Stepping Stones to Sustainability Within Cancer Clinical Trials in Ireland
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Survey Design
2.3. Participants and Recruitment
2.4. Data Collection Process
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Demographics
3.2. Awareness and Knowledge of Carbon Footprint Tools
3.3. Perceived Contributors to Trial Emissions
3.4. Training, Confidence, and Willingness to Implement Sustainable Practices
3.5. Perceptions of Innovative Measures to Reduce Carbon Footprint
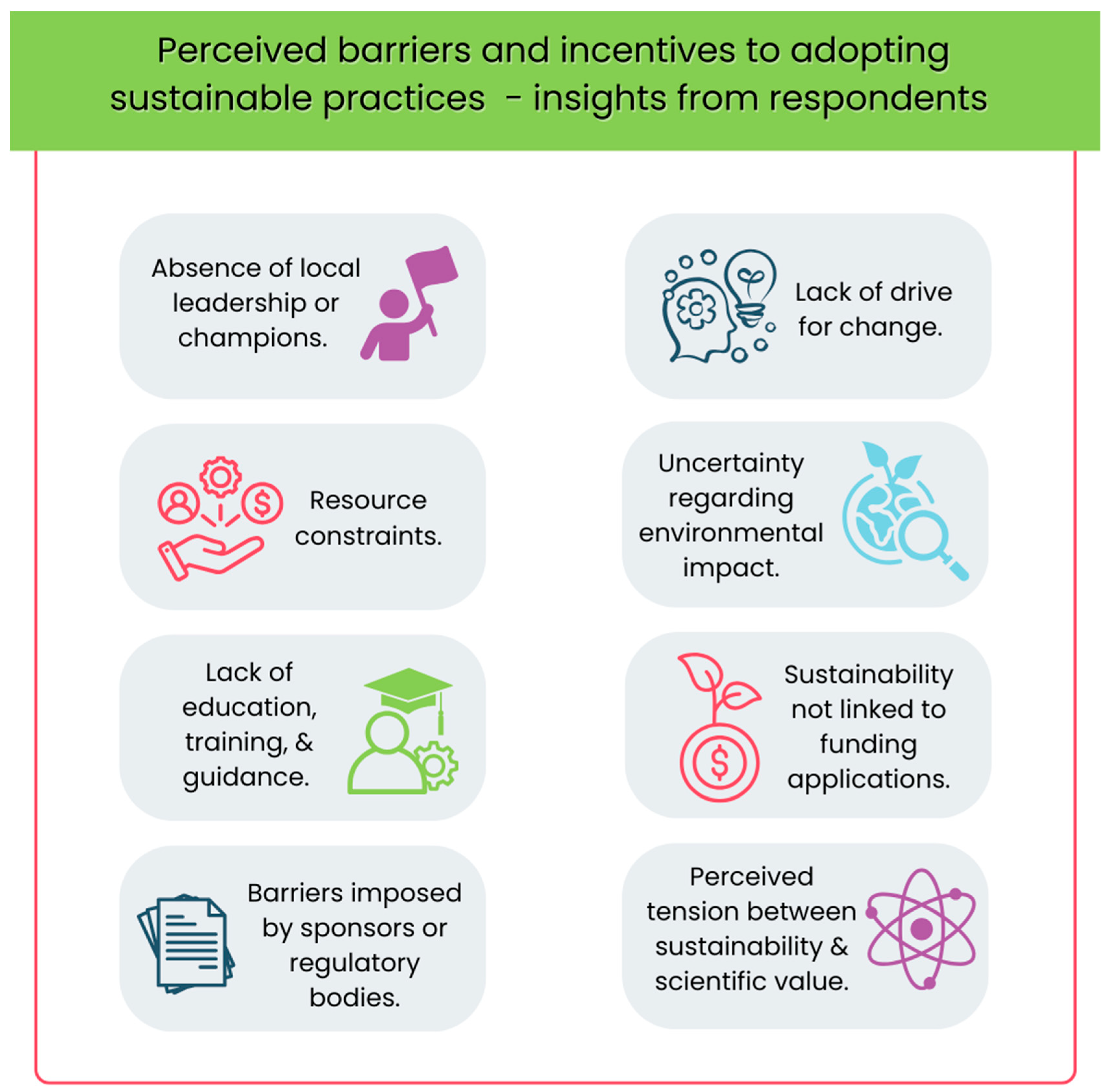
3.6. Barriers and Incentives to Sustainable Practice in Cancer Clinical Trials
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Intergovernmental Panel on Climate Change (IPCC). Climate Change 2023: Synthesis Report. Summary for Policymakers. 2023. Available online: https://www.ipcc.ch/report/ar6/syr/ (accessed on 10 May 2025).
- World Health Organization (WHO). Making the Case for Global Health in Climate Action 2021. Available online: https://who.foundation/latest-updates/making-the-case-for-global-health-in-climate-action/ (accessed on 10 May 2025).
- Health Care Without Harm. Health Care’s Climate Footprint: How The Health Sector Contributes To The Global Climate Crisis And Opportunities For Action. 2019. Available online: https://global.noharm.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (accessed on 10 May 2025).
- Romanello, M.; di Napoli, C.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Walawender, M.; Ali, Z.; Ameli, N.; Ayeb-Karlsson, S.; et al. The 2023 report of the Lancet Countdown on health and climate change: The imperative for a health-centred response in a world facing irreversible harms. Lancet 2023, 402, 2346–2394. [Google Scholar] [CrossRef]
- World Resources Institute, World Business Council for Sustainable Development. Greenhouse Gas Protocol 2022. Available online: https://ghgprotocol.org (accessed on 14 May 2025).
- Pak, L.M.; Morrow, M. Addressing the problem of overtreatment in breast cancer. Expert Rev. Anticancer. Ther. 2022, 22, 535–548. [Google Scholar] [CrossRef] [PubMed]
- Zikhathile, T.; Atagana, H.; Bwapwa, J.; Sawtell, D. A Review of the Impact that Healthcare Risk Waste Treatment Technologies Have on the Environment. Int. J. Environ. Res. Public Health 2022, 19, 11967. [Google Scholar] [CrossRef] [PubMed]
- Chuter, R.; Stanford-Edwards, C.; Cummings, J.; Taylor, C.; Lowe, G.; Holden, E.; Razak, R.; Glassborow, E.; Herbert, S.; Reggian, G.; et al. Towards estimating the carbon footprint of external beam radiotherapy. Phys. Med. 2023, 112, 102652. [Google Scholar] [CrossRef]
- Crowley, E.; Treweek, S.; Banister, K.; Breeman, S.; Constable, L.; Cotton, S.; Duncan, A.; El Feky, A.; Gardner, H.; Goodman, K.; et al. Using systematic data categorisation to quantify the types of data collected in clinical trials: The DataCat project. Trials 2020, 21, 535. [Google Scholar] [CrossRef]
- Academy of Medical Sciences. Enabling Greener Biomedical Research 2023. Available online: https://acmedsci.ac.uk/file-download/61695123 (accessed on 17 May 2025).
- Sustainable Trials Study Group Towards sustainable clinical trials. BMJ 2007, 334, 671–673. [CrossRef]
- Griffiths, J.; Fox, L.; Williamson, P.R.; Low Carbon Clinical Trials, G. Quantifying the carbon footprint of clinical trials: Guidance development and case studies. BMJ Open 2024, 14, e075755. [Google Scholar] [CrossRef]
- Hoffmann, J.M.; Bauer, A.; Grossmann, R. The carbon footprint of clinical trials: A global survey on the status quo and current regulatory guidance. BMJ Glob. Health 2023, 8, e012754. [Google Scholar] [CrossRef] [PubMed]
- Gervais, C. Health Care Workers’ Views of Health Care’s Contribution to Greenhouse Gas Emissions and Reducing Health Care Emissions. WMJ 2025, 124, 22–26. [Google Scholar]
- Elke Lister, H.; Mostert, K.; Botha, T.; Field, E.; Knock, D.; Mubi, N.; Odendaal, S.; Rohde, M.; Maric, F. Development and validation of a Knowledge, Attitudes and Practices (KAP) questionnaire for healthcare professionals on environmental sustainability in healthcare in Southern Africa. F1000Research 2025, 13, 1308. [Google Scholar] [CrossRef]
- Attia, N.M.; Hamed, A.E.M.; Elhafeez Elbarky, M.A.A.; Barakat, A.M.; Mohamed, H.S. Navigating sustainable practice: Environmental awareness and climate change as mediators of green competence of nurses. BMC Nurs. 2025, 24, 658. [Google Scholar] [CrossRef]
- Environmental Protection Agency. National Climate Change Risk Assessment: Summary for Policymakers. 2025. Available online: https://www.epa.ie/publications/monitoring--assessment/climate-change/national-climate-change-risk-assessment-summary-for-policymakers.php (accessed on 24 May 2025).
- Irish Pharmaceutical Healthcare Association (IPHA). Pharmaceutical Preparations Manufacturing in Ireland—Industry Market Research Report 2025. Available online: https://www.globenewswire.com/news-release/2024/11/11/2978464/28124/en/Ireland-Pharmaceutical-Preparations-Manufacturing-Market-Research-Report-2024-2029-A-Backlog-of-Healthcare-Appointments-has-Aided-Demand-for-Pharmaceutical-Products.html?utm_source=chatgpt.com (accessed on 24 May 2025).
- Enterprise Ireland. Pharma: Innovating to Enhance Patient Outcomes and Deliver a Sustainable Future 2025. Available online: https://www.enterprise-ireland.com/en/global/pharma?utm_source=chatgpt.com. (accessed on 24 May 2025).
- My Oo, N.; Weadick, C.S.; Murphy, L.; O’Reilly, S. Climate change advocacy and cancer clinical trial organisations. BJC Rep. 2024, 2, 49. [Google Scholar] [CrossRef]
- National Institute for Health and Care Research. NIHR Carbon Reduction Guidelines 2019. Available online: https://www.nihr.ac.uk/about-us/what-we-do/key-initiatives/climate-health-sustainability/carbon-reduction-guidelines (accessed on 28 May 2025).
- My Green Lab. My Green Lab Certification 2024. Available online: https://www.mygreenlab.org/green-lab-certification.html (accessed on 10 May 2025).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Braithwaite, J.; Pichumani, A.; Crowley, P. Tackling climate change: The pivotal role of clinicians. BMJ 2023, 382, e076963. [Google Scholar] [CrossRef]
- Aronsson, J.; Elf, M.; Warwick, P.; LoMartire, R.; Anaker, A. The relevance of climate change and sustainability in nursing education: A cross-sectional study of students’ perspectives. BMC Nurs. 2025, 24, 834. [Google Scholar] [CrossRef] [PubMed]
- Tiitta, I.; Kopra, J.; McDermott-Levy, R.; Jaakkola, J.J.K.; Kuosmanen, L. Climate change perceptions among nursing students: A comparative study between Finland and the United States. Nurse Educ. Today 2025, 146, 106541. [Google Scholar] [CrossRef]
- Sandal, S.; Onu, U.; Fung, W.; Pippias, M.; Smyth, B.; De Chiara, L.; Bajpai, D.; Bilchut, W.H.; Hafiz, E.; Kelly, D.M.; et al. Assessing the role of education level on climate change belief, concern and action: A multinational survey of healthcare professionals in nephrology. J. Nephrol. 2025, 38, 925–934. [Google Scholar] [CrossRef]
- Wen, S.; Chen, H.; Su, J. Engaging health professionals in climate change: A cross-national study of psychological distance across 12 countries. BMC Public Health 2025, 25, 1455. [Google Scholar] [CrossRef] [PubMed]
- Kish-Doto, J.; Roberts Francavillo, G. Public health professionals’ views on climate change, advocacy, and health. J. Commun. Healthc. 2025, 18, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Caraballo-Betancort, A.M.; Marcilla-Toribio, I.; Notario-Pacheco, B.; Cekrezi, S.; Perez-Moreno, A.; Martinez-Andres, M. Health professionals’ perceptions of climate change: A systematic review of qualitative studies. Public Health 2025, 245, 105773. [Google Scholar] [CrossRef]
- Dablander, F.; Sachisthal, M.S.M.; Haslbeck, J.M.B. Climate actions by climate and non-climate researchers. npj Clim. Action 2024, 3, 105. [Google Scholar] [CrossRef]
- Cologna, V.; Meiler, S.; Kropf, C.M.; Lüthi, S.; Mede, N.G.; Bresch, D.N.; Lecuona, O.; Berger, S.; Besley, J.; Brick, C.; et al. Extreme weather event attribution predicts climate policy support across the world. Nat. Clim. Chang. 2025, 15, 725–735. [Google Scholar] [CrossRef]
- Carlberg, C.; Jansonn, C. ‘Barriers to Eco-Innovation—A Qualitative Study on Large Manufacturing Companies’. Master’s Thesis, Uppsala University, Uppsala, Sweden, 2019. Available online: https://www.diva-portal.org/smash/get/diva2:1333528/FULLTEXT01.pdf (accessed on 3 June 2025).
- Huang, Y.-F.; Chen, A.P.-S.; Do, M.-H.; Chung, J.-C. Assessing the Barriers of Green Innovation Implementation: Evidence from the Vietnamese Manufacturing Sector. Sustainability 2022, 14, 4662. [Google Scholar] [CrossRef]
- Elia, M.R.; Toygar, I.; Tomlins, E.; Bagcivan, G.; Parsa, S.; Ginex, P.K. Climate change, climate disasters and oncology care: A descriptive global survey of oncology healthcare professionals. Support. Care Cancer 2024, 32, 764. [Google Scholar] [CrossRef]
- Rosa, C.; Marsch, L.A.; Winstanley, E.L.; Brunner, M.; Campbell, A.N.C. Using digital technologies in clinical trials: Current and future applications. Contemp. Clin. Trials 2021, 100, 106219. [Google Scholar] [CrossRef] [PubMed]
- Sustainable Healthcare Coalition. Clinical Trials: Carbon Footprint Assessment Guidance. Available online: https://shcoalition.org/clinical-trials-carbon-footprint-assessment-guidance-guidance-document/ (accessed on 8 June 2025).
- O’REilly, S.; Griffiths, J.; Fox, L.; Weadick, C.S.; Oo, N.M.; Murphy, L.; O’LEary, R.; Goulioti, T.; Adam, V.; Razis, E.D.; et al. Climate change impacts and sustainability integration among breast international group members. Breast 2025, 81, 104469. [Google Scholar] [CrossRef] [PubMed]
- Mackillop, N.; Shah, J.; Collins, M.; Costelloe, T.; Ohman, D. Carbon footprint of industry-sponsored late-stage clinical trials. BMJ Open 2023, 13, e072491. [Google Scholar] [CrossRef] [PubMed]
- A Ioannidis, J.P.; Greenland, S.; A Hlatky, M.; Khoury, M.J.; Macleod, M.R.; Moher, D.; Schulz, K.F.; Tibshirani, R. Increasing value and reducing waste in research design, conduct, and analysis. Lancet 2014, 383, 166–175. [Google Scholar] [CrossRef]
- Subaiya, S.; Hogg, E.; Roberts, I. Reducing the environmental impact of trials: A comparison of the carbon footprint of the CRASH-1 and CRASH-2 clinical trials. Trials 2011, 12, 31. [Google Scholar] [CrossRef]
- Coombs, N.J.; Coombs, J.M.; Vaidya, U.J.; Singer, J.; Bulsara, M.; Tobias, J.S.; Wenz, F.; Joseph, D.J.; A Brown, D.; Rainsbury, R.; et al. Environmental and social benefits of the targeted intraoperative radiotherapy for breast cancer: Data from UK TARGIT-A trial centres and two UK NHS hospitals offering TARGIT IORT. BMJ Open 2016, 6, e010703. [Google Scholar] [CrossRef]
- National Health Service. Delivering a “Net Zero” National Health Service 2020. Available online: https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2022/07/B1728-delivering-a-net-zero-nhs-july-2022.pdf (accessed on 15 June 2025).
- Tufts-Center for the Study of Drug Development. Rising protocol design complexity is driving rapid growth in clinical trial data volume. Impact Rep. Jan/Feb. 2021, 23, 1–4. [Google Scholar]
- Kelly, F.J. How can we reduce biomedical research’s carbon footprint? PLoS Biol. 2023, 21, e3002363. [Google Scholar] [CrossRef] [PubMed]
- Adshead, F.; Al-Shahi Salman, R.; Aumonier, S.; Collins, M.; Hood, K.; McNamara, C.; Moorea, K.; Smith, R.; Sydesg, M.R.; Williamson, P.R. A strategy to reduce the carbon footprint of clinical trials. Lancet 2021, 398, 281–282. [Google Scholar] [CrossRef] [PubMed]
| Question Number | Question Asked |
|---|---|
| 1. | What is your main specialty or role within CTI? |
| 2. | What is your current role in cancer research? |
| 3. | Have you ever held the role of National Lead or Chief Investigator? |
| 4. | In which province do you currently work? |
| 5. | What is your current affiliation as a CTI stakeholder? |
| 6. | Are you aware of any approaches or tools for calculating the carbon footprint of clinical trials (e.g., SCTG guidelines, NIHR calculator, My Green Lab certification)? |
| 7. | To what extent do you believe that industry-sponsored trials consider carbon footprint during design? |
| 8. | To what extent do you believe that academic trials consider carbon footprint during design? |
| 9. | Please rank the following trial-related activities based on their perceived impact on a trial’s carbon footprint. |
| 10. | Have you received any formal education or training on reducing the carbon footprint of clinical trials? |
| 11. | How confident do you feel in your ability to advise on or implement sustainability measures in clinical trials? |
| 12. | Would you be willing to participate in sustainability initiatives within clinical trials? |
| 13. | Which of the following innovative measures do you think would have the greatest impact on reducing carbon emissions in trials? |
| 14. | Do you have any additional practical suggestions for reducing a trial’s carbon footprint? |
| 15. | Have you observed or been involved in any changes that have reduced the carbon footprint of a clinical trial? |
| 16. | What do you think are the three main barriers to adopting sustainability measures in cancer clinical trials? |
| 17. | Have you personally encountered any of the barriers you identified above? Please describe. |
| 18. | What would have helped to overcome those barriers? |
| 19. | What do you believe are the three best incentives for encouraging sustainability in clinical trials? |
| 20. | Do you have any suggestions for accelerating the introduction of sustainable practices in cancer clinical trials? |
| 21. | Do you have any suggestions for promoting or informing change regarding sustainability in cancer research? |
| Specialty/Role | Number Currently Working in the Cancer Clinical Trials Community | Number Who Participated in the Survey | Representation |
|---|---|---|---|
| Consultant Medical Oncologist | 83 | 31 | 37% |
| Consultant Radiation Oncologist | 51 | 14 | 27% |
| Consultant Surgeon | 53 | 4 | 8% |
| Admin | figures not up to date | 13 | n/a |
| Data Manager/Bio Statistician | 39 | 11 | 28% |
| Hematologist | 54 | 9 | 17% |
| Translational Scientist | 19 | 9 | 47% |
| Research Specialist | 199 | 8 | 4% |
| Patient Consultant Committee member | 13 | 4 | 31% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Clayton-Lea, A.; Flynn, C.R.; Hopkins, C.; O’Reilly, S. Stepping Stones to Sustainability Within Cancer Clinical Trials in Ireland. Curr. Oncol. 2025, 32, 446. https://doi.org/10.3390/curroncol32080446
Clayton-Lea A, Flynn CR, Hopkins C, O’Reilly S. Stepping Stones to Sustainability Within Cancer Clinical Trials in Ireland. Current Oncology. 2025; 32(8):446. https://doi.org/10.3390/curroncol32080446
Chicago/Turabian StyleClayton-Lea, Angela, Calvin R. Flynn, Claire Hopkins, and Seamus O’Reilly. 2025. "Stepping Stones to Sustainability Within Cancer Clinical Trials in Ireland" Current Oncology 32, no. 8: 446. https://doi.org/10.3390/curroncol32080446
APA StyleClayton-Lea, A., Flynn, C. R., Hopkins, C., & O’Reilly, S. (2025). Stepping Stones to Sustainability Within Cancer Clinical Trials in Ireland. Current Oncology, 32(8), 446. https://doi.org/10.3390/curroncol32080446






