1. Introduction
Orbital fractures are one of the most common fractures of the maxillofacial territory, accounting 13.3% of facial fractures worldwide. These fractures compromise 1 or more bone structures were the eyes are contained and protected. The etiology of these fractures is usually a direct hit on the eye and/or orbital rim that causes fracture in the less resistant areas, being these the orbital flor and medial wall. [
1] In spite of this, in many cases there is lateral wall involvement resulting from a zygomatic displacement that compromises the fronto-zygomatic and spheno-zygomatic sutures.
This causes a bone structure loss of the orbital continent that leads to a modification of the eye spatial position, herniation of the periorbital tissue, entrapment of the eye extrinsic musculature and even secondary medial wall involvement, thus causing functional and aesthetic alterations. [
2,
3] Fractures that compromise the orbit must be resolved surgically in cases where there is an aesthetic involvement and/or in situations in which the fracture defect causes an alteration of the normal morphology of inferior and medial extrinsic muscles that could lead to diplopia and enophthalmos. [
2,
3]
For the above reasons, the approach to access the surgical area must respect aesthetic and functional principles to minimize facial sequelae, that might have already been caused by the trauma. The transconjunctival approach was first described in 1923 by Bourquet and was used to eliminate eyelid fatty tissue for aesthetic purposes. [
4] Tessier in 1973 used this technique to access bone structures that build the orbital rim to resolve structural abnormalities in patients with craniofacial malformation and trauma. [
5]
2. Material and Methods
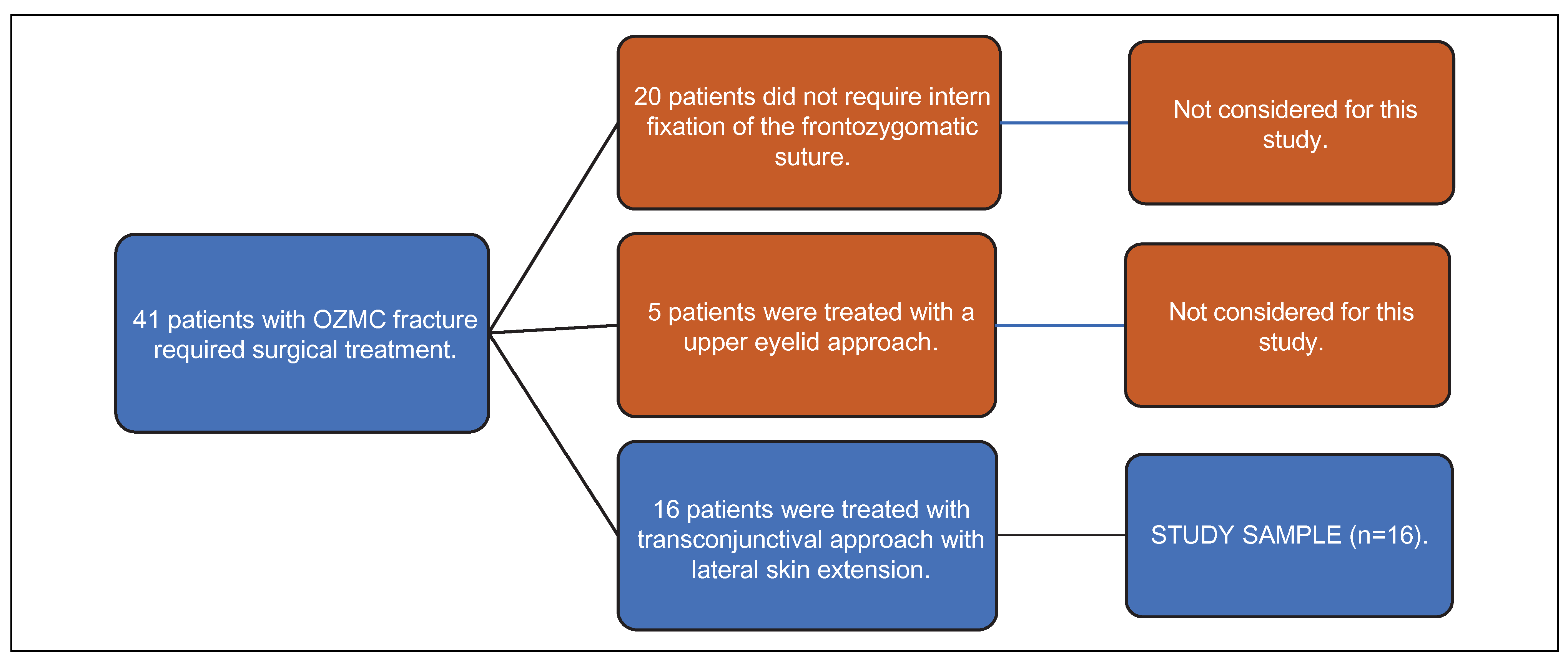
The clinical records of all patients diagnosed with orbitozygomatic complex (OZMC) fracture that needed surgical intervention and were treated in the Oral and Maxillofacial Surgery Service of El Carmen Metropolitan Clinical Hospital (Santiago, Chile) between January 2016 and September 2019 were reviewed. A total of 41 patients (32 men and 9 women) were selected, considering the following points as surgical criteria to repair the fracture: (1) diplopia, (2) enophthalmos >2 mm, (3) dysesthesia on the infraorbital area, (4) palpable irregularity of the infraorbital rim, (5) restriction of eye movement, (6) herniation of peri-orbital soft tissue, evaluated with computed tomography, and/or muscle entrapment of lower and/or middle rectus muscle, or orbital defect >2 cm. Among this group of patients, 20 of them were excluded for not presenting the need for intern fixation with osteosynthesis of the frontozygomatic suture, according to Ellis algorithm. [
6] In addition, 5 patients were also excluded for utilizing upper eyelid as unique approach to access the frontozygomatic suture and fix it with osteosynthesis. The transconjunctival approach was not necessary as there were no infraorbital rim or orbital floor involvement. [
6] Finally, we selected for this study all patients who underwent surgical treatment using a transconjunctival approach with lateral skin extension as unique approach to access the frontozygomatic fracture, orbital rim and/or orbital floor, obtaining a total of 16 patients as study sample (
Figure 1). All patients were followed-up for at least 9 months after surgery, and the appearance of the following post-surgical complications and its resolutions associated with the transconjunctival approach were analyzed: scleral exposure, eyelid position changes, chemosis, ectropion, and entropion. Those complications associated with trauma itself, orbit fracture, or orbital reconstruction, were not considered for this study as they are not associated with the transconjunctival approach technique. All patients received professional ophthalmologic evaluation before and after surgery.
3. Surgical Technique
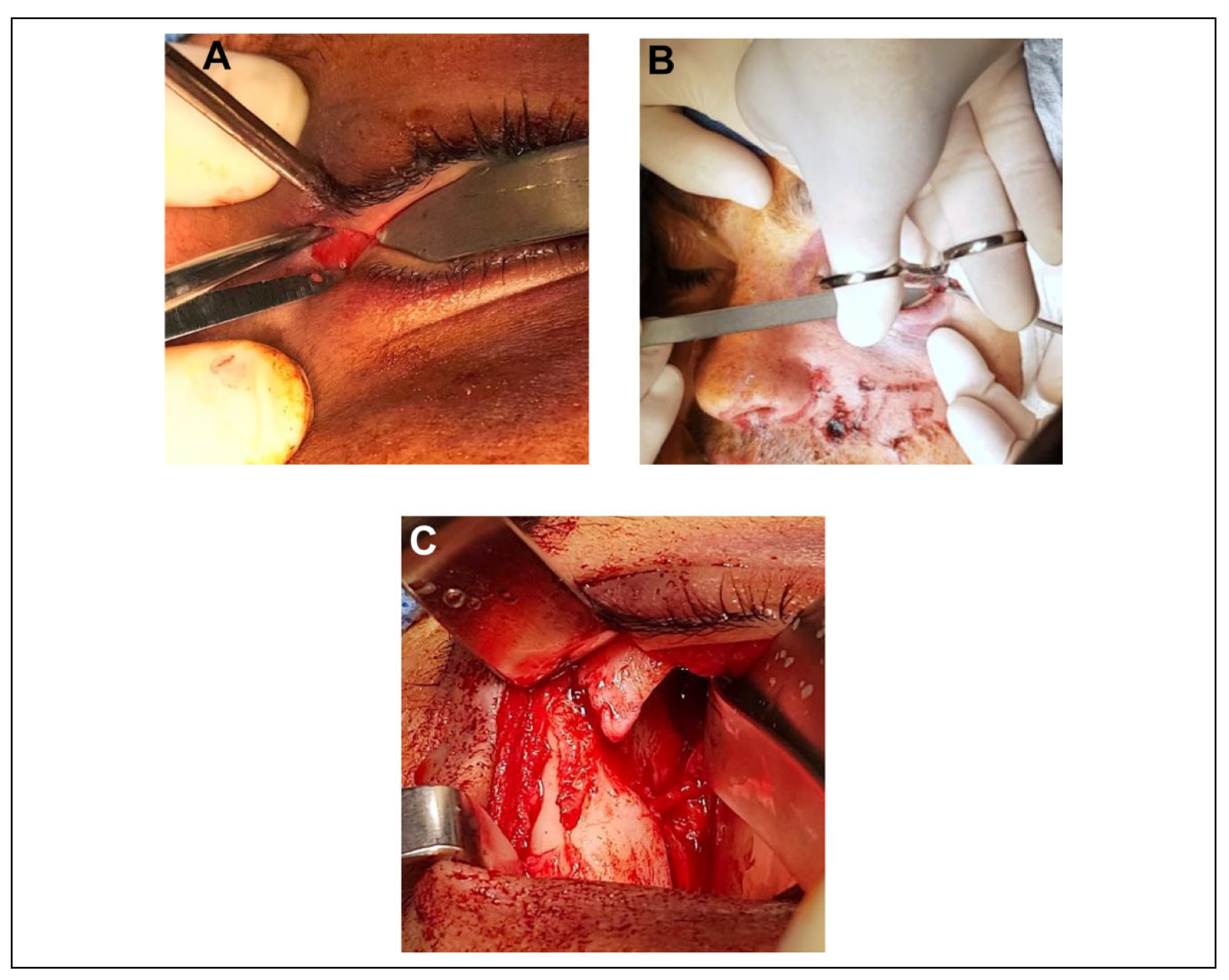
The transconjunctival approach using lateral skin extension aims to access the inferior and lateral rim, orbital floor, and lateral wall of the orbit, up to the sphenozygomatic suture. The transconjunctival incision can be performed using a preseptal incision. In this technique, the lateral first. The incision is made with scissors horizontally along the natural wrinkle of the palpebral fissure up to 0.8–1 cm. It is done by cutting the lateral edge of the orbit, skin incision, the orbicular muscle, orbital septum, lateral canthal tendon and finally the conjunctive tissue (
Figure 2A). After this, the lower eyelid continues being fixed to the lateral orbital edge along the lower end of the lateral canthal tendon, so a vertical cantholysis with scissors is required (
Figure 2B), allowing a total release of the lower eyelid. After finishing the canthotomy and lateral skin extension, the incision of the conjunctiva is made in order to access the inferior rim. To make this incision, an adequate exposure of the eyelid conjunctiva, and retraction and protection of the eye globe are necessary, thus gaining access to the orbital floor, inferior rim and lateral wall, and being able to extend vertically to the frontozygomatic suture through the conjunctiva (
Figure 2C). [
7] The lateral skin extension described in this article requires an incision on the skin up to 0.8 cm with a disinsertion of the superior canthal ligament and a conjunctival incision on the lateral zone, allowing bone exposure of the frontozygomatic suture and access to the lateral wall up to the spheno-zygomatic junction if necessary. In cases where is required, this approach can be combined with the retro-caruncular medial extension in order to access the medial wall of the orbit at the same surgical time.
Following reconstruction of the compromised fracture, the periosteum, the lateral canthal ligament and the orbicular muscular plane must be repositioned in the lateral area with an absorbable suture made of Polylactic Acid. The lateral canthal ligament, after performing the canthotomy and cantholysis on its lower portion, remains attached to the peri-orbit, so when the surgical area is closed, the canthal portion stands in its place no longer requiring to suture both canthal ligament endings with each other. Moreover, the lower portion reposition is reaffirmed with the suture of the lower peri-orbit at the same level. After this, external skin edge is fixed with blue monofilament polypropylene 6-0, and the conjunctival incision in all of 16 patients was sutured utilizing simple catgut 5-0.
4. Results
The group of study was conformed by 16 patients of El Carmen Metropolitan Clinical Hospital, of Santiago, Chile, that underwent surgical treatment for orbital reconstruction using the transconjunctival approach with lateral skin extension utilizing a preseptal incision in the conjunctiva. Of the total sample, the majority was male (81%), considering aggression as the main cause for seek medical treatment. On the other hand, the remaining 19% was female and compared to men, the leading cause of seeking surgical intervention was traffic accident. Among both groups, men and women, there were not intraoperative complications reported (
Table 1). Of the total study sample, only 1 patient presented an isolated lateral wall fracture, 13 patients had orbital rim, orbital floor, and lateral wall fracture, and only 2 patients had orbital floor fracture with medial and lateral wall involvement (
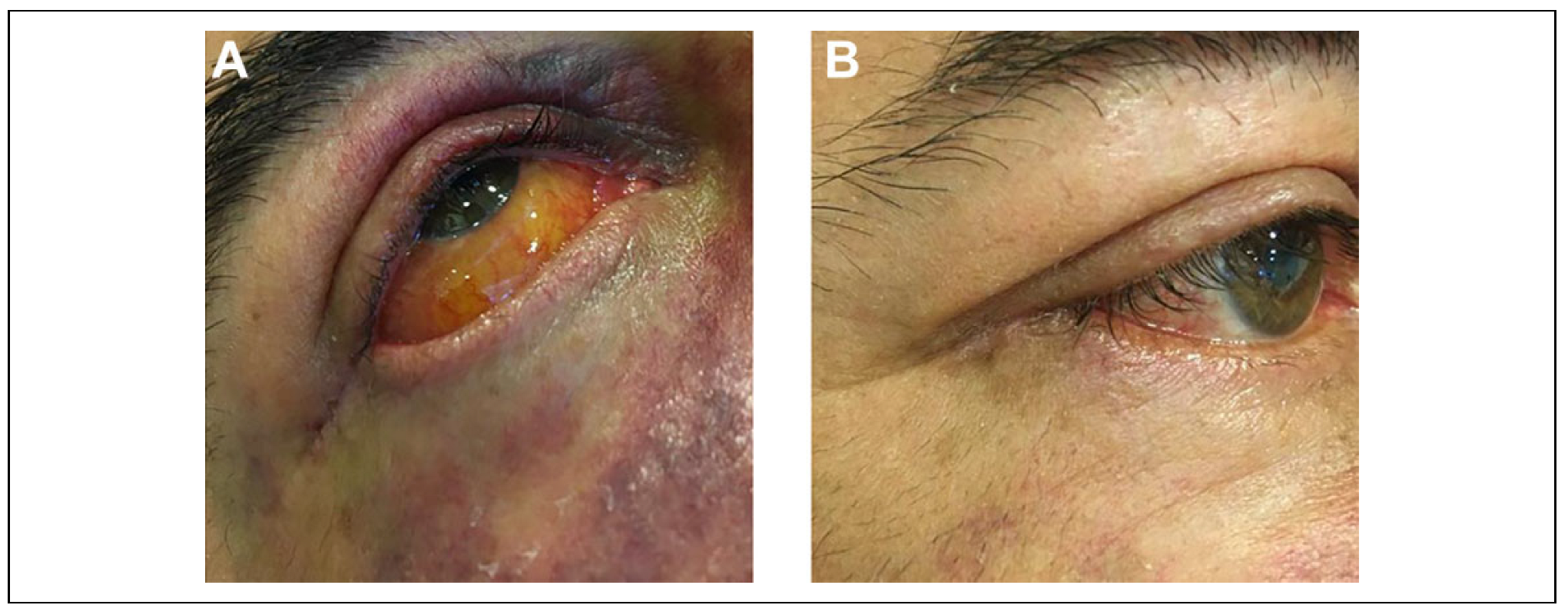
Table 2). On both patients with medial wall involvement, the fractures were fixed using a retrocaruncular extension due to the transconjunctival approach with lateral skin extension, being able to repair both medial and lateral wall and the orbital floor on the same surgical approach. All fractures were reduced and fixed with osteosynthesis plates and screws. A pre-formed titanium mesh was also used on those cases that needed orbital floor reconstruction (11 patients) using the same approach studied, after releasing the herniated peri-orbital tissue and the extrinsic eye musculature. The authors assessed vision changes, scleral exposure, eyelid position changes, chemosis, ectropion, and entropion as outcome measures for the transconjunctival approach complications. Only 1 patient presented post-surgical chemosis due to a suture stitch used on the conjunctival closure, that when removed resolved spontaneously 72 h later (
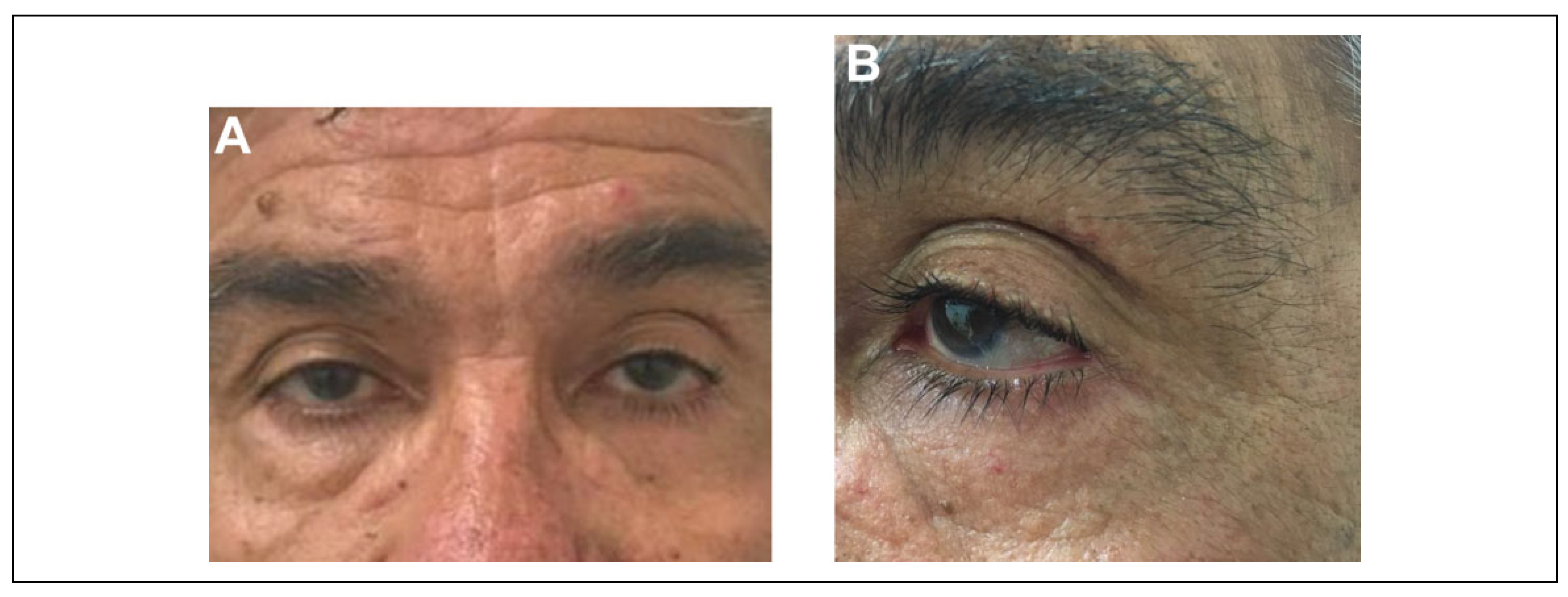
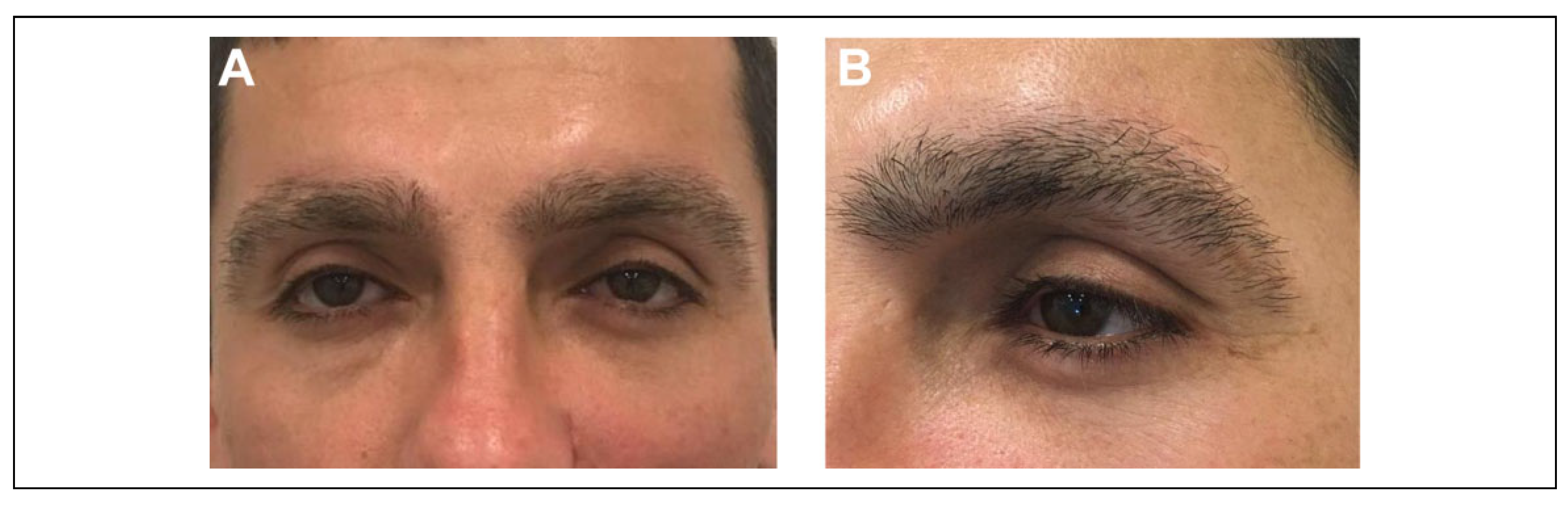
Figure 3A,B). After surgical intervention, patients underwent a duction test to corroborate eye movement and were hospitalized for 2 to 3 days before discharging them from the hospital. Then continued with outpatient follow up for 2 to 12 months. All patients were subjectively satisfied with the post-surgery aesthetic results and there were not observable changes on the lower eyelid position (
Figure 4A,B,
Figure 5A,B,
Figure 6A,B). During follow-up period it was not necessary to remove any of the osteosynthesis materials, but if needed in the future, the same approach can be used since it allows a direct and quick access to the surgical area without major complications.
5. Discussion
The sub-ciliary, sub-tarsal and inferior eyelid approaches are called transcutaneous approaches to access the orbit.
Many studies have shown that these approaches have disadvantages compared to the transconjunctival approach with its variants. [
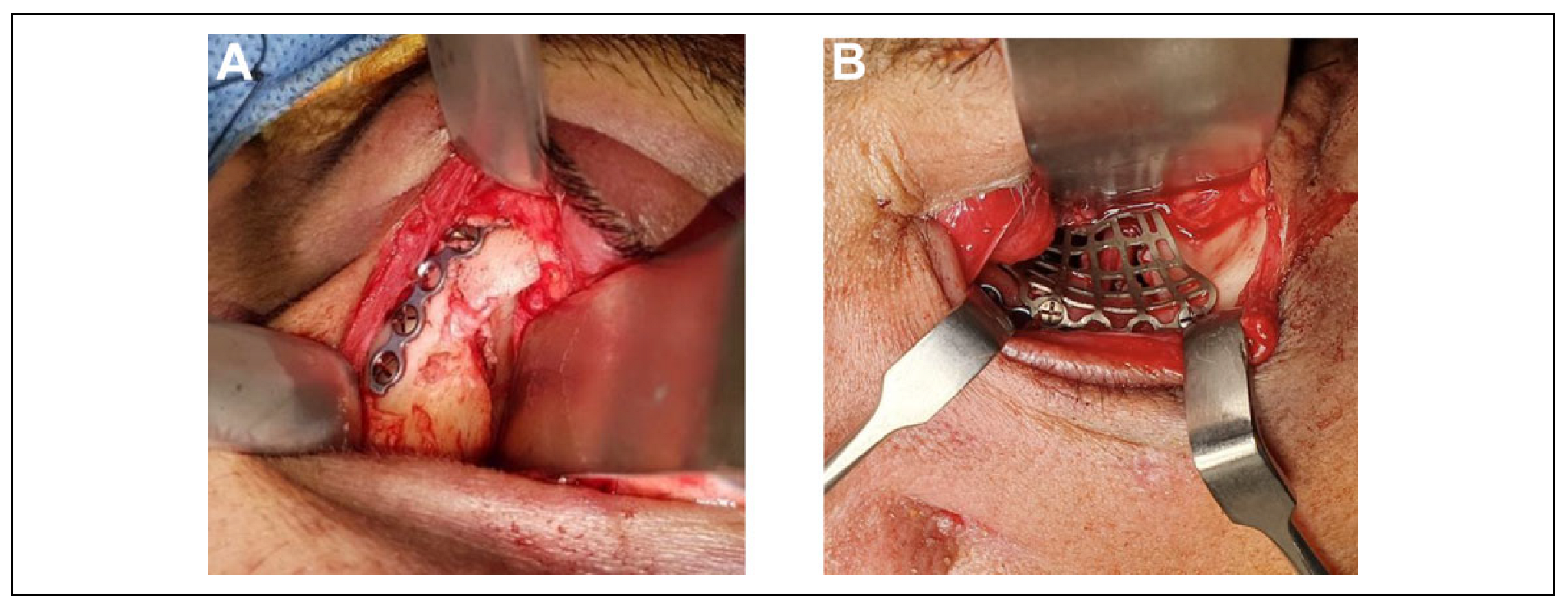
8] In this context, the use of trans or retro-caruncular modification, and the lateral skin extension described, allows an access to the medial, lateral, and infra orbital rim in addition to the orbital floor by a single incision and approach. Moreover, it is highlighted that lateral canthotomy in the transconjunctival approach is an important factor to reduce the frequency of complications, decreasing the tension on the tarsal plate during surgery, allowing the placement of osteosynthesis elements and reconstructive meshes when needed (
Figure 7A,B). [
9]
Although the transcutaneous approaches (sub-ciliary, sub-tarsal and inferior eyelid techniques) allow good access to the floor and orbital rim, they do not expose the lateral and medial wall by themselves. This limitation requires the use of a complementary approach in another surgical site, increasing the operating time, surgical complications and morbidity to the patient, due to the necessity of performing a second skin incision in order to access the frontozygomatic suture. [
10] Despite of the extensive use of transcutaneous approaches and combined among them to achieve the whole operational zone, the biggest disadvantage compared with the transconjunctival approach is aesthetic: a visible scar on skin is the evidence. Although in many cases this may look imperceptible, is not exempt from complications inherent to the scar tissue, such as the presence of keloids, hypertrophic scar, and scar adhesion. [
10] In a retrospective study published in 2020, the use of the transconjunctival approach was recommended as the first choice for infra-orbital rim and orbital floor fractures, after obtaining a 94% success rate when this approach was used to resolve fractures that compromised the orbit, and reporting only 6% of complications of which 5% corresponded to orbit trauma complications and not associated with the approach itself. [
11]
In our study, we observed that transconjunctival approach with lateral skin extension and canthotomy had an excellent performance for various orbital fractures, showing good visibility of the different structures involved with a single incision, minimum surgical time, low morbidity, and optimum aesthetic and functional results. Nevertheless, is written on the literature that this approach, although has multiple virtues, is not exempt of intra or post-surgical complications such as tarsal plate tear, cutaneous perforation, conjunctival chemosis, eyelid edema and entropion, among others. [
11,
12]
In 2009, Ridgway conducted a meta-analysis that compared different approaches to access the orbital fracture, concluding that the transconjunctival approach had significantly lower complications compared to the sub-ciliary and sub-tarsal approaches, considering entropion, ectropion and eyelid edema as the most common complications. [
9] Additionally, in 2015 Vaibhav conducted a study with a sample of 40 patients with orbital fractures and compared the use of the transconjunctival and the subciliary approach. At the end of the study, he concluded that although the sub-ciliary approach presented a good exposure of the infra-orbital rim and was very useful for fractures with a significant displacement component, the transconjunctival approach was comparatively quicker to perform, had a lower rate of postoperative complications and had more aesthetic acceptance [
12]; correlating to the results described by Ridgway on his meta-analysis.
In a retrospective study published in 2018, a granuloma associated with a suture stitch was described as the only post-operative complication in a sample of 30 patients treated with the transconjunctival approach with retrocaruncular extension. [
12] In line with this study, we also had only 1 post-operative complication associated with the transconjunctival approach: a conjunctival chemosis due to a suture stitch that resolved spontaneously after the irritating factor was removed. About this, there are different authors who recommend to not suture the transconjunctival approach because it reduces the operative time and favors the drainage of the post-operative edema. [
13] Contrary to this, and based on our own experience, we recommend the use of absorbable suture to close up the transconjunctival approach, as it brings benefits for the patient such as reducing not only post-operative bleeding but the risk of infection of the surgical wound. In addition to this, not suturing the transconjunctive surgical wound can produce the adhesion of clots in the conjunctival area, making necessary the constant cleaning of the wound and increasing the hospitalization time for the patient. [
12] Although the literature describes that not suturing the incision of the palpebral conjunctiva could improve drainage and reduce postoperative edema, in our own experience, the use of the lateral skin extension for the transconjunctival approach by itself reduces the tension exerted on the soft tissues, showing minimal postoperative edema, despite of the fact that all patients underwent suture of the palpebral conjunctival incision.
An important element not evaluated on this study, corresponds to patient’s adherence to the post-surgical indications, since these are critical for the correct evolution of the surgical wound, which could be the topic for another study.
6. Conclusions
The transconjunctival approach with lateral skin extension in our experience has proven to be a viable, versatile and safe alternative for the resolution of orbit zygomatic fractures, allowing a complete access to the orbital floor, rim, frontozygomatic suture and lateral wall with only 1 surgical incision. On the other hand, we observed in our case series that the rate of complications of the studied approach is low, being these reversible and easy to resolve. Finally, we can say this approach is a great alternative to access the frontozygomatic suture, with a low rate of complications, and that can be used in combination with other approaches.