Artificial Intelligence in Colorectal Cancer Surgery: Present and Future Perspectives
Abstract
Simple Summary
Abstract
1. Introduction
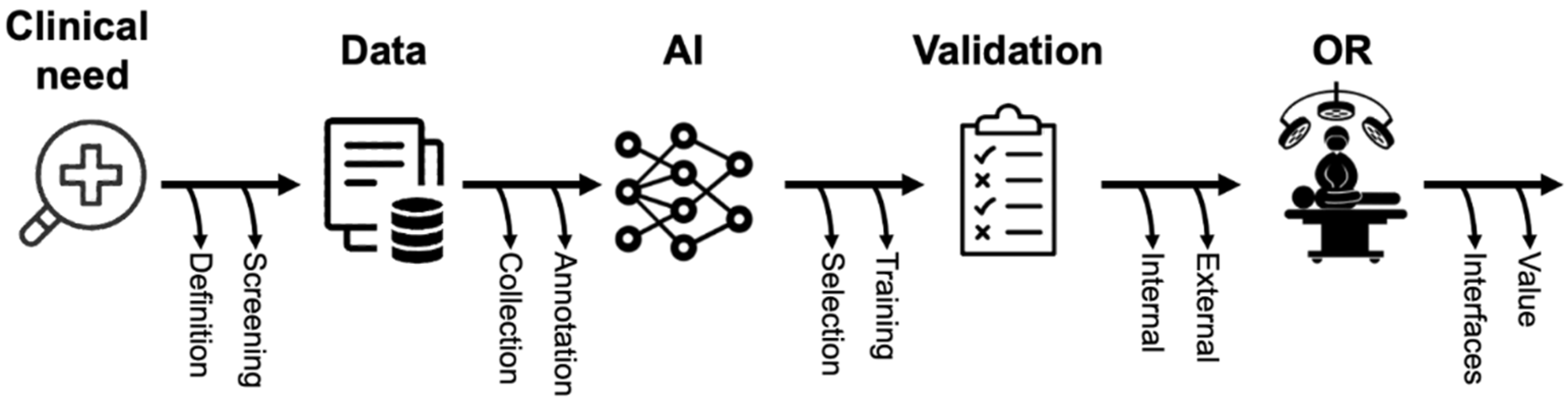
2. A Brief Introduction to AI for Surgeons
3. State-of-the-Art of the Intraoperative Application of AI
- Accuracy
- Sensitivity
- Specificity
- Intersection over Union (IoU)
- F1 Score
- Dice coefficient
- Receiver operating characteristics curve (ROC curve)
- Area under the curve (AUC)
3.1. Phase and Action Recognition
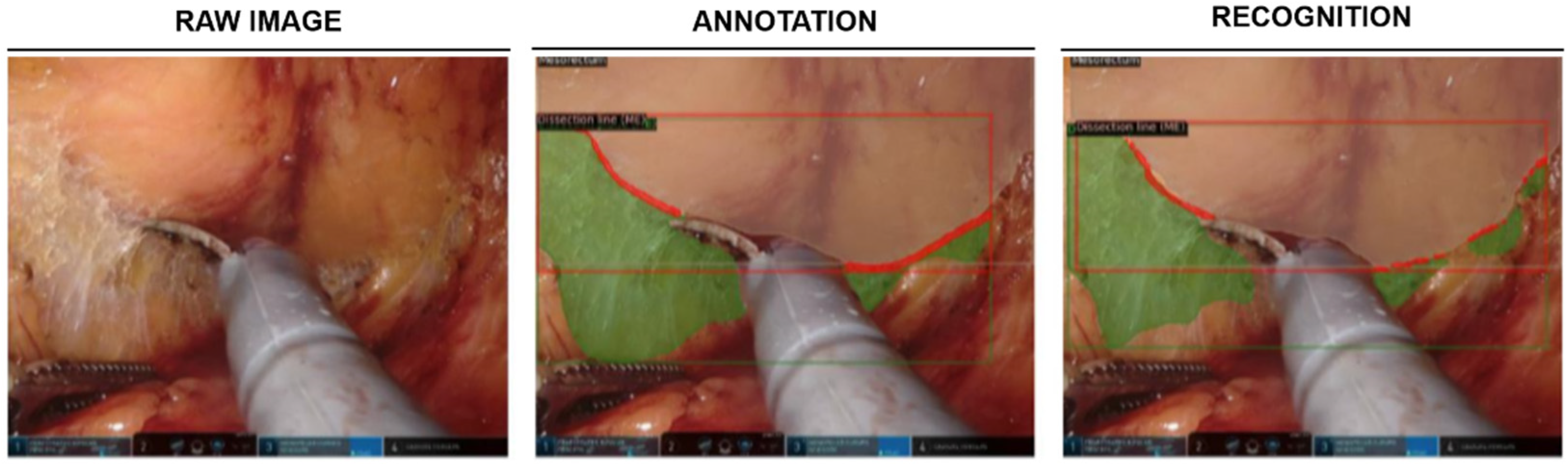
3.2. Intraoperative Guidance
3.3. Indocyanine Green Fluorescence in Colorectal Surgery: Can Artificial Intelligence Take the Next Step?
3.4. AI for Surgical Training in Colorectal Surgery
| First Author | Year | Task | Study Design (Study Period) | Cohort | AI Model | Validation | Performance |
|---|---|---|---|---|---|---|---|
| Kitaguchi, D. [44] | 2020 | Phase recognition, action classification and tool segmentation | Multicentic retrospective study (2009–2019) | 300 procedures (235 LSs; 65 LRRs) | Xception, U-Net | Out-of-sample | Phase recognition mean accuracy: 81.0% Action classification mean accuracy: 83.2% Tool segmentation mean IoU: 51.2% |
| Park, S.H. [65] | 2020 | Perfusion assessment | Monocentric study (2018–2019) | 65 LRRs | - | Out-of-sample | AUC: 0.842 Recall: 100% F1 score: 75% |
| Kitaguchi, D. [45] | 2020 | Phase recognition and action detection | Monocentric retrospective study (2009–2017) | 71 LSs | Inception-ResNet-v2 | Out-of-sample | Phase recognition (Phases 1–9):
|
| Kitaguchi, D. [70] | 2021 | Surgical skill assessment | Monocentric retrospective study (2016–2017 | 74 procedures (LSs and LHARs) | Inception-v1 I3D | Leave-one-out cross validation | Classification in 3 performance groups, mean accuracy:
|
| Kitaguchi, D. [46] | 2022 | Phase and step recognition | Monocentric retrospective study (2018–2019) | 50 TaTMEs | Xception | Out-of-sample | Phase recognition:
|
| Igaki, T. [55] | 2022 | Plane of dissection recognition | Monocentric study (2015–2019) | 32 LSs/LRRs | - | Out-of-sample validation | Accuracy of areolar tissue segmentation: 84% |
| Kolbinger, F.R. [54] | 2022 | Phase and step recognition, segmentation of anatomical structures and planes of dissection | Monocentric retrospective study (2019–2021) | 57 robot-assisted rectal resections | Phase recognition: LSTM, ResNet50 Segmentation: Detectron2, ResNet50 | Phase recognition: 4-fold cross validation Segmentation: Leave-one-out cross validation | Phase recognition:
Gerota’s fascia:
|
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Fitzmaurice, C.; Abate, D.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdel-Rahman, O.; Abdelalim, A.; Abdoli, A.; Abdollahpour, I.; Abdulle, A.S.M.; et al. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived with Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2019, 5, 1749–1768. [Google Scholar] [CrossRef] [PubMed]
- Mandel, J.S.; Bond, J.H.; Church, T.R.; Snover, D.C.; Bradley, G.M.; Schuman, L.M.; Ederer, F. Reducing Mortality from Colorectal Cancer by Screening for Fecal Occult Blood. N. Engl. J. Med. 1993, 328, 1365–1371. [Google Scholar] [CrossRef] [PubMed]
- Miller, K.D.; Nogueira, L.; Mariotto, A.B.; Rowland, J.H.; Yabroff, K.R.; Alfano, C.M.; Jemal, A.; Kramer, J.L.; Siegel, R.L. Cancer Treatment and Survivorship Statistics, 2019. CA Cancer J. Clin. 2019, 69, 363–385. [Google Scholar] [CrossRef]
- Xie, Y.H.; Chen, Y.X.; Fang, J.Y. Comprehensive Review of Targeted Therapy for Colorectal Cancer. Signal Transduct. Target. Ther. 2020, 5, 22. [Google Scholar] [CrossRef]
- Angelucci, G.P.; Sinibaldi, G.; Orsaria, P.; Arcudi, C.; Colizza, S. Morbidity and Mortality after Colorectal Surgery for Cancer. Surg. Sci. 2013, 4, 520–524. [Google Scholar] [CrossRef][Green Version]
- Alves, A.; Panis, Y.; Mathieu, P.; Mantion, G.; Kwiatkowski, F.; Slim, K. Postoperative Mortality and Morbidity in French Patients Undergoing Colorectal Surgery: Results of a Prospective Multicenter Study. Arch. Surg. 2005, 140, 278–283. [Google Scholar] [CrossRef]
- Mascagni, P.; Longo, F.; Barberio, M.; Seeliger, B.; Agnus, V.; Saccomandi, P.; Hostettler, A.; Marescaux, J.; Diana, M. New Intraoperative Imaging Technologies: Innovating the Surgeon’s Eye toward Surgical Precision. J. Surg. Oncol. 2018, 118, 265–282. [Google Scholar] [CrossRef]
- Mascagni, P.; Padoy, N. OR Black Box and Surgical Control Tower: Recording and Streaming Data and Analytics to Improve Surgical Care. J. Visc. Surg. 2021, 158, S18–S25. [Google Scholar] [CrossRef]
- Anteby, R.; Horesh, N.; Soffer, S.; Zager, Y.; Barash, Y.; Amiel, I.; Rosin, D.; Gutman, M.; Klang, E. Deep Learning Visual Analysis in Laparoscopic Surgery: A Systematic Review and Diagnostic Test Accuracy Meta-Analysis. Surg. Endosc. 2021, 35, 1521–1533. [Google Scholar] [CrossRef]
- Padoy, N. Machine and Deep Learning for Workflow Recognition during Surgery. Minim. Invasive Ther. Allied Technol. 2019, 28, 82–90. [Google Scholar] [CrossRef]
- Madani, A.; Namazi, B.; Altieri, M.S.; Hashimoto, D.A.; Rivera, A.M.; Pucher, P.H.; Navarrete-Welton, A.; Sankaranarayanan, G.; Brunt, L.M.; Okrainec, A.; et al. Artificial Intelligence for Intraoperative Guidance: Using Semantic Segmentation to Identify Surgical Anatomy During Laparoscopic Cholecystectomy. Ann. Surg. 2020; epub ahead of printing. [Google Scholar]
- Mascagni, P.; Vardazaryan, A.; Alapatt, D.; Urade, T.; Emre, T.; Fiorillo, C.; Pessaux, P.; Mutter, D.; Marescaux, J.; Costamagna, G.; et al. Artificial Intelligence for Surgical Safety: Automatic Assessment of the Critical View of Safety in Laparoscopic Cholecystectomy Using Deep Learning. Ann. Surg. 2021, 275, 955–961. [Google Scholar] [CrossRef]
- Mascagni, P.; Alapatt, D.; Urade, T.; Vardazaryan, A.; Mutter, D.; Marescaux, J.; Costamagna, G.; Dallemagne, B.; Padoy, N. A Computer Vision Platform to Automatically Locate Critical Events in Surgical Videos: Documenting Safety in Laparoscopic Cholecystectomy. Ann. Surg. 2021, 274, e93–e95. [Google Scholar] [CrossRef]
- Mascagni, P.; Alapatt, D.; Laracca, G.G.; Guerriero, L.; Spota, A.; Fiorillo, C.; Vardazaryan, A.; Quero, G.; Alfieri, S.; Baldari, L.; et al. Multicentric Validation of EndoDigest: A Computer Vision Platform for Video Documentation of the Critical View of Safety in Laparoscopic Cholecystectomy. Surg. Endosc. 2022, 1–8. [Google Scholar] [CrossRef]
- Takeuchi, M.; Collins, T.; Ndagijimana, A.; Kawakubo, H.; Kitagawa, Y.; Marescaux, J.; Mutter, D.; Perretta, S.; Hostettler, A.; Dallemagne, B. Automatic Surgical Phase Recognition in Laparoscopic Inguinal Hernia Repair with Artificial Intelligence. Hernia 2022, 1–10. [Google Scholar] [CrossRef]
- Ramesh, S.; Dall’Alba, D.; Gonzalez, C.; Yu, T.; Mascagni, P.; Mutter, D.; Marescaux, J.; Fiorini, P.; Padoy, N. Multi-Task Temporal Convolutional Networks for Joint Recognition of Surgical Phases and Steps in Gastric Bypass Procedures. Int. J. Comput. Assist. Radiol. Surg. 2021, 16, 1111–1119. [Google Scholar] [CrossRef]
- Hashimoto, D.A.; Rosman, G.; Witkowski, E.R.; Stafford, C.; Navarette-Welton, A.J.; Rattner, D.W.; Lillemoe, K.D.; Rus, D.L.; Meireles, O.R. Computer Vision Analysis of Intraoperative Video: Automated Recognition of Operative Steps in Laparoscopic Sleeve Gastrectomy. Ann. Surg. 2019, 270, 414–421. [Google Scholar] [CrossRef]
- Hassan, C.; Spadaccini, M.; Iannone, A.; Maselli, R.; Jovani, M.; Chandrasekar, V.T.; Antonelli, G.; Yu, H.; Areia, M.; Dinis-Ribeiro, M.; et al. Performance of Artificial Intelligence in Colonoscopy for Adenoma and Polyp Detection: A Systematic Review and Meta-Analysis. Gastrointest. Endosc. 2021, 93, 77–85.e6. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Kudo, S.E.; Misawa, M.; Saito, Y.; Ikematsu, H.; Hotta, K.; Ohtsuka, K.; Urushibara, F.; Kataoka, S.; Ogawa, Y.; et al. Real-Time Use of Artificial Intelligence in Identification of Diminutive Polyps during Colonoscopy a Prospective Study. Ann. Intern. Med. 2018, 169, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Ichimasa, K.; Kudo, S.E.; Mori, Y.; Misawa, M.; Matsudaira, S.; Kouyama, Y.; Baba, T.; Hidaka, E.; Wakamura, K.; Hayashi, T.; et al. Artificial Intelligence May Help in Predicting the Need for Additional Surgery after Endoscopic Resection of T1 Colorectal Cancer. Endoscopy 2018, 50, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Maier-Hein, L.; Wagner, M.; Ross, T.; Reinke, A.; Bodenstedt, S.; Full, P.M.; Hempe, H.; Mindroc-Filimon, D.; Scholz, P.; Tran, T.N.; et al. Heidelberg Colorectal Data Set for Surgical Data Science in the Sensor Operating Room. Sci. Data 2021, 8, 101. [Google Scholar] [CrossRef]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-Level Classification of Skin Cancer with Deep Neural Networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef]
- Korbar, B.; Olofson, A.; Miraflor, A.; Nicka, C.; Suriawinata, M.; Torresani, L.; Suriawinata, A.; Hassanpour, S. Deep Learning for Classification of Colorectal Polyps on Whole-Slide Images. J. Pathol. Inform. 2017, 8, 30. [Google Scholar] [CrossRef]
- Campanella, G.; Hanna, M.G.; Geneslaw, L.; Miraflor, A.; Werneck Krauss Silva, V.; Busam, K.J.; Brogi, E.; Reuter, V.E.; Klimstra, D.S.; Fuchs, T.J. Clinical-Grade Computational Pathology Using Weakly Supervised Deep Learning on Whole Slide Images. Nat. Med. 2019, 25, 1301–1309. [Google Scholar] [CrossRef]
- Repici, A.; Badalamenti, M.; Maselli, R.; Correale, L.; Radaelli, F.; Rondonotti, E.; Ferrara, E.; Spadaccini, M.; Alkandari, A.; Fugazza, A.; et al. Efficacy of Real-Time Computer-Aided Detection of Colorectal Neoplasia in a Randomized Trial. Gastroenterology 2020, 159, 512–520.e7. [Google Scholar] [CrossRef]
- Wang, P.; Liu, X.; Berzin, T.M.; Glissen Brown, J.R.; Liu, P.; Zhou, C.; Lei, L.; Li, L.; Guo, Z.; Lei, S.; et al. Effect of a Deep-Learning Computer-Aided Detection System on Adenoma Detection during Colonoscopy (CADe-DB Trial): A Double-Blind Randomised Study. Lancet Gastroenterol. Hepatol. 2020, 5, 343–351. [Google Scholar] [CrossRef]
- Alapatt, D.; Mascagni, P.; Srivastav, V.; Padoy, N. Artificial Intelligence in Surgery: Neural Networks and Deep Learning. arXiv 2020, arXiv:2009.13411. [Google Scholar]
- Ward, T.M.; Mascagni, P.; Ban, Y.; Rosman, G.; Padoy, N.; Meireles, O.; Hashimoto, D.A. Computer Vision in Surgery. Surgery 2021, 169, 1253–1256. [Google Scholar] [CrossRef]
- Mascagni, P.; Fiorillo, C.; Urade, T.; Emre, T.; Yu, T.; Wakabayashi, T.; Felli, E.; Perretta, S.; Swanstrom, L.; Mutter, D.; et al. Formalizing Video Documentation of the Critical View of Safety in Laparoscopic Cholecystectomy: A Step towards Artificial Intelligence Assistance to Improve Surgical Safety. Surg. Endosc. 2020, 34, 2709–2714. [Google Scholar] [CrossRef]
- Ward, T.M.; Fer, D.M.; Ban, Y.; Rosman, G.; Meireles, O.R.; Hashimoto, D.A. Challenges in Surgical Video Annotation. Comput. Assist. Surg. 2021, 26, 58–68. [Google Scholar] [CrossRef]
- Meireles, O.R.; Rosman, G.; Altieri, M.S.; Carin, L.; Hager, G.; Madani, A.; Padoy, N.; Pugh, C.M.; Sylla, P.; Ward, T.M.; et al. SAGES Consensus Recommendations on an Annotation Framework for Surgical Video. Surg. Endosc. 2021, 35, 4918–4929. [Google Scholar] [CrossRef]
- Mascagni, P.; Alapatt, D.; Garcia, A.; Okamoto, N.; Vardazaryan, A.; Costamagna, G.; Dallemagne, B.; Padoy, N. Surgical Data Science for Safe Cholecystectomy: A Protocol for Segmentation of Hepatocystic Anatomy and Assessment of the Critical View of Safety. arXiv 2021, arXiv:2106.10916. [Google Scholar]
- Reinke, A.; Tizabi, M.D.; Sudre, C.H.; Eisenmann, M.; Rädsch, T.; Baumgartner, M.; Acion, L.; Antonelli, M.; Arbel, T.; Bakas, S.; et al. Common Limitations of Image Processing Metrics: A Picture Story. arXiv 2021, arXiv:2104.05642. [Google Scholar]
- Munir, K.; Elahi, H.; Ayub, A.; Frezza, F.; Rizzi, A. Cancer Diagnosis Using Deep Learning: A Bibliographic Review. Cancers 2019, 11, 1235. [Google Scholar] [CrossRef]
- Bar, O.; Neimark, D.; Zohar, M.; Hager, G.D.; Girshick, R.; Fried, G.M.; Wolf, T.; Asselmann, D. Impact of Data on Generalization of AI for Surgical Intelligence Applications. Sci. Rep. 2020, 10, 22208. [Google Scholar] [CrossRef]
- Cruz Rivera, S.; Liu, X.; Chan, A.W.; Denniston, A.K.; Calvert, M.J.; Ashrafian, H.; Beam, A.L.; Collins, G.S.; Darzi, A.; Deeks, J.J.; et al. Guidelines for Clinical Trial Protocols for Interventions Involving Artificial Intelligence: The SPIRIT-AI Extension. Lancet Digit. Health 2020, 2, e549–e560. [Google Scholar] [CrossRef]
- Vasey, B.; Nagendran, M.; Campbell, B.; Clifton, D.A.; Collins, G.S.; Denaxas, S.; Denniston, A.K.; Faes, L.; Geerts, B.; Ibrahim, M.; et al. Reporting Guideline for the Early-Stage Clinical Evaluation of Decision Support Systems Driven by Artificial Intelligence: DECIDE-AI. Nat. Med. 2022, 28, 924–933. [Google Scholar] [CrossRef]
- Liu, X.; Cruz Rivera, S.; Moher, D.; Calvert, M.J.; Denniston, A.K.; Chan, A.W.; Darzi, A.; Holmes, C.; Yau, C.; Ashrafian, H.; et al. Reporting Guidelines for Clinical Trial Reports for Interventions Involving Artificial Intelligence: The CONSORT-AI Extension. Nat. Med. 2020, 26, 1364–1374. [Google Scholar] [CrossRef] [PubMed]
- Weede, O.; Dittrich, F.; Worn, H.; Jensen, B.; Knoll, A.; Wilhelm, D.; Kranzfelder, M.; Schneider, A.; Feussner, H. Workflow Analysis and Surgical Phase Recognition in Minimally Invasive Surgery. In Proceedings of the 2012 IEEE International Conference on Robotics and Biomimetics, ROBIO 2012—Conference Digest, Guangzhou, China, 11–14 December 2012. [Google Scholar]
- Garrow, C.R.; Kowalewski, K.F.; Li, L.; Wagner, M.; Schmidt, M.W.; Engelhardt, S.; Hashimoto, D.A.; Kenngott, H.G.; Bodenstedt, S.; Speidel, S.; et al. Machine Learning for Surgical Phase Recognition: A Systematic Review. Ann. Surg. 2021, 273, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Kassem, H.; Alapatt, D.; Mascagni, P.; Consortium, A.; Karargyris, A.; Padoy, N. Federated Cycling (FedCy): Semi-Supervised Federated Learning of Surgical Phases. arXiv 2022, arXiv:2203.07345. [Google Scholar]
- Ward, T.M.; Hashimoto, D.A.; Ban, Y.; Rattner, D.W.; Inoue, H.; Lillemoe, K.D.; Rus, D.L.; Rosman, G.; Meireles, O.R. Automated Operative Phase Identification in Peroral Endoscopic Myotomy. Surg. Endosc. 2021, 35, 4008–4015. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Takeshita, N.; Matsuzaki, H.; Oda, T.; Watanabe, M.; Mori, K.; Kobayashi, E.; Ito, M. Automated Laparoscopic Colorectal Surgery Workflow Recognition Using Artificial Intelligence: Experimental Research. Int. J. Surg. 2020, 79, 88–94. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Takeshita, N.; Matsuzaki, H.; Takano, H.; Owada, Y.; Enomoto, T.; Oda, T.; Miura, H.; Yamanashi, T.; Watanabe, M.; et al. Real-Time Automatic Surgical Phase Recognition in Laparoscopic Sigmoidectomy Using the Convolutional Neural Network-Based Deep Learning Approach. Surg. Endosc. 2020, 34, 4924–4931. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Takeshita, N.; Matsuzaki, H.; Hasegawa, H.; Igaki, T.; Oda, T.; Ito, M. Deep Learning-Based Automatic Surgical Step Recognition in Intraoperative Videos for Transanal Total Mesorectal Excision. Surg. Endosc. 2022, 36, 1143–1151. [Google Scholar] [CrossRef]
- Heald, R.J.; Ryall, R.D.H. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986, 327, 1479–1482. [Google Scholar] [CrossRef]
- Mackenzie, H.; Miskovic, D.; Ni, M.; Parvaiz, A.; Acheson, A.G.; Jenkins, J.T.; Griffith, J.; Coleman, M.G.; Hanna, G.B. Clinical and Educational Proficiency Gain of Supervised Laparoscopic Colorectal Surgical Trainees. Surg. Endosc. 2013, 27, 2704–2711. [Google Scholar] [CrossRef]
- Martínez-Pérez, A.; de’Angelis, N. Oncologic Results of Conventional Laparoscopic TME: Is the Intramesorectal Plane Really Acceptable? Tech. Coloproctol. 2018, 22, 831–834. [Google Scholar] [CrossRef]
- Martínez-Pérez, A.; Carra, M.C.; Brunetti, F.; De’Angelis, N. Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer: A Systematic Review and Meta-Analysis. JAMA Surg. 2017, 152, e165665. [Google Scholar] [CrossRef]
- Zeng, W.G.; Liu, M.J.; Zhou, Z.X.; Wang, Z.J. A Distal Resection Margin of ≤1 Mm and Rectal Cancer Recurrence After Sphincter-Preserving Surgery: The Role of a Positive Distal Margin in Rectal Cancer Surgery. Dis. Colon Rectum 2017, 60, 1175–1183. [Google Scholar] [CrossRef]
- Rickles, A.S.; Dietz, D.W.; Chang, G.J.; Wexner, S.D.; Berho, M.E.; Remzi, F.H.; Greene, F.L.; Fleshman, J.W.; Abbas, M.A.; Peters, W.; et al. High Rate of Positive Circumferential Resection Margins Following Rectal Cancer Surgery a Call to Action. Ann. Surg. 2015, 262, 891–898. [Google Scholar] [CrossRef]
- Leonard, D.; Penninckx, F.; Fieuws, S.; Jouret-Mourin, A.; Sempoux, C.; Jehaes, C.; Van Eycken, E. Factors Predicting the Quality of Total Mesorectal Excision for Rectal Cancer. Ann. Surg. 2010, 252, 982–988. [Google Scholar] [CrossRef]
- Kolbinger, F.R.; Leger, S.; Carstens, M.; Rinner, F.M.; Krell, S.; Chernykh, A.; Nielen, T.P.; Bodenstedt, S.; Welsch, T.; Kirchberg, J. Artificial Intelligence for Context-Aware Surgical Guidance in Complex Robot-Assisted Oncological Procedures: An Exploratory Feasibility Study. medRxiv 2022. [Google Scholar] [CrossRef]
- Igaki, T.; Kitaguchi, D.; Kojima, S.; Hasegawa, H.; Takeshita, N.; Mori, K.; Kinugasa, Y.; Ito, M. Artificial Intelligence-Based Total Mesorectal Excision Plane Navigation in Laparoscopic Colorectal Surgery. Dis. Colon Rectum 2022, 65, e329–e333. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, J.; Ota, M.; Suwa, Y.; Suzuki, S.; Suwa, H.; Momiyama, M.; Ishibe, A.; Watanabe, K.; Masui, H.; Nagahori, K.; et al. Evaluation of the Intestinal Blood Flow near the Rectosigmoid Junction Using the Indocyanine Green Fluorescence Method in a Colorectal Cancer Surgery. Int. J. Colorectal Dis. 2015, 30, 329–335. [Google Scholar] [CrossRef]
- Quero, G.; Lapergola, A.; Barberio, M.; Seeliger, B.; Saccomandi, P.; Guerriero, L.; Mutter, D.; Saadi, A.; Worreth, M.; Marescaux, J.; et al. Discrimination between Arterial and Venous Bowel Ischemia by Computer-Assisted Analysis of the Fluorescent Signal. Surg. Endosc. 2019, 33, 1988–1997. [Google Scholar] [CrossRef]
- Song, W.; Tang, Z.; Zhang, D.; Burton, N.; Driessen, W.; Chen, X. Comprehensive Studies of Pharmacokinetics and Biodistribution of Indocyanine Green and Liposomal Indocyanine Green by Multispectral Optoacoustic Tomography. RSC Adv. 2015, 5, 3807–3813. [Google Scholar] [CrossRef]
- Alander, J.T.; Kaartinen, I.; Laakso, A.; Pätilä, T.; Spillmann, T.; Tuchin, V.V.; Venermo, M.; Välisuo, P. A Review of Indocyanine Green Fluorescent Imaging in Surgery. Int. J. Biomed. Imaging 2012, 2012, 940585. [Google Scholar] [CrossRef]
- Emile, S.H.; Khan, S.M.; Wexner, S.D. Impact of Change in the Surgical Plan Based on Indocyanine Green Fluorescence Angiography on the Rates of Colorectal Anastomotic Leak: A Systematic Review and Meta-Analysis. Surg. Endosc. 2022, 36, 2245–2257. [Google Scholar] [CrossRef]
- Mok, H.T.; Ong, Z.H.; Yaow, C.Y.L.; Ng, C.H.; Buan, B.J.L.; Wong, N.W.; Chong, C.S. Indocyanine Green Fluorescent Imaging on Anastomotic Leakage in Colectomies: A Network Meta-Analysis and Systematic Review. Int. J. Colorectal Dis. 2020, 35, 2365–2369. [Google Scholar] [CrossRef]
- Chan, D.K.H.; Lee, S.K.F.; Ang, J.J. Indocyanine Green Fluorescence Angiography Decreases the Risk of Colorectal Anastomotic Leakage: Systematic Review and Meta-Analysis. Surgery 2020, 168, 1128–1137. [Google Scholar] [CrossRef]
- Jafari, M.D.; Pigazzi, A.; McLemore, E.C.; Mutch, M.G.; Haas, E.; Rasheid, S.H.; Wait, A.D.; Paquette, I.M.; Bardakcioglu, O.; Safar, B.; et al. Perfusion Assessment in Left-Sided/Low Anterior Resection (PILLAR III): A Randomized, Controlled, Parallel, Multicenter Study Assessing Perfusion Outcomes with PINPOINT Near-Infrared Fluorescence Imaging in Low Anterior Resection. Dis. Colon Rectum 2021, 64, 995–1002. [Google Scholar] [CrossRef]
- De Nardi, P.; Elmore, U.; Maggi, G.; Maggiore, R.; Boni, L.; Cassinotti, E.; Fumagalli, U.; Gardani, M.; De Pascale, S.; Parise, P.; et al. Intraoperative Angiography with Indocyanine Green to Assess Anastomosis Perfusion in Patients Undergoing Laparoscopic Colorectal Resection: Results of a Multicenter Randomized Controlled Trial. Surg. Endosc. 2020, 34, 53–60. [Google Scholar] [CrossRef]
- Park, S.H.; Park, H.M.; Baek, K.R.; Ahn, H.M.; Lee, I.Y.; Son, G.M. Artificial Intelligence Based Real-Time Microcirculation Analysis System for Laparoscopic Colorectal Surgery. World J. Gastroenterol. 2020, 26, 6945–6962. [Google Scholar] [CrossRef]
- Miskovic, D.; Ni, M.; Wyles, S.M.; Parvaiz, A.; Hanna, G.B. Observational Clinical Human Reliability Analysis (OCHRA) for Competency Assessment in Laparoscopic Colorectal Surgery at the Specialist Level. Surg. Endosc. 2012, 26, 796–803. [Google Scholar] [CrossRef]
- Martin, J.A.; Regehr, G.; Reznick, R.; Macrae, H.; Murnaghan, J.; Hutchison, C.; Brown, M. Objective Structured Assessment of Technical Skill (OSATS) for Surgical Residents. Br. J. Surg. 1997, 84, 273–278. [Google Scholar] [CrossRef]
- Gofton, W.T.; Dudek, N.L.; Wood, T.J.; Balaa, F.; Hamstra, S.J. The Ottawa Surgical Competency Operating Room Evaluation (O-SCORE): A Tool to Assess Surgical Competence. Acad. Med. 2012, 87, 1401–1407. [Google Scholar] [CrossRef]
- Azari, D.P.; Frasier, L.L.; Quamme, S.R.P.; Greenberg, C.C.; Pugh, C.M.; Greenberg, J.A.; Radwin, R.G. Modeling Surgical Technical Skill Using Expert Assessment for Automated Computer Rating. Ann. Surg. 2019, 269, 574–581. [Google Scholar] [CrossRef]
- Kitaguchi, D.; Takeshita, N.; Matsuzaki, H.; Igaki, T.; Hasegawa, H.; Ito, M. Development and Validation of a 3-Dimensional Convolutional Neural Network for Automatic Surgical Skill Assessment Based on Spatiotemporal Video Analysis. JAMA Netw. Open 2021, 4, e2120786. [Google Scholar] [CrossRef]
- Hamamoto, R.; Suvarna, K.; Yamada, M.; Kobayashi, K.; Shinkai, N.; Miyake, M.; Takahashi, M.; Jinnai, S.; Shimoyama, R.; Sakai, A.; et al. Application of Artificial Intelligence Technology in Oncology: Towards the Establishment of Precision Medicine. Cancers 2020, 12, 3532. [Google Scholar] [CrossRef]
- Kennedy-Metz, L.R.; Mascagni, P.; Torralba, A.; Dias, R.D.; Perona, P.; Shah, J.A.; Padoy, N.; Zenati, M.A. Computer Vision in the Operating Room: Opportunities and Caveats. IEEE Trans. Med. Robot. Bionics 2021, 3, 2–10. [Google Scholar] [CrossRef]
- Ward, T.M.; Mascagni, P.; Madani, A.; Padoy, N.; Perretta, S.; Hashimoto, D.A. Surgical Data Science and Artificial Intelligence for Surgical Education. J. Surg. Oncol. 2021, 124, 221–230. [Google Scholar] [CrossRef]
- Maier-Hein, L.; Eisenmann, M.; Sarikaya, D.; März, K.; Collins, T.; Malpani, A.; Fallert, J.; Feussner, H.; Giannarou, S.; Mascagni, P.; et al. Surgical Data Science—From Concepts toward Clinical Translation. Med. Image Anal. 2022, 76, 102306. [Google Scholar] [CrossRef]
- Nazarian, S.; Glover, B.; Ashrafian, H.; Darzi, A.; Teare, J. Diagnostic Accuracy of Artificial Intelligence and Computer-Aided Diagnosis for the Detection and Characterization of Colorectal Polyps: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2021, 23, e27370. [Google Scholar] [CrossRef]
- Ding, L.; Liu, G.W.; Zhao, B.C.; Zhou, Y.P.; Li, S.; Zhang, Z.D.; Guo, Y.T.; Li, A.Q.; Lu, Y.; Yao, H.W.; et al. Artificial Intelligence System of Faster Region-Based Convolutional Neural Network Surpassing Senior Radiologists in Evaluation of Metastatic Lymph Nodes of Rectal Cancer. Chin. Med. J. 2019, 132, 379–387. [Google Scholar] [CrossRef]
- Lu, Y.; Yu, Q.; Gao, Y.; Zhou, Y.; Liu, G.; Dong, Q.; Ma, J.; Ding, L.; Yao, H.; Zhang, Z.; et al. Identification of Metastatic Lymph Nodes in MR Imaging with Faster Region-Based Convolutional Neural Networks. Cancer Res. 2018, 78, 5135–5143. [Google Scholar] [CrossRef]
- Li, Y.; Eresen, A.; Shangguan, J.; Yang, J.; Lu, Y.; Chen, D.; Wang, J.; Velichko, Y.; Yaghmai, V.; Zhang, Z. Establishment of a New Non-Invasive Imaging Prediction Model for Liver Metastasis in Colon Cancer. Am. J. Cancer Res. 2019, 9, 2482–2492. [Google Scholar]
- Rathore, S.; Hussain, M.; Aksam Iftikhar, M.; Jalil, A. Novel Structural Descriptors for Automated Colon Cancer Detection and Grading. Comput. Methods Programs Biomed. 2015, 121, 92–108. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Jia, Z.; Wang, L.B.; Ai, Y.; Zhang, F.; Lai, M.; Chang, E.I.C. Large Scale Tissue Histopathology Image Classification, Segmentation, and Visualization via Deep Convolutional Activation Features. BMC Bioinform. 2017, 18, 281. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, D.A.; Axelsson, C.G.; Jones, C.B.; Phitayakorn, R.; Petrusa, E.; McKinley, S.K.; Gee, D.; Pugh, C. Surgical Procedural Map Scoring for Decision-Making in Laparoscopic Cholecystectomy. Am. J. Surg. 2019, 217, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Curtis, N.J.; Dennison, G.; Brown, C.S.B.; Hewett, P.J.; Hanna, G.B.; Stevenson, A.R.L.; Francis, N.K. Clinical Evaluation of Intraoperative Near Misses in Laparoscopic Rectal Cancer Surgery. Ann. Surg. 2021, 273, 778–784. [Google Scholar] [CrossRef] [PubMed]
| Name | Year | Procedure (Data Type) | Online Links | Annotation | Size |
|---|---|---|---|---|---|
| EndoVis-Instrument | 2015 | Laparoscopic colorectal procedures * | https://endovissub-instrument.grand-challenge.org/Data/ Accessed on 22 July 2022 | Instrument segmentation, center coordinates, 2D pose | 270 images, 6 1-min long videos |
| EndoVis-Workflow | 2017 | Laparoscopic rectal resection, sigmoidectomy, proctocolectomy (videos, device signals) | https://endovissub2017-workflow.grand-challenge.org/Data/ Accessed on 19 July 2022 | Phases, instrument types | 30 full-length videos |
| EndoVis-ROBUST-MIS | 2019 | Laparoscopic rectal resection, sigmoidectomy, proctocolectomy (videos) | https://www.sciencedirect.com/science/article/pii/S136184152030284X Accessedon 23 July 2022 | Instrument types and segmentation | 10,040 images, 30 full-length videos |
| Heidelberg colorectal data | 2021 | Laparoscopic rectal resection, sigmoidectomy, proctocolectomy (videos, device signals) | https://www.nature.com/articles/s41597-021-00882-2 Accessed on 22 July 2022 | Phases, instrument types and segmentation | 10,040 images, 30 full-length videos |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Quero, G.; Mascagni, P.; Kolbinger, F.R.; Fiorillo, C.; De Sio, D.; Longo, F.; Schena, C.A.; Laterza, V.; Rosa, F.; Menghi, R.; et al. Artificial Intelligence in Colorectal Cancer Surgery: Present and Future Perspectives. Cancers 2022, 14, 3803. https://doi.org/10.3390/cancers14153803
Quero G, Mascagni P, Kolbinger FR, Fiorillo C, De Sio D, Longo F, Schena CA, Laterza V, Rosa F, Menghi R, et al. Artificial Intelligence in Colorectal Cancer Surgery: Present and Future Perspectives. Cancers. 2022; 14(15):3803. https://doi.org/10.3390/cancers14153803
Chicago/Turabian StyleQuero, Giuseppe, Pietro Mascagni, Fiona R. Kolbinger, Claudio Fiorillo, Davide De Sio, Fabio Longo, Carlo Alberto Schena, Vito Laterza, Fausto Rosa, Roberta Menghi, and et al. 2022. "Artificial Intelligence in Colorectal Cancer Surgery: Present and Future Perspectives" Cancers 14, no. 15: 3803. https://doi.org/10.3390/cancers14153803
APA StyleQuero, G., Mascagni, P., Kolbinger, F. R., Fiorillo, C., De Sio, D., Longo, F., Schena, C. A., Laterza, V., Rosa, F., Menghi, R., Papa, V., Tondolo, V., Cina, C., Distler, M., Weitz, J., Speidel, S., Padoy, N., & Alfieri, S. (2022). Artificial Intelligence in Colorectal Cancer Surgery: Present and Future Perspectives. Cancers, 14(15), 3803. https://doi.org/10.3390/cancers14153803






