Introduction
The exploration of maxillofacial fractures is common, but a consensus on their patterns cannot be achieved as all epidemiologic surveys conducted vary with geographic location, population density of the region, educational and socioeconomic status of its people, regional preventive strategies, and local laws and protocols.[
1,
2] Although the mandible is the largest and strongest bone of the face it is very frequently fractured (second to the nasal bone) as a result of its position.[
2] Mandibular fractures account for twice the number of midface fractures and comprise the majority of injuries treated by an oral and maxillofacial surgeon.[
3] The incidence of ramus fractures is quite low among mandibular fractures and rank just above the least encountered fractures of the coronoid and alveolar processes.[
2,
4,
5,
6]
Anatomically the ramus is located between the subcondyle and angle of mandible. Fractures in this area have been observed to run obliquely or horizontally.[
1] No classification exists for such fractures, as a result of which there is a dearth of understanding about their management and, generally, are either left untreated or treated overzealously.
The proposed reference arrangement of fracture lines of the ramus of mandible, to the best of our knowledge, does not exist till date.
Methodology
A literature search was carried out in PubMed, Science-Direct, and Google Scholar, and references from the reported articles were cross-checked to look for cases of ramal fractures in English language till 2018. Also, we retrospectively reviewed our own patients with ramus fractures who visited our oral and maxillofacial surgery unit in the previous 5 years.
Mandibular fracture patients who reported were evaluated clinically and also subjected to orthopantomograms and computerized tomograms. Patients were diagnosed as having mandibular ramus fractures when the fracture line was between the subcondyle and angle of mandible and were included for evaluation. Due to the retrospective nature of this study, ethical clearance was exempted by the institutional review board.
In lieu of a nonexistent classification of ramus fractures, this study was carried out to be able to delineate these fractures. Fractures were categorized into repititive patterns on the basis of radiological observations and similar clinical presentations. In addition, incidence, gender distribution, cause of trauma, surgical treatment options utilized, and potential complications arising from the management of such fractures were also studied in our patients and reviewed in the literature.
Results
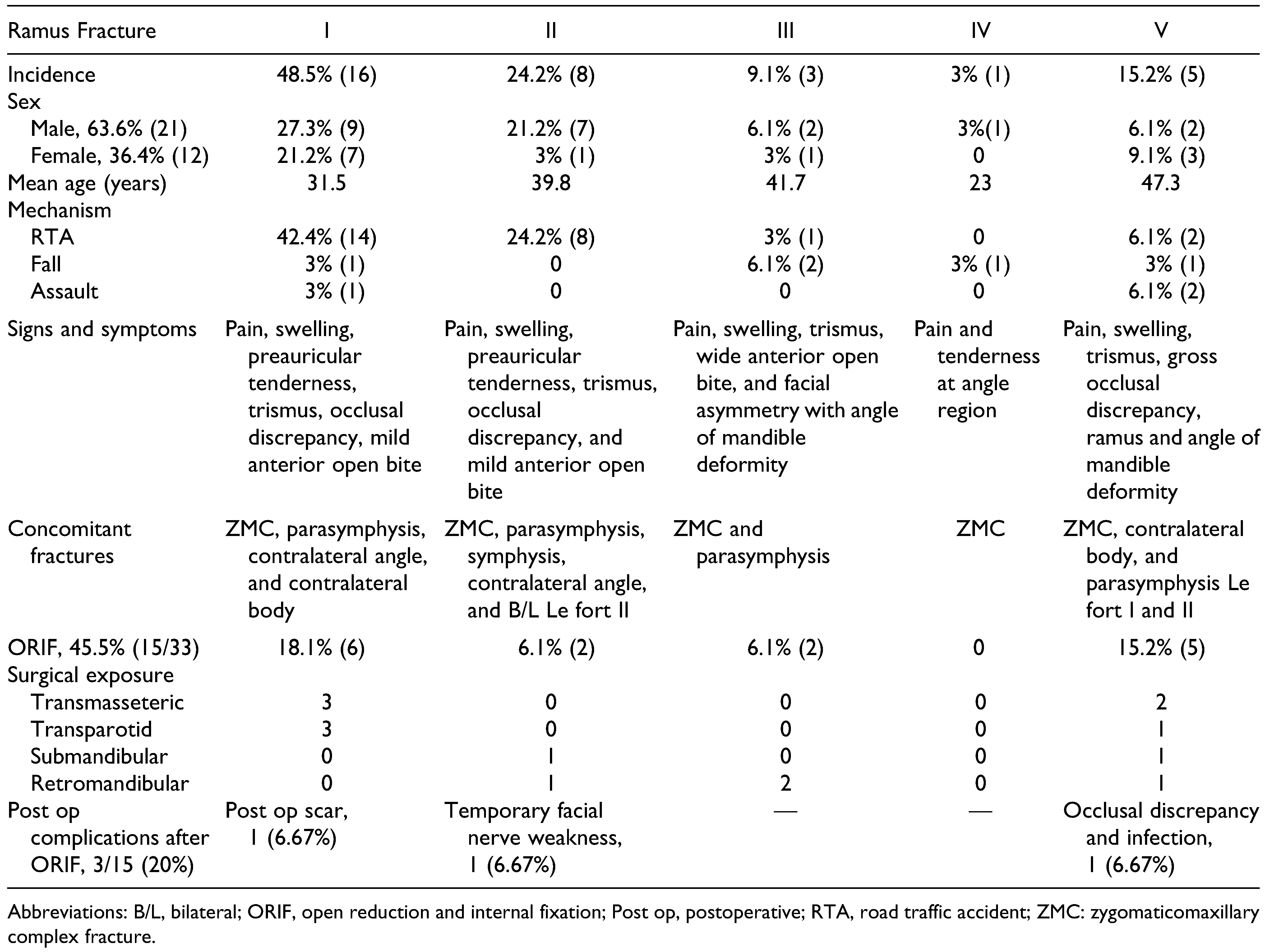
Of the 1372 mandibular trauma patients in a period of 5 years from 2014 to 2018, ramus fractures accounted for 2.4%. Of the 33 ramus fractures encountered, 21 patients were male (63.6%), while 12 were female (36.4%).
The cause of injury was road traffic accidents (RTAs) in 25 patients (75.7%), fall from height in 5 patients (15.2%), and assault in 3 (9.1%) patients. Ramus fractures due to RTA occurred more in those driving two-wheelers without helmets (16, 64%) and in light motor vehicle accidents (7, 28%) and less commonly in heavy motor vehicle accidents (2, 8%). Association with seat belt use and alcoholism could not be ascertained.
Clinical symptoms of ramus fractures included pain and swelling over the ramus region and trismus with an anterior open bite, while no step deformity could be elicited.
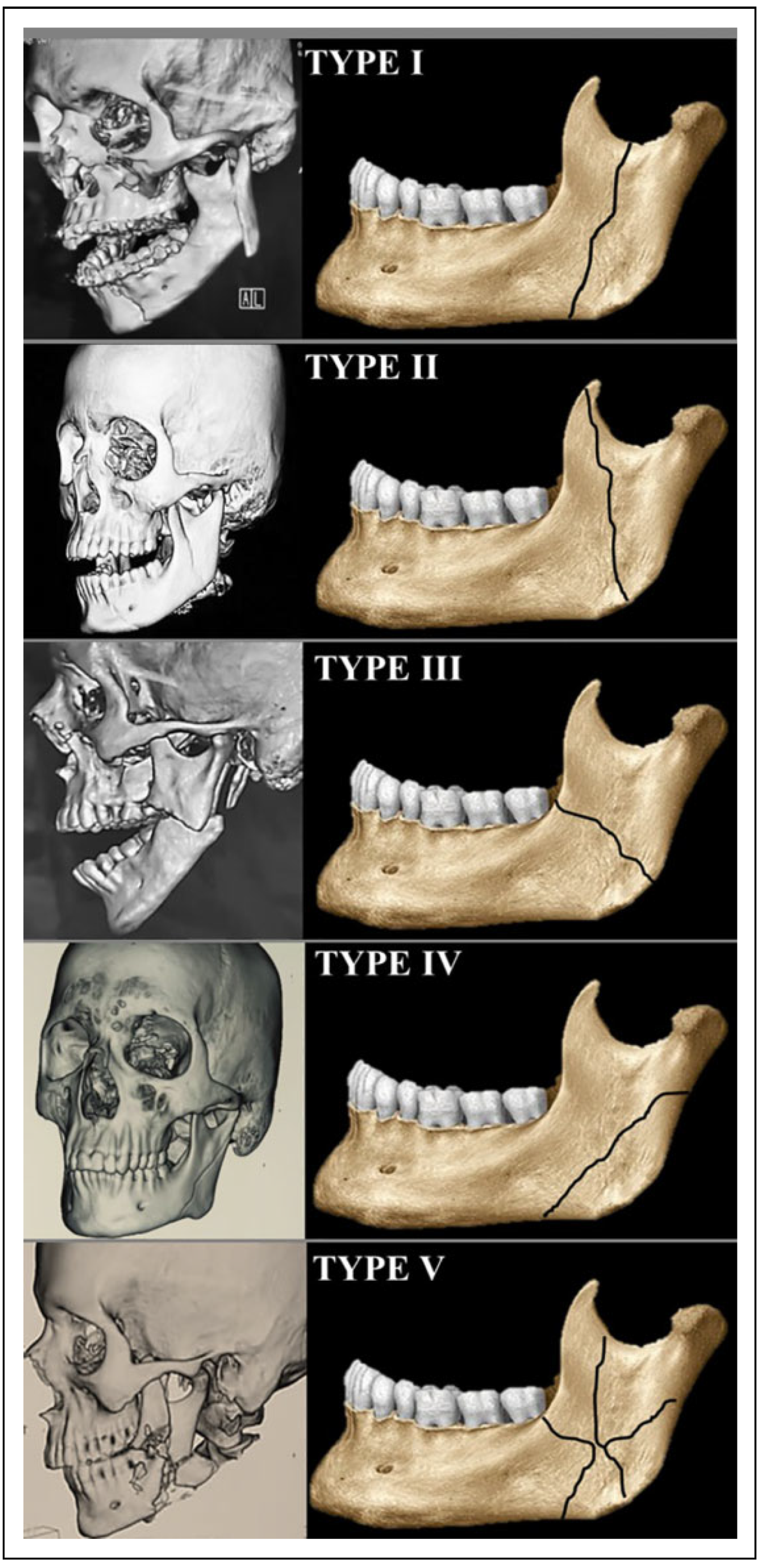
Classification— Ramus fractures were divided into 5 types according to the 5 repetitive patterns observed (
Figure 1).
Type I fractures were the most common, accounting for 48.5% (16 fractures), followed by type II in 24.2% (8 cases), but types III and IV were relatively uncommon at 9.1% and 3% (3 and 1 patient), respectively, while type V fractures were encountered in 15.2% (5 patients). Isolated ramus fractures were not seen and were always associated with other mandibular and/or maxillary fractures. Bilateral ramus fractures were never encountered.
Clinically, types I and II had tenderness around the preauricular region which was absent in other types. A wide anterior open bite was the most common in type III fractures, and a mild anterior open bite with occasional occlusal discrepancies was present in types I, II, and V fractures. Type IV fractures were mostly asymptomatic with only tenderness around the angle region. Bony overlap/crepitus was present in few cases of types I, II, and V fractures. Type III fractures had an obvious deformity/deficit at the angle of mandible and a ramal/angle deformity was present in type V fractures with obvious facial asymmetry.
Types, I, II, and IV were found to be anatomically more stable and horizontally and vertically favorable fractures owing to the pterygomasseteric sling and could be managed by closed reduction, whereas types III and V were horizontally unfavorable that necessitated open reduction and internal fixation (ORIF).
The patients managed by closed reduction were thus treated due to anatomically favorable fracture, minimal displacement, medical comorbidities, unwillingness for open reduction, or associated injuries that anyways required maxillomandibular fixation (MMF). These patients underwent MMF for 3 to 4 weeks.
Surgical management by ORIF was done for 45.5% when a satisfactory occlusion could not be achieved only by MMF or patients refused MMF or the patient was undergoing ORIF of adjacent fractures or the ramus fractures were comminuted. (15 patients: 6 of type I, 2 type II, 2 type III, and 5 type V). Incisions used for surgical exposure included transmasseteric, transparotid, retromandibular, and submandibular approaches. Complications of ORIF included mild occlusal discrepancy, transient facial nerve palsy on the operated side, infection, and hypertrophic postoperative scarring, which occurred in 3 of the operated patients (20%;
Table 1).
Discussion
The purpose of this article was to review and study ramus fractures and to devise a classification for the same.
A highly variable incidence of mandibular ramus fractures has been reported. In a densely populated country like India, a skewed incidence of 0.9% of mandibular fractures in Goa,[
7] 3.0% in Tamil Nadu,[
6] 3.09% in Maharashtra,[
1] and 2.3% in Karnataka[
8] have been reported with a comparable incidence of 2.4% in our patients. Internationally the ramus fractures account for about 1.35% in Saudi population,[
9] 3.19% in Kuwait,[
10] 6.6% in Taiwan,[
11] and 2% in the United States, Germany, and Australia.[
12,
13,
14]
The disparity and lesser observed incidence of ramus fractures can be a result of the currently unavailable structural delineation of fracture lines in this region. Also, the overlapping of the condyle, coronoid, and angle fracture in this major subsite of the mandible precludes a clear ramus fracture diagnosis. The ramus is draped by the muscles of mastication—buccally by the masseter, the lower border by the pterygomasseteric sling, lingually by the medial pterygoid, forming a muscular envelope. This facilitates minimum displacement of the mandibular ramus when fractured and thus attributes a potential to remain undiagnosed.[
1]
Earlier theories of the strong ramal buttress causing minimal ramal fractures has been abrogated by the increasing overall incidence of RTAs all around the world, with an increase in the high-velocity accidents.[
1,
6,
7,
11] This major etiologic factor due to inadequate road safety awareness, violation of speed limits, unsuitable road conditions, illmaintained vehicles with lack of essential safety features, failure to wear seat belts or helmets, violation of the highway code, driving in the wrong traffic lanes, and driving after consumption of alcohol or other intoxicating agents are the cardinal reasons for the large numbers of RTAs in India. The two-wheeler accidents predominate due to driver inattention, disregard for helmet use, and poor road conditions.[
2]
Clinical symptoms of ramus fractures include pain and swelling over the region with trismus. Step deformity is relatively uncommon owing to the overlapping muscular sling although angle deformities are present in type III fractures. Anterior open bite was wide and most common in type III fractures, and mild anterior open bite combined with occasional occlusal discrepancies is present in types I, II, and V fractures. Type IV fractures were mostly asymptomatic with tenderness around the angle. Bony overlap/ crepitus along the fracture line was present in types I, II, and V. The absence of segmental mobility and overlapping symptoms due to contiguous fractures (as ramus fractures seldom occur isolated) make radiographs indispensable for a final diagnosis and for differentiating from adjacent fractures of the mandible. Diagnosis can be easily confirmed by orthopantomograms and computerized tomography scans.[
15]
The most commonly encountered fractures are types I and II.[
1,
15,
16] The least common are types III and IV, which have been earlier described as atypical fractures of the angle[
17] due to the lack of clear demarcation of the ramus and its fracture patterns, which in turn leads to a false reporting of incidence of ramus fractures.
Management of these fractures is still an enigma and treatment algorithms continue to remain amenable to personal judgments and clinical impressions. Mandibular ramus is located between the dentulous part of mandible (angle and body region) and the edentulous part (the condyle and coronoid region).[
1] There is confusion as to whether the ramus should be considered in dentate or edentate segment and, hence, the confusion regarding its management as well.[
15] No clear indications and contraindications about open or closed treatment of these fractures exist, and can be debated at length due to a lack of evidence.[
1] More comparative and randomized controlled studies need to be carried out for the clarification of the same.
Ramus fractures are conventionally treated by closed reduction with an average MMF period of 3 weeks because of their difficult accessibility and occasional occlusal derangement.[
1,
15,
18] Disadvantages include prolonged MMF, noncompliance of patients, nutritional compromise, difficulty in oral hygiene maintenance, risk of airway embarrassment, and delayed recovery.[
18]
Ramus fractures are generally associated with other facial fractures and seldom occur isolated, similar to our patients.[
1,
15] In cases where closed reduction of ramal fractures is performed, the concomitant fractures should be subjected to ORIF.[
1]
When opting for ORIF of the fractured ramus, Risdon’s submandibular, retromandibular, transmasseteric, or transparotid incisions were used for surgical exposure. Intraoral or transbuccal approaches only give limited access in this region.[
15] ORIF provides advantages of early functional and anatomical rehabilitation with easier maintenance of a patent airway and oral hygiene with improved nutrition.[
1]
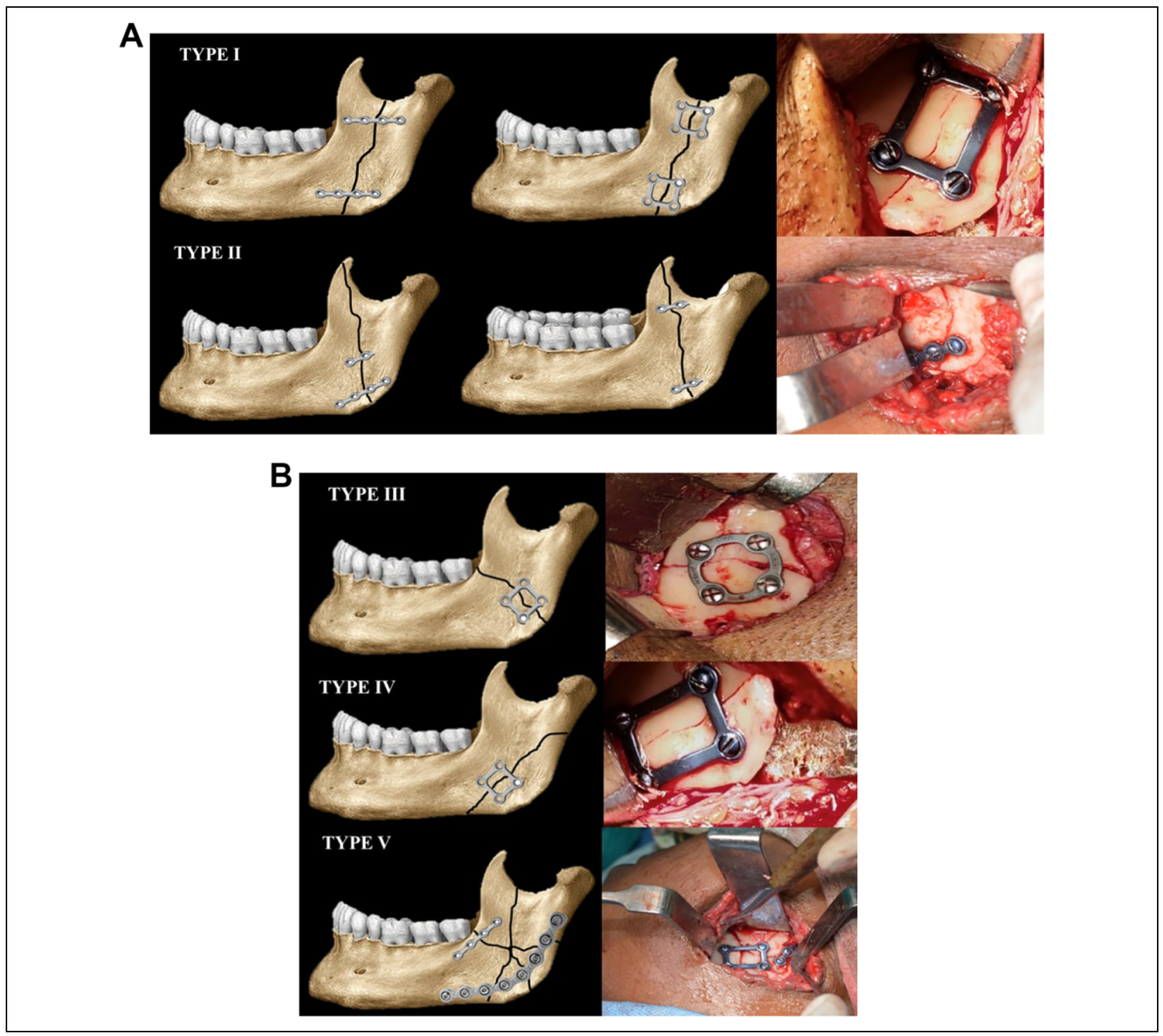
For ORIF, we fixed the ramus at 2 points because of the large rectangular surface area of the mandible as plating at the superior or inferior border only can result in torquing forces that may lead to opening up of the fracture on the opposite side.[
15] Fixation was done by load sharing fixation using 2 non-compression mini-plates or 3-D plates (more so for types I and II) and was opted for due to its larger cross-sectional area to prevent both torquing and splaying at fracture ends under the influence of the attached musculature (
Figure 2A).[
1,
16] Few authors have also advocated the use of three 2-hole non-compression mini-plates along the fracture site for 3-point stabilization owing to the length of the fracture line in such cases.[
16] However, 2 such plates at both ends of the fracture line were also found to be sufficient, conferring adequate anatomical and functional reduction. Type III fractures were efficiently managed by 3-D plates/rectangular/trapezoidal/ strut plates. Type IV fractures did not require any form of intervention due to their anatomical advantage, but in cases of gross displacement, aesthetic compromise, load sharing fixation could be acceptable. Type V fractures needed mini-plates for orientation and load bearing fixation in the form of reconstruction plates (
Figure 2B).
Essential for consideration during plating is the position of the mandibular canal. Complications with open reduction may include risk of inferior alveolar nerve paresthesia, facial palsy, parotid fistulas, or surgical scars[
1,
18] similar to 3 of our patients. Postoperative trismus due to stripping of the musculature can also occur and can be managed with the use of physiotherapy and muscle relaxants.[
1]
Satisfactory occlusion posttreatment has been reported in all cases of ramus fractures managed by closed reduction but in one patient managed by open reduction, there was mild occlusal discrepancy (type V) which improved with postoperative MMF. Complications ultimately depend on the surgeon’s expertise, availability of armamentarium, fracture classification, amount of displacement, and presence of preoperative occlusal discrepancies.
The new classification of ramus fractures was proposed because none existed till date, and this can help in delineating and accordingly managing them better. Since an overlap of ramus fractures with adjacent angle or condylar and coronoid fractures exists, this classification will help to clarify diagnosis of fractures of this area of the mandible.