Basal Cell Adenoma of Retromolar Region from Minor Salivary Gland Origin in a 45-Year-Old Female: A Case Report
Abstract
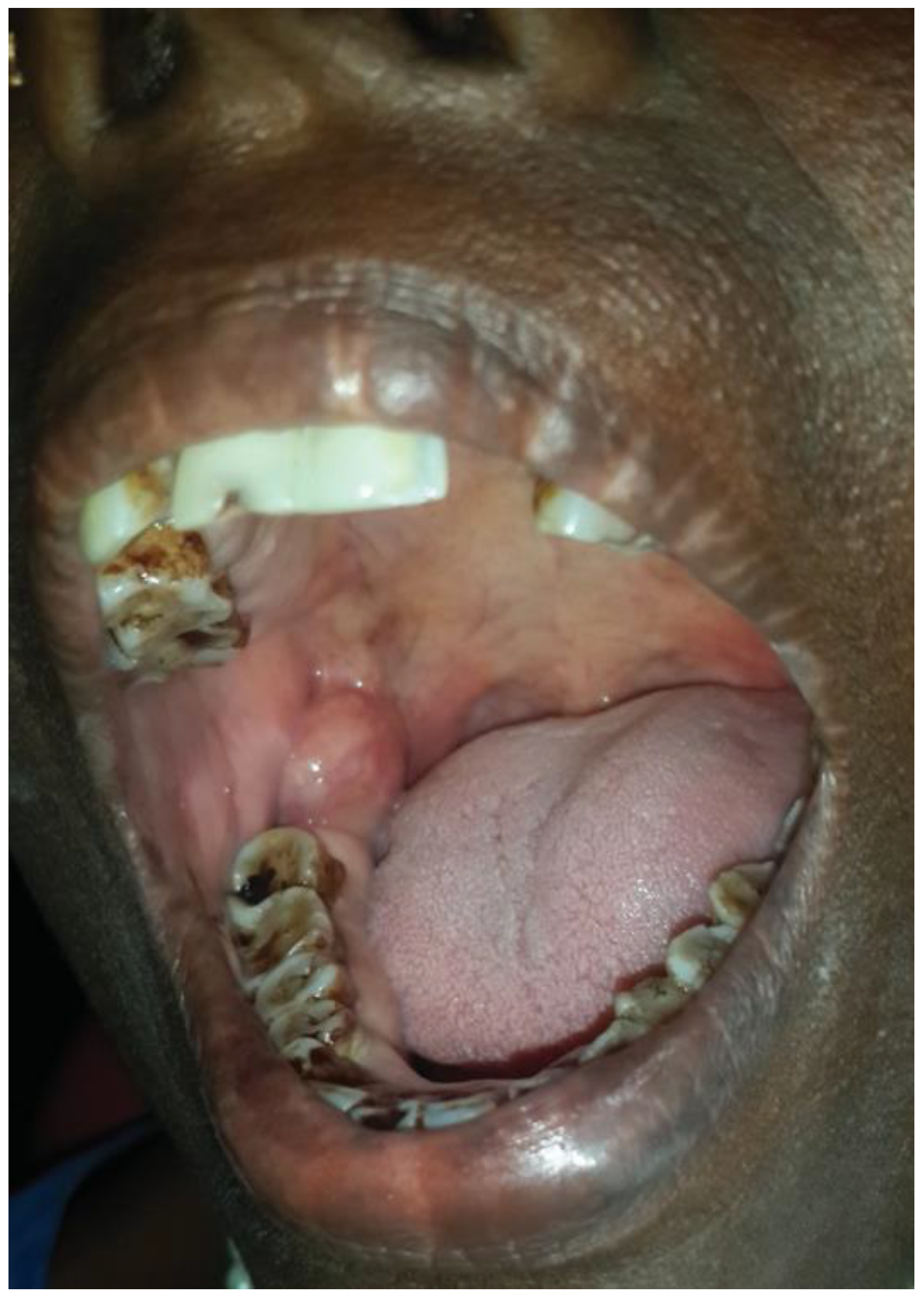
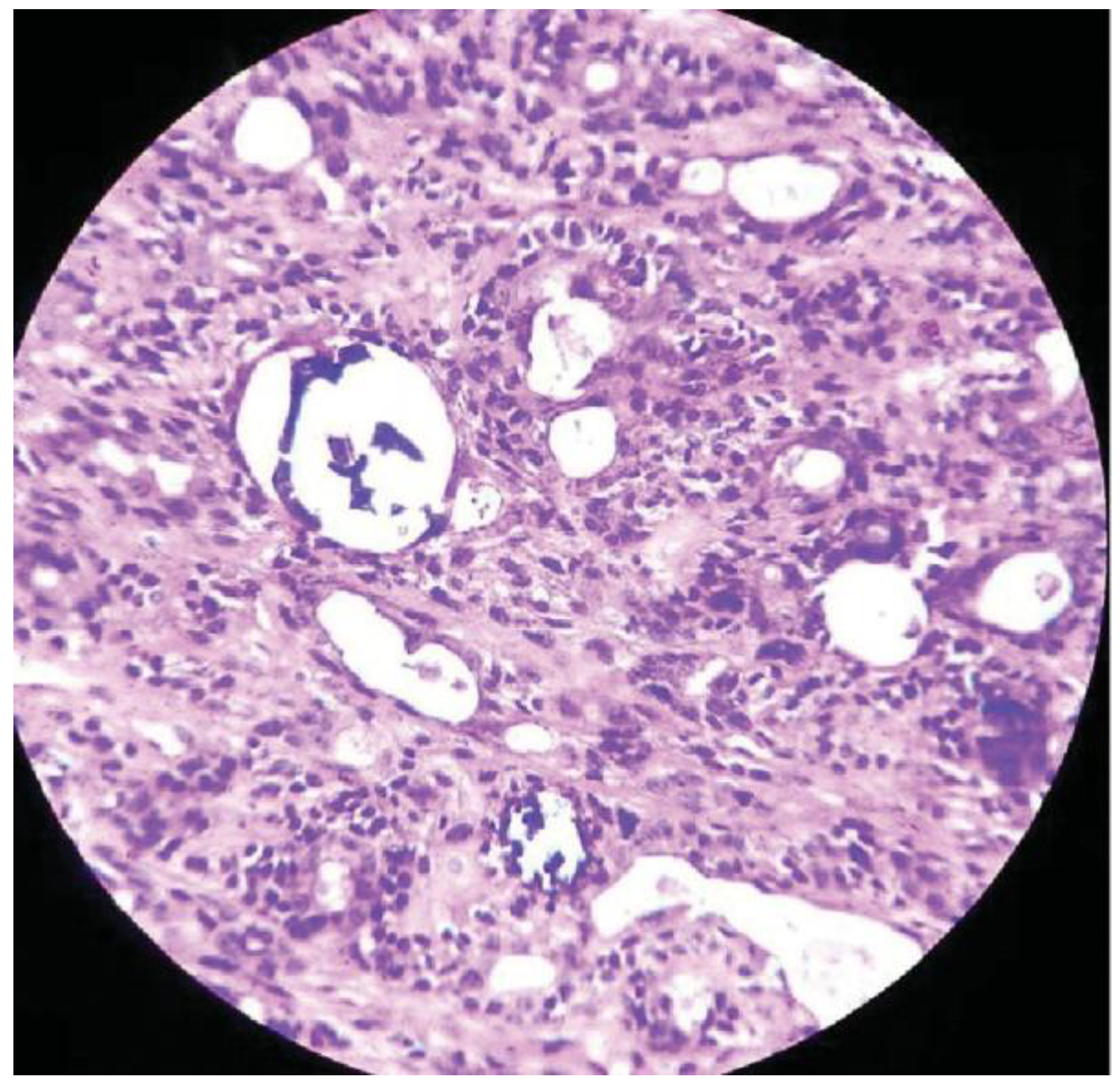
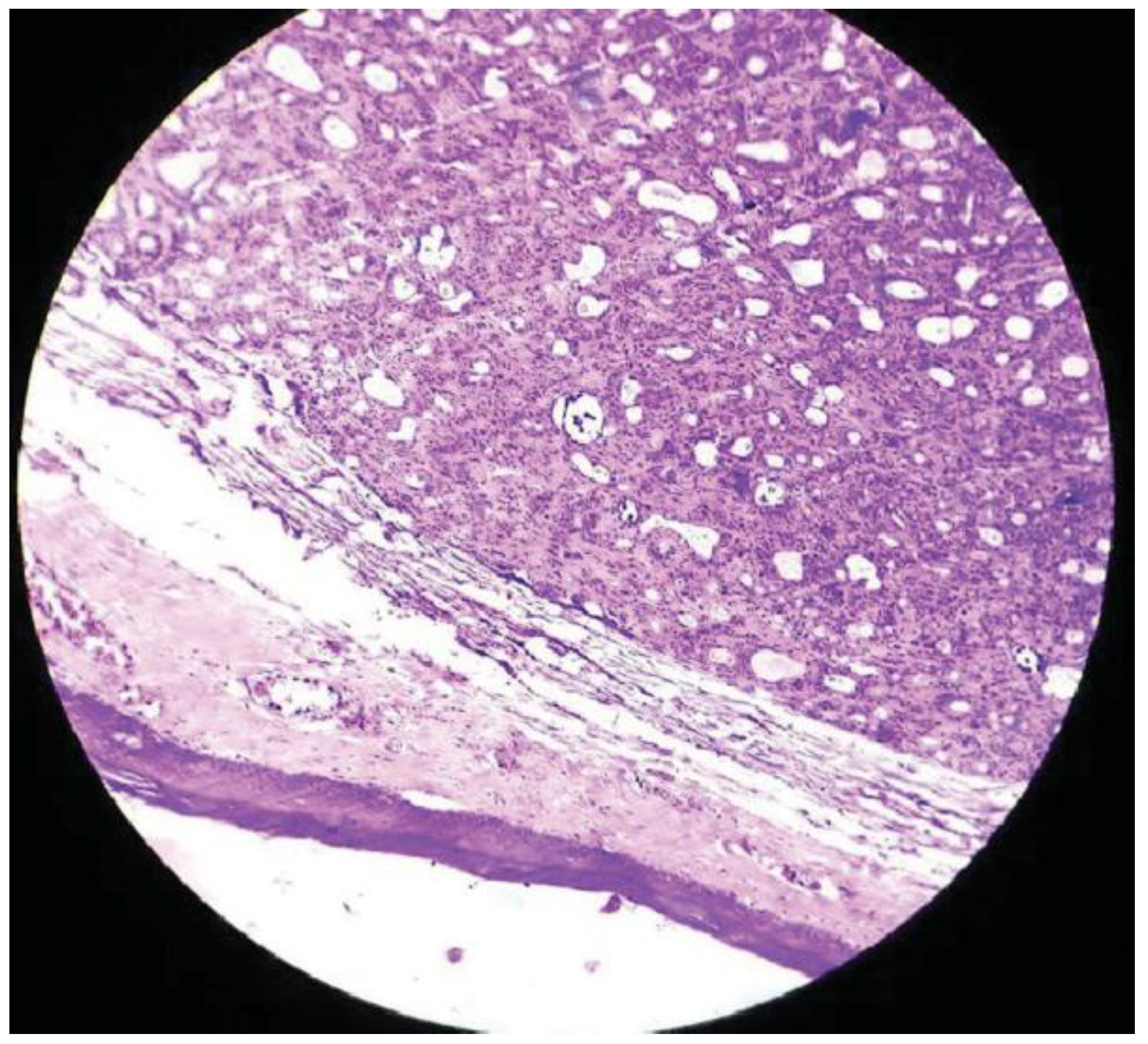
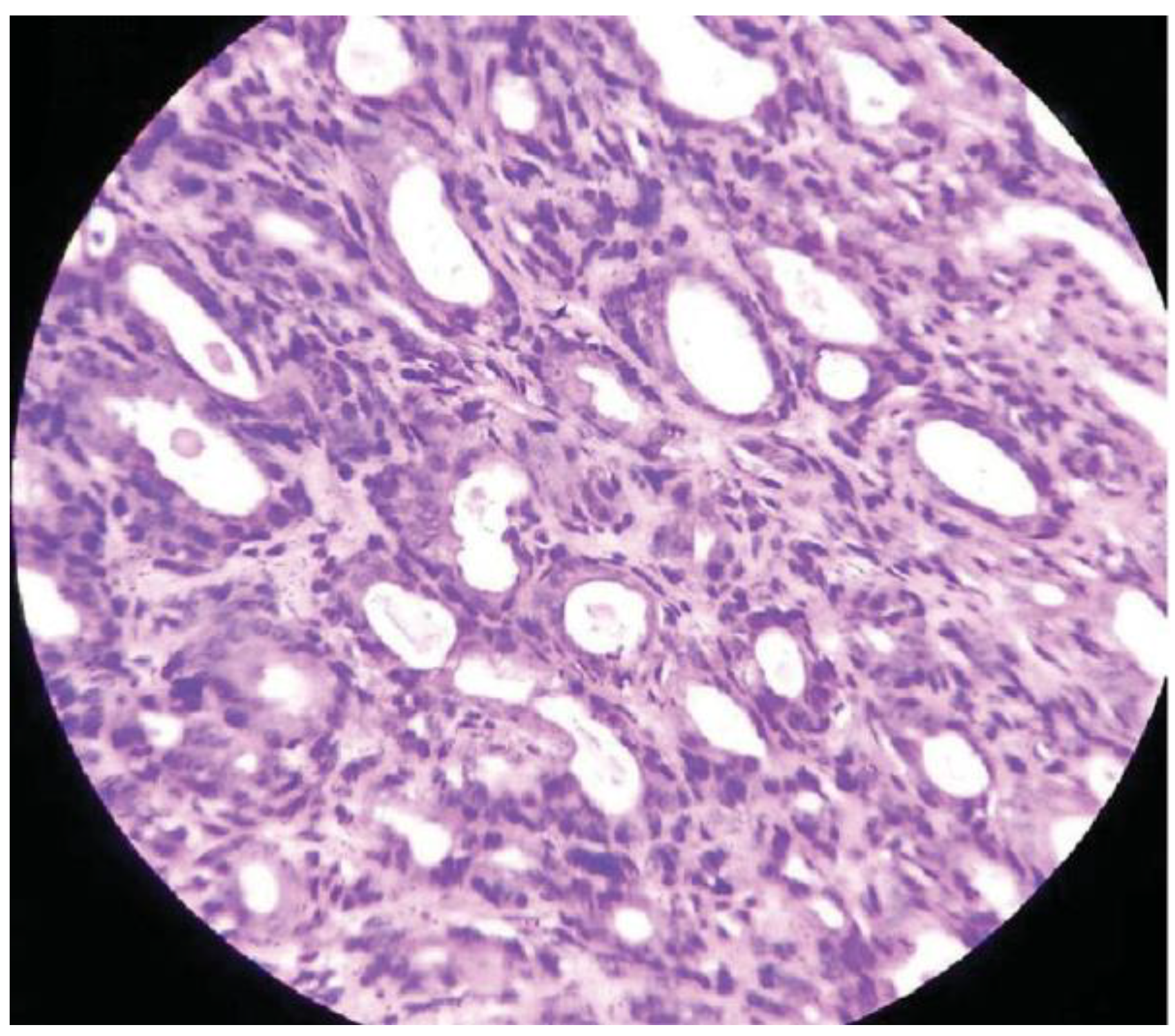
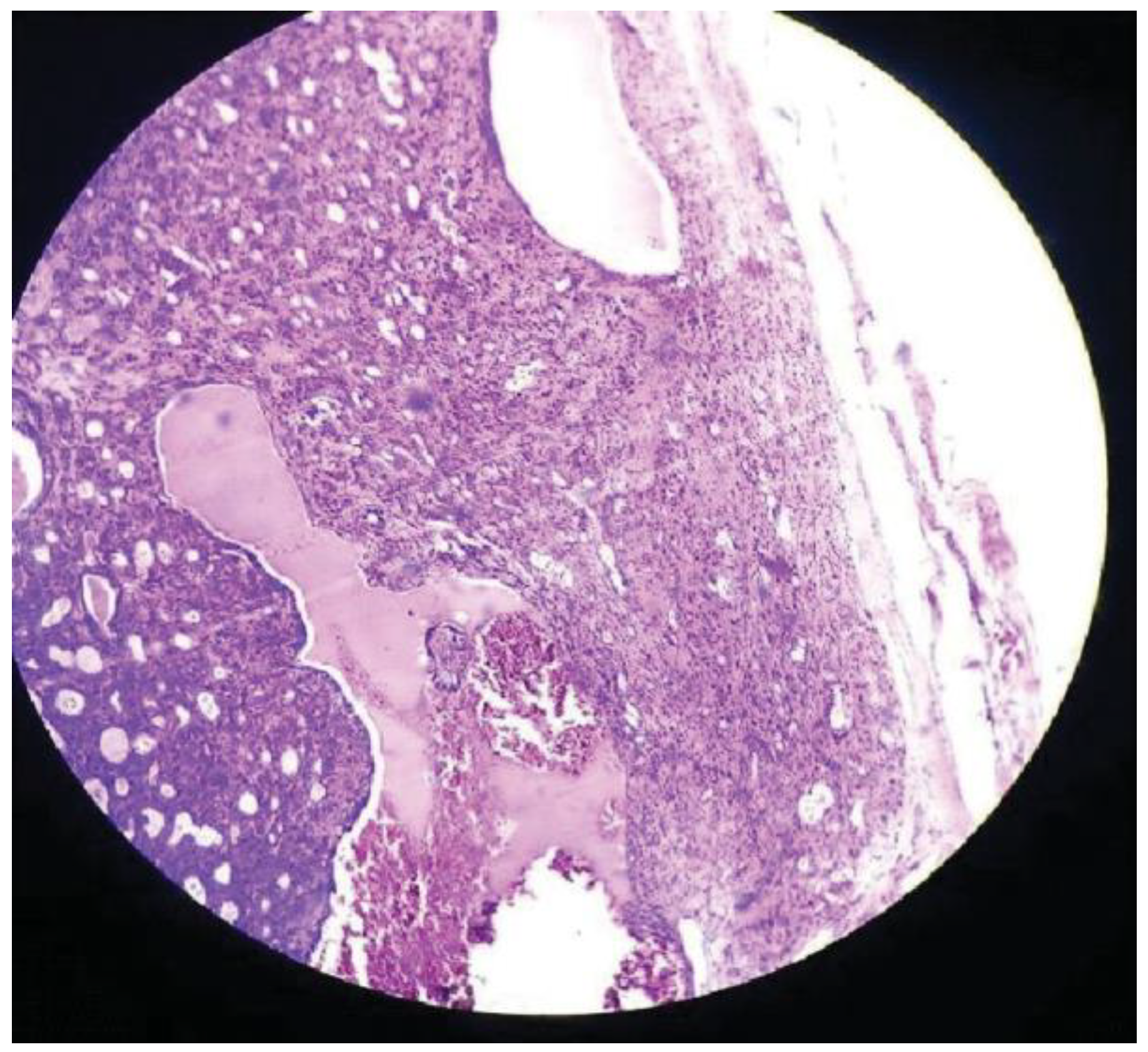
:Case Presentation
Discussion
Conclusion
References
- Leegard, T.; Lindeman, H. Salivary gland tumours: Clinical picture and treatment. Acta Otolaryngol. Suppl. 1969, 263, 55–59. [Google Scholar] [CrossRef]
- Eveson, J.W.; Cawson, R.A. Tumours of the minor (oropharyngeal) salivary glands: A demographic study of 336 cases. J. Oral. Pathol. 1985, 14, 500–509. [Google Scholar] [CrossRef]
- Minicucci, E.M.; de Campos, E.B.; Weber, S.A.; Domingues, M.A.; Ribeiro, D.A. Basal cell adenoma of the upper lip from minor salivary gland origin. Eur. J. Dent. 2008, 2, 213–216. [Google Scholar] [CrossRef]
- Basal Cell Adenoma. Available online: http://medical-dictionary.the-freedictionary.com/basal+cell+adenoma.
- Takeshita, T.; Tanaka, H.; Harasawa, A.; Kaminaga, T.; Imamura, T.; Furui, S. CT and MR findings of basal cell adenoma of the parotid gland. Radiat. Med. 2004, 22, 260–264. [Google Scholar] [PubMed]
- González-García, R.; Nam-Cha, S.H.; Muñoz-Guerra, M.F.; GamalloAmat, C. Basal cell adenoma of the parotid gland. Case report and review of the literature. Med. Oral. Patol. Oral. Cir. Bucal 2006, 11, E206–E209. [Google Scholar]
- Basal Cell Adenoma. Available online: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675 (accessed on 13 June 2016).
- Machado de Sousa, S.O.; Soares de Araújo, N.; Corrêa, L.; Pires Soubhia, A.M.; Cavalcanti de Araújo, V. Immunohistochemical aspects of basal cell adenoma and canalicular adenoma of salivary glands. Oral. Oncol. 2001, 37, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Seifert, G.; Donath, K. Hybrid tumours of salivary glands. Definition and classification of five rare cases. Eur. J. Cancer B Oral. Oncol. 1996, 32B, 251–259. [Google Scholar] [CrossRef]
- Choi, H.R.; Batsakis, J.G.; Callender, D.L.; Prieto, V.G.; Luna, M.A.; El-Naggar, A.K. Molecular analysis of chromosome 16q regions in dermal analogue tumors of salivary glands: A genetic link to dermal cylindroma? Am. J. Surg. Pathol. 2002, 26, 778–783. [Google Scholar] [CrossRef]
- Ellis, G. Basal cell adenocarcinoma. In World Health Organization Classification of Tumours: Head and Neck Tumours; Barnes, L., Eveson, J.W., Reichart, P., Sidransky, D., Eds.; IARC Press: Lyon, 2005; pp. 229–230. [Google Scholar]
- Kawahara, A.; Harada, H.; Akiba, J.; Yokoyama, T.; Kage, M. Fine-needle aspiration cytology of basal cell adenoma of the parotid gland: Characteristic cytological features and diagnostic pitfalls. Diagn. Cytopathol. 2007, 35, 85–90. [Google Scholar] [CrossRef]
- Muller, S.; Barnes, L. Basal cell adenocarcinoma of the salivary glands. Report of seven cases and review of the literature. Cancer 1996, 78, 2471–2477. [Google Scholar] [CrossRef]
- Nagao, T.; Sugano, I.; Ishida, Y.; et al. Basal cell adenocarcinoma of the salivary glands: Comparison with basal cell adenoma through assessment of cell proliferation, apoptosis, and expression of p53 and bcl-2. Cancer 1998, 82, 439–447. [Google Scholar] [PubMed]
- Yerli, H.; Teksam, M.; Aydin, E.; Coskun, M.; Ozdemir, H.; Agildere, A.M. Basal cell adenoma of the parotid gland: Dynamic CT and MRI findings. Br. J. Radiol. 2005, 78, 642–645. [Google Scholar] [PubMed]
- Hemachandran, M.; Lal, A.; Vaiphei, K. Basal cell adenoma-an unusual presentation. Ann. Diagn. Pathol. 2003, 7, 292–295. [Google Scholar] [PubMed]
- Katsuno, S.; Ishii, K.; Otsuka, A.; Ezawa, S.; Usami, S. Bilateral basal-cell adenomas in the parotid glands. J. Laryngol. Otol. 2000, 114, 83–85. [Google Scholar]
- Hall-Craggs, M.; Toker, C. Basaloid tumor of the sigmoid colon. Hum. Pathol. 1982, 13, 497–500. [Google Scholar]
- Chow, L.T.; Chow, W.H. Co-existing pleomorphic and tubular basal cell adenomas of the parotid gland. J. Laryngol. Otol. 1997, 111, 182–185. [Google Scholar]
- Yadav, A.B.; Narwal, A.; Devi, A.; Kumar, S.; Yadav, S.K. Basal Cell Adenoma of Palate, a Rare Occurrence with Review of Literature. J. Dent. 2015, 16 (Suppl. S3), 291–295. [Google Scholar]
- Chow, L.T.; Chow, W.H. Co-existing pleomorphic and tubular basal cell adenomas of the parotid gland. J. Laryngol. Otol. 1997, 111, 182–185. [Google Scholar]
- Chiu, N.C.; Wu, H.M.; Chou, Y.H.; et al. Basal cell adenoma versus pleomorphic adenoma of the parotid gland: CT findings. AJR Am. J. Roentgenol. 2007, 189, W254–W261. [Google Scholar]
- Luna, M.A.; Batsakis, J.G.; Ordóñez, N.G.; Mackay, B.; Tortoledo, M.E. Salivary gland adenocarcinomas: A clinicopathologic analysis of three distinctive types. Semin. Diagn. Pathol. 1987, 4, 117–135. [Google Scholar]
- Gupta, N.; Jadhav, K.; Ahmed, M.B.; Amberkar, V.S. Basal cell adenoma in a relatively rare site. J. Oral. Maxillofac. Pathol. 2009, 13, 101–104. [Google Scholar] [PubMed]

© 2016 by the author. The Author(s) 2016.
Share and Cite
Krishnan, V.; Shunmugavelu, K.; Rose, J.; Subramaniam, K. Basal Cell Adenoma of Retromolar Region from Minor Salivary Gland Origin in a 45-Year-Old Female: A Case Report. Craniomaxillofac. Trauma Reconstr. 2017, 10, 162-165. https://doi.org/10.1055/s-0036-1584394
Krishnan V, Shunmugavelu K, Rose J, Subramaniam K. Basal Cell Adenoma of Retromolar Region from Minor Salivary Gland Origin in a 45-Year-Old Female: A Case Report. Craniomaxillofacial Trauma & Reconstruction. 2017; 10(2):162-165. https://doi.org/10.1055/s-0036-1584394
Chicago/Turabian StyleKrishnan, Velavan, Karthik Shunmugavelu, Jamila Rose, and Kumaravel Subramaniam. 2017. "Basal Cell Adenoma of Retromolar Region from Minor Salivary Gland Origin in a 45-Year-Old Female: A Case Report" Craniomaxillofacial Trauma & Reconstruction 10, no. 2: 162-165. https://doi.org/10.1055/s-0036-1584394
APA StyleKrishnan, V., Shunmugavelu, K., Rose, J., & Subramaniam, K. (2017). Basal Cell Adenoma of Retromolar Region from Minor Salivary Gland Origin in a 45-Year-Old Female: A Case Report. Craniomaxillofacial Trauma & Reconstruction, 10(2), 162-165. https://doi.org/10.1055/s-0036-1584394


