In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery
Abstract
:Materials and Methods
- Fabrication of a diagnostic cast
- Wax up of the missing teeth according to prosthodontic parameters
- Fabrication of a radiographic stent
- Obtaining a CBCT scan along with the radiographic stent in place
- Fabrication of a working cast
- Determining the 3D implant position on the working cast
- Fabrication of surgical stent
- Fabrication of a diagnostic cast: Primary impression was made with alginate impression material (Alginoplast fast set; Heraeus Kulzer GmbH, Hanau, Germany) using a dentate impression tray and poured with type 3 dental stone (Mold stone type 3; PARS DENTAL Co., Iran). The diagnostic cast was fabricated as such.
- Wax up of the missing teeth according to prosthodontic parameters: A full wax up of the missing teeth in the edentulous regions was performed on the diagnostic cast using modeling wax (Star wax CB; Dentaurum Co., Germany), according to the prosthetic parameters.
- Fabrication of a radiographic stent:
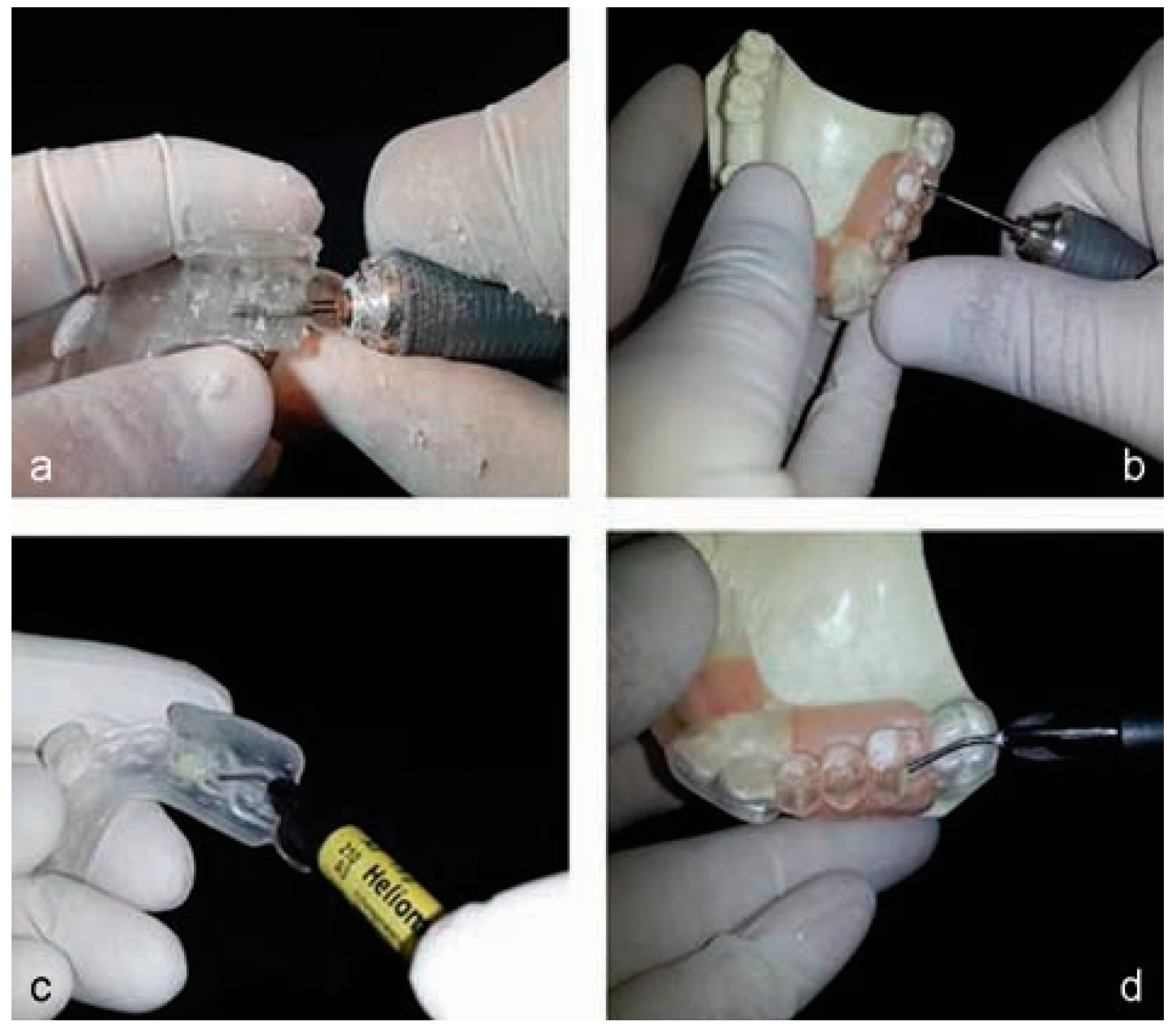
- Wax up of the radiographic stent was also performed on the diagnostic cast using modeling wax (Cavex Set Up regular modeling wax; Cavex Holland B.V., Haarlem, the Netherland). The stent margins were extended up to the depth of vestibule in the edentulous areas and over the crown margins of the adjacent teeth. The modeling wax was merged with the wax up and an acrylic model was fabricated by flasking and injection of clear, heat-cure acrylic resin (Meliodent; Heraeus-Kulzer GmbH, Wehrheim, Germany; Figure 1).
- Preparation of reference markers on the radiographicstent: Using a fissure bur (HM 33 701; Meisinger Co., Hansemannstr, Neuss, Germany), a 1-mm deep groove was prepared in the middle of the mesiodistal width of the formed crowns at the most suitable location for the sagittal view of the 3D tomographic imaging. The groove was marked by applying flowable composite resin (Heliomolar Flow, Ivoclar Vivadent Co., Amherst, NY; Figure 2) and subsequent light curing (Aria Luxe Blue Pess; T. Apadana Co., Iran). Using a rotary bur (HM 487 GX; Meisinger Co., Germany) and strong series micromotor handpiece (Saeshin Precision Co., Daegu, Korea), a thin layer was removed from beneath the radiographic stent at the edentulous areas and after ensuring there was no contact between the acrylic and patient’s gingival mucosa, a layer of flowable composite was applied beneath the stent. Radiographic stent was placed in the patient’s mouth and the flowable composite was polymerized using UV light curing unit (Aria Luxe Blue Pess; T. Apadana Co., Iran) for 20 s.
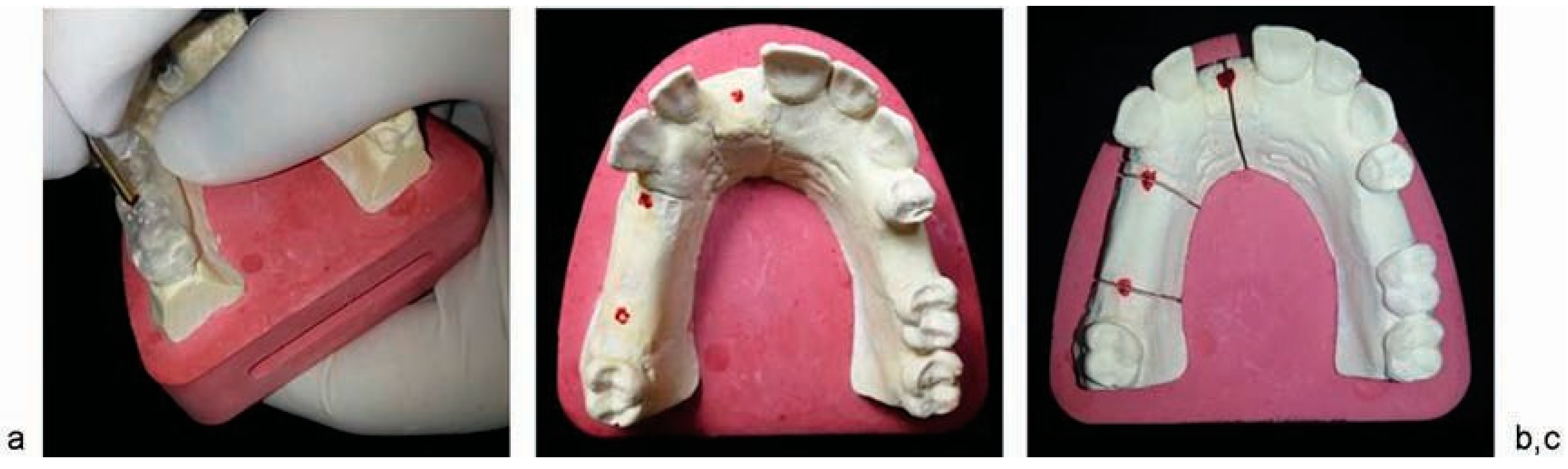
- Obtaining a CBCT scan along with the radiographic stent in place: A 3D tomogram was obtained with the radiographic stent in patient’s mouth. Using the composite marker in the groove prepared on crowns, an optimal tomographic section was chosen for the assessment of bone and softtissue structures. In the cross-sectional view, thecomposite laid beneath the radiographic stent indicates the outer surface of the soft tissue (Figure 3).
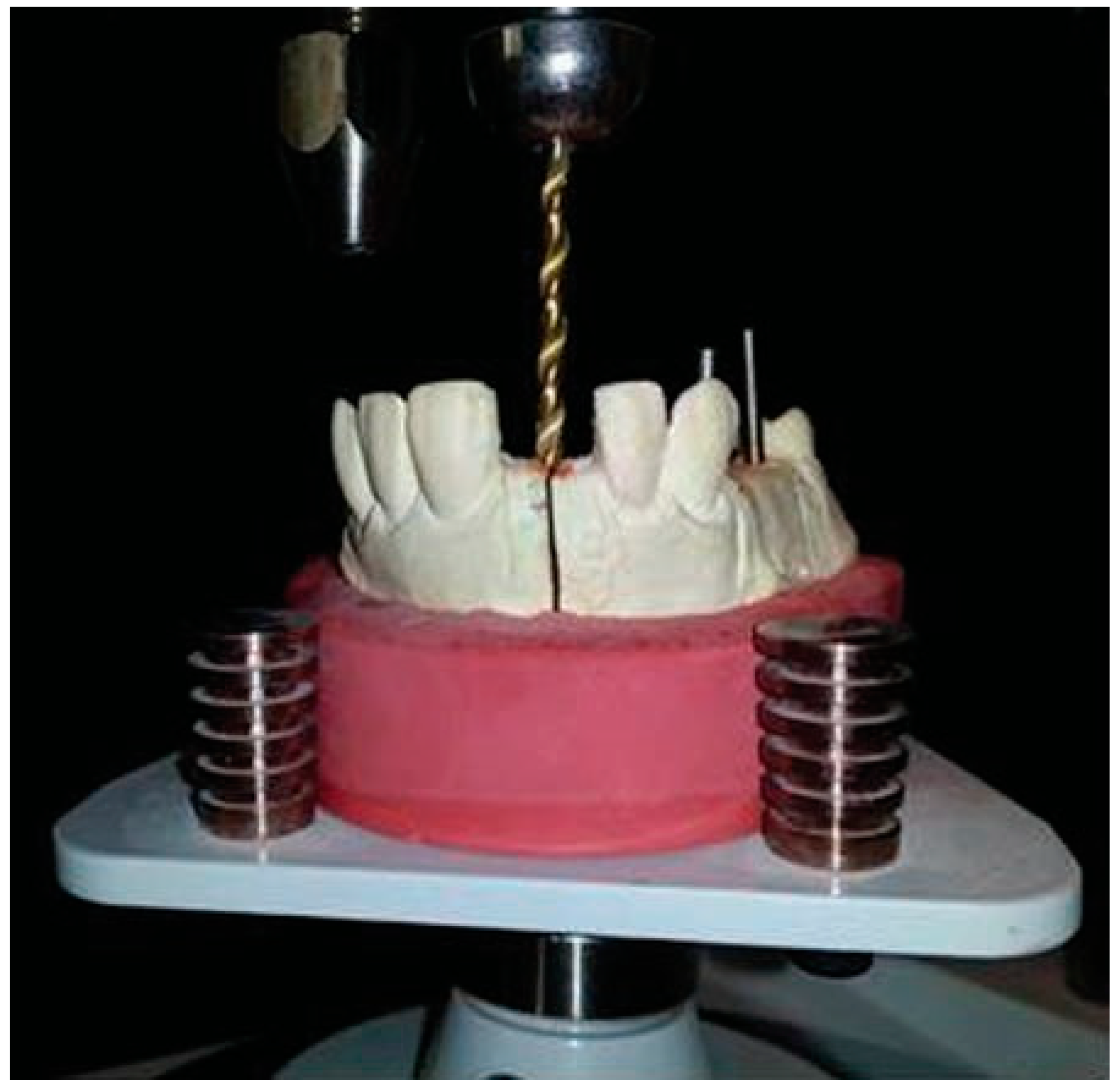
- Fabrication of surgical stent: Another impression was made from patient’s mouth using additional silicon impression material (Monopren; Kettenbach Co., Germany) and poured with dental stone (type IV stone; GC Co., Belgium). After completion of the setting time, several parallel dowel pins were placed in the impression using the Pindex method to provide a master cast with individually removable dies at the site of hypothetical implants. The base was then poured with dental stone (Figure 4).
- Determining the 3D implant position on the working cast:
- Determination of the center of implant placement: A round-end fissure bur (NO 882; Teeskavan Co., Iran) was inserted into the crown center along the longitudinal axis of the crown until reaching the cast surface. The tip of a pin was soaked with fit checker and inserted into the created path to mark the prosthetically optimal point for implant placement at the center of the final crown. Three sections were made at the center of the marked area to provide individually removable segments (Figure 5).
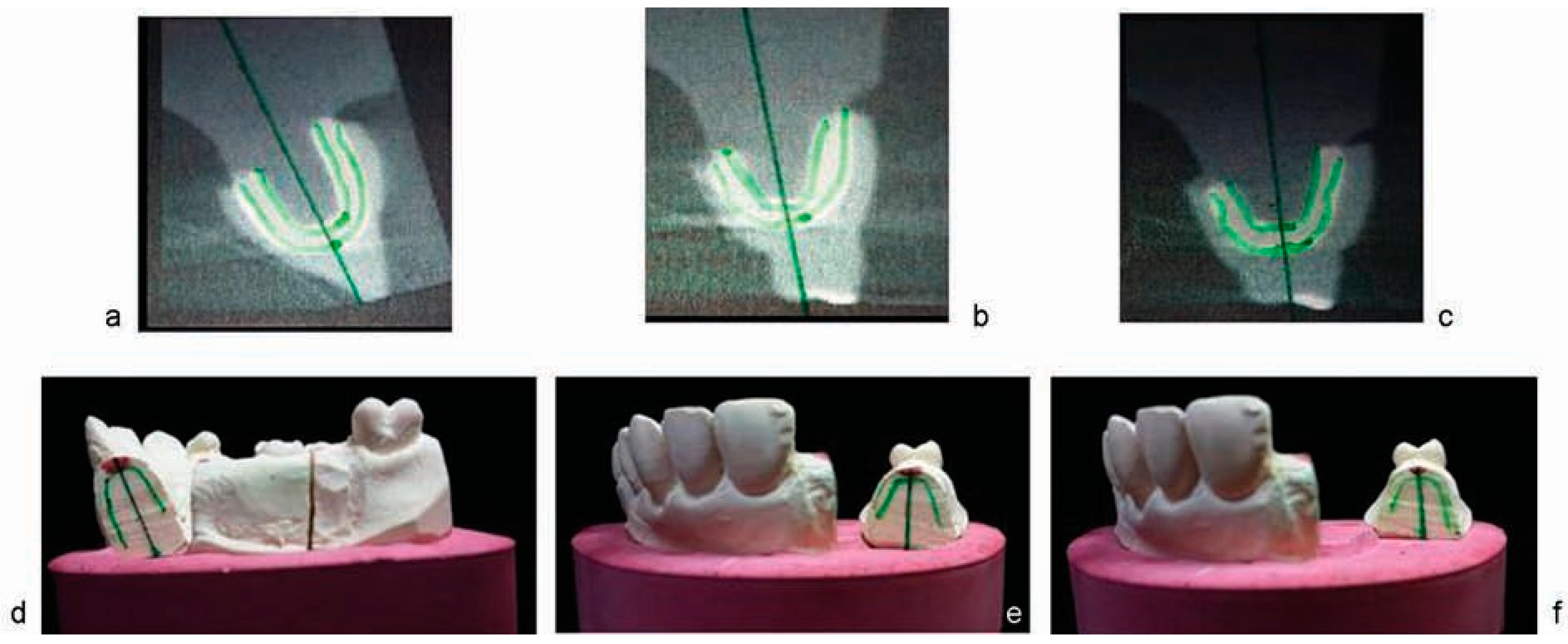
- Determination of the bucco-palatal direction of implant insertion: A transparent sheet was superimposed on the tomogram of the implant site and fixed. The internal borders of the soft tissue and external borders of bone were outlined on the sheet. Using the lateral view of the crown and bone, the best bucco-palatal position for implant insertion was determined by drawing a line. The coronal point of the line corresponded to the predetermined central point (Figure 6). The transparent sheet was cut along the soft-tissue indicator line and the remaining piece was adapted to the sectioned cast. The bone indicator lines and the hypothetical long axis of the implant were also transferred to the cast. Considering the preset mesiodistal and buccolingual position of implant and the direction of its long axis, the osteotomy hole was simulated on the cast using a surveyor and milling machine (Saeshin Precision Co.). The hole measured 2 mm in diameter with a depth at the level of the cast base. To ensure optimal accuracy, the cast was transferred to a surveyor with an analyzer rod along the hypothetical line indicative of the long axis of implant. The surveyor was fixed in this position and the hole was prepared by the milling machine (Figure 7).
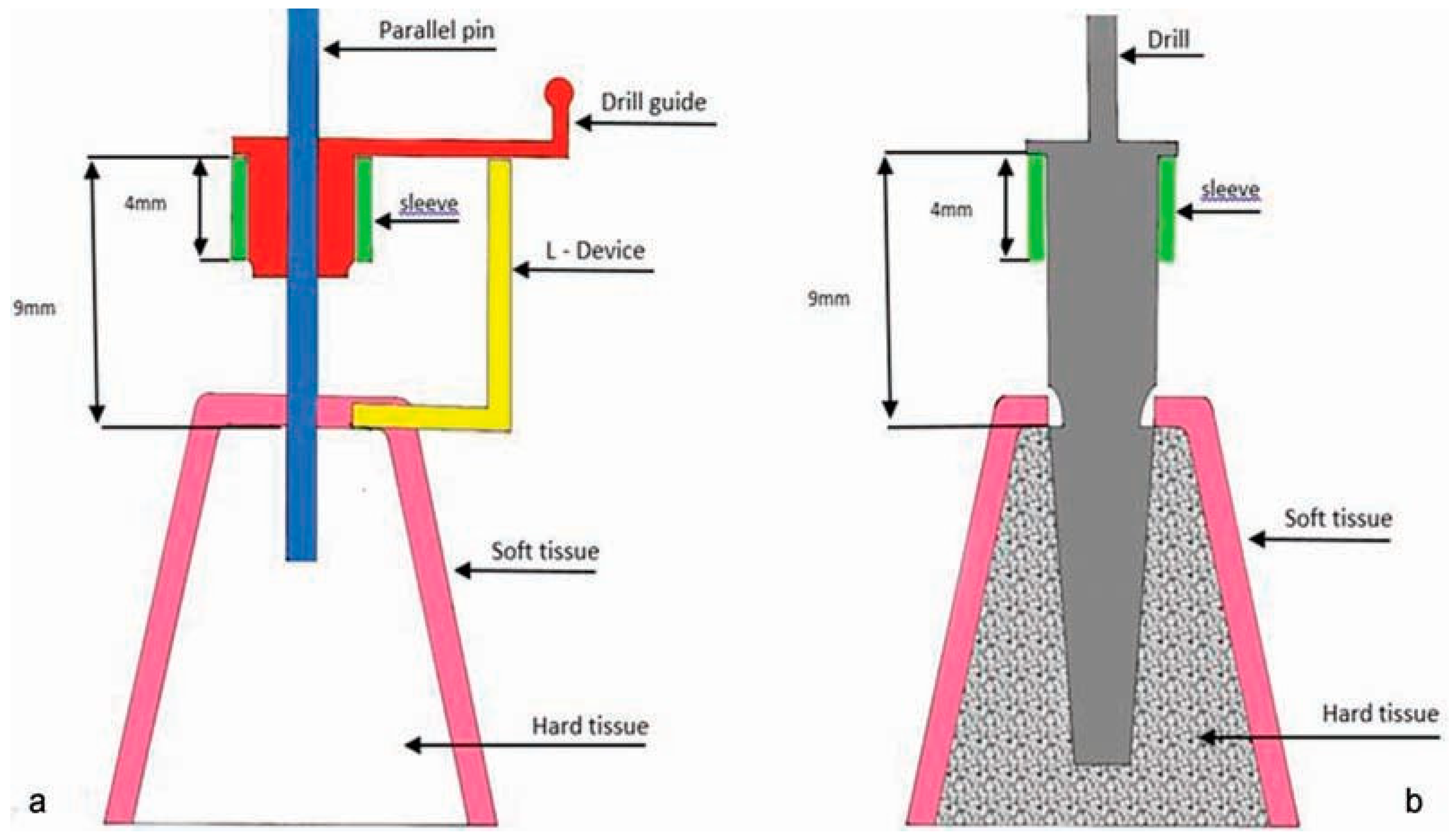
- Determining the penetration depth of drill: The soft-tissue thickness, sleeve height, and the size of the possible gap between the sleeve and the underlying soft tissue were transferred to the surgical stent to precisely determine the penetration depth of drill and consequent depth of implant insertion. For this purpose, a horizontal line was drawn tangent to the crestal bone indicator line and perpendicular to the long axis of the implant path. An L-shaped guide was cut out of a plastic sheet in such way that the length of its long arm was 9 mm. The 9-mm length was selected because the drill stopper height was 9 mm in the implant system used (Noble Guide, Noble Biocare Co., Sweden). The short arm of the L-shaped guide was placed on bone crest tangent to the hypothetical horizontal line. The parallel pin was placed in the osteotomy hole parallel to the long arm of the L-shaped guide (Figure 8). The sleeve was fixed to the drill guide using wax. The complex of drill guide and sleeve was placed over the pin and the drill guide shank was fixed to the superior margin of the long arm of L-shaped guide. In other words, the drill guide and sleeve had 9 mm height similar to the length of the long arm of L-shaped guide. Thus, when the drill guide–sleeve was placed on the gingival tissue, the drill stopper corresponded to the coronal position of sleeve and pin guide and the actual height of drill would enter in the bone (Figure 9).
- Fabrication of surgical stent: This was done with two different materials. We used heat-cure acrylic resin (Meliodent heat-curing polymer; Meliodent, Heraeus-Kulzer GmbH, Wehrheim, Germany) and pressure pot in areas other than the surgical site and clear cold-cure acrylic resin (cold-curing polymer; Meliodent, Heraeus-Kulzer GmbH, Wehrheim, Germany) at the site of implant placement. By merging these two components, the sleeve was fixed in the acrylic resin in such a way that the distance from the sleeve crest to the bone crest was 9 mm (Figure 10). The polished surgical stent was placed in the patient’s mouth and the drilling was completed using guided surgery drills specific for each implant system.



Results

Discussion




- Inclusion of the thickness and anatomy of the soft tissue in designing and manufacturing the surgical model
- Simultaneous use of 3D data acquired from the tomogram and diagnostic cast
- Determining the 3D position of bone based on the available bone on the 3D tomogram and position of the final crown (diagnostic cast wax up)
- Introducing an affordable and easily accessible technique not requiring specific laboratory equipment
- Compatibility with different implant systems
- Applicability in both flap and flapless surgeries
- Applicable for placement of one or several implants
- High accuracy and safety
- Requiring tomographic imaging data
- Time required for preparation of surgical model
- Requiring sleeve and guided surgery drills specific for each implant system
- Requiring intraoral references such as the adjacent teeth in partially edentulous patients or fixation of surgical model in fully edentulous cases
Conclusion
References
- Schneider, D.; Marquardt, P.; Zwahlen, M.; Jung, R.E. A systematic review on the accuracy and the clinical outcome of computerguided template-based implant dentistry. Clin Oral Implants Res 2009, 20 (Suppl. S4), 73–86. [Google Scholar] [CrossRef] [PubMed]
- Akça, K.; Iplikçioğlu, H.; Cehreli, M.C. A surgical guide for accurate mesiodistal paralleling of implants in the posterior edentulous mandible. J Prosthet Dent 2002, 87, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Tsuzuki, T.; Matsuura, T.; Kido, H.; Ishikawa, M.; Ukon, S.; Sato, H. New fabrication system for dental implant surgical stents: Time-saving laboratory technique using a light-curing resin and transparent artificial teeth. Clin Implant Dent Relat Res 2001, 3, 107–110. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Lee, J.W.; Lim, S.H.; Kim, Y.H.; Kim, M.K. Verification of the usability of a navigation method in dental implant surgery: In vitro comparison with the stereolithographic surgical guide template method. J Craniomaxillofac Surg 2014, 42, 1530–1535. [Google Scholar] [CrossRef] [PubMed]
- de Almeida, E.O.; Pellizzer, E.P.; Goiatto, M.C.; et al. Computer-guided surgery in implantology: Review of basic concepts. J Craniofac Surg 2010, 21, 1917–1921. [Google Scholar] [CrossRef] [PubMed]
- Widmann, G.; Bale, R.J. Accuracy in computer-aided implant surgery—A review. Int J Oral Maxillofac Implants 2006, 21, 305–313. [Google Scholar] [PubMed]
- Whitehouse, J. Technology helps an “amateur” place implants. Dent Today 2008, 27, 120–124. [Google Scholar] [PubMed]
- Van Assche, N.; Vercruyssen, M.; Coucke, W.; Teughels, W.; Jacobs, R.; Quirynen, M. Accuracy of computer-aided implant placement. Clin Oral Implants Res 2012, 23 (Suppl. S6), 112–123. [Google Scholar] [CrossRef] [PubMed]
- Sicilia, A.; Botticelli, D.; Working Group 3. Computer-guided implant therapy and soft- and hard-tissue aspects. The Third EAO Consensus Conference 2012. Clin Oral Implants Res 2012, 23 (Suppl. S6), 157–161. [Google Scholar] [CrossRef] [PubMed]
- Hultin, M.; Svensson, K.G.; Trulsson, M. Clinical advantages of computer-guided implant placement: A systematic review. Clin Oral Implants Res 2012, 23 (Suppl. S6), 124–135. [Google Scholar] [CrossRef] [PubMed]
- Azari, A.; Nikzad, S. Flapless implant surgery: Review of the literature and report of 2 cases with computer-guided surgical approach. J Oral Maxillofac Surg 2008, 66, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Neugebauer, J.; Stachulla, G.; Ritter, L.; et al. Computer-aided manufacturing technologies for guided implant placement. Expert Rev Med Devices 2010, 7, 113–129. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, H.J.; Eitner, S.; Rothamel, D.; Wichmann, M.; Zöller, J.E. Possibilities and limitations of implant placement by virtual planning data and surgical guide templates. Int J Comput Dent 2012, 15, 9–21. [Google Scholar] [PubMed]
- Elsyad, M.A. A new surgical template with a handpiece positioner for use during flapless placement of four dental implants to retain a mandibular overdenture. J Prosthodont 2012, 21, 573–577. [Google Scholar] [CrossRef]
© 2016 by the author. The Author(s) 2016.
Share and Cite
Karami, D.; Alborzinia, H.R.; Amid, R.; Kadkhodazadeh, M.; Yousefi, N.; Badakhshan, S. In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery. Craniomaxillofac. Trauma Reconstr. 2017, 10, 246-254. https://doi.org/10.1055/s-0036-1584891
Karami D, Alborzinia HR, Amid R, Kadkhodazadeh M, Yousefi N, Badakhshan S. In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery. Craniomaxillofacial Trauma & Reconstruction. 2017; 10(3):246-254. https://doi.org/10.1055/s-0036-1584891
Chicago/Turabian StyleKarami, Daryoush, Hamid Reza Alborzinia, Reza Amid, Mahdi Kadkhodazadeh, Navid Yousefi, and Sarina Badakhshan. 2017. "In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery" Craniomaxillofacial Trauma & Reconstruction 10, no. 3: 246-254. https://doi.org/10.1055/s-0036-1584891
APA StyleKarami, D., Alborzinia, H. R., Amid, R., Kadkhodazadeh, M., Yousefi, N., & Badakhshan, S. (2017). In-Office Guided Implant Placement for Prosthetically Driven Implant Surgery. Craniomaxillofacial Trauma & Reconstruction, 10(3), 246-254. https://doi.org/10.1055/s-0036-1584891


