Is the Use of Intermaxillary Fixation Screws an Alternative to Erich Arch Bars for Maxillomandibular Fixation During Management of Maxillofacial Fractures? A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
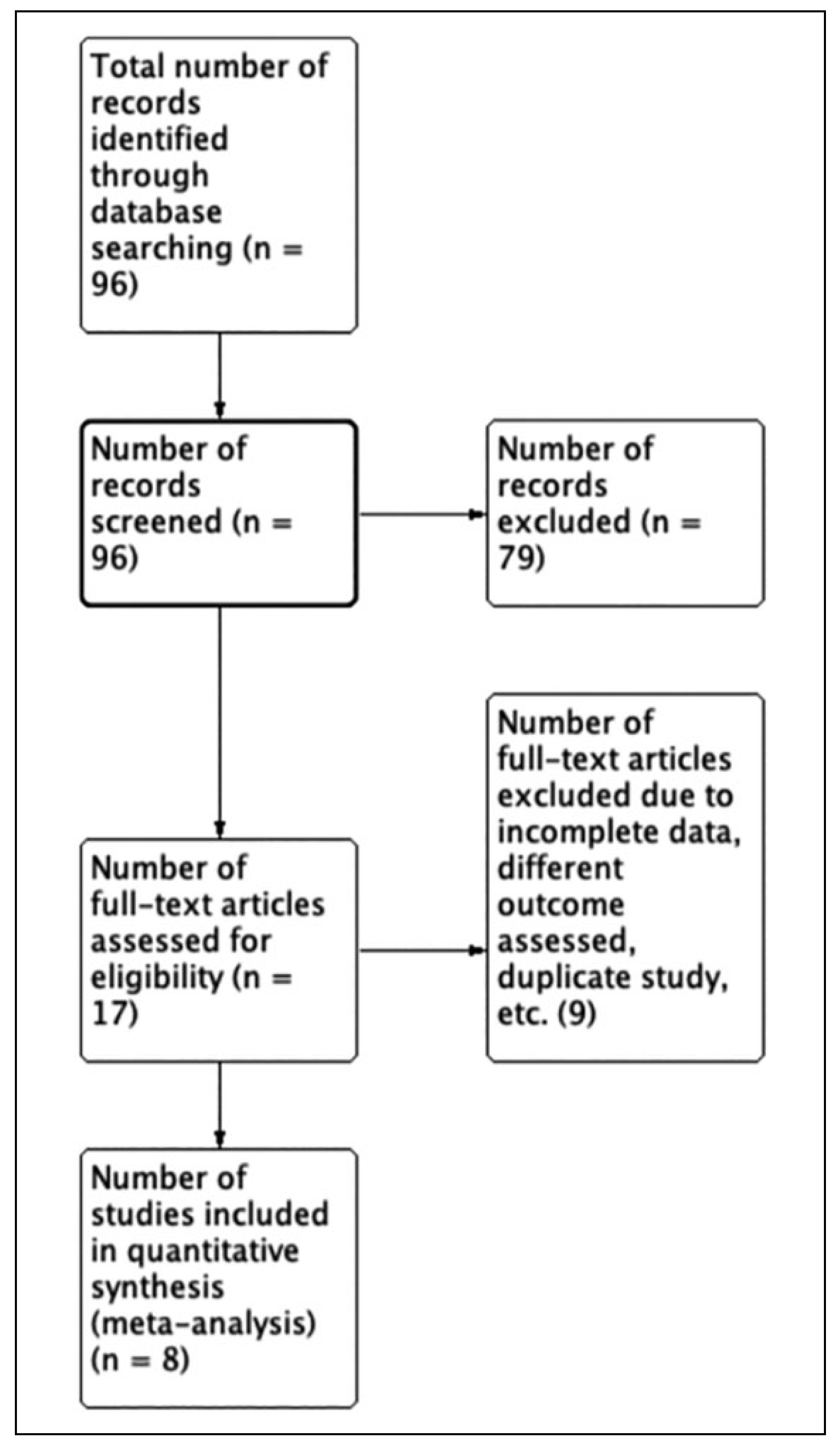
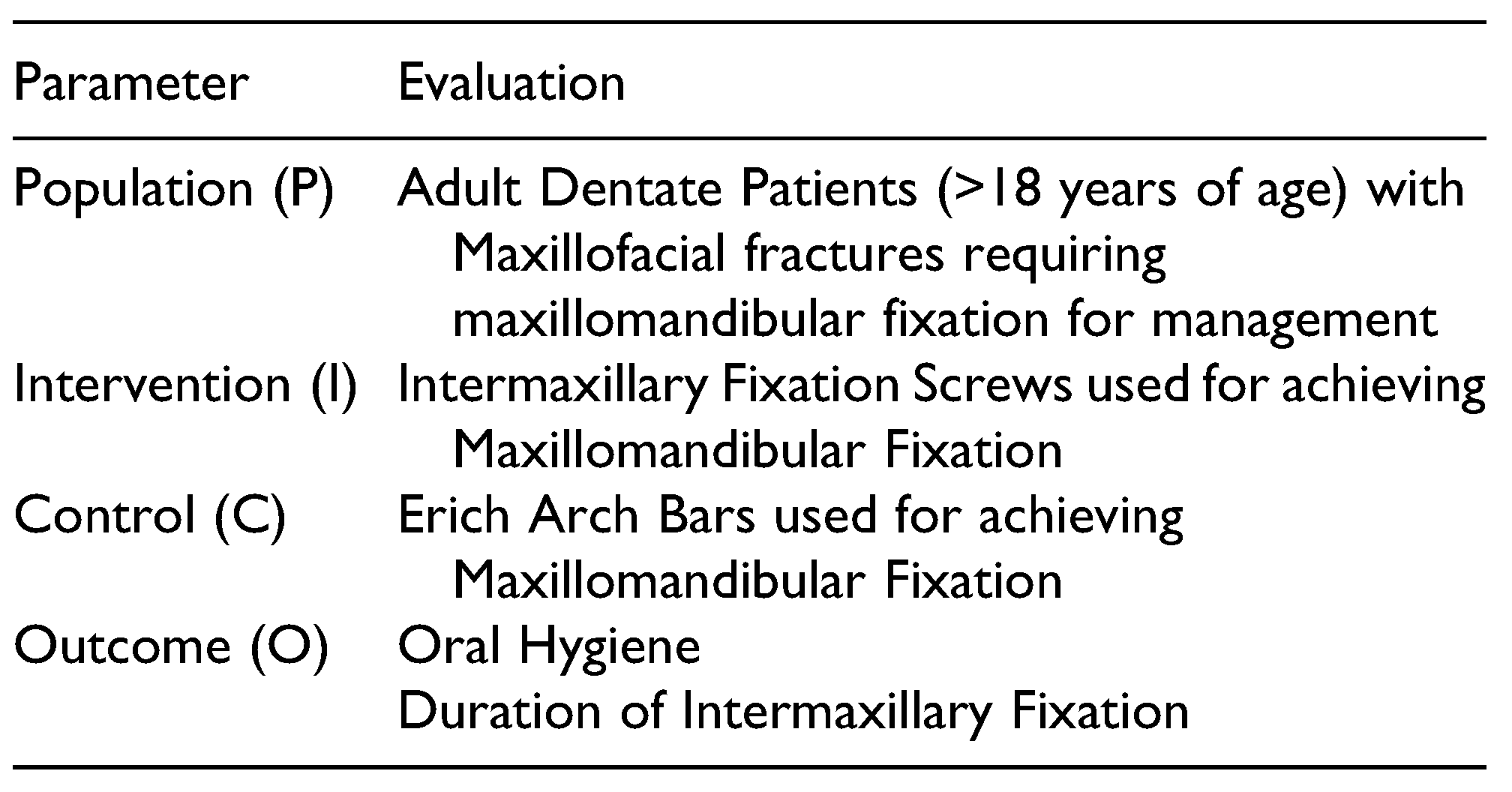
2. Methodology
2.1. Search Strategy
2.2. Study Selection
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Analysis
2.7. Grading
3. Results
3.1. Literature Search Results
3.2. Quality Assessment Results
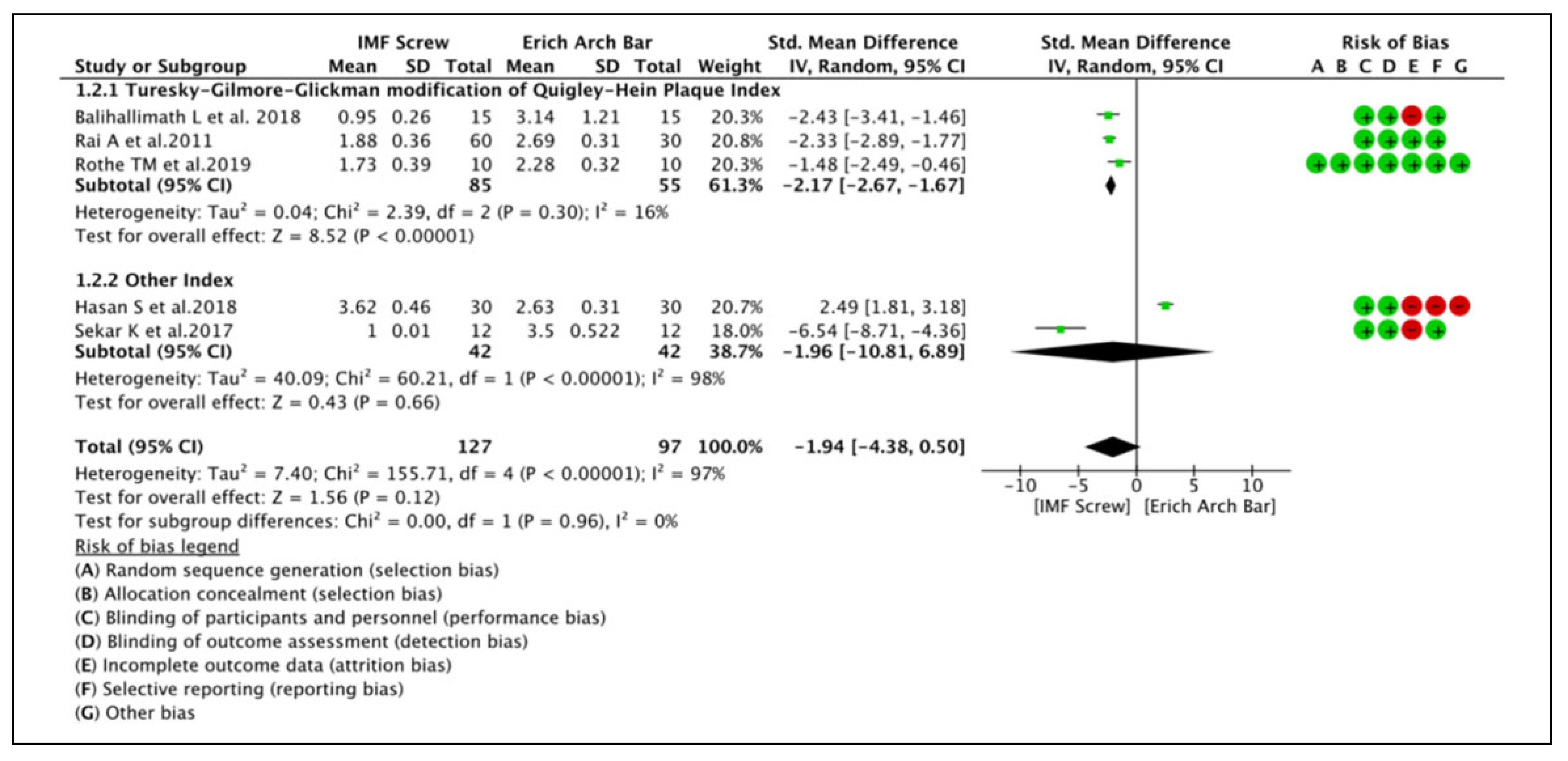
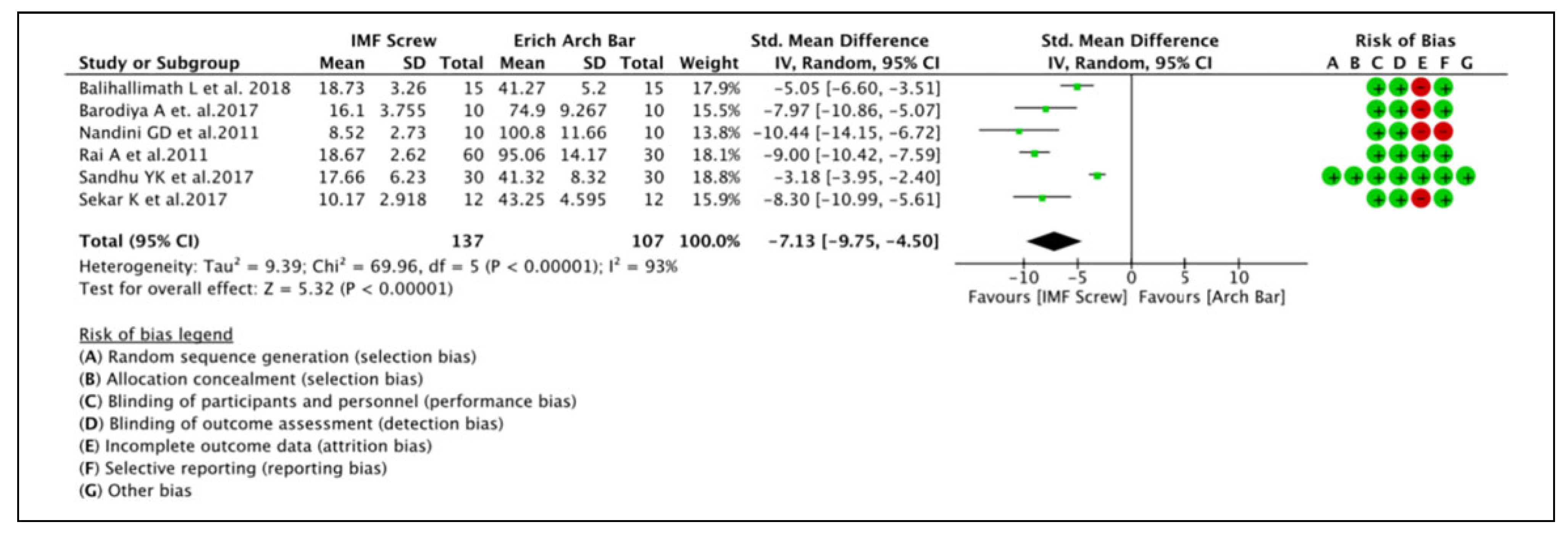
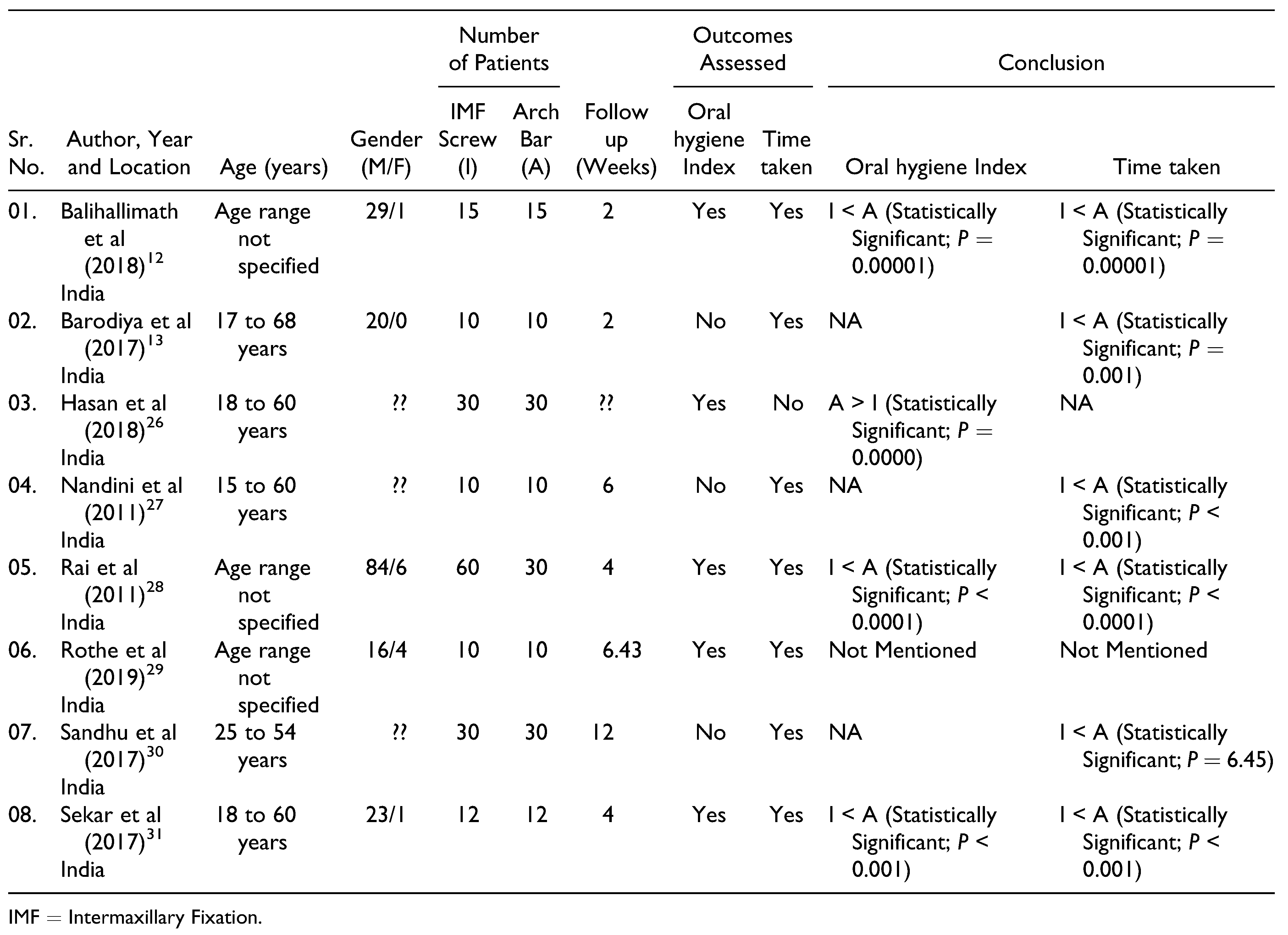
3.3. Meta-Analysis Results
3.4. Narrative Review
3.5. GRADE Analysis Result
4. Discussion
5. Conclusions
Funding
Conflicts of Interest
References
- Rai, A.; Jain, A.; Datarkar, A. Comparison of single versus two non-compression miniplates in the management of unfavourable angle fracture of the mandible: A prospective randomized clinical study. Oral. Maxillofac. Surg. 2018, 22, 157–161. [Google Scholar] [PubMed]
- Kotrashetti, S.M.; Lingaraj, J.B.; Khurana, V. A comparative study of closed versus open reduction and internal fixation (using retromandibular approach) in the management of subcondylar fracture. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2013, 115, e7–e11. [Google Scholar]
- Karan, A.; Kedarnath, N.S.; Reddy, G.S.; Kumar, T.H.; Neelima, C.; Bhavani, M.; Nayyar, A.S. Condylar fractures: Surgical versus conservative management. Ann. Maxillofac. Surg. 2019, 9, 15–22. [Google Scholar]
- Mukerji, R.; Mukerji, G.; McGurk, M. Mandibular fractures: Historical perspective. Br. J. Oral. Maxillofac. Surg. 2006, 44, 222–228. [Google Scholar]
- Arthur, G.; Berardo, N. A simplified technique of maxillomandibular fixation. J. Oral. Maxillofac. Surg. 1989, 47, 1234. [Google Scholar]
- Hollows, P.; Brennan, J. Temporary intermaxillary fixation: A quick reliable 64 method. Br. J. Oral. Maxillofac. Surg. 1999, 37, 422–423. [Google Scholar]
- Rai, A.; Jain, A.; Rasal, S. Use of two miniplates to achieve intraoperative maxillomandibular fixation. J. Stomatol. Oral. Maxillofac. Surg. 2017, 118, 289–290. [Google Scholar] [CrossRef]
- Rai, A.; Jain, A. A technique for intraoperative maxillomandibular fixation. Oral. Maxillofac. Surg. 2017, 21, 485–486. [Google Scholar] [CrossRef]
- Rai, A.; Jain, A.; Datarkar, A.; Purohit, S. Are bondable buttons a better option than intermaxillary fixation screws for achieving maxillomandibular fixation? A prospective randomized clinical study. J. Maxillofac. Oral. Surg. 2019, 18, 551–554. [Google Scholar]
- Rai, A.; Jain, A.; Datarkar, A.; Mandora, D. Intermaxillary fixation with two loop wires: The Rai technique. Br. J. Oral. Maxillofac. Surg. 2020, 58, 613–614. [Google Scholar] [CrossRef]
- Ring, M.E.; Harry, N. (Eds.) Dentistry—A Illustrated History 1992.; Abrahams Inc. Publishers: New York, NY, USA, 1992; Volume 70. [Google Scholar]
- Balihallimath, L.; Jain, R.; Mehrotra, U.; Rangnekar, N. To compare the efficiency of maxillomandibular fixation screws over Erich arch bar in achieving intermaxillary fixation in maxillofacial trauma: A clinical study. J. Int. Clin. Dent. Res. Organ. 2018, 10, 27–31. [Google Scholar]
- Barodiya, A.; Thukral, R.; Agrawal, S.M.; Chouhan, A.S.; Singh, S.; Loksh, Y. Self-tapping intermaxillary fixation screw: An alternative to arch bar. J. Contemp. Dent. Pract. 2017, 18, 147–151. [Google Scholar] [PubMed]
- Choi, J.W.; Kim, H.B.; Jeong, W.S.; Kim, S.C.; Koh, K.S. Comparison between intermaxillary fixation with screws and an arch bar for mandibular fracture. J. Craniofac. Surg. 2019, 30, 1787–1789. [Google Scholar]
- Jain, A.; Rai, A. Meta-analysis to evaluate the efficacy of sternocleidomastoid muscle flap as a reconstruction modality in prevention of Frey’s syndrome following parotidectomy. J. Maxillofac. Oral. Surg. 2020. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: London, UK, 2011. [Google Scholar]
- Ryan, R.; Hill, S. How to GRADE the Quality of the Evidence; Version 3.0; Cochrane Consumers and Communication Group, 2016. [Google Scholar]
- Jain, R.; Pathak, R.; Agrawal, S.; Dadsena, K.; Kumar, V.; Ramavath, M.N. Comparison of the efficiency of maxillomandibular fixation screws over Erich arch bars in achieving intermaxillary fixation in maxillofacial trauma: A clinical study. Int. J. Oral. Care Res. 2018, 6, 12–16. [Google Scholar]
- Majeti, V.D.; Reddy, S.; Sinha, R.; Kiran, U.; Tahseen; Srikanth, D. IMF screws an alternative to Arch bar. Int. J. Recent. Sci. Res. 2017, 8, 21198–21202. [Google Scholar]
- Park, K.N.; Oh, S.M.; Lee, C.Y.; Kim, J.Y.; Yang, B.E. Design and application of hybrid maxillomandibular fixation for facial bone fractures. J. Craniofac. Surg. 2013, 24, 1801–1805. [Google Scholar]
- Qureshi, A.A.; Reddy, U.K.; Warad, N.M.; Badal, S.; Jamadar, A.A.; Qurishi, N. Intermaxillary fixation screws versus Erich arch bars in mandibular fractures: A comparative study and review of literature. Ann. Maxillofac. Surg. 2016, 6, 25–30. [Google Scholar]
- van den Bergh, B.; Blankestijn, J.; van der Ploeg, T.; Tuinzing, D.B.; Forouzanfar, T. Conservative treatment of a mandibular condyle fracture: Comparing intermaxillary fixation with screws or arch bar. A Randomised clinical trial. J. Craniomaxillofac. Surg. 2015, 43, 671–676. [Google Scholar]
- van den Bergh, B.; de Mol van Otterloo, J.J.; van der Ploeg, T.; Tuinzing, D.B.; Forouzanfar, T. IMF-screws or arch bars as conservative treatment for mandibular condyle fractures: Quality of life aspects. J. Craniomaxillofac. Surg. 2015, 43, 1004–1009. [Google Scholar]
- Vartanian, A.J.; Alvi, A. Bone-screw mandible fixation: An intraoperative alternative to arch bars. Otolaryngol. Head. Neck Surg. 2000, 123, 718–721. [Google Scholar]
- Vatsa, P.; Siddaraju, A. A comparative clinical study on selfdrilling screws and Erich arch bars in mandibular fractures. Int. J. App Dent. Sci. 2018, 4, 212–217. [Google Scholar]
- Hassan, S.; Farooq, S.; Kapoor, M.; Shah, A. Comparative evaluation of modified Erich’s arch bar, conventional Erich’s arch bar and intermaxillary fixation screws in maxillo-mandibular fixation: A prospective clinical study. Int. J. Med. Res. Prof. 2018, 4, 41–45. [Google Scholar]
- Nandini, G.D.; Balakrishna, R.; Rao, J. Self tapping screws v/s Erich arch bar for inter maxillary fixation: A comparative clinical study in the treatment of mandibular fractures. J. Maxillofac. Oral. Surg. 2011, 10, 127–131. [Google Scholar]
- Rai, A.; Datarkar, A.; Borle, R.M. Are maxillomandibular fixation screws a better option than Erich arch bars in achieving maxillomandibular fixation? A randomized clinical study. J. Oral. Maxillofac. Surg. 2011, 69, 3015–3018. [Google Scholar]
- Rothe, T.M.; Kumar, P.; Shah, N.; Shah, R.; Mahajan, A.; Kumar, A. Comparative evaluation of efficacy of conventional arch bar, intermaxillary fixation screws, and modified arch bar for intermaxillary fixation. J. Maxillofac. Oral. Surg. 2019, 18, 412–418. [Google Scholar]
- Sandhu, Y.K.; Padda, S.; Kaur, T.; Dhawan, A.; Kapila, S.; Kaur, J. Comparison of efficacy of transalveolar screws and conventional dental wiring using Erich arch bar for maxillomandibular fixation in mandibular fractures. J. Maxillofac. Oral. Surg. 2018, 17, 211–217. [Google Scholar]
- Sekar, K.; Natarajan, P.M.; Kapasi, A. Comparison of arch bar, eyelets and transmucosal screws for maxillo mandibular fixation in jaw fracture. Biomed. Pharmacol, J. 2017, 10, 497–508. [Google Scholar]
- Turesky, S.; Gilmore, G. Reduced plaque formation by chloro-methyl analogue of Vit. C. J. Periodontol. 1970, 41, 41–43. [Google Scholar]
- Baurmash, H.; Farr, D.; Baurmash, M. Direct bonding of arch bars in the management of maxillomandibular injuries. J. Oral. Maxillofac. Surg. 1988, 46, 813–815. [Google Scholar]
- Jones, D.C. The intermaxillary screw: A dedicated bicortical bone screw for temporary intermaxillary fixation. Br. J. Oral. Maxillofac. Surg. 1999, 37, 115–116. [Google Scholar] [PubMed]
- Murray, W.B.; Gouws, E. “No difference v. not enough evidence”—Calculating the power and beta error. S. Afr. Med. J. 1993, 83, 863–865. [Google Scholar] [PubMed]
- Gibbons, A.J.; Hodder, S.C. A self-drilling intermaxillary fixation screw. Br. J. Oral. Maxillofac. Surg. 2003, 41, 48–49. [Google Scholar] [PubMed]
- Bins, A.; Oomens, M.A.E.; Boffano, P.; Forouzanfar, T. Is there enough evidence to regularly apply bone screws for intermaxillary fixation in mandibular fractures? J. Oral. Maxillofac. Surg. 2015, 73, 1963–1969. [Google Scholar]
 |
 |
 |
 |
 |
© 2020 by the author. The Author(s) 2020.
Share and Cite
Jain, A.; Rai, A. Is the Use of Intermaxillary Fixation Screws an Alternative to Erich Arch Bars for Maxillomandibular Fixation During Management of Maxillofacial Fractures? A Systematic Review and Meta-Analysis. Craniomaxillofac. Trauma Reconstr. 2021, 14, 236-245. https://doi.org/10.1177/1943387520971410
Jain A, Rai A. Is the Use of Intermaxillary Fixation Screws an Alternative to Erich Arch Bars for Maxillomandibular Fixation During Management of Maxillofacial Fractures? A Systematic Review and Meta-Analysis. Craniomaxillofacial Trauma & Reconstruction. 2021; 14(3):236-245. https://doi.org/10.1177/1943387520971410
Chicago/Turabian StyleJain, Anuj, and Anshul Rai. 2021. "Is the Use of Intermaxillary Fixation Screws an Alternative to Erich Arch Bars for Maxillomandibular Fixation During Management of Maxillofacial Fractures? A Systematic Review and Meta-Analysis" Craniomaxillofacial Trauma & Reconstruction 14, no. 3: 236-245. https://doi.org/10.1177/1943387520971410
APA StyleJain, A., & Rai, A. (2021). Is the Use of Intermaxillary Fixation Screws an Alternative to Erich Arch Bars for Maxillomandibular Fixation During Management of Maxillofacial Fractures? A Systematic Review and Meta-Analysis. Craniomaxillofacial Trauma & Reconstruction, 14(3), 236-245. https://doi.org/10.1177/1943387520971410




