Nigerian Muslim’s Perceptions of Changes in Diet, Weight, and Health Status during Ramadan: A Nationwide Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Design, Setting, and Participants
2.2. Ethics
2.3. Study Instrument and Data Collection
2.4. Sample Size
2.5. Description of Measures
2.6. Sociodemographics
2.7. Dietary Habits, Eating Behaviors, and Food Choices
3. Assessment of Weight, Height, Perceived Weight Changes, and Health Status
Data Analysis
4. Results
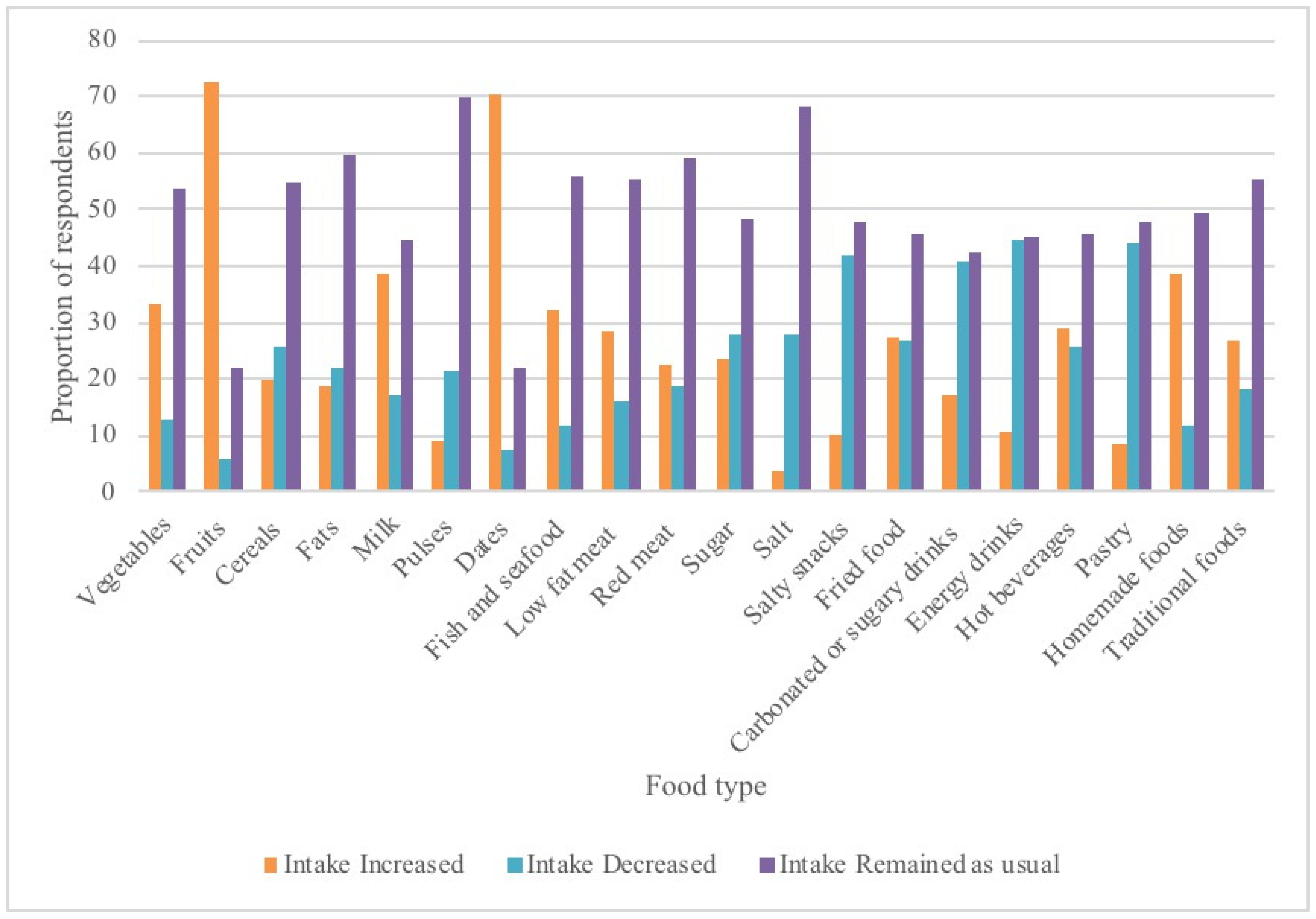
4.1. Diet Pattern and Diversity during Ramadan
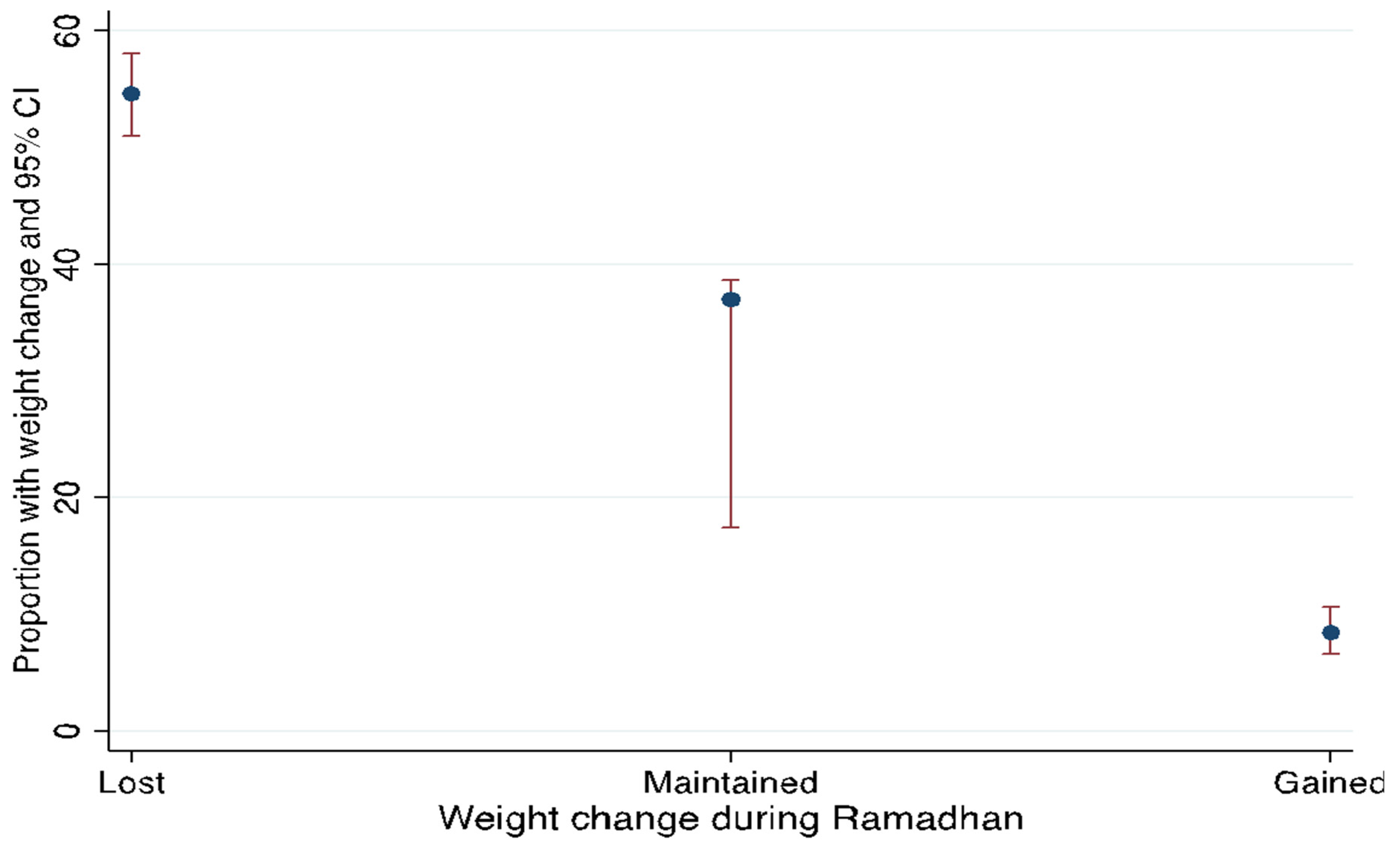
4.2. Weight Change and Health State during Ramadan
4.3. Predictors of Weight Change and Health State during Ramadan
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Jahrami, H.A.; Faris, M.E.; Janahi, A.I.; Janahi, M.I.; Abdelrahim, D.N.; Madkour, M.I.; Sater, M.S.; Hassan, A.B.; Bahammam, A.S. Does four-week consecutive, dawn-to-sunset intermittent fasting during Ramadan affect cardiometabolic risk factors in healthy adults? A systematic review, meta-analysis, and meta-regression. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 2273–2301. [Google Scholar] [CrossRef] [PubMed]
- Ali, Z.; Abizari, A.-R. Ramadan fasting alters food patterns, dietary diversity and body weight among Ghanaian adolescents. Nutr. J. 2018, 17, 75. [Google Scholar] [CrossRef] [PubMed]
- Fernando, H.A.; Zibellini, J.; Harris, R.A.; Seimon, R.V.; Sainsbury, A. Effect of Ramadan fasting on weight and body composition in healthy non-athlete adults: A systematic review and meta-analysis. Nutrients 2019, 11, 478. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Alsibai, J.; Clark, C.C.T.; Faris, M.A.-I.E. A systematic review, meta-analysis, and meta-regression of the impact of diurnal intermittent fasting during Ramadan on body weight in healthy subjects aged 16 years and above. Eur. J. Nutr. 2020, 59, 2291–2316. [Google Scholar] [CrossRef]
- Alkandari, J.R.; Maughan, R.J.; Roky, R.; Aziz, A.R.; Karli, U. The implications of Ramadan fasting for human health and well-being. J. Sport. Sci. 2012, 30, S9–S19. [Google Scholar] [CrossRef]
- Toda, M.; Morimoto, K. Ramadan Fasting—Effect On Healthy Muslims. Soc. Behav. Personal. Int. J. 2004, 32, 13–18. [Google Scholar] [CrossRef]
- Lee, J.H.; Verma, N.; Thakkar, N.; Yeung, C.; Sung, H.-K. Intermittent Fasting: Physiological Implications on Outcomes in Mice and Men. Physiology 2020, 35, 185–195. [Google Scholar] [CrossRef]
- De Cabo, R.; Mattson, M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N. Engl. J. Med. 2019, 381, 2541–2551. [Google Scholar] [CrossRef]
- Di Francesco, A.; Di Germanio, C.; Bernier, M.; de Cabo, R. A time to fast. Science 2018, 362, 770–775. [Google Scholar] [CrossRef]
- Idris, I.O.; Oguntade, A.S.; Mensah, E.A.; Kitamura, N. Prevalence of non-communicable diseases and its risk factors among Ijegun-Isheri Osun residents in Lagos State, Nigeria: A community based cross-sectional study. BMC Public Health 2020, 20, 1258. [Google Scholar] [CrossRef]
- Faris, M.A.-I.E.; Jahrami, H.A.; Alsibai, J.; Obaideen, A.A. Impact of Ramadan diurnal intermittent fasting on the metabolic syndrome components in healthy, non-athletic Muslim people aged over 15 years: A systematic review and meta-analysis. Br. J. Nutr. 2020, 123, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Adawi, M.; Watad, A.; Brown, S.; Aazza, K.; Aazza, H.; Zouhir, M.; Sharif, K.; Ghanayem, K.; Farah, R.; Mahagna, H.; et al. Ramadan Fasting Exerts Immunomodulatory Effects: Insights from a Systematic Review. Front. Immunol. 2017, 8, 1144. [Google Scholar] [CrossRef] [PubMed]
- Ebrahimi, S.; Gargari, B.P.; Aliasghari, F.; Asjodi, F.; Izadi, A. Ramadan fasting improves liver function and total cholesterol in patients with nonalcoholic fatty liver disease. Int. J. Vitam. Nutr. Res. 2020, 90, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Kiyani, M.M.; Memon, A.R.; Amjad, M.I.; Ameer, M.R.; Sadiq, M.; Mahmood, T. Study of Human Biochemical Parameters During and After Ramadan. J. Relig. Health 2017, 56, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Salim, I.; Suwaidi, J.A.; Ghadban, W.; Alkilani, H.; Salam, A.M. Impact of religious Ramadan fasting on cardiovascular disease: A systematic review of the literature. Curr. Med. Res. Opin. 2013, 29, 343–354. [Google Scholar] [CrossRef] [PubMed]
- Norouzy, A.; Salehi, M.; Philippou, E.; Arabi, H.; Shiva, F.; Mehrnoosh, S.; Mohajeri, S.M.R.; Mohajeri, S.A.R.; Larijani, A.M.; Nematy, M. Effect of fasting in Ramadan on body composition and nutritional intake: A prospective study. J. Hum. Nutr. Diet. 2013, 26, 97–104. [Google Scholar] [CrossRef]
- Faris, M.A.-I.E.; Salem, M.L.; Jahrami, H.A.; Madkour, M.I.; BaHammam, A.S. Ramadan intermittent fasting and immunity: An important topic in the era of COVID-19. Ann. Thorac. Med. 2020, 15, 125–133. [Google Scholar] [CrossRef]
- Abunada, T.; Abunada, H.; Zayed, H. Fasting Ramadan During COVID-19 Pandemic: Immunomodulatory Effect. Front. Nutr. 2020, 7, 557025. [Google Scholar] [CrossRef]
- Faris, M.A.-I.E.; Jahrami, H.A.; Obaideen, A.A.; Madkour, M.I. Impact of diurnal intermittent fasting during Ramadan on inflammatory and oxidative stress markers in healthy people: Systematic review and meta-analysis. J. Nutr. Intermed. Metab. 2019, 15, 18–26. [Google Scholar] [CrossRef]
- Bakhotmah, B.A. The puzzle of self-reported weight gain in a month of fasting (Ramadan) among a cohort of Saudi families in Jeddah, Western Saudi Arabia. Nutr. J. 2011, 10, 84. [Google Scholar] [CrossRef]
- Morgan, A.E.; Fanzo, J. Nutrition Transition and Climate Risks in Nigeria: Moving Towards Food Systems Policy Coherence. Curr. Environ. Health Rep. 2020, 7, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Awosan, K.J.; Ibrahim, M.T.O.; Essien, E.; Yusuf, A.A.; Okolo, A.C. Dietary pattern, lifestyle, nutrition status and prevalence of hypertension among traders in Sokoto Central market, Sokoto, Nigeria. IJNAM 2014, 6, 9–17. [Google Scholar] [CrossRef]
- Iheme, G.; Jagun, A.O.; Egechizuorom, I.M.; Ogbonna, O.C.; Edafioghor, L.O.; Adeleke, F.A.; Asouzu, N.C.; Mebude, A.S.; Enuka, H.C.; Kupoluyi, O.E.; et al. Food consumption and coping strategies of urban-households in Nigeria during the COVID-19 pandemic lockdown. World Nutr. 2020, 11, 35–50. [Google Scholar] [CrossRef]
- Bakki, B.; Talle, M.A.; Gezawa, I.D.; Ibrahim, H.; Baba, M.; Goni, B.W.; Yusuph, H.; Buba, F. Ramadan Fasting: Effect on the Metabolic Profile of Healthy Medical Students in north east, Nigeria. Saudi J. Med. 2017, 2, 5. [Google Scholar]
- Ajibola, A.A.; Azeez, A.O.; Ajibola, A. The Beneficial Effects of Ramadan Fasting from the Medical and Sociocultural Perspectives. J. Fasting Health 2021, 9, 1–13. [Google Scholar] [CrossRef]
- Fernandez, R.M. SDG3 Good Health and Well-Being: Integration and Connection with Other SDGs. In Good Health and Well-Being; Leal Filho, W., Wall, T., Azul, A.M., Brandli, L., Özuyar, P.G., Eds.; Cham: Springer International Publishing: New York, NY, USA, 2020; pp. 629–636. [Google Scholar] [CrossRef]
- Khan, M.A.; Menon, P.; Govender, R.; Samra, A.; Nauman, J.; Ostlundh, L.; Mustafa, H.; Smith, J.E.; Al Kaabi, J.M. Systematic review of the effects of pandemic confinements on body weight and their determinants. Br. J. Nutr. 2021, 127, 298–317. [Google Scholar] [CrossRef] [PubMed]
- Tsenoli, M.; Moverley Smith, J.E.; Khan, M. A community perspective of COVID-19 and obesity in children: Causes and consequences. Obes. Med. 2021, 1003, 27. [Google Scholar] [CrossRef]
- Khan, M.A.; Moverley Smith, J.E. “Covibesity”, a new pandemic. Obes. Med. 2020, 19, 100282. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; de Edelenyi, F.S.; Allès, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019, (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef]
- Athanasiadis, D.I.; Hernandez, E.; Hilgendorf, W.; Roper, A.; Embry, M.; Selzer, D.; Stefanidis, D. How are bariatric patients coping during the coronavirus disease 2019, (COVID-19) pandemic? Analysis of factors known to cause weight regain among postoperative bariatric patients. Surg. Obes. Relat. Dis. 2021, 17, 756–764. [Google Scholar] [CrossRef]
- Osler, M.; Heitmann, B.L. The validity of a short food frequency questionnaire and its ability to measure changes in food intake: A longitudinal study. Int. J. Epidemiol. 1996, 25, 1023–1029. [Google Scholar] [CrossRef] [PubMed]
- Blomquist, K.K.; Roberto, C.A.; Barnes, R.D.; White, M.A.; Masheb, R.M.; Grilo, C.M. Development and validation of the Eating Loss of Control Scale. Psychol. Assess. 2014, 26, 77. [Google Scholar] [CrossRef] [PubMed]
- Bolarinwa, O.A. Sample size estimation for health and social science researchers: The principles and considerations for different study designs. Niger. Postgrad. Med. J. 2020, 27, 67. [Google Scholar] [CrossRef]
- Hajek, P.; Myers, K.; Dhanji, A.-R.; West, O.; McRobbie, H. Weight change during and after Ramadan fasting. J. Public Health 2012, 34, 377–381. [Google Scholar] [CrossRef]
- Afolabi, B.M.; Ezedinachi, E.N.; Arikpo, I.; Okon, B.I.; Meremikwu, M.; Oparah, S.; Ganiyu, D.F. Self-reported Well-being and Perceived Health Status of Women in Child-Producing Age Living in Rural Communities on the Atlantic Ocean Coast in Southwest Nigeria. Divers. Equal. Health Care 2018, 15. [Google Scholar] [CrossRef]
- NWUDE EC. The Politics of Minimum Wage in Nigeria: The Unresolved Issues. Asian J. Empir. Res. 2013, 3, 477–492. [Google Scholar]
- Nigeria: Monthly Living Wage 2020|Statista 2021. Available online: https://www.statista.com/statistics/1119087/monthly-living-wage-in-nigeria/ (accessed on 15 December 2021).
- Yeoh, E.C.K.; Zainudin, S.B.; Loh, W.N.; Chua, C.L.; Fun, S.; Subramaniam, T.; Sum, C.F.; Lim, S.C. Fasting during Ramadan and Associated Changes in Glycaemia, Caloric Intake and Body Composition with Gender Differences in Singapore. Ann. Acad. Med. Singap. 2015, 44, 202–206. [Google Scholar] [CrossRef]
- Sajjadi, S.F.; Hassanpour, K.; Assadi, M.; Yousefi, F.; Ostovar, A.; Nabipour, I.; Rahbar, A. Effect of Ramadan fasting on Macronutrients & Micronutrients intake: An essential lesson for healthcare professionals. J. Nutr. Fasting Health 2018, 6, 205–212. [Google Scholar] [CrossRef]
- Osman, F.; Haldar, S.; Henry, C.J. Effects of Time-Restricted Feeding during Ramadan on Dietary Intake, Body Composition and Metabolic Outcomes. Nutrients 2020, 12, 2478. [Google Scholar] [CrossRef]
- Kohandani, A.; Hozoori, M.; Aasafari, M. Surveying the Dietary Diversity of Fasting Individuals in Qom in Ramadan. Health Spiritual. Med. Ethics 2015, 2, 6–10. [Google Scholar]
- Shatila, H.; Baroudi, M.; El Sayed Ahmad, R.; Chehab, R.; Forman, M.R.; Abbas, N.; Faris, M.; Naja, F. Impact of Ramadan Fasting on Dietary Intakes Among Healthy Adults: A Year-Round Comparative Study. Front. Nutr. 2021, 8, 689788. [Google Scholar] [CrossRef]
- Iddir, M.; Brito, A.; Dingeo, G.; Fernandez Del Campo, S.S.; Samouda, H.; La Frano, M.R.; Bohn, T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients 2020, 12, 1562. [Google Scholar] [CrossRef]
- Nutrition Advice for Adults during the COVID-19 Outbreak. World Health Organization—Regional Office for the Eastern Mediterranean n.d. Available online: http://www.emro.who.int/nutrition/news/nutrition-advice-for-adults-during-the-covid-19-outbreak.html (accessed on 10 March 2022).
- Sadiya, A.; Ahmed, S.; Siddieg, H.H.; Babas, I.J.; Carlsson, M. Effect of Ramadan fasting on metabolic markers, body composition, and dietary intake in Emiratis of Ajman (UAE) with metabolic syndrome. Diabetes. Metab. Syndr. Obes. 2011, 4, 409–416. [Google Scholar] [CrossRef]
- Nachvak, S.M.; Pasdar, Y.; Pirsaheb, S.; Darbandi, M.; Niazi, P.; Mostafai, R.; Speakman, J.R. Effects of Ramadan on food intake, glucose homeostasis, lipid profiles and body composition composition. Eur. J. Clin. Nutr. 2019, 73, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Daradkeh, G.; Abuzaid, H.; Al-Muhannadi, A.; Abuhmaira, M.; Calapano, M.; Khalili, A.; Acido, H.; Rustom, M.; Cajayon, C.; Hernando, A. Effect of Ramadan Fasting on Body Composition and Dietary Intake: A Prospective Study in the State of Qatar. J. Nutr. Food Sci. 2021, 11, 800. [Google Scholar] [CrossRef]
- Khaled, B.M.; Belbraouet, S. Effect of Ramadan fasting on anthropometric parameters and food consumption in 276 type 2 diabetic obese women. Int. J. Diabetes. Dev. Ctries. 2009, 29, 62–68. [Google Scholar] [CrossRef][Green Version]
- Hozoori, M.; Kohandani, A.; Mohammadi Veldani, A.; Mirizadeh, M. Nutrient Intake during Ramadan in Fasting People Referring to Health Centers in Qom, Iran. Health Spiritual. Med. Ethics 2017, 4, 9–11. [Google Scholar]
- Lamri-Senhadji, M.Y.; El Kebir, B.; Belleville, J.; Bouchenak, M. Assessment of dietary consumption and time-course of changes in serum lipids and lipoproteins before, during and after Ramadan in young Algerian adults. Singap. Med. J. 2009, 50, 288–294. [Google Scholar]
- Saibu, A. The role of Islamic social finance instruments in providing services in Nigeria. Ph.D. Thesis, Loughborough University, Loughborough, UK, 2020. [Google Scholar]
- Kocaaga, T.; Tamer, K.; Karli, U.; Yarar, H. Effects of Ramadan Fasting on Physical Activity Level and Body Composition in Young Males. Int. J. Appl. Exerc. Physiol. 2019, 8, 23–31. [Google Scholar]
- Bouhlel, E.; Denguezli, M.; Zaouali, M.; Tabka, Z.; Shephard, R.J. Ramadan fastings effect on plasma leptin, adiponectin concentrations, and body composition in trained young men. Int. J. Sport Nutr. Exerc. Metab. 2008, 18, 617–627. [Google Scholar] [CrossRef]
- Fahrial Syam, A.; Suryani Sobur, C.; Abdullah, M.; Makmun, D. Ramadan Fasting Decreases Body Fat but Not Protein Mass. Int. J. Endocrinol Metab. 2016, 14, e29687. [Google Scholar] [CrossRef] [PubMed]
- Faris, M.A.-I.E.; Madkour, M.I.; Obaideen, A.K.; Dalah, E.Z.; Hasan, H.A.; Radwan, H.; Jahrami, H.A.; Hamdy, O.; Mohammad, M.G. Effect of Ramadan diurnal fasting on visceral adiposity and serum adipokines in overweight and obese individuals. Diabetes Res. Clin. Pr. 2019, 153, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Al-Barha, N.S.; Aljaloud, K.S. The Effect of Ramadan Fasting on Body Composition and Metabolic Syndrome in Apparently Healthy Men. Am. J. Mens Health 2019, 13, 1557988318816925. [Google Scholar] [CrossRef] [PubMed]
- Khan Khattak, M.M.A.; Abu Bakar, I.; Yeim, L. Does religious fasting increase fat free mass (FFM) and reduce abdominal obesity? Nutr. Food Sci. 2012, 42, 87–96. [Google Scholar] [CrossRef]
- Radhakishun, N.N.E. Childhood Obesity: Medical, Cultural and Psychological Factors. Ph.D. Thesis, Philadelphia College of Osteopathic Medicine, Philadelphia, PA, USA, 2014. Research and Graduation External. [Google Scholar]
- Dahiru, T.; Aliyu, A.; Shehu, A. A review of population-based studies on diabetes mellitus in Nigeria. Sub-Sahar. Afr. J. Med. 2016, 3, 59. [Google Scholar] [CrossRef]
- Adeloye, D.; Ige-Elegbede, J.O.; Ezejimofor, M.; Owolabi, E.O.; Ezeigwe, N.; Omoyele, C.; Mpazanje, R.G.; Dewan, M.T.; Agogo, E.; Gadanya, M.A.; et al. Estimating the prevalence of overweight and obesity in Nigeria in 2020: A systematic review and meta-analysis. Ann. Med. 2021, 53, 495–507. [Google Scholar] [CrossRef]
- Troesch, B.; Biesalski, H.K.; Bos, R.; Buskens, E.; Calder, P.C.; Saris, W.H.M.; Spieldenner, J.; Verkade, H.J.; Weber, P.; Eggersdorfer, M. Increased Intake of Foods with High Nutrient Density Can Help to Break the Intergenerational Cycle of Malnutrition and Obesity. Nutrients 2015, 7, 6016–6037. [Google Scholar] [CrossRef]
| Variable | Frequency (%), N = 770 |
|---|---|
| Place of permanent domicile | |
| Urban | 562 (73.0) |
| Rural | 208 (27.0) |
| Sex | |
| Men | 86 (37.1) |
| Women | 484 (62.9) |
| Age group (Years) | |
| Less than or equal to 20 | 76 (9.9) |
| 21–30 | 476 (61.8) |
| 31–40 | 191 (24.8) |
| 41–50 | 24 (3.1) |
| 51–60 | 3 (0.4) |
| Marital status | |
| Single | 510 (66.2) |
| Married | 249 (32.3) |
| Divorced | 8 (1.0) |
| Widowed | 3 (0.4) |
| Highest educational level | |
| Tertiary or higher | 164 (21.3) |
| Undergraduate | 508 (66.0) |
| Secondary | 95 (12.3) |
| Primary | 3 (0.4) |
| Occupation | |
| Employed | 371 (48.2) |
| Unemployed | 399 (51.8) |
| * Monthly family income | |
| Less than NGN 137,600 | 250 (32.4) |
| NGN 137,600 or more | 231 (30.0) |
| Do not know | 289 (37.5) |
| BMI (kg/m2) | |
| Normal (<18.5 kg/m2) | 271 (35.2) |
| Underweight (18.5–24.9 kg/m2) | 78 (10.1) |
| Overweight (25–30) kg/m2 | 113 (14.77) |
| Obese (>30 kg/m2) | 186 (24.2) |
| Do not know | 122 (15.8) |
| History of diabetes, hypertension, or heart disease | |
| Yes | 98 (12.7) |
| No | 672 (87.3) |
| Family history of diabetes, hypertension, or heart disease | |
| Yes | 467 (60.7)) |
| No | 303 (39.3) |
| Days fasted | |
| None | 21 (2.7) |
| 1–10 | 5 (0.7) |
| 11–20 | 105 (13.6) |
| 21–30 | 639 (83.0) |
| Frequency of snacking from Iftar to Suhoor | |
| 1 to 2 times daily | 294 (38.2) |
| 3 or more times daily | 86 (11.2) |
| 1 to 6 times weekly | 218 (28.3) |
| Less than once weekly | 172 (22.3) |
| Modification of diet during Ramadan | |
| No | 123 (16.0) |
| Yes, a little | 245 (31.8) |
| Yes, moderately | 270 (35.1) |
| Yes, a lot | 132 (17.1) |
| Variable | Before Ramadan | During Ramadan | p-Value |
|---|---|---|---|
| Self-evaluated quality of diet | |||
| Good | 684 (88.8) | 716 (92.9) | 0.005 |
| Poor | 86 (11.2) | 54 (7.1) | |
| Cups of water drunk/day | |||
| 1–3 | 183 (23.8) | 223 (29.0) | 0.03 |
| 4–7 | 360 (46.8) | 314 (40.8) | |
| 8 or more | 227 (29.5) | 233 (30.3) | |
| Frequency of ordering takeaway food | |||
| Never or rarely | 378 (49.1) | 507 (65.8) | <0.001 |
| Daily | 24 (3.1) | 17 (2.2) | |
| 1–2 times weekly | 60 (7.8) | 55 (7.2) | |
| 3–6 times weekly | 67 (8.7) | 37 (4.8) | |
| 1 or more times monthly | 241 (31.3) | 154 (20.0) | |
| Frequency of eating out | |||
| Never or rarely | 354 (46.0) | 581 (75.5) | <0.001 |
| Daily | 33 (4.3) | 10 (1.3) | |
| 1–2 times weekly | 63 (8.2) | 24 (3.1) | |
| 3–6 times weekly | 73 (9.5) | 23 (3.0) | |
| 1 or more times monthly | 247 (32.1) | 132 (17.1) | |
| Snacking | |||
| Less often | 485 (63.0) | 540 (70.0) | <0.001 |
| More often | 173 (22.5) | 67 (8.7) | |
| No | 112 (14.6) | 163 (21.2) | |
| Consuming large quantities of food | |||
| Less often | 200 (26.0) | 198 (25.7) | 0.27 |
| More often | 437 (56.8) | 461 (59.9) | |
| No | 133 (17.3) | 111 (14.4) | |
| Eating despite not feeling hungry | |||
| Less often | 219 (28.4) | 238 (30.9) | 0.001 |
| More often | 414 (53.8) | 445 (57.8) | |
| No | 137 (17.8) | 87 (11.3) |
| Variable | Lost Weight | Gained Weight | p-Value | Lost Weight | Gained Weight | p-Value |
|---|---|---|---|---|---|---|
| Crude OR (95% CI) | Crude OR (95% CI) | * Adjusted OR (95% CI) | * Adjusted OR (95% CI) | |||
| Place of permanent domicile | ||||||
| Urban | Reference | 0.98 | ||||
| Rural | 1.1 (0.7–1.4) | 1.0 (0.5–1.8) | ||||
| Age (years) | ||||||
| 20 or less | Reference | 0.51 | Reference | Reference | ||
| 21–30 | 0.6 (0.4–1.1) | 0.7 (0.3–1.8) | 0.8 (0.4–1.4) | 0.8 (0.3–2.4) | ||
| 31–40 | 0.9 (0.5–1.5) | 0.7 (0.3–2.0) | 1.0 (0.5–2.1) | 0.9 (0.3–3.4) | 0.47 | |
| 41–50 | 1.3 (0.5–3.9) | 1.1 (1.8–6.7) | 1.6 (0.5–5.3) | 1.6 (0.2–12.1) | ||
| 51–60 | 1.0 9 (0.1–11.6) | -- | 1.4 (0.1–16.5) | --- | ||
| Sex | ||||||
| Men | Reference | 0.35 | Reference | Reference | ||
| Women | 0.9 (0.7–1.2) | 1.3 (0.8–2.3) | 0.9 (0.6–1.2) | 1.1 (0.5–2.1) | 0.43 | |
| Occupation | ||||||
| Employed | Reference | 0.67 | ||||
| Unemployed | 1.0 (0.7–1.3) | 1.2 (0.7–2.1) | ||||
| Pre-Ramadan BMI (kg/m2) | ||||||
| Normal | Reference | 0.33 | Reference | Reference | ||
| Underweight | 0.7 (0.4–1.2) | 0.3 (0.1–1.1) | 0.7 (0.4–1.2) | 0.3 (0.1–1.20 | 0.19 | |
| Overweight | 1.1 (0.7–1.8) | 1.4 (0.6–3.1) | 1.0 (0.6–1.7) | 1.3 (0.6–3.1) | ||
| Obese | 0.9 (0.6–1.3) | 1.0 (0.5–2.1) | 0.9 (0.6–1.3) | 1.0 (0.5–2.2) | ||
| Days fasted | ||||||
| None | Reference | 0.24 | ||||
| 1–10 | 0.3 (0.1–2.7) | -- | ||||
| 11–20 | 1.9 (0.7–5.) | 1.0 (0.3–4.5) | ||||
| 21–30 | 1.5 (0.6–3.7) | 0.6 (1.7–2.4) | ||||
| Improved self-evaluated diet quality during Ramadan | ||||||
| No | Reference | 0.97 | ||||
| Yes | 1.0 (0.6–1.8) | 0.9 (0.3–2.5) | ||||
| Cups of water drunk/day during Ramadan | ||||||
| 1–3 | Reference | 0.03 | 0.05 | |||
| 4–7 | 0.7 (0.3–1.0) | 0.5 (0.3–0.9) | 0.7 (0.5–1.0) | 0.6 (0.3–1.1) | ||
| 8 or more | 1.0 (0.7–1.5) | 0.5 (0.3–1.1) | 1.0 (0.7–1.7) | 0.5 (0.2–1.0) | ||
| Frequency of ordering food or takeaway during Ramadan | ||||||
| Never or rarely | Reference | 0.01 | 0.04 | |||
| Daily | 2.9 (0.8–10.2) | 1.8 (0.2–18.2) | 3.5 (0.8–14.9) | 3.0 (0.3–35.3) | ||
| 1–2 times weekly | 1.0 (0.5–1.8) | 3.4 (1.5–7.8) | 1.2 (0.6–2.4) | 3.7 (1.4–9.8) | ||
| 3–6 times weekly | 1.7 (0.8–3.7) | 3.1(1.0–9.7) | 1.7 (0.7–4.1) | 1.9 (0.5–7.5) | ||
| 1 or more times monthly | 0.7 (0.5–2.1) | 1.2 (0.6–2.3) | 0.7 (0.5–1.1) | 0.9 (0.4–2.0) | ||
| Frequency of eating out during Ramadan | ||||||
| Never or rarely | Reference | 0.08 | 0.34 | |||
| Daily | 1.6 (0.4–6.1) | - | 0.8 (0.2–4.1) | -- | ||
| 1–2 times weekly | 0.5 (0.2–1.2) | 1.3 (0.4–4.8) | 0.5 (0.2–1.4) | 0.7 (1.4–3.0) | ||
| 3–6 times weekly | 1.6 (0.6–4.7) | 6.2 (1.8–21.6) | 1.3 (0.4–4.3) | 4.8 (1.0–20.7) | ||
| 1 or more times monthly | 1.0 (0.7–1.5) | 1.5 (0.8–3.0) | 1.1 (0.7–1.7) | 1.3 (0.6–2.8) | ||
| Snacking during Ramadan | ||||||
| No | Reference | 0.02 | <0.001 | |||
| Less often | 1.3 (.0–1.8) | 2.5 (1.1–5.5) | ||||
| More often | 0.7 (0.4–1.2) | 1 (0.3–3.4) | ||||
| Consuming large quantities of food during Ramadan | ||||||
| No | Reference | 0.17 | Reference | 0.04 | ||
| Less often | 1.2 (0.9–1.7) | 1.8 (0.9–3.5) | 1.4 (0.9–2.0) | 2.6 (1.2–5.9) | ||
| More often | 0.9 (0.5–1.4) | 0.8 (0.3–2.1) | 0.7 (0.4–1.2) | 0.8 (0.2–3.1) | ||
| Eating despite not feeling hungry during Ramadan | ||||||
| No | Reference | 0.61 | ||||
| Less often | 1.1 (0.8–1.5) | 1.7 (0.9–3.2) | ||||
| More often | 1.0 (0.6–1.7) | 1.3 (0.5–3.5) | ||||
| Frequency of snacking from Iftar to Suhoor | ||||||
| Less than once weekly | Reference | 0.18 | ||||
| 1 to 2 times daily | 0.7 (0.5–1.1) | 1.2 (0.5–2.8) | ||||
| 3 or more times daily | 0.8 (0.4–1.3) | 2.5 (0.9–6.6) | ||||
| 1 to 6 times weekly | 0.8 (0.5–1.2) | 1.7 (0.8–4.1) |
| Variable | Crude OR (95% CI) | p-Value | Adjusted OR * (95% CI) | p-Value |
|---|---|---|---|---|
| Weight change during Ramadan | ||||
| Maintained | Reference | 0.42 | ||
| Lost | 0.5 (0.2–1.5) | |||
| Gained | 0.6 (0.1–3.0) | |||
| Sex | ||||
| Men | Reference | 0.15 | Reference | 0.81 |
| Women | 0.5 (0.2–1.3) | 0.9 (0.3–2.5) | ||
| Age (Years) | ||||
| 20 or less | Reference | 0.57 | Reference | 0.64 |
| 21–30 | 2.2 (0.7–6.8) | 2.7 (9.7–9.6) | ||
| 31–40 | 2.6 (0.6–10.7) | 1.6 (0.2–9.9) | ||
| 41–50 | 1.3 (0.1–12.0) | 0.9 (9.1–12.2) | ||
| 51–60 | -- | |||
| Place of permanent domicile | ||||
| Urban | Reference | 0.7 | ||
| Rural | 1.2 (0.4–3.3) | |||
| Occupation | ||||
| Employed | Reference | 0.06 | 0.09 | |
| Unemployed | 0.4 (0.2–1.1) | 0.5 (0.2–1.1) | ||
| BMI (kg/m2) | ||||
| Normal | Reference | 0.60 | Reference | 0.74 |
| Underweight | 0.7 (0.2–3.8) | 0.8 (0.2–4.5) | ||
| Overweight | 0.5 (0.2–1.9) | 0.5(0.2–2.0) | ||
| Obese | 0.5 (0.2–1.5) | 0.5 (0.1–1.6) | ||
| History of DM, hypertension, or heart disease | ||||
| No | Reference | 0.16 | ||
| Yes | 0.5 (0.2–1.3) | |||
| How many days fasted | ||||
| None | 0.31 | |||
| 1–10 | 0.1 (0–1.1) | |||
| 11–20 | 1 (0.1–9.0) | |||
| 21–30 | 2.4 (0.3–19.3) | |||
| Changed diet quality during Ramadan | ||||
| No | Reference | 0.05 | 0.08 | |
| Yes | 3.3 (1.1–10.1) | 2.9 (0.9–9.0) | ||
| Cups of water drunk/day during Ramadan | ||||
| 1–3 | Reference | 0.45 | ||
| 4–7 | 1.3 (0.5–3.3) | |||
| 8 or more | 2.1 (0.6–7.2) | |||
| Frequency of ordering food or takeaway during Ramadan | ||||
| Never or rarely | Reference | 0.81 | ||
| Daily | -- | |||
| 1–2 times weekly | 1.8 (0.2–13.5) | |||
| 3–6 times weekly | -- | |||
| 1 or more times monthly | 1.2 (0.4–3.7) | |||
| Frequency of eating out during Ramadan | ||||
| Never or rarely | Reference | 0.18 | ||
| Daily | 0.2 (0.1–1.5) | |||
| 1–2 times weekly | 0.2 (0.1–1.0) | |||
| 3–6 times weekly | 0.4 (0.1–3.4) | |||
| 1 or more times monthly | 0.4 (0.2–1.1) | |||
| Snacking during Ramadan | ||||
| No | Reference | 0.10 | Reference | 0.20 |
| Less often | 0.2 (0.1–1.4) | 0.2 (0.1–1.4) | ||
| More often | 0.2 (0.1–2.3) | 0.2 (0.1–2.3) | ||
| Consuming large quantities of food during Ramadan | ||||
| No | Reference | 0.16 | ||
| Less often | 0.3 (0.1–1.3) | |||
| More often | 0.4 (0.1–2.2) | |||
| Eating despite not feeling hungry during Ramadan | ||||
| No | Reference | 0.20 | ||
| Less often | 0.4 (0.1–1.3) | |||
| More often | 0.4 (0.1–1.8) | |||
| Frequency of snacking from Iftar to Suhoor | ||||
| 1 to 2 times daily | Reference | 0.23 | ||
| 3 or more times daily | 0.6 (01–3.2) | |||
| 1 to 6 times weekly | 0.3 (0.1–1.1) | |||
| Less than once weekly | 0.4 (0.1–1.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sulaiman, S.K.; Tsiga-Ahmed, F.I.; Faris, M.E.; Musa, M.S.; Akpan, U.A.-o.; Umar, A.M.; Abubakar, S.M.; Allaham, K.K.; Alyammahi, T.; Abdbuljalil, M.A.; et al. Nigerian Muslim’s Perceptions of Changes in Diet, Weight, and Health Status during Ramadan: A Nationwide Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 14340. https://doi.org/10.3390/ijerph192114340
Sulaiman SK, Tsiga-Ahmed FI, Faris ME, Musa MS, Akpan UA-o, Umar AM, Abubakar SM, Allaham KK, Alyammahi T, Abdbuljalil MA, et al. Nigerian Muslim’s Perceptions of Changes in Diet, Weight, and Health Status during Ramadan: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(21):14340. https://doi.org/10.3390/ijerph192114340
Chicago/Turabian StyleSulaiman, Sahabi Kabir, Fatimah Isma’il Tsiga-Ahmed, MoezAlIslam E. Faris, Muhammad Sale Musa, Udoyen Abasi-okot Akpan, Abdullahi Muhammad Umar, Salisu Maiwada Abubakar, Kholoud K. Allaham, Taif Alyammahi, Munther A. Abdbuljalil, and et al. 2022. "Nigerian Muslim’s Perceptions of Changes in Diet, Weight, and Health Status during Ramadan: A Nationwide Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 21: 14340. https://doi.org/10.3390/ijerph192114340
APA StyleSulaiman, S. K., Tsiga-Ahmed, F. I., Faris, M. E., Musa, M. S., Akpan, U. A.-o., Umar, A. M., Abubakar, S. M., Allaham, K. K., Alyammahi, T., Abdbuljalil, M. A., Javaid, S. F., & Khan, M. A. (2022). Nigerian Muslim’s Perceptions of Changes in Diet, Weight, and Health Status during Ramadan: A Nationwide Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(21), 14340. https://doi.org/10.3390/ijerph192114340








