Midfacial fractures, often caused by traffic accidents, sports, and interpersonal violence, damaging the integrity of the orbital skeleton, are frequently complicated by ophthalmic injury. The severity of the fractures is heterogeneous, so are the complications. Correct assessment of the injury and possible complications is important in the decision-making process of the treatment. Initial diagnosis and management is standardized. History taking and clinical and radiological examination include assessment of soft and bone tissue of orbit, globe, and adjacent structures.
Ophthalmic complications range from minor injuries, such as hematomas and subconjunctival bleeds, to major injuries, such as nerve injury or blow out of the globe. This article is a retrospective study, describing the spectrum and incidence of ophthalmic injury in 106 patients presenting with midfacial fractures at the Department of Oral and Maxillofacial surgery of the University Hospitals Leuven over a period of 16 months (January 2013 to April 2014). The aim of this study is to evaluate the incidence of ophthalmic complications following midfacial fractures and investigate its relation to surgical or nonsurgical treatment.
Patients and Methods
This is a retrospective study of 106 patients presenting with a midfacial fracture at the Department of Oral and Maxillofacial Surgery of the University Hospitals Leuven, Belgium, between January 2013 and April 2014. All patients with ophthalmic trauma without fracture of midfacial bone were excluded.
Population
Patients presenting at the department mainly came from Leuven and its surroundings. Because the University Hospitals Leuven is a tertiary trauma center, patients from other parts of the country were also transferred to the department for treatment.
Definitions
Midfacial trauma: All fractures of the maxilla, orbitae, and zygomatic complex occurred between January 2013 and April 2014 were included in the study. Some patients presented with fractures of limbs as well. Those fractures were not included in the study.
Ophthalmic injury: Not only visual impairment but also nerve and muscle injuries were included in the study. Injuries to eyelids and lacrimal ducts were evaluated as well.
Analysis
The following parameters were recorded: age, sex, number and extension of fractures, cause of trauma, ophthalmic injuries, treatment, and evolution. The results are presented separately. Recommendations for the clinical setting are made.
Results
Age
The mean age of the patients was 45.6 years. The youngest patient was 4 years old, and the oldest 90 years. The histogram of the data (
Figure 1), grouped per decade, shows that the group of patients between the age of 41 and 50 years was the biggest, with 20 cases or 18.9% of the population.
Gender
The patients showed a gender distribution of 68 men (64.2%) and 38 women (35.8%).
Causes of Trauma
The five main causes of midfacial trauma were road traffic accidents (43.3%), sports accidents (6.6%), violence (11.4%), accidents at work (6.6%), and other falls (32%; due to intoxication, syncope, epilepsy, etc.). Patients presenting with fracture after a road traffic accident were cyclists in 74% of the cases, car passengers in 15.2%, bikers in 8.6%, and pedestrians in 4.3% of the cases.
Fractures and Treatment
Fractures were classified as single fracture in 41.5% of the cases (
n = 44) or multiple fractures in 58.5% of the cases (
n = 62). All fractures were then divided into 12 categories, depending on which bone structure was affected. Orbital floor fractures and maxillary sinus fractures were the most frequent (
Table 1 and
Table 2).
Fifty patients (47.2%) were treated surgically: 42 of them underwent an open reduction and the other 8 patients underwent intermaxillary fixation or closed reduction. The remaining 52.8% (n = 56) of the patients were treated conservatively.
Ophthalmic Injury
Ophthalmic injury was recorded in 41 patients or 38.7% of the population. Injuries to the globe, enophthalmos, exophthalmos, traumatic neuropathy, restriction of eye movements, eyelid injuries, lacrimal duct injuries, and nerve or muscle injuries were noted (
Table 3). Of those 41 patients, 11 had a single midfacial fracture, and the remaining 30 patients with ophthalmic injury had multiple fractures.
Two patients or 1.9% of the population lost their vision in one eye. Both were caused by perforation of the globe. Two patients had a permanent decreased visual acuity due to traumatic optic neuropathy. In this retrospective study, three patients presented with decreased visual acuity in one eye due to compression of the optic nerve. One patient’s vision restored completely after surgical intervention (lateral canthotomy), and the two other patients maintained a decreased visual acuity in one eye after a conservative treatment.
Sixteen of the 20 patients presenting with reduced motility of the eye or diplopia had a fracture of the orbital floor.
Four patients presented with exophthalmos, and three with enophthalmos. Lacrimal duct injury was reported in 3 patients and eyelid injury in 13 patients. Sixteen patients presented with lesions to the eye. Minor injuries, such as conjunctival lesions, were the most common.
In this study, all five children younger than 16 years have a persistent ophthalmic problem.
Treatment of Ophthalmic Injury
There is no standardized treatment for ophthalmic injury following trauma because of the large number of different injuries. An ophthalmologist was always consulted following midfacial trauma for diagnostic evaluation and treatment advice when ophthalmic injuries were suspected. In one case, a lateral canthotomy was performed due to acute decreased visual acuity and suspected retrobulbar hematoma (RBH). The intervention was successful. Other treatments installed by the maxillofacial surgeon included surgical repair of the fractures or a conservative treatment (observation, antibiotics, painkillers, and corticosteroids if necessary).
Of the 41 patients, 21 (51.2%) patients with ophthalmic injury following trauma underwent a surgical repair of the fractures. Three of the 11 (27.3%) patients with only a single fracture were treated surgically. Eighteen of the 30 (60%) patients with multiple fractures were treated surgically.
All zygoma fractures were surgically repaired, as were the frontal bone fractures, temporal bone fractures, mandibular fractures, and Le Fort I and II fractures. Of the 31 patients with orbital floor fractures and ophthalmic injury, 16 patients (51.6%) were surgically repaired and/or reconstructed. Nasal bone fractures were repositioned in four cases and surgically repaired in three cases. One case was treated conservatively. Forty percent of orbital roof fractures in patients with ophthalmic injury were treated surgically. Lateral and medial orbital wall fractures were treated in 62.5 and 57.1% of cases, respectively. Only 16.7% of maxillary sinus fractures were treated. This fracture is sometimes small or minimally displaced, but can also be extensive with a lot of loose bone fragments. Surgical fixation is not needed in the first case or not possible in the latter.
Another analysis regarding treatment of ophthalmic injury was made. The kind of treatment each patient received was compared with the ophthalmic injury they had (
Table 3). Fractures of the patients with lacrimal duct injury were treated conservatively. Soft-tissue injury and lacerations were sutured and lacrimal duct function was restored. An ophthalmic surgeon performed this procedure. Eyelid injuries were also sutured. Of the 13 patients with eyelid injuries, only 3 needed a surgical fixation of the fracture. Of the 20 patients presenting with diplopia, 12 were treated surgically. Globe injuries were usually caused by direct trauma to the globe (
Table 4). Type of fracture was of no importance. Seven patients presenting with trauma to the globe were treated surgically. Damage to the conjunctiva, retina, etc., was attended by the ophthalmologist.
One of the three patients with traumatic optic neuropathy was treated surgically (lateral canthotomy). All of the four patients with exophthalmos were treated surgically and all of the three patients with enophthalmos were treated surgically.
Follow-up Ophthalmologic Problems
Persisting ophthalmic problems following trauma were found in 12 patients (11.3%). Trauma caused blindness in one eye in two patients; two patients had persisting decreased visual acuity in one eye, five patients complained of diplopia and decreased motility of one eye, one patient had a persistent exophthalmos, and two patients presented with lower eyelid retraction postoperatively. Removing the osteosynthesis material after 3 to 6 months can solve postoperative lower eyelid retraction. This procedure was successful in both the cases.
All other persistent lesions were already present immediately following trauma.
Both patients with permanent complete loss of vision had a perforation of the globe and multiple fractures. Despite immediate ocular surgery, their vision did not recover. Reconstruction of the facial fractures was delayed. Vitrectomy was also performed on one patient with decreased visual acuity. The intervention did not change the visual loss. Three out of four patients presenting with exophthalmos were successfully treated surgically. One patient has persistent exophthalmos after primary surgical intervention due to the extent of the initial defect. Of the five patients with persistent diplopia, three were treated surgically, and two conservatively. No muscle surgery was performed.
Other ophthalmic problems resolved after treatment, sometimes immediately, sometimes over several weeks.
Number of Transferred Patients with Ophthalmic Injury
University Hospitals Leuven is a tertiary trauma center. Patients from other parts of the country were transferred to the department for treatment. The number of transferred patients with ophthalmic injury following a midfacial fracture was recorded. Fifteen (36.6%) of the 41 patients with ophthalmic injury due to midfacial fractures was transferred from another hospital to the University Hospitals Leuven for further treatment. Five patients (41.7%) of the 12 with persistent ophthalmic injury were transferred from another hospital to the University hospitals Leuven. We can conclude that ophthalmic injury, and the persistence of it, does not correlate with the fact that the patient was transferred to our hospital.
Discussion
This study is comparable to other studies regarding the recorded parameters, sex, age, fracture site, ophthalmic injury, and cause of trauma. A considerable number of road traffic–related injuries concerned cyclists. Leuven is mostly inhabited by students, which explains this high number.
The incidence of ophthalmic injuries reported in other articles varies between 29 and 90%. [
1] Blindness remains a rare complication of midfacial trauma and is generally associated with serious and complex trauma.
Epidemiology
A recent study from China [
2] in which 1,000 patients with midfacial trauma were registered over a period of 10 years revealed that 18.4% of the patient population presented with ophthalmic injuries following midfacial trauma. This is much higher than observed in our retrospective study. The cause of this significant difference is probably the inclusion criteria of minor ophthalmic injuries.
Other parameters such as age, sex, and cause of injury were also recorded. The mean age of the patients was between 30 and 39 years. Few children presented with ophthalmic injury. The main cause of midfacial trauma was road traffic accidents. The kinetic energy released during a collision is the biggest risk factor for trauma and thus for ophthalmic injuries as well.
A study from Teheran, Iran, shows a totally different distribution of causes of midfacial trauma, as the study indicates that firearms caused most injuries [
3] (Teheran was a war zone at the time).
Literature shows, like this study, that patients with multiple fractures are at greater risk for ophthalmic problems than patients with a single fracture. [
4] However, we see that in patients with mandibular fractures in association with midfacial fractures, the incidence of ophthalmic injuries is lower. The mandible often absorbs the impact.
Due to the small number of case reports presenting blindness following trauma, it is difficult to obtain a reliable incidence of its occurrence.
Blindness following trauma is generally caused by perforation of the globe or by traumatic optic neuropathy. [
5] Traumatic optic neuropathy is a rare but serious complication of midfacial trauma. Literature describes an incidence of 0.5 to 5% of optic neuropathy following midfacial trauma. [
6] A study from Canada reveals that 0.4% of patients with midfacial trauma present with traumatic optic neuropathy. [
7] Complex craniofacial trauma is the biggest risk factor.
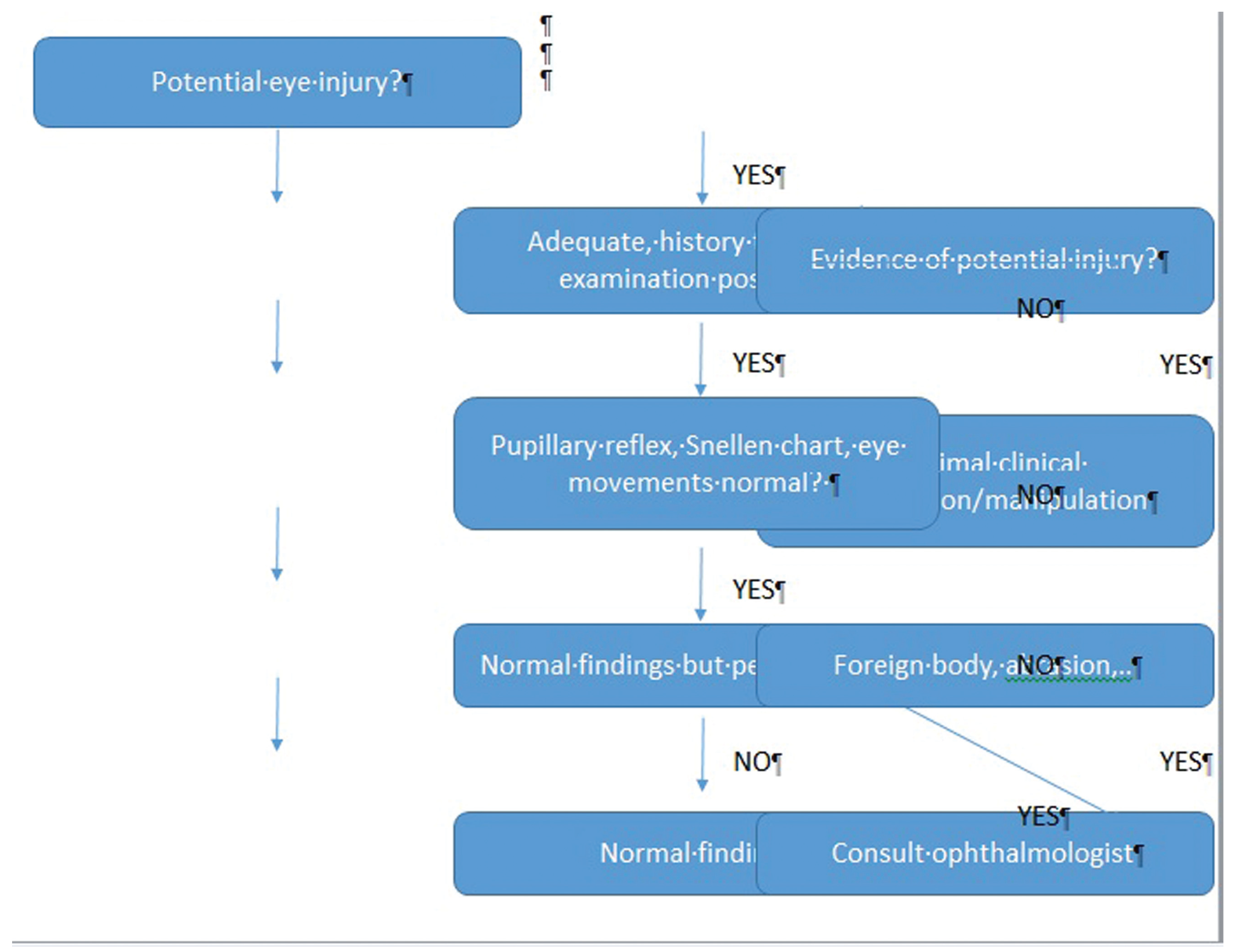
Loss of vision is a very serious complication following trauma. An ophthalmologic examination should be routinely performed after a midfacial trauma and should always take place prior to surgical intervention. Research on incidence, cause, and treatment regarding this subject should lead to standard decision of care and multidisciplinary treatment protocols (
Figure 2).
Pathogenesis of Ophthalmic Injury
Maxillary sinus and orbital floor fractures were associated the most frequent with ophthalmic injury. As these are in fact the most common midfacial fractures, we cannot say that they per se cause ophthalmic injury.
Trauma to the globe itself was caused by direct trauma to the eye; the nature of the fracture was of no importance.
A systematic review of the literature of 2011, including more than 14,500 patients, [
8] stated that “periorbital and orbital blowout fractures were more often complicated by ocular injuries compared with other facial fracture patterns. High-impact zygomatic fractures were most commonly associated with blindness.”
The first part of this statement was also observed in our study; 73% of patients with an orbital floor fracture presented with an ocular injury. The second part of this statement does not correlate with our study. In this study, two patients are now blind in one eye following maxillofacial trauma. In both cases, this was caused by perforation of the globe. Further conclusions regarding fracture pattern and ocular injurycould not be drawn from this study, as the population is too small.
Children
Children with midfacial trauma present with fewer fractures. They still have a flexible skeleton, pneumatization of the sinuses is incomplete, and there are many unerupted teeth in the maxillae (mostly between the age of 7 and 12 years). These elements explain why the incidence of fractures following midfacial trauma is low in children. If children do present with fractures, these generally are complex fractures and ophthalmic problems are present.
Blindness
The cause of posttraumatic blindness is not always found. This is generally a rupture of the globe or compression of the optic nerve by a hematoma or a bone fragment. Loss of vision due to traumatic optic neuropathy following trauma is multifactorial: decreased blood flow to the optic nerve leads to hypoperfusion and ischemia, edema, and hematoma lead to compression of the nerve and nerve bodies and axons lose their function due to acceleration–deceleration movement of the accident. The impact of the accident is absorbed by the eye and its surrounding structures. The impact causes vitroretinal damage as well. Retinal ischemia, retinal bleeds, and retinal detachments are other causes of blindness. [
9]
Lacrimal Duct
Nasolacrimal trauma can cause temporary or permanent dysfunction of the lacrimal duct. Temporary dysfunction is caused by hematoma or edema. Persistent dysfunction is caused by direct trauma to the canal, lacrimal sac, or by a fracture of the bone structure in which the canal passes. Patients with a Le Fort II fracture and naso-orbito-ethmoidal fractures are at risk. [
10] Occasionally, the lacrimal duct is damaged by osteosynthesis material.
Diagnosis
An ophthalmic examination is an indispensable part of clinical examination after maxillofacial trauma. Whenever communication is possible with the patient, a clinical evaluation is mandatory. In nonresponsive patients, it is very difficult to evaluate visual acuity. Pupillary reaction to light is often the only parameter. Edema and hematoma compromise correct evaluation of proptosis or enophthalmos. An ophthalmologic examination must always precede surgical repair in patients presenting with midfacial fractures. Pupillary reflex is tested, we use a Snellen chart to check visual acuity, and we evaluate eye movements and ask if there is diplopia. If any of these parameters is abnormal, an ophthalmologist is consulted.
Radiological examination includes computed tomography (CT) and/or magnetic resonance imaging (MRI). CT reveals the bone structures; MRI reveals more detailed information on the soft tissues and is more interesting from an ophthalmic or neurologic point of view. Globe deformations, without rupture or puncture, increase the intraocular pressure and cause traction on the retina and cornea. By draining RBH or surgically reducing the fracture, deformation of the globe can be undone and vision can be restored. However, reducing the fracture can also increase pressure by reducing the size of the orbit.
Papilledema caused by swelling of the optic nerve may predict the prognosis of visual impairment. Papilledema is seen on funduscopy and is impossible to visualize on radiological images.
Treatment
As stated earlier, all patients must undergo ophthalmic examination. Any ophthalmic intervention must precede operative repair of fractures. In case of minimal displacement of the fractured segments, we do not perform a surgical reduction if this could further exacerbate the ophthalmic symptoms.
There is no standard treatment for ophthalmic injuries following midfacial trauma. Decreased visual acuity after maxillofacial trauma can be caused by an expanding intraorbital lesion. This causes elevated intraorbital pressure and damages the eye and nerve tissue. Retrobulbar hemorrhage and edema are the most common causes of elevated intraorbital pressure.
Acute RBH can be classified into three categories according to Zimmer et al. [
12] RBH Class I is defined as a patient presenting with orbital injury without specific clinical or radiological signs, Class II is defined as a patient presenting with orbital injury with either clinical or radiological signs, and Class III is defined as a patient presenting with orbital injury and clear clinical and radiological signs. In our study, one patient presented with RBH Class III. A lateral canthotomy was successfully performed in that patient.
Surgical decompressionwith a lateral canthotomy is a simple procedure to preserve vision from sight-threatening retrobulbar hemorrhage. In this approach, the inferior and sometimes the superior lateral canthal tendon is cut. The most common method is canthotomy and cantholysis of the tendon securing the lateral part of the inferior eyelid. [
11] It is believed to be the safest surgical option for tension release in the orbit.
Another procedure used to decompress the orbit is called transcutaneous, transseptal orbital decompression. [
12] It decreases pressure in the orbit rapidly and with this procedure it is possible to evacuate blood that might otherwise stay trapped when performing a lateral canthotomy. It is a more extensive approach.
To reduce swelling, corticosteroids are often administered. Corticosteroids reduce swelling and have an antioxidant effect, but show objective improvement of vision only in 50% of cases. The pharmacological risks of steroids must be weighed against the gain of vision we could achieve by administering them.
Studies show that surgical decompression, corticosteroids, and placebo have the same result. [
13] According to Kloss et al., [
13] cortisol administration is no longer recommended.
Because the eye is a direct bulge of the brain and the central nervous system, 8 hours after trauma, the eye is irreversibly damaged if blood flow is not restored. Hyperventilation, anti-Trendelenburg, osmotic diuretics, and local hypothermia can stretch this period a little, but adequate and quick decision making is necessary.
Recent studies have shown that erythropoietin and progesterone are promising treatments for traumatic brain injury and thus probably for traumatic optic neuropathy as well. [
14,
15]
Surgical Repair of the Fracture
The decision to treat a patient surgically correlates with the extent of the injuries. Complex fractures or multiple fractures are more often treated than single fractures. The fracture site is also a crucial factor in the choice between a surgical and a conservative treatment. The degree of displacement of the bone fragments is very important in the decision making.
Analysis of results of nonsurgical versus surgical approaches of midfacial fractures is rare in the literature. It is difficult to compare both groups because many variables influence the decision making. Most studies compare only surgical techniques.
There are currently no standards available in oral and maxillofacial surgery to optimize patient care and reduce complications following midfacial trauma.
Conclusion
In our retrospective series, 106 trauma patients, who presented with midfacial fractures at the Department of Oral and Maxillofacial Surgery of the University Hospitals Leuven, Belgium, between January 2013 and April 2014, were analyzed. The mean age of the patients was 45.6 years with a gender distribution of 68 men (64.2%) and 38 women (35.8%). The main cause of trauma was road traffic accidents (43%). Fortyone (38.7%) patients suffered an ophthalmic injury. Twelve of them (11.3%) have a persistent ophthalmic problem.
Trauma caused blindness in one eye in two patients, two patients have persisting decreased visual acuity in one eye, five patients complain of diplopia and decreased motility of one eye, one patient has a persistent exophthalmos, and two patients presented with lower eyelid retraction postoperatively. Removing the osteosynthesis material after 3 to 6 months can solve postoperative lower eyelid retraction. This procedure was successful in both cases. All other persistent lesions were already present immediately following trauma.
Periorbital fractures were associated more with ocular injury than with other fractures. No other pattern between type of fracture and ocular injury could be found as the study consists of limited data.
We recently introduced an evaluation form for maxillofacial fractures in the emergency setting and hence forward patient information will be recorded in a more standardized manner.
Prompt ophthalmic examination in all midfacial fractures is necessary during the initial assessment. The time window for preservation of vision is very small and treatment should be started immediately when indicated. Development of an emergency trauma scale that includes facial fractures, symptoms of visual impairment, and patient history is recommended and might stimulate a multidisciplinary approach of complex cases. We made a suggestion for a protocol (protocol 1). In cases of visual impairment due to traumatic optic neuropathy where a RBH is suspected, lateral canthotomy and inferior cantholysis remains a straightforward and effective intervention.