Health Services and Patient Satisfaction in IRAN during the COVID-19 Pandemic: A Methodology Based on Analytic Hierarchy Process and Artificial Neural Network
Abstract
:1. Introduction
2. Literature Review
3. Methodology
3.1. Analytic Hierarchy Process (AHP)
3.2. Development of the Hierarchy Model
3.3. Pairwise Comparison Matrix and the Priority Weights within the Hierarchy
3.4. Consistency Index and Consistency Ratio
3.5. Artificial Neural Network (Multi-Layer Perceptron Model)
3.6. Data Collection
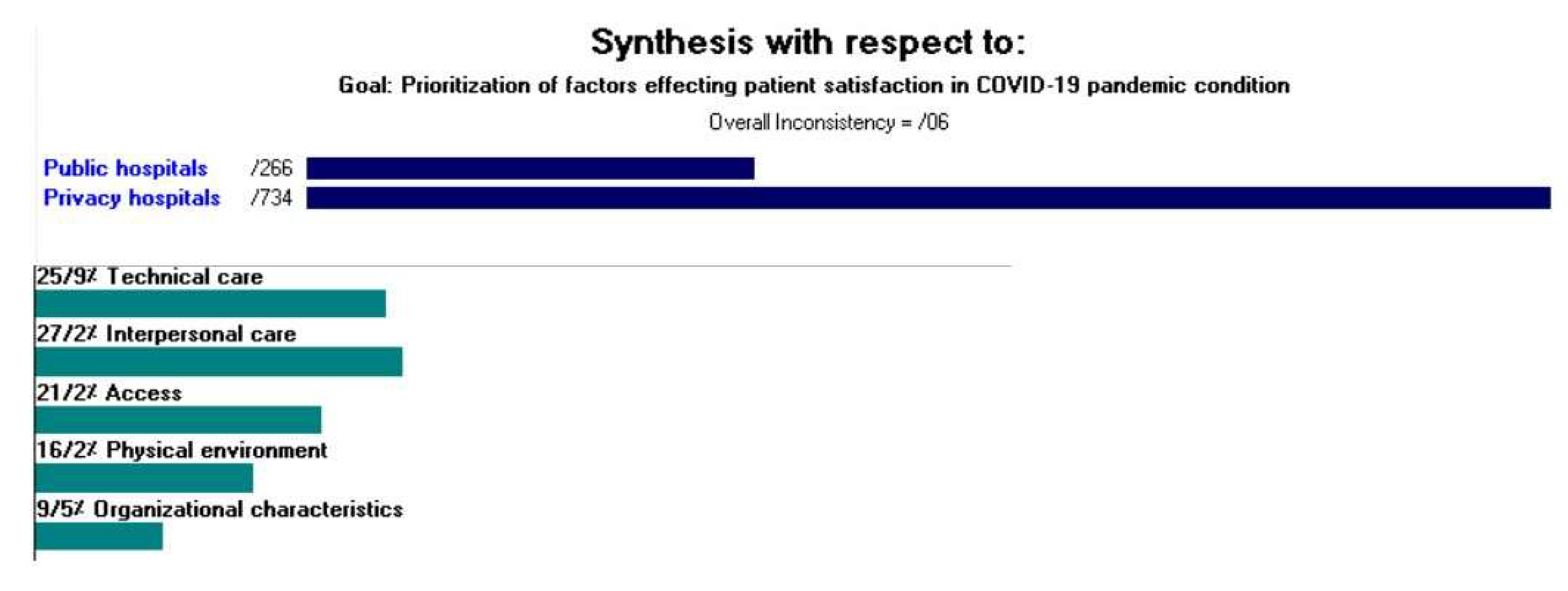
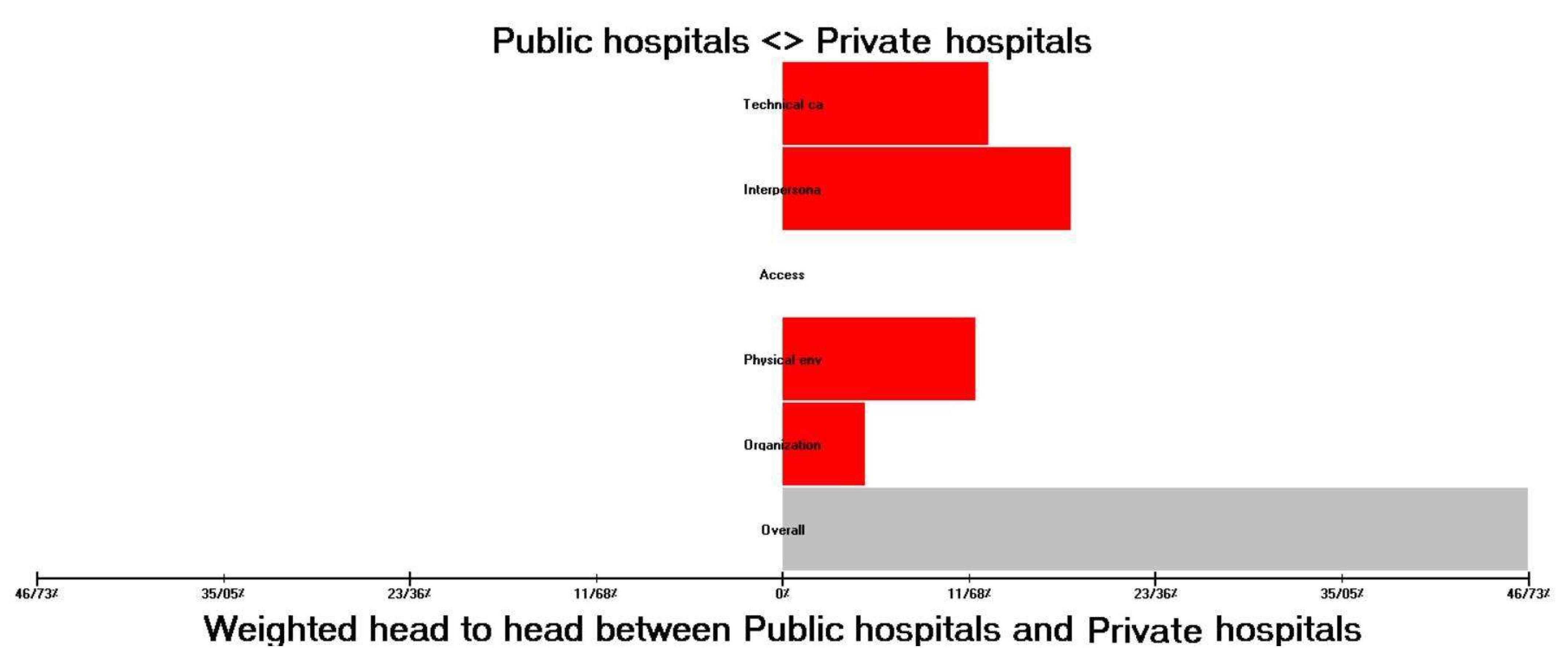
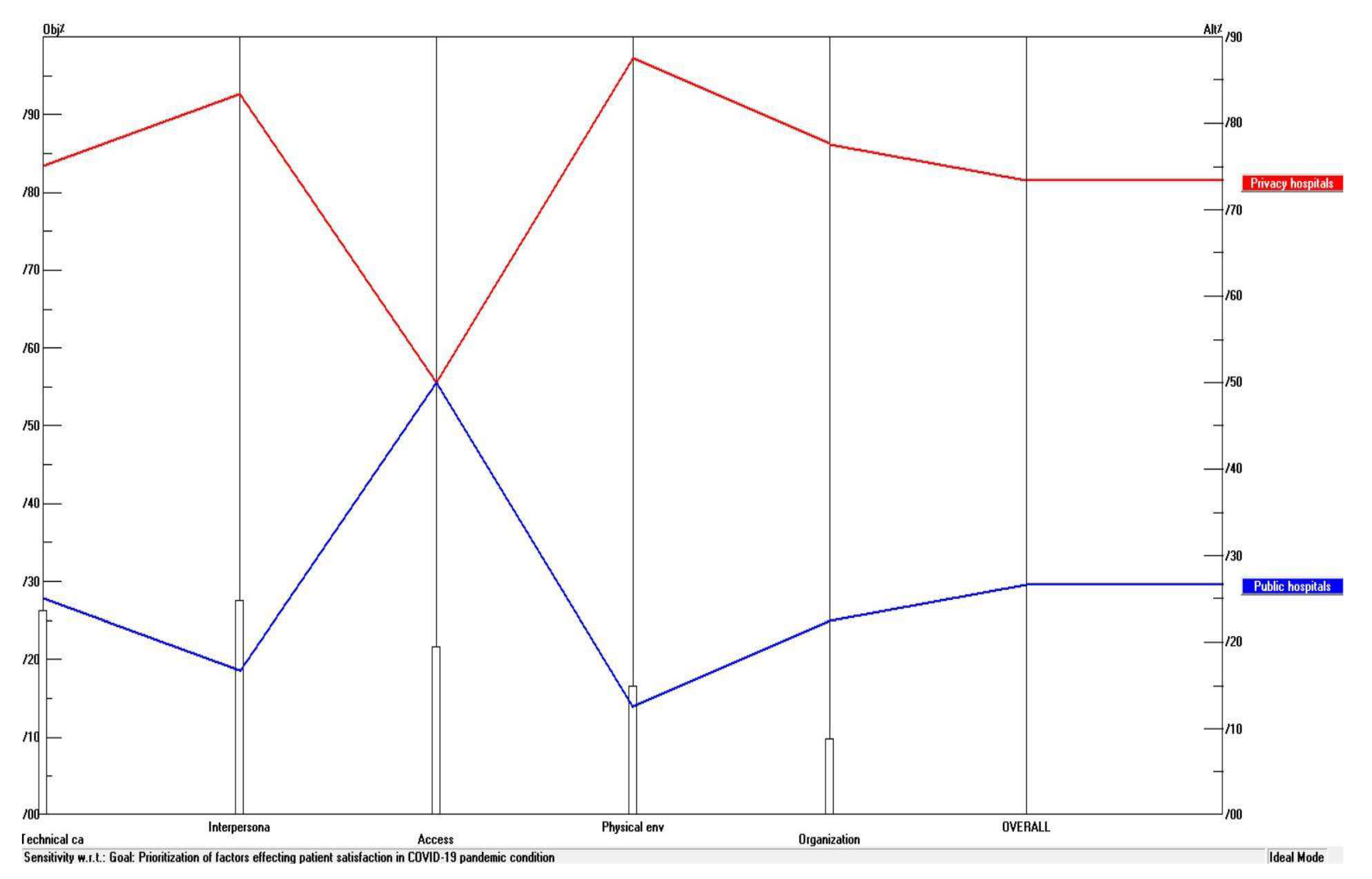
4. Data Analysis and Findings
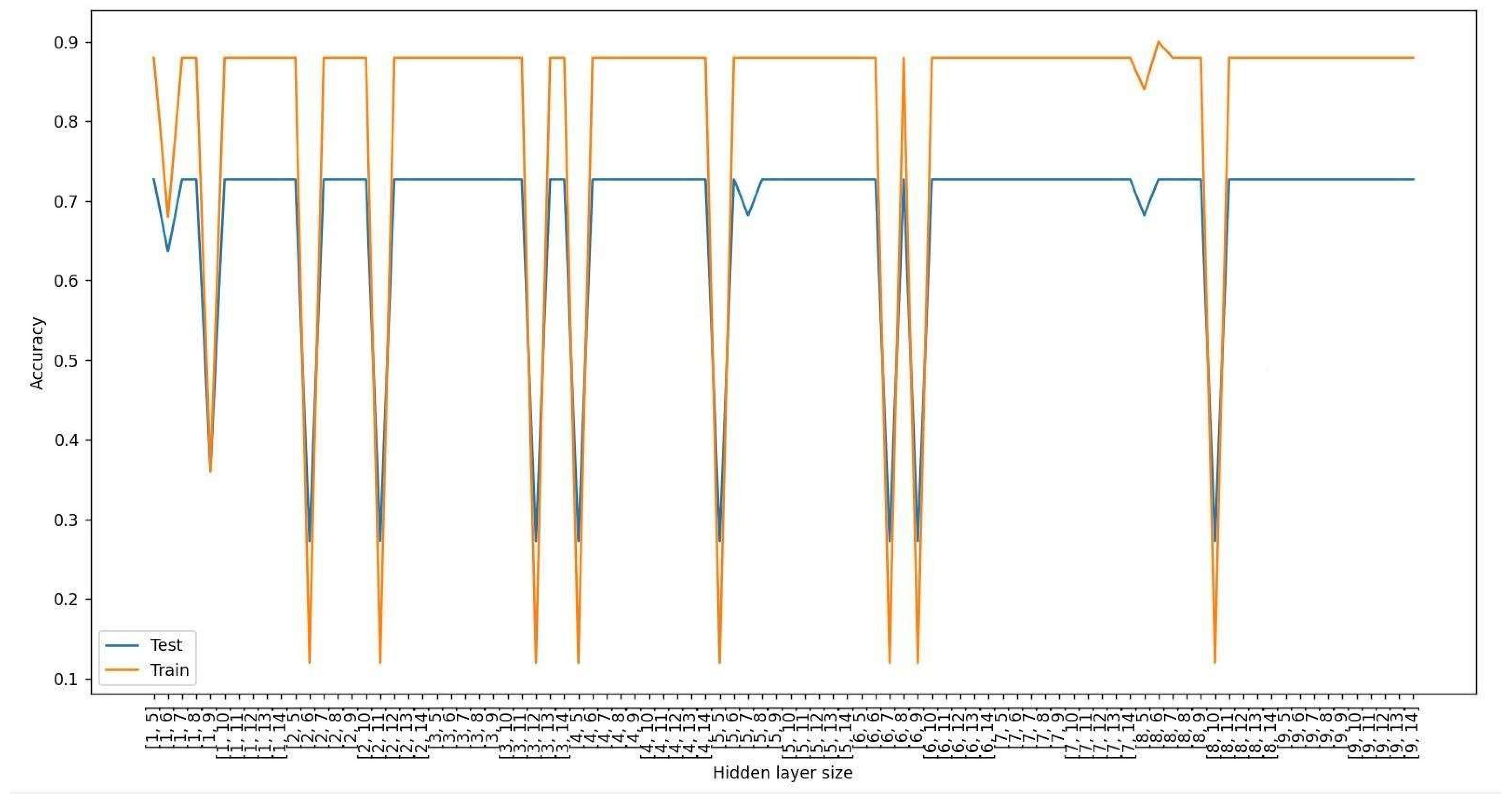
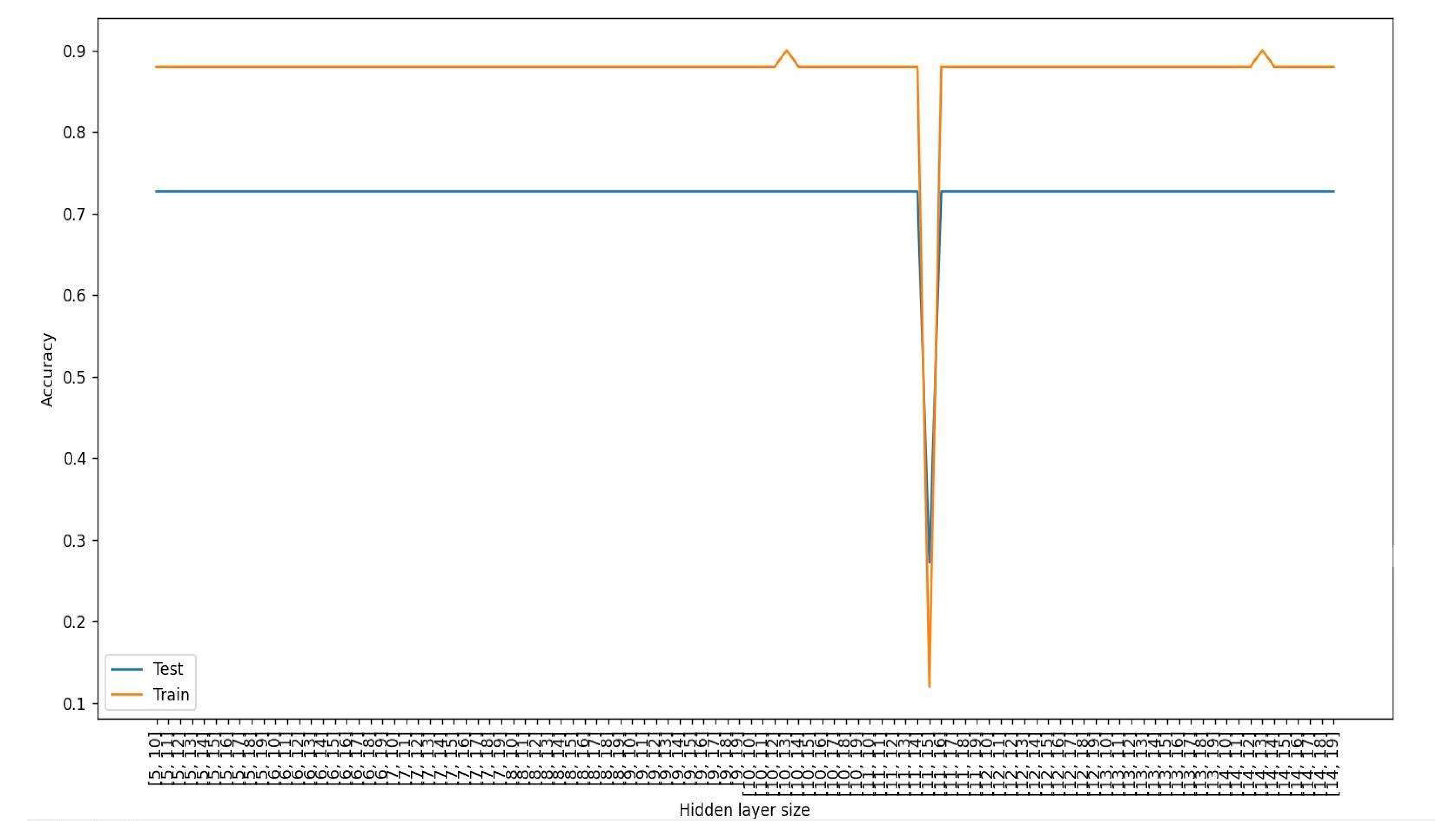
5. Application of ANN-MLP to Predict Accuracy of the Model
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Abbaszadeh, Abbas, Manijeh Eskandari, and Fariba Borhani. 2013. Changing the care process: A new concept in Iranian rural health care. Asian Nursing Research 7: 38–43. [Google Scholar] [CrossRef] [Green Version]
- Akyüz, Ahmet Mutlu, and Hasan Ayyildiz. 2012. A Structural Equation Model Test of Patient Satisfaction in the Health Service Organizations in Trabzon City. Available online: https://www.researchgate.net/publication/265261173_A_STRUCTURAL_EQUATION_MODEL_TEST_OF_PATIENT_SATISFACTION_IN_THE_HEALTH_SERVICE_ORGANIZATIONS_IN_TRABZON_CITY (accessed on 27 May 2022).
- Alasad, Jafar A., and Muayyad M. Ahmad. 2003. Patients’ satisfaction with nursing care in Jordan. International Journal of health Care Quality Assurance 16: 279–85. [Google Scholar] [CrossRef]
- Albayrak, Esra, and Yasemin Claire Erensal. 2004. Using analytic hierarchy process (AHP) to improve human performance: An application of multiple criteria decision making problem. Journal of Intelligent Manufacturing 15: 491–503. [Google Scholar] [CrossRef]
- Alberto Sánchez, Carlos, Francisco Javier Prado-Galbarro, Sonia García-Pérez, and Antonio Sarría Santamera. 2014. Factors associated with patient satisfaction with primary care in Europe: Results from the EUprimecare project. Quality in Primary Care 22: 147–55. [Google Scholar]
- Aloosh, M., A. Salavati, and A. Aloosh. 2019. Economic sanctions threaten population health: The case of Iran. Public Health 169: 10–13. [Google Scholar] [CrossRef]
- Alosaimi, Fahad D., Futoon S. Alsaleh, Luluh Y. Alsughayer, Lamees A. Altamimi, Ibrahim A. Alfurayh, Nashwa M. Abdel-Aziz, and Khalid A. Alsaleh. 2022. Psychosocial and Clinical Predictors of Patient Satisfaction with Cancer Care. Saudi Pharmaceutical Journal 30: 414–20. [Google Scholar] [CrossRef]
- Alzahrani, Ahmed Ibrahim, Hosam Al-Samarraie, Atef Eldenfria, Joana Eva Dodoo, and Nasser Alalwan. 2022. Users’ intention to continue using mHealth services: A DEMATEL approach during the COVID-19 pandemic. Technology in Society 68: 101862. [Google Scholar] [CrossRef]
- Aminbakhsh, Saman, Murat Gunduz, and Rifat Sonmez. 2013. Safety risk assessment using analytic hierarchy process (AHP) during planning and budgeting of construction projects. Journal of Safety Research 46: 99–105. [Google Scholar] [CrossRef]
- Andaleeb, Syed Saad. 2001. Service quality perceptions and patient satisfaction: A study of hospitals in a developing country. Social Science & Medicine 52: 1359–70. [Google Scholar]
- Anuszkiewicz, Karolina, Piotr Stogowski, Marta Zawadzka, Przemysław Waszak, Ewa Sokolewicz, Natalia Aleksandra Dułak, Kamil Dzwilewski, Karolina Jażdżewska, Kamila Karbowiak, Daria Karlińska, and et al. 2022. COVID-19 pandemic influence on epilepsy course in pediatric patients. Epilepsy & Behavior 129: 108581. [Google Scholar]
- Badri, Masood A., Samaa Attia, and Abdulla M. Ustadi. 2009. Healthcare quality and moderators of patient satisfaction: Testing for causality. International Journal of Health Care Quality Assurance 22: 382–410. [Google Scholar] [CrossRef]
- Baffoe, Gideon. 2019. Exploring the utility of Analytic Hierarchy Process (AHP) in ranking livelihood activities for effective and sustainable rural development interventions in developing countries. Evaluation and Program Planning 72: 197–204. [Google Scholar] [CrossRef]
- Batbaatar, Enkhjargal, Javkhlanbayar Dorjdagva, Ariunbat Luvsannyam, Matteo Mario Savino, and Pietro Amenta. 2017. Determinants of patient satisfaction: A systematic review. Perspectives in Public Health 137: 89–101. [Google Scholar] [CrossRef]
- Birhanu, Zewdie, Tsion Assefa, Mirkuzie Woldie, and Sudhakar Morankar. 2010. Determinants of satisfaction with health care provider interactions at health centres in central Ethiopia: A cross sectional study. BMC Health Services Research 10: 78. [Google Scholar] [CrossRef] [Green Version]
- Bouzari, Parisa, Aidin Salamzadeh, Maryam Soleimani, and Pejman Ebrahimi. 2021. Online Social Networks and Women’s Entrepreneurship: A Comparative Study between Iran and Hungary. Journal of Women’s Entrepreneurship and Education (JWEE) 3/4: 61–75. [Google Scholar]
- Carlucci, Daniela, Paolo Renna, and Giovanni Schiuma. 2013. Evaluating service quality dimensions as antecedents to outpatient satisfaction using back propagation neural network. Health Care Management Science 16: 37–44. [Google Scholar] [CrossRef]
- Chahal, Hardeep, and Shivani Mehta. 2013. Modeling patient satisfaction construct in the Indian health care context. International Journal of Pharmaceutical and Healthcare Marketing 7: 75–92. [Google Scholar] [CrossRef]
- Chen, Ming-Kuen, and Shih-Ching Wang. 2010. The critical factors of success for information service industry in developing international market: Using analytic hierarchy process (AHP) approach. Expert Systems with Applications 37: 694–704. [Google Scholar] [CrossRef]
- Cheng, Shou-Hsia, Ming-Chin Yang, and Tung-Liang Chiang. 2003. Patient satisfaction with and recommendation of a hospital: Effects of interpersonal and technical aspects of hospital care. International Journal for Quality in Health Care 15: 345–55. [Google Scholar] [CrossRef]
- Cui, Z., L. Hao, and J. Xu. 2018. Lighting of a cardiac intensive care unit: Emotional and visual effects on patients and nurses. Lighting Research & Technology 50: 701–15. [Google Scholar]
- Danielsen, Kirsten, Oyvind A. Bjertnaes, Andrew Garratt, Oddvar Forland, Hilde Hestad Iversen, and Steinar Hunskaar. 2010. The association between demographic factors, user reported experiences and user satisfaction: Results from three casualty clinics in Norway. BMC Family Practice 11: 73. [Google Scholar] [CrossRef] [Green Version]
- Darko, Amos, Albert Ping Chuen Chan, Ernest Effah Ameyaw, Emmanuel Kingsford Owusu, Erika Pärn, and David John Edwards. 2019. Review of application of analytic hierarchy process (AHP) in construction. International Journal of Construction Management 19: 436–52. [Google Scholar] [CrossRef]
- de la Fuente-Mella, Hanns, Rolando Rubilar, Karime Chahuán-Jiménez, and Victor Leiva. 2021. Modeling COVID-19 cases statistically and evaluating their effect on the economy of countries. Mathematics 9: 1558. [Google Scholar] [CrossRef]
- Ebrahimi, Pejman, Aidin Salamzadeh, Maryam Soleimani, Seyed Mohammad Khansari, Hadi Zarea, and Maria Fekete-Farkas. 2022a. Startups and Consumer Purchase Behavior: Application of Support Vector Machine Algorithm. Big Data and Cognitive Computing 6: 34. [Google Scholar] [CrossRef]
- Ebrahimi, Pejman, Marjan Basirat, Ali Yousefi, Md Nekmahmud, Abbas Gholampour, and Maria Fekete-Farkas. 2022b. Social Networks Marketing and Consumer Purchase Behavior: The Combination of SEM and Unsupervised Machine Learning Approaches. Big Data and Cognitive Computing 6: 35. [Google Scholar] [CrossRef]
- Ebrahimi, Pejman, Sebastian Kot, and Maria Fekete-Farkas. 2020. Platform entrepreneurship: An interpretative structural modeling. Nordic Journal of Media Management 1: 385–400. [Google Scholar]
- Faramarzi, Ahmad, Javad Javan-Noughabi, Seyed Saeed Tabatabaee, Ali Asghar Najafpoor, and Aziz Rezapour. 2021. The lost productivity cost of absenteeism due to COVID-19 in health care workers in Iran: A case study in the hospitals of Mashhad University of Medical Sciences. BMC Health Services Research 21: 1169. [Google Scholar] [CrossRef]
- Fekete-Farkas, Maria, Abbas Gholampour, Parisa Bouzari, Hadi Jarghooiyan, and Pejman Ebrahimi. 2021. How gender and age can affect consumer purchase behavior? Evidence from A microeconomic perspective from Hungary. AD-Minister 39: 25–46. [Google Scholar] [CrossRef]
- Footman, Katharine, Bayard Roberts, Anne Mills, Erica Richardson, and Martin McKee. 2013. Public satisfaction as a measure of health system performance: A study of nine countries in the former Soviet Union. Health Policy 112: 62–69. [Google Scholar] [CrossRef] [Green Version]
- Gholampour, Abbas, Mir Hadi Moazen Jamshidi, Alireza Habibi, Narges Motamedi Dehkordi, and Pejman Ebrahimi. 2020. The Impact of Hospital Information System on Nurses’ Satisfaction in Iranian Public Hospitals: The Moderating Role of Computer Literacy. Journal of Information Technology Management 12: 141–59. [Google Scholar]
- Ghosh, Manimay. 2014. Measuring patient satisfaction: An empirical study in India. Leadership in Health Services 27: 240–54. [Google Scholar] [CrossRef]
- Gopalan, Hema S., and Anoop Misra. 2020. COVID-19 pandemic and challenges for socio-economic issues, healthcare and National Health Programs in India. Diabetes & Metabolic Syndrome: Clinical Research & Reviews 14: 757–59. [Google Scholar]
- Graves, Claire E., Neha Goyal, Anna Levin, Miriam A. Nuño, Jina Kim, Michael J. Campbell, Wen T. Sen, Jessica E. Gosnell, Sanziana A. Roman, Julie A. Sosa, and et al. 2022. Anxiety During the COVID-19 Pandemic: A Web-Based Survey of Thyroid Cancer Survivors. Endocrine Practice 28: 405–13. [Google Scholar] [CrossRef] [PubMed]
- Hall, Judith A., and Michael C. Dornan. 1988. What patients like about their medical care and how often they are asked: A meta-analysis of the satisfaction literature. Social Science & Medicine 27: 935–39. [Google Scholar]
- Hall, Judith A., Julie T. Irish, Debra L. Roter, Carol M. Ehrlich, and Lucy H. Miller. 1994. Satisfaction, gender, and communication in medical visits. Medical Care 32: 1216–31. [Google Scholar] [CrossRef]
- Hemadeh, Randa, Rawan Hammoud, Ola Kdouh, Tarek Jaber, and Lea Ammar. 2019. Patient satisfaction with primary healthcare services in Lebanon. The International Journal of Health Planning and Management 34: e423–e435. [Google Scholar] [CrossRef] [Green Version]
- Imanaka, Y., S. Araki, K. Murata, and K. Nobutomo. 1993. Determinants of patient satisfaction and intention to continue service utilization: Analysis of a survey of outpatients at general hospital. [Nihon Koshu Eisei Zasshi] Japanese Journal of Public Health 40: 624–35. [Google Scholar]
- Improta, Giovanni, Antonietta Perrone, Mario Alessandro Russo, and Maria Triassi. 2019. Health technology assessment (HTA) of optoelectronic biosensors for oncology by analytic hierarchy process (AHP) and Likert scale. BMC Medical Research Methodology 19: 140. [Google Scholar] [CrossRef]
- Jenkinson, Crispin, Angela Coulter, S. Bruster, N. Richards, and T. Chandola. 2002. Patients’ experiences and satisfaction with health care: Results of a questionnaire study of specific aspects of care. Qual Saf Health Care 11: 335–39. [Google Scholar] [CrossRef]
- Lin, Chin-Tsai, and Cheng-Shiung Wu. 2008. Selecting a marketing strategy for private hotels in Taiwan using the analytic hierarchy process. The Service Industries Journal 28: 1077–91. [Google Scholar] [CrossRef]
- Manenti, Ambrogio. 2011. Health situation in Iran. Medical Journal of Islamic Republic of Iran 25: 1–7. [Google Scholar]
- Mazurenko, Olena, Jason Richter, Abby Swanson-Kazley, and Eric Ford. 2016. Examination of the relationship between management and clinician agreement on communication openness, teamwork, and patient satisfaction in the US hospitals. Journal of Hospital Administration 5: 20–27. [Google Scholar] [CrossRef] [Green Version]
- Mazurenko, Olena, Jason Richter, Abby Swanson Kazley, and Eric Ford. 2019. Examination of the relationship between management and clinician perception of patient safety climate and patient satisfaction. Health Care Management Review 44: 79–89. [Google Scholar] [CrossRef]
- Miziara, Roberta Amparado, Jonathan Yugo Maesaka, Danielle Ramos Martin Matsumoto, Laura Penteado, Ariane Andrade dos Santos Anacleto, Tarso Augusto Duenhas Accorsi, Karine De Amicis Lima, and Eduardo Cordioli. 2022. Teleoncology Orientation of Low-Income Breast Cancer Patients during the COVID-19 Pandemic: Feasibility and Patient Satisfaction. Revista Brasileira de Ginecologia e Obstetrícia 43: 840–46. [Google Scholar] [CrossRef]
- Montoya, Madeline I., Cary S. Kogan, Tahilia J. Rebello, Karolina Sadowska, José A. Garcia-Pacheco, Brigitte Khoury, Maya Kulygina, Chihiro Matsumoto, Rebeca Robles, and Jingjing Huang. 2022. An international survey examining the impact of the COVID-19 pandemic on telehealth use among mental health professionals. Journal of Psychiatric Research 148: 188–96. [Google Scholar] [CrossRef]
- Naidu, Aditi. 2009. Factors affecting patient satisfaction and healthcare quality. International Journal of health Care Quality Assurance 22: 366–81. [Google Scholar] [CrossRef]
- Nasiri, Taha, Mohammadkarim Bahadori, Ramin Ravangard, and Mohammad Meskarpour_Amiri. 2020. Factors Affecting the Failure to Report Medical Errors by Nurses Using the Analytical Hierarchy Process (AHP). Hospital Topics 98: 135–44. [Google Scholar] [CrossRef]
- Oppel, Eva-Maria, Vera Winter, and Jonas Schreyögg. 2017. Evaluating the link between human resource management decisions and patient satisfaction with quality of care. Health Care Management Review 42: 53–64. [Google Scholar] [CrossRef]
- Otani, Koichiro, Patrick A. Herrmann, and Richard S. Kurz. 2010. Patient satisfaction integration process: Are there any racial differences? Health Care Management Review 35: 116–23. [Google Scholar] [CrossRef]
- Otani, Koichiro, Patrick A. Herrmann, and Richard S. Kurz. 2011. Improving patient satisfaction in hospital care settings. Health Services Management Research 24: 163–69. [Google Scholar] [CrossRef]
- Otani, Koichiro, Richard S. Kurz, Thomas E. Burroughs, and Brian Waterman. 2003. Reconsidering models of patient satisfaction and behavioral intentions. Health Care Management Review 28: 7–20. [Google Scholar] [CrossRef] [PubMed]
- Ozkoc, H. Hatice, and M. Vedat Pazarlioglu. 2011. Patient satisfaction of in-patients treated in a university hospital in Turkey. Scientific Research and Essays 6: 5555–62. [Google Scholar]
- Petruni, Alberto, Evanthia Giagloglou, Ewan Douglas, Jie Geng, Maria Chiara Leva, and Micaela Demichela. 2019. Applying Analytic Hierarchy Process (AHP) to choose a human factors technique: Choosing the suitable Human Reliability Analysis technique for the automotive industry. Safety Science 119: 229–39. [Google Scholar] [CrossRef] [Green Version]
- Rehman, Salma Abdul, and Parveen Azam Ali. 2016. A review of factors affecting patient satisfaction with nurse led triage in emergency departments. International Emergency Nursing 29: 38–44. [Google Scholar] [CrossRef] [Green Version]
- Roshandel-Arbatani, Taher, Hiroko Kawamorita, Saeid Ghanbary, and Pejman Ebrahimi. 2019. Modelling media entrepreneurship in social media: SEM and MLP-ANN Approach. AD-Minister 34: 35–57. [Google Scholar]
- Russell, Roberta S., Dana M. Johnson, and Sheneeta W. White. 2015. Patient perceptions of quality: Analyzing patient satisfaction surveys. International Journal of Operations & Production Management 35: 1158–81. [Google Scholar]
- Saad Andaleeb, Syed. 1998. Determinants of customer satisfaction with hospitals: A managerial model. International Journal of Health Care Quality Assurance 11: 181–87. [Google Scholar] [CrossRef]
- Saaty, Tomas. 1980. The Analysis Hierarchy Process. New York: McGraw-Hill. [Google Scholar]
- Sadeh, Ehsan. 2017. Interrelationships among quality enablers, service quality, patients’ satisfaction and loyalty in hospitals. The TQM Journal 29: 101–17. [Google Scholar] [CrossRef]
- Salamzadeh, Aidin, and Leo Paul Dana. 2021. The coronavirus (COVID-19) pandemic: Challenges among Iranian startups. Journal of Small Business & Entrepreneurship 33: 489–512. [Google Scholar]
- Schoenfelder, Tonio, Joerg Klewer, and Joachim Kugler. 2011. Determinants of patient satisfaction: A study among 39 hospitals in an in-patient setting in Germany. International Journal for Quality in Health Care 23: 503–9. [Google Scholar] [CrossRef]
- Scotti, Dennis J. 2005. Satisfaction with medical care among elderly patients: A review of research findings with implications for management practice and future inquiry. Journal of Hospital Marketing & Public Relations 15: 3–32. [Google Scholar]
- Shahriarirad, Reza, Zohre Khodamoradi, Amirhossein Erfani, Hamidreza Hosseinpour, Keivan Ranjbar, Yasaman Emami, Alireza Mirahmadizadeh, Mehrzad Lotfi, Babak Shirazi Yeganeh, and Abolfazl Dorrani Nejad. 2020. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infectious Diseases 20: 427. [Google Scholar] [CrossRef] [PubMed]
- Skime, Michelle K., Ajeng J. Puspitasari, Melanie T. Gentry, Dagoberto Heredia Jr., Craig N. Sawchuk, Wendy R. Moore, Monica J. Taylor-Desir, and Kathryn M. Schak. 2022. Patient Satisfaction and Recommendations for Delivering a Group-Based Intensive Outpatient Program via Telemental Health During the COVID-19 Pandemic: Cross-sectional Cohort Study. JMIR Mental Health 9: e30204. [Google Scholar] [CrossRef] [PubMed]
- Solatianaghizi, Ramezan, Pejman Ebrahimi, T. Bazghaleh, and Zahra Norouzi. 2017. The effect of job attitude and affective commitment on OCB of nurses. Pharmacophore 8: 1–11. [Google Scholar]
- Sorra, Joann, Kabir Khanna, Naomi Dyer, Russ Mardon, and Theresa Famolaro. 2012. Exploring relationships between patient safety culture and patients’ assessments of hospital care. Journal of Patient Safety 8: 131–39. [Google Scholar] [CrossRef]
- Stanhope, Kaitlyn K., Kendra Piper, Peggy Goedken, Tatyana Johnson, Naima T. Joseph, Angeline Ti, Franklyn Geary, and Sheree L. Boulet. 2022. Quality and satisfaction with care following changes to the structure of obstetric care during the COVID-19 pandemic in a safety-net hospital in Georgia: Results from a mixed-methods study. Journal of the National Medical Association 114: 94–103. [Google Scholar] [CrossRef]
- Tokunaga, Junya, and Yuichi Imanaka. 2002. Influence of length of stay on patient satisfaction with hospital care in Japan. International Journal for Quality in Health Care 14: 493–502. [Google Scholar] [CrossRef] [Green Version]
- Tokunaga, Junya, Yuichi Imanaka, and Koichi Nobutomo. 2000. Effects of patient demands on satisfaction with Japanese hospital care. International Journal for Quality in Health Care 12: 395–401. [Google Scholar] [CrossRef] [Green Version]
- Tu, Chuc Anh, Ehsan Rasoulinezhad, and Tapan Sarker. 2020. Investigating solutions for the development of a green bond market: Evidence from analytic hierarchy process. Finance Research Letters 34: 101457. [Google Scholar] [CrossRef]
- Varasteh, Saeideh, Maryam Esmaeili, and Monir Mazaheri. 2021. Factors affecting Iranian nurses’ intention to leave or stay in the profession during the COVID-19 pandemic. International Nursing Review 69: 139–49. [Google Scholar] [CrossRef]
- Verma, Surabhi, and Anders Gustafsson. 2020. Investigating the emerging COVID-19 research trends in the field of business and management: A bibliometric analysis approach. Journal of Business Research 118: 253–61. [Google Scholar] [CrossRef] [PubMed]
- Wong, Johnny K. W., and Heng Li. 2008. Application of the analytic hierarchy process (AHP) in multi-criteria analysis of the selection of intelligent building systems. Building and Environment 43: 108–25. [Google Scholar] [CrossRef]
- Xiao, Hong, and Janet P. Barber. 2008. The effect of perceived health status on patient satisfaction. Value in Health 11: 719–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoosefi Lebni, Javad, Jaffar Abbas, Farideh Moradi, Mohammad Reza Salahshoor, Fakhreddin Chaboksavar, Seyed Fahim Irandoost, Nazila Nezhaddadgar, and Arash Ziapour. 2021. How the COVID-19 pandemic effected economic, social, political, and cultural factors: A lesson from Iran. International Journal of Social Psychiatry 67: 298–300. [Google Scholar] [CrossRef]
- Zekhnini, Kamar, Anass Cherrafi, Imane Bouhaddou, and Youssef Benghabrit. 2020. Analytic Hierarchy Process (AHP) for Supply Chain 4.0 Risks Management. In Proceedings of International Conference on Artificial Intelligence & Industrial Applications. Cham: Springer, pp. 89–102. [Google Scholar]
- Zineldin, Mosad. 2006. The quality of health care and patient satisfaction: An exploratory investigation of the 5Qs model at some Egyptian and Jordanian medical clinics. International Journal of Health Care Quality Assurance 19: 60–92. [Google Scholar] [CrossRef]
- Zopf, David, Andrew W. Joseph, and Marc C. Thorne. 2012. Patient and family satisfaction in a pediatric otolaryngology clinic. International Journal of Pediatric Otorhinolaryngology 76: 1339–42. [Google Scholar] [CrossRef]
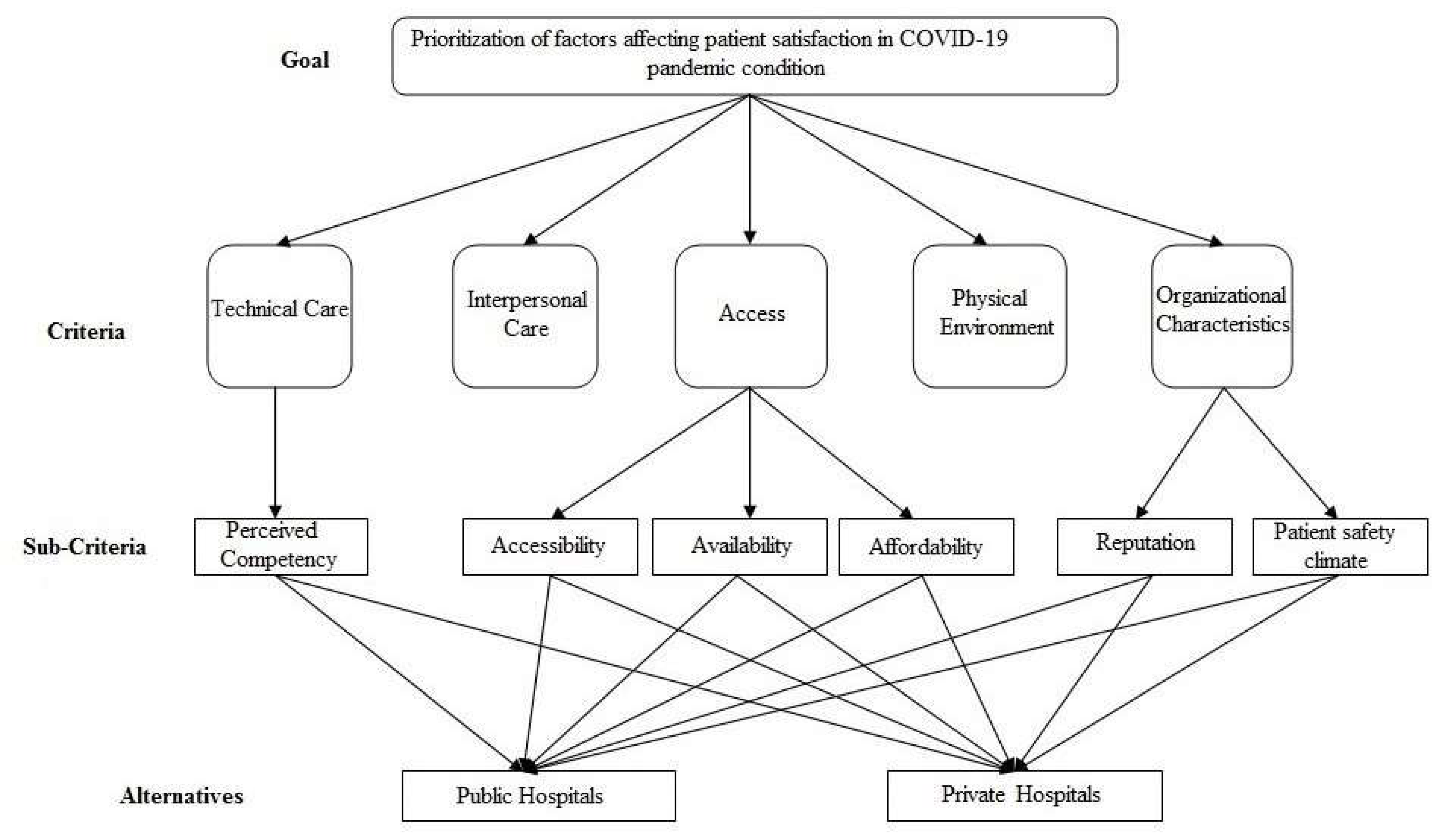
| Categories | Factors | References |
|---|---|---|
| Technical Care | Perceived competency of health professionals | (Andaleeb 2001; Cheng et al. 2003; Hall and Dornan 1988; Saad Andaleeb 1998) |
| Interpersonal care | (Alasad and Ahmad 2003; Alosaimi et al. 2022; Chahal and Mehta 2013; Otani et al. 2003; Rehman and Ali 2016; Stanhope et al. 2022) | |
| Physical environment | (Cui et al. 2018; Ghosh 2014; Ozkoc and Pazarlioglu 2011) | |
| Access | Accessibility | (Montoya et al. 2022; Otani et al. 2003; Zopf et al. 2012) |
| Availability | (Batbaatar et al. 2017; Oppel et al. 2017) | |
| Affordability | (Saad Andaleeb 1998; Xiao and Barber 2008) | |
| Organizational characteristics | Reputation | (Imanaka et al. 1993; Tokunaga et al. 2000) |
| Patient safety climate | (Mazurenko et al. 2016; Mazurenko et al. 2019; Sorra et al. 2012) |
| Criteria | Weights | Ranking | Sub-Criteria | Weights | Ranking |
|---|---|---|---|---|---|
| Technical care | 0.259 | 2 | Perceived competency | 1.000 | |
| Interpersonal care | 0.272 | 1 | |||
| Access | 0.212 | 3 | Accessibility | 0.200 | 5 |
| Availability | 0.400 | 2 | |||
| Affordability | 0.400 | 2 | |||
| Physical environment | 0.162 | 4 | |||
| Organizational characteristics | 0.095 | 5 | Reputation | 0.333 | 4 |
| Patient safety climate | 0.667 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khansari, S.M.; Arbabi, F.; Moazen Jamshidi, M.H.; Soleimani, M.; Ebrahimi, P. Health Services and Patient Satisfaction in IRAN during the COVID-19 Pandemic: A Methodology Based on Analytic Hierarchy Process and Artificial Neural Network. J. Risk Financial Manag. 2022, 15, 288. https://doi.org/10.3390/jrfm15070288
Khansari SM, Arbabi F, Moazen Jamshidi MH, Soleimani M, Ebrahimi P. Health Services and Patient Satisfaction in IRAN during the COVID-19 Pandemic: A Methodology Based on Analytic Hierarchy Process and Artificial Neural Network. Journal of Risk and Financial Management. 2022; 15(7):288. https://doi.org/10.3390/jrfm15070288
Chicago/Turabian StyleKhansari, Seyed Mohammad, Farzin Arbabi, Mir Hadi Moazen Jamshidi, Maryam Soleimani, and Pejman Ebrahimi. 2022. "Health Services and Patient Satisfaction in IRAN during the COVID-19 Pandemic: A Methodology Based on Analytic Hierarchy Process and Artificial Neural Network" Journal of Risk and Financial Management 15, no. 7: 288. https://doi.org/10.3390/jrfm15070288
APA StyleKhansari, S. M., Arbabi, F., Moazen Jamshidi, M. H., Soleimani, M., & Ebrahimi, P. (2022). Health Services and Patient Satisfaction in IRAN during the COVID-19 Pandemic: A Methodology Based on Analytic Hierarchy Process and Artificial Neural Network. Journal of Risk and Financial Management, 15(7), 288. https://doi.org/10.3390/jrfm15070288








