal Piva, A.M.d.O.; Ausiello, P.; De Benedictis, A.; Bottino, M.A.; Borges, A.L.S. Biomechanical Analysis of a Custom-Made Mouthguard Reinforced With Different Elastic Modulus Laminates During a Simulated Maxillofacial Trauma. Craniomaxillofac. Trauma Reconstr. 2021, 14, 254-260. https://doi.org/10.1177/1943387520980237
Tribst JPM, Dal Piva AMdO, Ausiello P, De Benedictis A, Bottino MA, Borges ALS. Biomechanical Analysis of a Custom-Made Mouthguard Reinforced With Different Elastic Modulus Laminates During a Simulated Maxillofacial Trauma. Craniomaxillofacial Trauma & Reconstruction. 2021; 14(3):254-260. https://doi.org/10.1177/1943387520980237
Chicago/Turabian StyleTribst, João Paulo Mendes, Amanda Maria de Oliveira Dal Piva, Pietro Ausiello, Arianna De Benedictis, Marco Antonio Bottino, and Alexandre Luiz Souto Borges. 2021. "Biomechanical Analysis of a Custom-Made Mouthguard Reinforced With Different Elastic Modulus Laminates During a Simulated Maxillofacial Trauma" Craniomaxillofacial Trauma & Reconstruction 14, no. 3: 254-260. https://doi.org/10.1177/1943387520980237
APA StyleTribst, J. P. M., Dal Piva, A. M. d. O., Ausiello, P., De Benedictis, A., Bottino, M. A., & Borges, A. L. S. (2021). Biomechanical Analysis of a Custom-Made Mouthguard Reinforced With Different Elastic Modulus Laminates During a Simulated Maxillofacial Trauma. Craniomaxillofacial Trauma & Reconstruction, 14(3), 254-260. https://doi.org/10.1177/1943387520980237




