Investigation on the Potential Use of Polypropylene Mesh for the Reinforcement of Heat-Polymerized PMMA Denture Base Resin
Abstract
1. Introduction
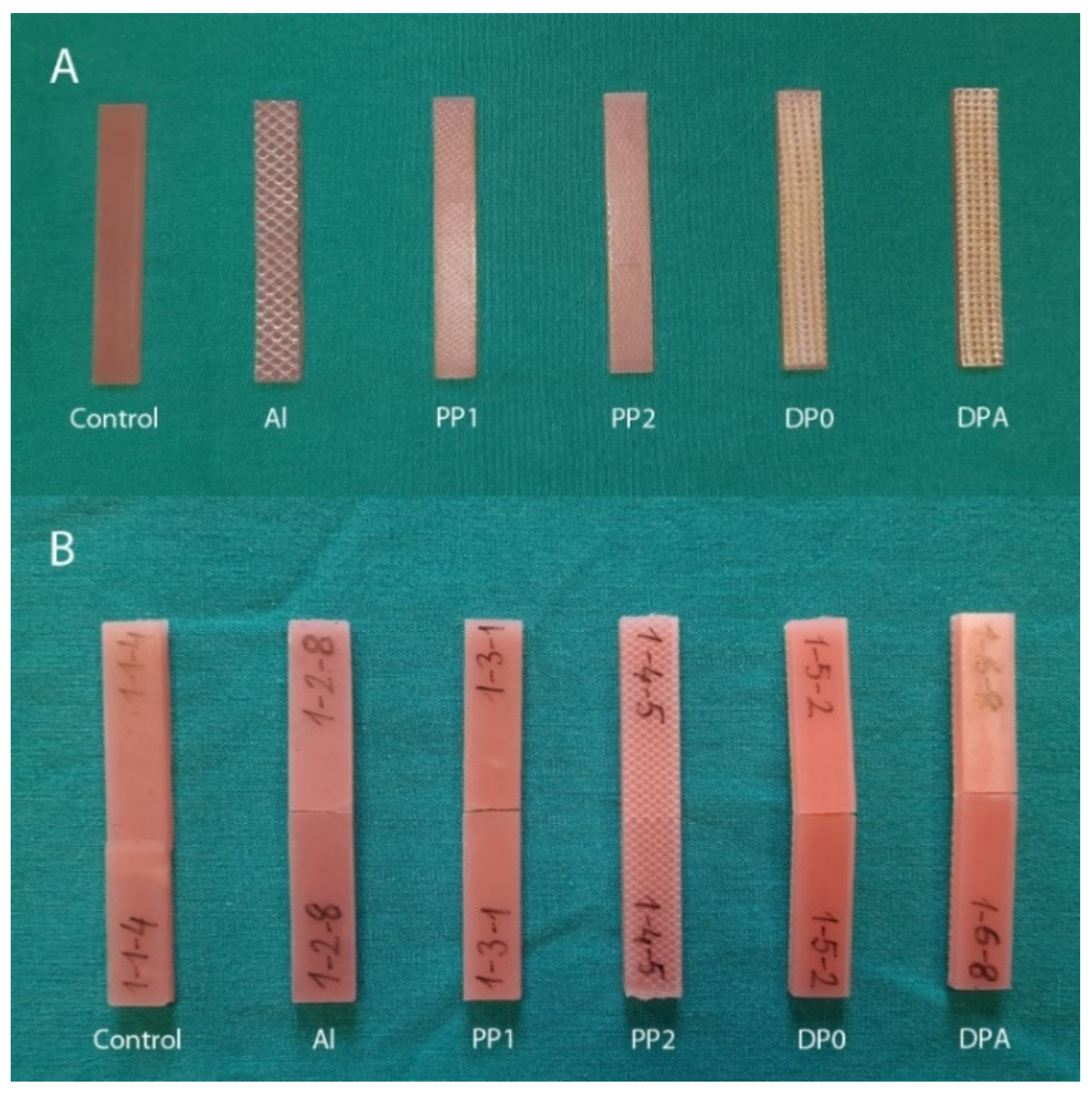
2. Materials and Methods
3. Results
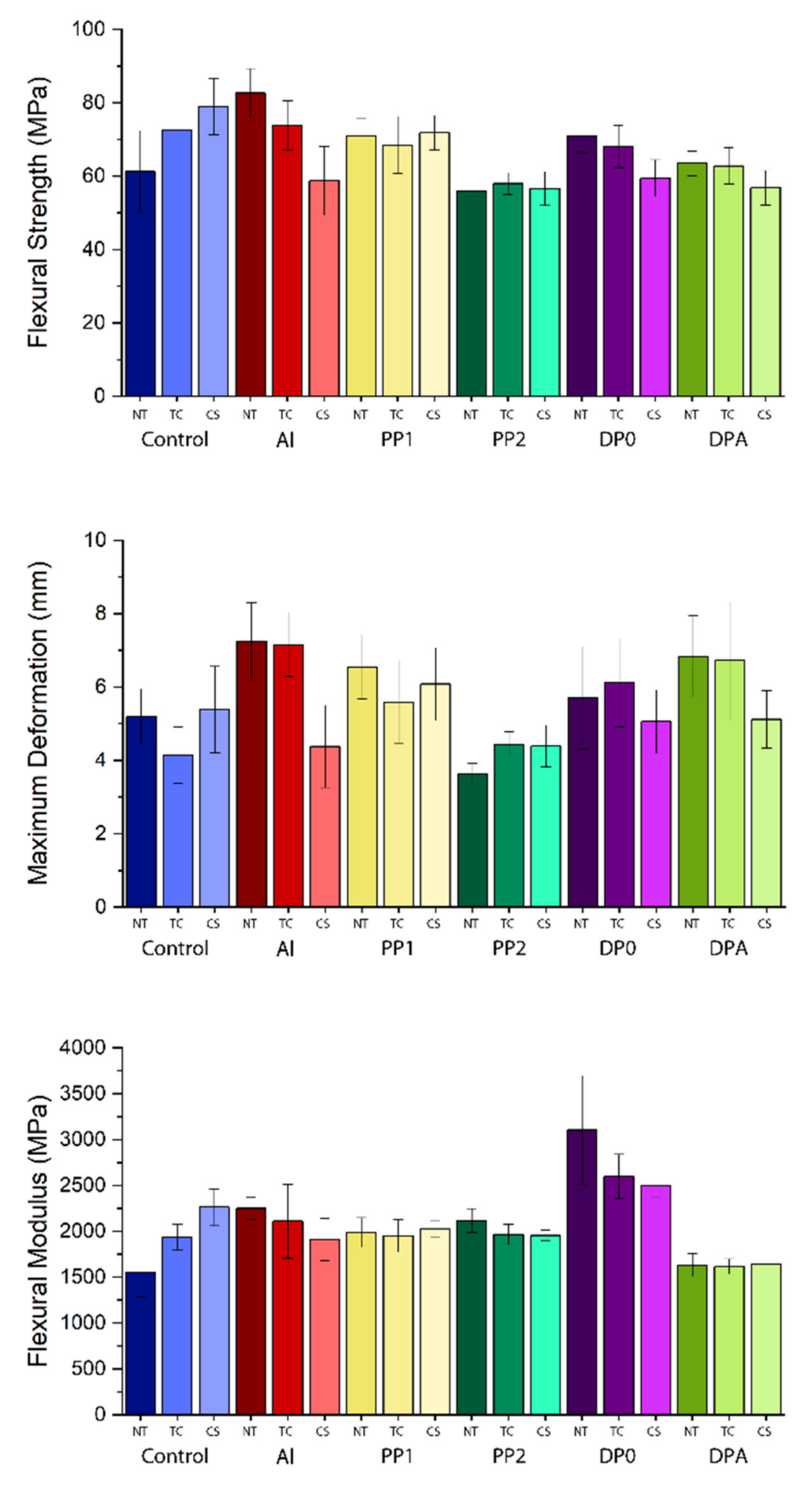
3.1. Mechanical Tests
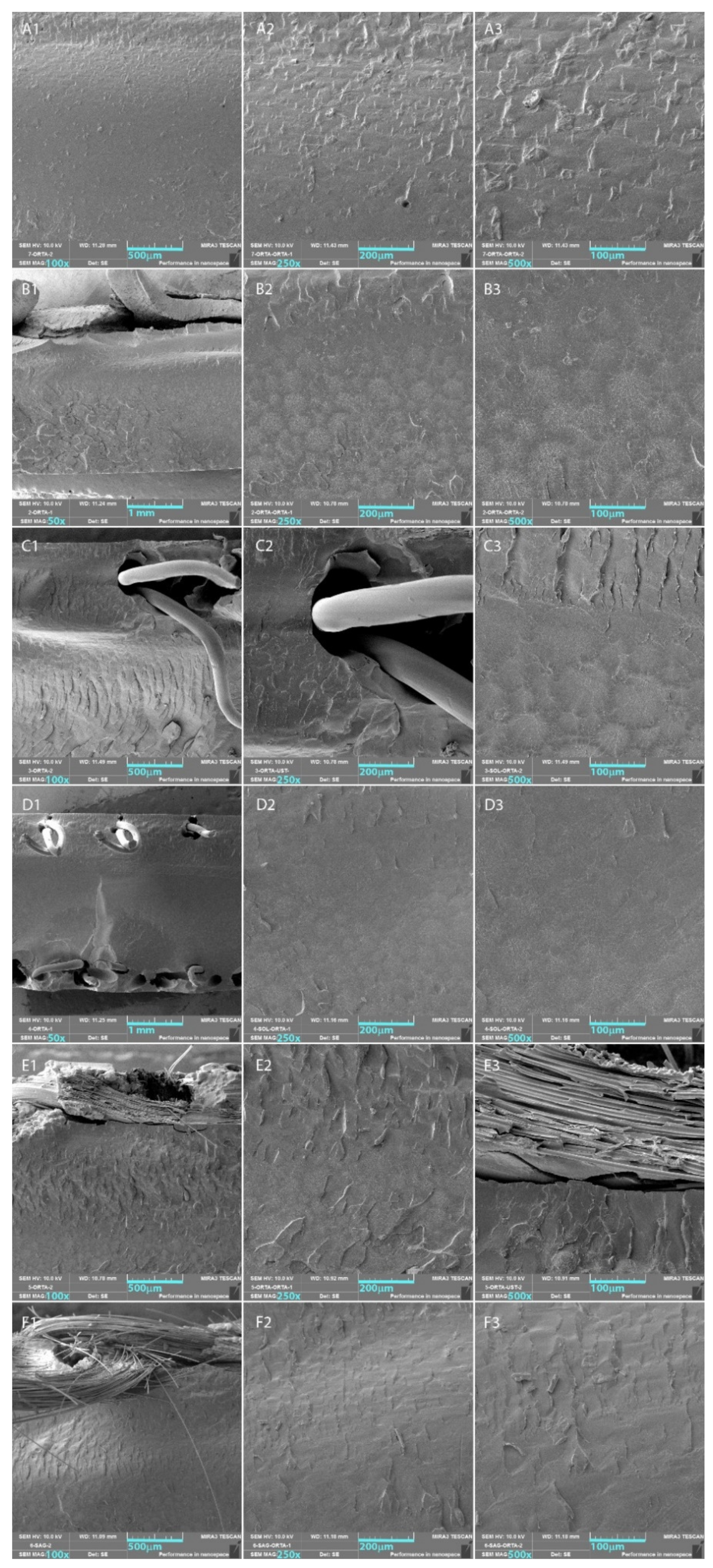
3.2. SEM Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Uzun, G.; Hersek, N.; Tincer, T. Effect of five woven fiber reinforcements on the impact and transverse strength of a denture base resin. J. Prosthet. Dent. 1999, 81, 616–620. [Google Scholar] [CrossRef]
- Al-Dwairi, Z.N.; Tahboub, K.Y.; Baba, N.Z.; Goodacre, C.J.; Özcan, M. A comparison of the surface properties of CAD/CAM and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 2019, 28, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.Y.; Liang, W.M.; Yen, P.S. Reinforcement of acrylic denture base resin by incorporation of various fibers. J. Biomed. Mater. Res. (Appl. Biomater.) 2001, 58, 203–208. [Google Scholar] [CrossRef]
- Gad, M.M.; Abualsaud, R.; Fouda, S.M.; Rahoma, A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Al-Harbi, F.A. Effects of denture cleansers on the flexural strength of PMMA denture base resin modified with ZrO2 nanoparticles. J. Prosthodont. 2021, 30, 235–244. [Google Scholar] [CrossRef]
- John, J.; Gangadhar, S.A.; Shah, I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J. Prosthet. Dent. 2001, 86, 424–427. [Google Scholar] [CrossRef]
- Spasojevic, P.; Zrilic, M.; Panic, V.; Stamenkovic, D.; Seslija, S.; Velickovic, S. The mechanical properties of a poly (methyl methacrylate) denture base material modified with dimethyl itaconate and di-n-butyl itaconate. Int. J. Polym. Sci. 2015, 2015, 561012. [Google Scholar] [CrossRef]
- Gad, M.M.; Al-Thobity, A.M.; Rahoma, A.; Abualsaud, R.; Al-Harbi, F.A.; Akhtar, S. Reinforcement of PMMA denture base material with a mixture of ZrO2 nanoparticles and glass fibers. Int. J. Dent. 2019, 2019, 2489393. [Google Scholar] [CrossRef]
- Somani, M.V.; Khandelwal, M.; Punia, V.; Sharma, V. The effect of incorporating various reinforcement materials on flexural strength and impact strength of polymethylmethacrylate: A meta-analysis. J. Indian Prosthodont. Soc. 2019, 19, 101–112. [Google Scholar] [CrossRef]
- Salih, S.I.; Oleiwi, J.K.; Mohamed, A.S. Investigation of mechanical properties of PMMA composite reinforced with different types of natural powders. J. Eng. Appl. Sci. (Asian Res. Publ. Netw.) 2018, 13, 8889–8900. [Google Scholar]
- Mowade, T.K.; Dange, S.P.; Thakre, M.B.; Kamble, V.D. Effect of fiber reinforcement on impact strength of heat polymerized polymethyl methacrylate denture base resin: In vitro study and SEM analysis. J. Adv. Prosthodont. 2012, 4, 30–36. [Google Scholar] [CrossRef]
- Johnston, E.P.; Nicholls, J.I.; Smith, D.E. Flexure fatigue of 10 commonly used denture base resins. J. Prosthet. Dent. 1981, 46, 478–483. [Google Scholar] [CrossRef]
- Zaghloul, M.M.Y.; Zaghloul, M.Y.M.; Zaghloul, M.M.Y. Experimental and modeling analysis of mechanical-electrical behaviors of polypropylene composites filled with graphite and MWCNT fillers. Polym. Test. 2017, 63, 467–474. [Google Scholar] [CrossRef]
- Zaghloul, M.Y.M.; Zaghloul, M.M.Y.; Zaghloul, M.M.Y. Developments in polyester composite materials–An in-depth review on natural fibres and nano fillers. Compos. Struct. 2021, 278, 114698. [Google Scholar] [CrossRef]
- Zaghloul, M.M.Y.; Mohamed, Y.S.; El-Gamal, H. Fatigue and tensile behaviors of fiber-reinforced thermosetting composites embedded with nanoparticles. J. Compos. Mater. 2019, 53, 709–718. [Google Scholar] [CrossRef]
- Zaghloul, M.M.Y.; Zaghloul, M.M.Y. Influence of flame retardant magnesium hydroxide on the mechanical properties of high density polyethylene composites. J. Reinf. Plast. Compos. 2017, 36, 1802–1816. [Google Scholar] [CrossRef]
- Fuseini, M.; Zaghloul, M.M.Y.; Elkady, M.F.; El-Shazly, A.H. Evaluation of synthesized polyaniline nanofibres as corrosion protection film coating on copper substrate by electrophoretic deposition. J. Mater. Sci. 2022, 57, 6085–6101. [Google Scholar] [CrossRef]
- Zaghloul, M.M.Y.M. Mechanical properties of linear low-density polyethylene fire-retarded with melamine polyphosphate. J. Appl. Polym. Sci. 2018, 135, 46770. [Google Scholar] [CrossRef]
- Banerjee, S.; Engelmeier, R.L.; O’Keefe, K.L.; Powers, J.M. In vitro tensile bond strength of denture repair acrylic resins to primed base metal alloys using two different processing techniques. J. Prosthodont. 2009, 18, 676–683. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Lassila, V.P. Effect of metal strengthener’s surface roughness on fracture resistance of acrylic denture base material. J. Oral Rehabil. 1992, 19, 385–391. [Google Scholar] [CrossRef]
- Özdemir, A.K.; Özdemir-Doğan, D.; Tuğut, F.; Demir, H.; Akin, H. Effects of boron on the mechanical properties of polymethylmethacrylate denture base material. Eur. Oral Res. 2021, 55, 45–53. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int. J. Nanomed. 2017, 12, 3801–3812. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Abualsaud, R.; Alqarawi, F.K.; Emam, A.N.M.; Khan, S.Q.; Akhtar, S.; Mahrous, A.A.; Al-Harbi, F.A. Translucency of nanoparticle-reinforced PMMA denture base material: An invitro comparative study. Dent. Mater. J. 2021, 40, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Alla, R.K.; Sajjan, S.; Alluri, V.R.; Ginjupalli, K.; Upadhya, N. Influence of fiber reinforcement on the properties of denture base resins. J. Biomater. Nanobiotechnol. 2013, 4, 91–97. [Google Scholar] [CrossRef]
- Mallikarjuna Murthy, H.B.; Shaik, S.; Sachdeva, H.; Khare, S.; Haralur, S.B.; Roopa, K.T. Effect of reinforcement using stainless steel mesh, glass fibers, and polyethylene on the impact strength of heat cure denture base resin—An in vitro study. J. Int. Oral Health 2015, 7, 71–79. [Google Scholar]
- Rana, M.H.; Shaik, S.; Hameed, M.S.; Al-Saleh, S.; AlHamdan, E.M.; Alshahrani, A.; Alqahtani, A.; Albaqawi, A.H.; Vohra, F.; Abduljabbar, T. Influence of dental glass fibers and orthopedic mesh on the failure loads of polymethyl methacrylate denture base resin. Polymers 2021, 13, 2793. [Google Scholar] [CrossRef]
- Sakaguchi, R.L.; Powers, J.M. Craig’s Restorative Dental Materials; Elsevier Mosby: Philadelphia, PA, USA, 2012. [Google Scholar]
- Im, S.M.; Huh, Y.H.; Cho, L.R.; Park, C.J. Comparison of the fracture resistances of glass fiber mesh-and metal mesh-reinforced maxillary complete denture under dynamic fatigue loading. J. Adv. Prosthodont. 2017, 9, 22–30. [Google Scholar] [CrossRef]
- Ardakani, Z.H.; Giti, R.; Dabiri, S.; Hosseini, A.H.; Moayedi, M. Flexural strength of polymethyl methacrylate reinforced with high-performance polymer and metal mesh. Dent. Res. J. 2021, 18, 30. [Google Scholar]
- Yu, S.H.; Cho, H.W.; Oh, S.; Bae, J.M. Effects of glass fiber mesh with different fiber content and structures on the compressive properties of complete dentures. J. Prosthet. Dent. 2015, 113, 636–644. [Google Scholar] [CrossRef]
- Abbas, S.O.; Mahfouz, O.A.; Aboushelib, M.N.; Rady, N.A. Evaluation of impact strength of heat cure acrylic resin reinforced with nylon fiber mesh with and without prestressing (in vitro study). Alex. Dent. J. 2021, 46, 85–90. [Google Scholar] [CrossRef]
- Mathew, M.; Shenoy, K.; Ravishankar, K.S. Impact strength of poly propylene fiber reinforced PMMA. Int. J. Sci. Eng. Res. 2014, 5, 951–955. [Google Scholar]
- Mathew, M.; Shenoy, K.; Ravishankar, K.S. Flexural strength of hydrogen plasma-treated polypropylene fiber-reinforced polymethyl methacrylate denture base material. J. Indian Prosthodont. Soc. 2018, 18, 257–262. [Google Scholar] [CrossRef]
- Cobb, W.S.; Kercher, K.W.; Heniford, B.T. The argument for lightweight polypropylene mesh in hernia repair. Surg. Innov. 2005, 12, 63–69. [Google Scholar] [CrossRef]
- 178:2003; Plastics—Determination of Flexural Properties. ISO: Geneva, Switzerland, 2019.
- Prechtel, A.; Reymus, M.; Edelhoff, D.; Hickel, R.; Stawarczyk, B. Comparison of various 3D printed and milled PAEK materials: Effect of printing direction and artificial aging on Martens parameters. Dent. Mater. 2020, 36, 197–209. [Google Scholar] [CrossRef]
- Ramadan, R.; Elsherbeeny, Y.; Thabet, Y.; Kandil, B.; Ghali, R. Retention of a telescopic overdenture on customized abutments after the simulation of 1 year in function. Dent. Med. Probl. 2021, 58, 201–206. [Google Scholar] [CrossRef]
- Benli, M.; Eker-Gümüş, B.; Kahraman, Y.; Gökçen-Rohlig, B.; Evlioğlu, G.; Huck, O.; Özcan, M. Surface roughness and wear behavior of occlusal splint materials made of contemporary and high-performance polymers. Odontology 2020, 108, 240–250. [Google Scholar] [CrossRef]
- Park, J.H.; Park, S.; Lee, K.; Yun, K.D.; Lim, H.P. Antagonist wear of three CAD/CAM anatomic contour zirconia ceramics. J. Prosthet. Dent. 2014, 111, 20–29. [Google Scholar] [CrossRef]
- Yu, S.H.; Ahn, D.H.; Park, J.S.; Chung, Y.S.; Han, I.S.; Lim, J.S.; Oh, S.; Oda, Y.; Bae, J.M. Comparison of denture base resin reinforced with polyaromatic polyamide fibers of different orientations. Dent. Mater. J. 2013, 32, 332–340. [Google Scholar] [CrossRef][Green Version]
- Fonseca, R.B.; Favarão, I.N.; Kasuya, A.V.B.; Abrão, M.; Luz, N.F.M.; Naves, L.Z. Influence of glass fiber wt% and silanization on mechanical flexural strength of reinforced acrylics. J. Mater. Sci. Chem. Eng. 2014, 2, 11–15. [Google Scholar] [CrossRef][Green Version]
- Vallittu, P.K. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven glass fibers. J. Prosthet. Dent. 1999, 81, 318–326. [Google Scholar] [CrossRef]
- Kanie, T.; Arikawa, H.; Fujii, K.; Ban, S. Deformation and flexural properties of denture base polymer reinforced with glass fiber sheet. Dent. Mater. J. 2005, 24, 297–303. [Google Scholar] [CrossRef][Green Version]
- Singh, K.; Sharma, S.K.; Negi, P.; Kumar, M.; Rajpurohit, D.; Khobre, P. Comparative evaluation of flexural strength of heat polymerised denture base resins after reinforcement with glass fibres and nylon fibres: An in vitro study. Adv. Hum. Biol. 2016, 6, 91–94. [Google Scholar] [CrossRef]
- Calamote, C.; Coelho, I.C.; Silva, A.S.; Esteves, J.L.; Moreira, L.; Pinto, A.C.; Manzanares-Céspedes, M.C.; Escuín, T. Comparison of the masticatory force (with 3D Models) of complete denture base acrylic resins with reline and reinforcing materials. Materials 2021, 14, 3308. [Google Scholar] [CrossRef]
- Vojvodic, D.; Komar, D.; Schauperl, Z.; Celebic, A.; Mehulic, K.; Zabarovic, D. Influence of different glass fiber reinforcements on denture base polymer strength (Fiber reinforcements of dental polymer). Med. Glas. 2009, 6, 227–234. [Google Scholar]
- Takahashi, Y.; Yoshida, K.; Shimizu, H. Effect of location of glass fiber-reinforced composite reinforcement on the flexural properties of a maxillary complete denture in vitro. Acta Odontol. Scand. 2011, 69, 215–221. [Google Scholar] [CrossRef]
- Foo, S.H.; Lindquist, T.J.; Aquilino, S.A.; Schneider, R.L.; Williamson, D.L.; Boyer, D.B. Effect of polyaramid fiber reinforcement on the strength of 3 Denture Base polymethyl methacrylate resin. J. Prosthodont. 2001, 3, 148–153. [Google Scholar] [CrossRef]
- Balch, J.H.; Smith, P.D.; Marin, M.A.; Cagna, D.R. Reinforcement of a mandibular complete denture with internal metal framework. J. Prosthet. Dent. 2013, 109, 202–205. [Google Scholar] [CrossRef]
- Hirajima, Y.; Takahashi, H.; Minakushi, S. Influence of a denture strengthener on the deformation of a maxillary complete denture. Dent. Mater. J. 2009, 28, 507–512. [Google Scholar] [CrossRef][Green Version]
- Vogdani, M.; Bagheri, R.; Khaledi, A.A.R. Effects of aluminum oxide addition on the flexural strength, surface hardness, and roughness of heat-polymerized acrylic resin. J. Dent. Sci. 2012, 7, 238–244. [Google Scholar] [CrossRef]
- Silva, E.P.E.; Rosa, E.L.; Barbosa, S.V. Tissue reactions to polypropylene mesh used in maxillofacial trauma. Braz. Dent. J. 2001, 12, 121–125. [Google Scholar]
- Dogan, O.M.; Bolayir, G.; Keshin, S.; Dogan, A.; Bek, B. The evaluation of some flexural properties of a denture base resin reinforced with various aesthetic fibers. J. Mater. Sci. Mater. Med. 2008, 19, 2343–2349. [Google Scholar] [CrossRef] [PubMed]
- Praveen, B.; Babaji, H.V.; Prasanna, B.G.; Rajalbandi, S.K.; Sheeharsha, T.V.; Prashant, G.M. Comparison of impact strength and fracture morphology of different heat cure denture acrylic resins: An in vitro study. J. Int. Oral Health 2014, 6, 12–16. [Google Scholar] [PubMed]
- Bertassoni, L.E.; Marshall, G.W.; Souza, E.M.; Rached, R.N. Effect of pre and post polymerization on flexural strength and elastic modules of impregnated, fiber-reinforced denture base acrylic resins. J. Prosthet. Dent. 2008, 100, 449–457. [Google Scholar] [CrossRef]
| Material | Density g/cm3 | Tensile Strength (MPa) | Elongation at Break (%) |
|---|---|---|---|
| Al | 2.7 | 54.62 | 32.54 |
| PP | 0.9 | 14.24 | 53.13 |
| DPA | 2.5 | 34.87 | 36.68 |
| Variable | Comparison | Sum of Squares | df | Mean Square | F | p |
|---|---|---|---|---|---|---|
| Flexural strength | Treatment | 432.343 | 2 | 216.171 | 5.548 | 0.005 * |
| Mesh reinforcement | 4438.059 | 5 | 887.612 | 22.780 | 0.000 * | |
| Treatment x mesh reinforcement | 4047.818 | 10 | 404.782 | 10.389 | 0.000 * | |
| Maximum deformation | Treatment | 16.831 | 2 | 8.416 | 8.537 | 0.000 * |
| Mesh reinforcement | 86.273 | 5 | 17.255 | 17.503 | 0.000 * | |
| Treatment x mesh reinforcement | 59.213 | 10 | 5.921 | 6.007 | 0.000 * | |
| Flexural modulus | Treatment | 161,098.685 | 2 | 80,549.342 | 1.565 | 0.213 |
| Mesh reinforcement | 15,999,143.508 | 5 | 3,199,828.702 | 62.182 | 0.000 * | |
| Treatment x mesh reinforcement | 4,155,670.119 | 10 | 415,567.012 | 8.076 | 0.000 * |
| Treatment or Mesh Group | Flexural Strength (MPa) | Maximum Deformation (mm) | Flexural Modulus (MPa) |
|---|---|---|---|
| No treatment | 67.58 ± 10.47 (x) | 5.86 ± 1.53 (x) | 2109.42 ± 582.13 (x) |
| Thermal cycling | 67.33 ± 8.08 (x) | 5.70 ± 1.50 (x) | 2030.30 ± 362.65 (x) |
| Chewing simulation | 63.78 ± 10.49 (y) | 5.07 ± 1.07 (y) | 2051.45 ± 310.46 (x) |
| Control | 70.96 ± 11.43 (a) | 4.91 ± 1.04 (de) | 1919.50 ± 356.70 (b) |
| Al | 71.76 ± 12.47 (a) | 6.26 ± 1.67 (ab) | 2091.22 ± 300.41 (b) |
| PP1 | 70.46 ± 5.82 (a) | 6.08 ± 1.04 (ac) | 1991.47 ± 143.56 (b) |
| PP2 | 56.88 ± 3.46 (b) | 4.16 ± 55 (e) | 2013.36 ± 125.12 (b) |
| DP0 | 66.24 ± 7.02 (a) | 5.63 ± 1.21 (bcd) | 2735.07 ± 449.88 (a) |
| DPA | 61.07 ± 5.19 (b) | 6.23 ± 1.41 (a) | 1631.73 ± 115.94 (c) |
| Treatment | Mesh Group | Flexural Strength (MPa) | Maximum Deformation (mm) | Flexural Modulus (MPa) |
|---|---|---|---|---|
| No treatment | Control | 61.28 ± 11.17 (y,c) | 5.20 ± 0.75 (x,b) | 1556.98 ± 270.62 (z,c) |
| Al | 82.66 ± 6.65 (x,a) | 7.25 ± 1.05 (x,a) | 2251.24 ± 124.29 (x,b) | |
| PP1 | 71.01 ± 4.70 (x,b) | 6.55 ± 0.87 (x,ab) | 1991.45 ± 160.91 (x,b) | |
| PP2 | 55.98 ± 2.66 (x,c) | 3.64 ± 0.28 (x,c) | 2117.56 ± 130.41 (x,b) | |
| DP0 | 71.04 ± 4.62 (x,b) | 5.70 ± 1.40 (x,ab) | 3106.07 ± 588.68 (x,a) | |
| DPA | 63.49 ± 3.38 (x,bc) | 6.84 ± 1.11 (x,a) | 1633.25 ± 122.86 (x,c) | |
| Thermal cycle | Control | 72.60 ± 7.84 (x,a) | 4.15 ± 0.77 (x,c) | 1936.88 ± 138.48 (y,b) |
| Al | 73.87 ± 6.73 (y,a) | 7.16 ± 0.87 (x,a) | 2109.74 ± 403.53 (xy,b) | |
| PP1 | 68.49 ± 7.75 (x,ab) | 5.59 ± 1.13 (x,b) | 1952.45 ± 174.58 (x,b) | |
| PP2 | 58.03 ± 2.96 (x,c) | 4.44 ± 0.34 (x,c) | 1966.98 ± 110.54 (x,b) | |
| DP0 | 68.16 ± 5.79 (x,ab) | 6.12 ± 1.20 (x,ab) | 2598.06 ± 243.44 (y,a) | |
| DPA | 62.82 ± 4.94 (x,bc) | 6.72 ± 1.60 (x,ab) | 1617.71 ± 86.06 (x,c) | |
| Chewing simulation | Control | 78.99 ± 7.70 (x,a) | 5.39 ± 1.18 (x,ab) | 2264.64 ± 197.42 (x,a) |
| Al | 58.76 ± 9.34 (z,b) | 4.38 ± 1.12 (y,b) | 1912.68 ± 228.39 (y,bc) | |
| PP1 | 71.89 ± 4.71 (x,a) | 6.08 ± 0.99 (x,a) | 2030.53 ± 88.67 (x,b) | |
| PP2 | 56.64 ± 4.59 (x,b) | 4.39 ± 0.57 (x,b) | 1955.54 ± 59.41 (x,bc) | |
| DP0 | 59.51 ± 4.98 (y,b) | 5.06 ± 0.86 (x,ab) | 2501.07 ± 133.68 (y,a) | |
| DPA | 56.90 ± 4.74 (x,b) | 5.12 ± 0.78 (y,ab) | 1644.24 ± 145.81(x,c) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yerliyurt, K.; Eğri, S. Investigation on the Potential Use of Polypropylene Mesh for the Reinforcement of Heat-Polymerized PMMA Denture Base Resin. Polymers 2022, 14, 3300. https://doi.org/10.3390/polym14163300
Yerliyurt K, Eğri S. Investigation on the Potential Use of Polypropylene Mesh for the Reinforcement of Heat-Polymerized PMMA Denture Base Resin. Polymers. 2022; 14(16):3300. https://doi.org/10.3390/polym14163300
Chicago/Turabian StyleYerliyurt, Kaan, and Sinan Eğri. 2022. "Investigation on the Potential Use of Polypropylene Mesh for the Reinforcement of Heat-Polymerized PMMA Denture Base Resin" Polymers 14, no. 16: 3300. https://doi.org/10.3390/polym14163300
APA StyleYerliyurt, K., & Eğri, S. (2022). Investigation on the Potential Use of Polypropylene Mesh for the Reinforcement of Heat-Polymerized PMMA Denture Base Resin. Polymers, 14(16), 3300. https://doi.org/10.3390/polym14163300






