Concomitant “Ear Bleed and Styloid Fracture”: An Unusual Complication of Impacted Mandibular Third Molar Removal
Abstract
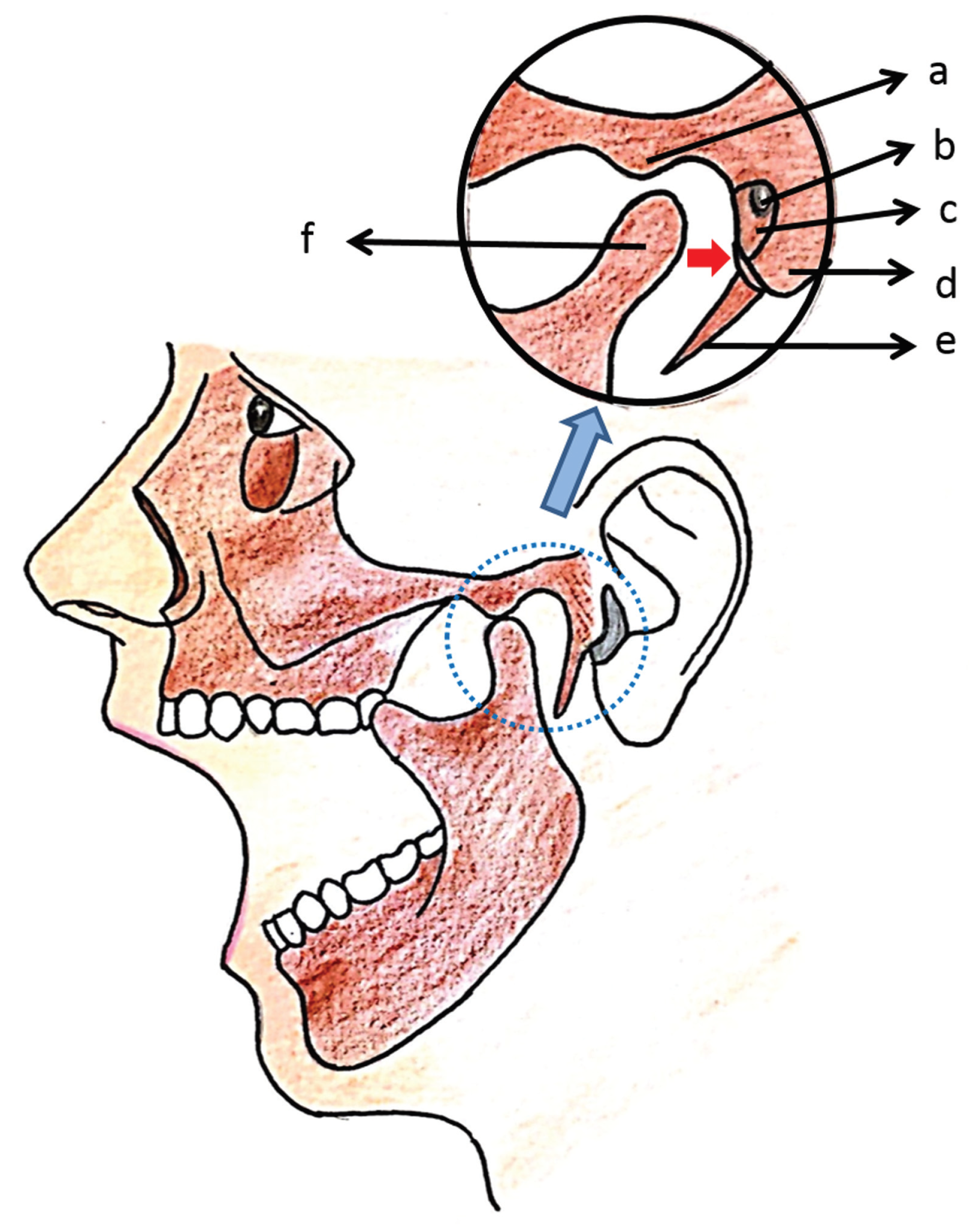
:Case Report
Discussion
Conclusion
Conflicts of Interest
Patient Consent
References
- Chiapasco, M.; De Cicco, L.; Marrone, G. Side effects and complications associated with third molar surgery. Oral Surg Oral Med Oral Pathol 1993, 76, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Martis, C.; Karakasis, D. Bleeding from the ear in maxillofacial injuries. J Maxillofac Surg 1974, 2, 126–128. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; He, D.; Yang, C. Which craniofacial fractures are associated with external auditory canal bleeding? J Oral Maxillofac Surg 2014, 72, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Bayram, B.; Aydin, E.; Uckan, S. External auditory canal injury following removal of an impacted third molar: A case report. J Oral Maxillofac Surg 2007, 65, 1372–1374. [Google Scholar] [PubMed]
- Reichart, P.A.; Sooss, W. Fracture of the styloid process of the temporal bone: An unusual complication of dental treatment. Report of a case. Oral Surg Oral Med Oral Pathol 1976, 42, 150–154. [Google Scholar] [PubMed]
- Armao, T.A. Diagnosis and treatment of a styloid fracture. Oral Surg Oral Med Oral Path Oral Radiol 1960, 13, 1423–1424. [Google Scholar] [CrossRef]
- Dubey, K.N.; Bajaj, A.; Kumar, I. Fracture of the styloid process associated with the mandible fracture. Contemp Clin Dent 2013, 4, 116–118. [Google Scholar] [CrossRef] [PubMed]
- Miloro, M. Fracture of the styloid process: A case report and review of the literature. J Oral Maxillofac Surg 1994, 52, 1073–1077. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.R.; Cherry, J.E. Traumatic Eagle’s syndrome: Report of a case and review of the literature. J Oral Maxillofac Surg 1988, 46, 606–609. [Google Scholar] [PubMed]
- Raman, U.; Samraj, T. Fracture of the styloid process associated with mandibular fracture. A case report. Int J Oral Maxillofac Surg 1990, 19, 350–351. [Google Scholar] [CrossRef] [PubMed]
- Babbitt, J.A. Fracture of the styloid process and its tonsil fossa complications, with report of a case. Ann Otol Rhinol Laryngol 1993, 42, 789–798. [Google Scholar] [CrossRef]
- Steinmann, E.P. A new light on the pathogenesis of the styloid syndrome. Arch Otolaryngol 1970, 91, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Vasconcelos, B.C.; Rocha, N.S.; Cypriano, R.V. Posterior dislocation in intact mandibular condyle: An unusual case. Int J Oral Maxillofac Surg 2010, 39, 89–91. [Google Scholar] [CrossRef] [PubMed]
- Psimopoulou, M.; Antoniades, K.; Magoudi, D.; Karakasis, D. Tympanic plate fracture following mandibular trauma. Dentomaxillofac Radiol 1997, 26, 344–346. [Google Scholar] [PubMed]
- Loh, F.C.; Tan, K.B.; Tan, K.K. Auditory canal haemorrhage following mandibular condylar fracture. Br J Oral Maxillofac Surg 1991, 29, 12–13. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, G.R.; Scopp, I.W. Radiographic interpretation of calcified stylomandibular and stylohyoid ligaments. J Prosthet Dent 1973, 30, 330–334. [Google Scholar] [CrossRef] [PubMed]
- Blythe, J.N.; Matthews, N.S.; Connor, S. Eagle’s syndrome after fracture of the elongated styloid process. Br J Oral Maxillofac Surg 2009, 47, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Frommer, J. Anatomic variations in the stylohyoid chain and their possible clinical significance. Oral Surg Oral Med Oral Pathol 1974, 38, 659–667. [Google Scholar] [PubMed]
- Gayathri, G.; Elavenil, P.; Sasikala, B.; Pathumai, M.; Krishnakumar Raja, V.B. ‘Stylo-mandibular complex’ fracture from a maxillofacial surgeon’s perspective—Review of the literature and proposal of a management algorithm. Int J Oral Maxillofac Surg 2016, 45, 297–303. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the author. The Author(s) 2016.
Share and Cite
Raja, K.; Gopi, G.; Panneerselvam, E.; Ramamoorthy, J.; Doss, G.T.; Sharma, A.R. Concomitant “Ear Bleed and Styloid Fracture”: An Unusual Complication of Impacted Mandibular Third Molar Removal. Craniomaxillofac. Trauma Reconstr. 2017, 10, 212-215. https://doi.org/10.1055/s-0036-1592086
Raja K, Gopi G, Panneerselvam E, Ramamoorthy J, Doss GT, Sharma AR. Concomitant “Ear Bleed and Styloid Fracture”: An Unusual Complication of Impacted Mandibular Third Molar Removal. Craniomaxillofacial Trauma & Reconstruction. 2017; 10(3):212-215. https://doi.org/10.1055/s-0036-1592086
Chicago/Turabian StyleRaja, Krishnakumar, Gayathri Gopi, Elavenil Panneerselvam, Jegatheesan Ramamoorthy, Guruprasad Thulasi Doss, and Aditi Rajendra Sharma. 2017. "Concomitant “Ear Bleed and Styloid Fracture”: An Unusual Complication of Impacted Mandibular Third Molar Removal" Craniomaxillofacial Trauma & Reconstruction 10, no. 3: 212-215. https://doi.org/10.1055/s-0036-1592086
APA StyleRaja, K., Gopi, G., Panneerselvam, E., Ramamoorthy, J., Doss, G. T., & Sharma, A. R. (2017). Concomitant “Ear Bleed and Styloid Fracture”: An Unusual Complication of Impacted Mandibular Third Molar Removal. Craniomaxillofacial Trauma & Reconstruction, 10(3), 212-215. https://doi.org/10.1055/s-0036-1592086


