Orbitocerebral impalement by inanimate objects is a relatively uncommon event; however, transorbital trauma comprises up to 25% of penetrating head injuries in adult patients [
1]. There have been previous case reports published on various objects causing orbitocerebral impalement, including wood fragments and branches [
2], pencils [
3], pens [
4], windshield wiper control indicator [
4], and an industrial hook [
4] (
Table 1). The aim of this case report is to describe the unique mechanism of a remarkable, deep orbitocerebral impalement from a walker brake lever through the orbital roof after a fall from standing. This case report protocol was reviewed by the Duke University Medical Center Institutional Review Board (IRB; Protocol # Pro00065824), and deemed exempt from formal review as no identifiable patient health information is supplied. A waiver of consent was also granted by the IRB.
Case Discussion
An 82-year-old woman with a history of vascular dementia presented to our emergency department after a fall from standing while at her assisted living facility onto her walker. She fell face first onto the walker resulting in impalement of the walker brake lever through her right orbit. Emergency medical services were immediately called and found her conscious, oriented, and only reporting right orbital pain.
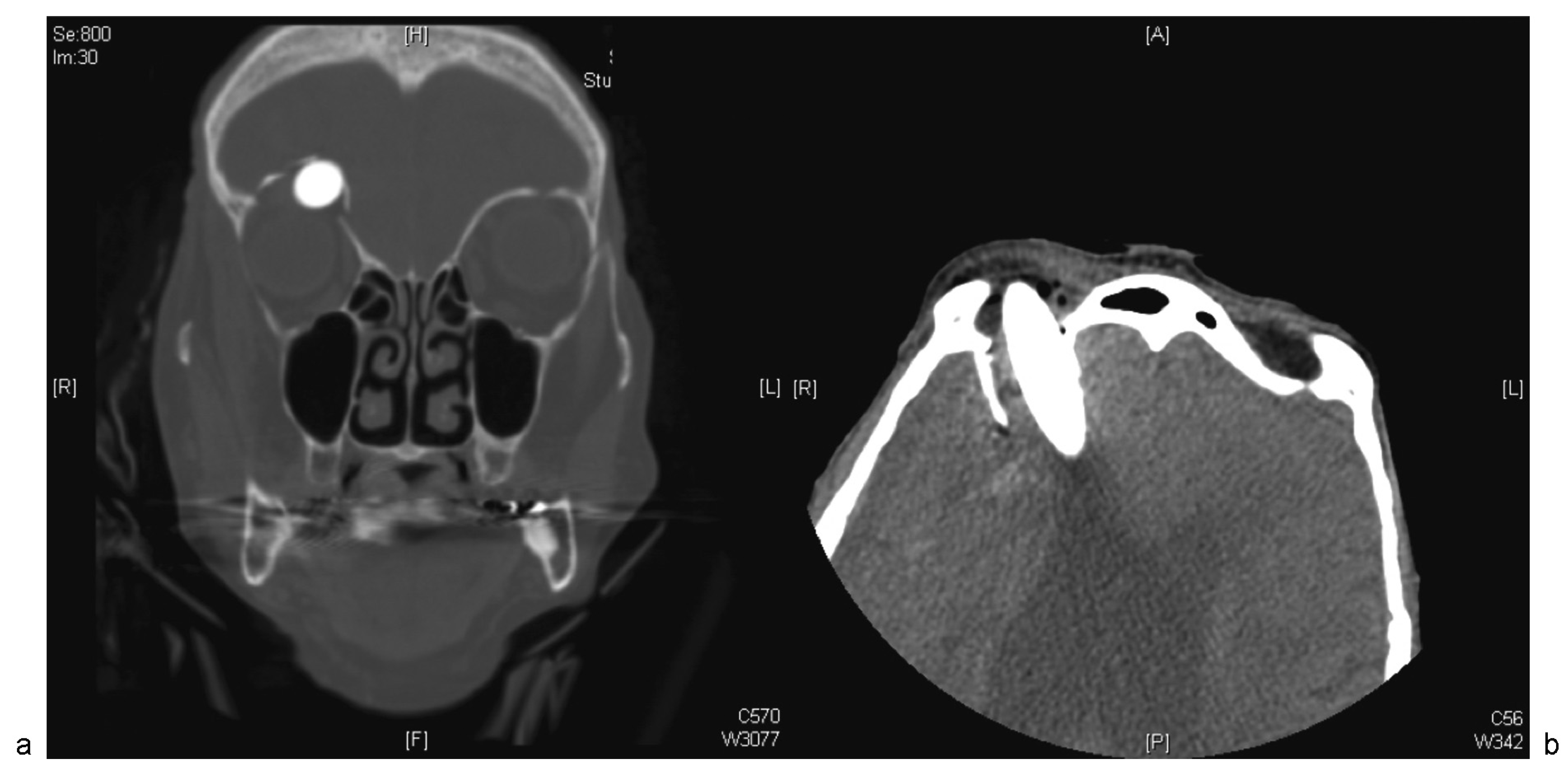
Upon arrival, the patient’s Glasgow Coma Scale (GCS) was 14 with an obvious metallic object embedded into the right superomedial aspect of the orbit. There was significant periorbital ecchymosis and edema, and clear fluid drainage around the entry site. A spot X-ray skull film was rapidly completed which showed a metallic object traversing her right orbit and into the right anterior cranial cavity. Empiric intravenous antibiotics were administered. A computed tomographic (CT) scan of the head and facial bones with three-dimensional reconstruction was completed along with CT angiography (CTA) to assess for vascular disruption (
Figure 1 and
Figure 2). The CT scan demonstrated a penetrating metal rod with a 3-cm intracranial segment terminating in the right frontal lobe. The scan was also notable for a comminuted right orbital roof fracture with herniation of the infraorbital fat and superior rectus muscles into the anterior cranial fossa. The globe and optic nerve were intact. The CTA demonstrated no evidence of arterial injury; however, the distal rod tip was only 1.5 cm lateral to the right anterior cerebral artery (ACA), and 1.4 cm superior to the right M1 segment of the middle cerebral artery (MCA).
The patient’s do not resuscitate (DNR)/do not intubate (DNI) status was temporarily lifted, and she was taken to the operating room emergently for a combined surgical repair with neurosurgery, neuroanesthesiology, craniomaxillofacial surgery, and ophthalmology. A rapid sequence induction of anesthesia was performed. The metal brake lever was manually stabilized by an assistant during the intubation to prevent possible cervical spinal cord injury and to prevent the metal brake lever from penetrating deeper into the brain. Due to the limited workspace around the patient’s mouth and oropharynx and to avoid the need to extend her neck, the airway was visualized using a MAC McGRATH video laryngoscope (Covidien/Medtronic, Minneapolis, MN). The airway was secured with a 7.0-cuffed endotracheal tube. The endotracheal tube was then carefully secured in place while an assistant stabilized the metal brake rod in the orbit. Anesthesia was then maintained with infusions of propofol and remifentanil rather than a volatile agent, to avoid the potential cerebral vasodilatory effects (and the possible increase in intracranial pressure) from volatile anesthetic use. A phenylephrine infusion was titrated to maintain the patient’s mean arterial pressure in the range of 70 to 90 mm Hg.
The patient’s head was prepped and draped, and the neurosurgery team performed a frontal craniotomy via a coronal incision to dissect around the metal rod. Upon satisfactory 360-degree dissection, the rod was slowly removed from the orbit and the cavity was explored and irrigated. The dura was repaired primarily, and the craniotomy bone flap was reattached with titanium miniplates. The craniomaxillofacial surgery team then repositioned the superior periorbital contents, and the fractured orbital roof fragments were placed in alignment with the remainder of the cranial vault. A titanium mesh plate was contoured to the dimensions of the superior orbit, and secured in place over the defect with screws. Finally, the ophthalmology service performed a 360-degree conjunctival peritomy, which revealed globe dehiscence and uveal prolapse. A small amount of scleral thinning with tissue loss was noted and closed with running suture. The patient was then transported to the neurocritical care unit intubated and sedated in stable condition.
On postoperative day 2, an external ventricular drain was placed to decompress the ventricles and reduce the likelihood of a cerebrospinal fluid (CSF) leak. On postoperative day 3, multidisciplinary discussions were completed with the family regarding goals of care and a do not resuscitate order was implemented at the family’s wishes with a plan to extubate. Her sedation was weaned and her neurological examination determined that she localized to pain, but demonstrated no other purposeful movements. On postoperative day 5, the family wished to withdraw care and provided comfort measures only in the setting of significant preexisting debility and poor prognosis for neurological recovery. The patient passed away soon thereafter.
Management Discussion
Penetrating orbitocerebral impalement is an uncommon cause of head and neck trauma in adult patients [
1]. Transorbital impalement with different objects has been described in the past [
2,
3,
4]. In one case series, victims of transorbital trauma were most often males, younger than 19 years and with entry sites medial and through the medial canthus [
2]. If orbitocerebral impalement is suspected, management entails prompt referral to a trauma facility with neurosurgical, neuroanesthesiology, craniomaxillofacial, and ophthalmological expertise. Upon initial examination in a tertiary facility, a noncontrasted maxillofacial CT scan is obtained followed by CTA to rule out vascular injury [
4]. If the object is still in place, removal of the foreign body under general anesthesia, subsequent repair of the dura as required, and craniomaxillofacial reconstruction is then completed. In this article, we describe the first known report of a patient falling onto a wheel chair/walker resulting in a significant intracranial foreign body with subsequent management as outlined earlier.
Despite the rarity of incidence, the thin bony components of the orbit may allow for passage of a foreign body through the orbit and into the anterior cranial vault with little resistance. After an object engages the orbit, the pyramidal shape of the orbit directs objects toward its apex and through to the anterior cranial cavity either via the superior or inferior orbital fissure, orbital roof or optic canal [
2]. An excellent review of the pathophysiology of this mechanism by Turbin et al. classifies the zones of entry of penetrating orbitocerebral impalements into four predictable locations [
2]. Zone 1 includes central, lateral, upper eyelid, or superior conjunctival entry points. Zone 2 includes central, lateral, lower eyelid, or inferior entry points. Zone 3 includes all medial and canthal penetrations, and zone 4 entry sites are via nonmedial upper and lower eyelid and conjunctival lacerations (zones 1 and 2;
Figure 3) [
2]. The most common zone of entry is zone 3, and our patient is no exception [
2].
Initial management of penetrating orbitocerebral impalement first involves the fundamentals of trauma care including the primary and secondary surveys. If the patient arrives with the object in place, it is to be left in place and stabilized. Expedient imaging is crucial for characterizing the location and depth of the foreign body relative to important extracranial and intracranial neurovascular structures. Failure to detect intracranial injuries may lead to neurological deficits and death. Orbitocerebral impalement increases the risk of intracranial arterial injury, especially if the entry wound is over the frontobasal-temporal region, involving bilateral hemispheres, and close in proximity to the circle of Willis [
5]. As such, CTA is recommended prior to surgical removal of the object. In a review of the literature, routine use of arteriography has been lacking (
Table 1). The importance of CTA imaging is twofold—securing the airway and removing the impaled object. CTA imaging is necessary to understand the three-dimensional relationship between the object and nearby blood vessels, so as to determine the probability of the object injuring major cerebral blood vessels or fiber tracts. For example, at-risk regions include the corticospinal tract and pathways to motor cortex, arcuate fasciculus, or to Broca area. This imaging provides rationale to understand how important it is to immobilize the object for both the surgical and the anesthesiology teams. Armed with this information, the teams can gauge the probability of sudden major cerebrovascular bleeding, and prepare appropriately for this possibility. We have prepared a simple management algorithm that outlines the place for CT/CTA in the initial management of this injury (
Figure 4).
Surgical management of these patients is composed of removal of the foreign body and closure or repair of the subsequent defect. Considering the proximity of the globe and extracranial facial skeleton, a combined neurosurgical approach with ophthalmology, craniomaxillofacial surgery, and neuroanesthesiology is warranted. Postoperatively, patients will need neurointensive care monitoring and vigilant surveillance for CSF leak and infection, as well as posttraumatic epilepsy [
6]. The late development of pseudoaneurysms is another complication of penetrating cerebral trauma that requires a low index of suspicion [
4]. Penetrating cerebral trauma portends a relatively good prognosis if immediate and excellent care is provided and the patient survives past the first week. In a large case review of penetrating cerebral trauma from the Vietnam conflict, only 8% of patients who survived past the first week since injury died [
6]. Of those deaths after the first week, one-third occurred in the first 3 months since injury.
Conclusion
Our report illustrates an unusual case of orbitocerebral impalement from a brake lever of a wheelchair after a fall from standing. Management of these injuries requires stabilization of the object to limit further injury and expedient transfer to a tertiary care facility with neurosurgical, neuroanesthesiology, ophthalmologic, and craniomaxillofacial surgery expertise. CT imaging with an angiogram is critical to establish the location of the foreign body as well as possible arterial disruption. Reconstruction after object removal is often needed, and the prognosis for these patients is good if they are able to survive the first week after injury.