Risk of Cardiovascular Events and Lipid Profile Change in Patients with Breast Cancer Taking Aromatase Inhibitor: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
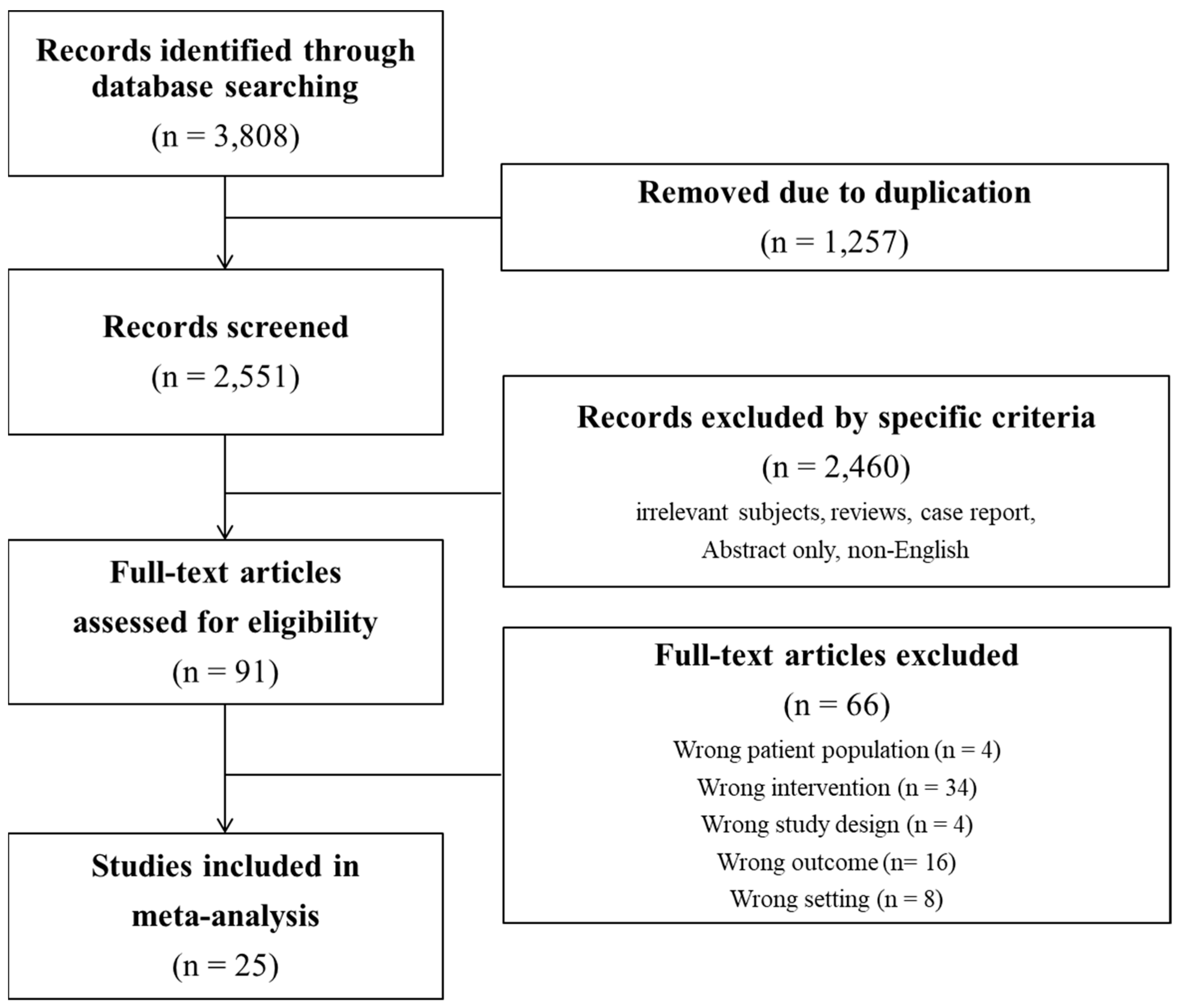
2. Materials and Methods
2.1. Inclusion Criteria, Exclusion Criteria, and Study Outcomes
2.2. Search Strategy
2.3. Study Selection and Data Extraction
2.4. Methodological Quality and Risk of Bias Assessment
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Included Studies
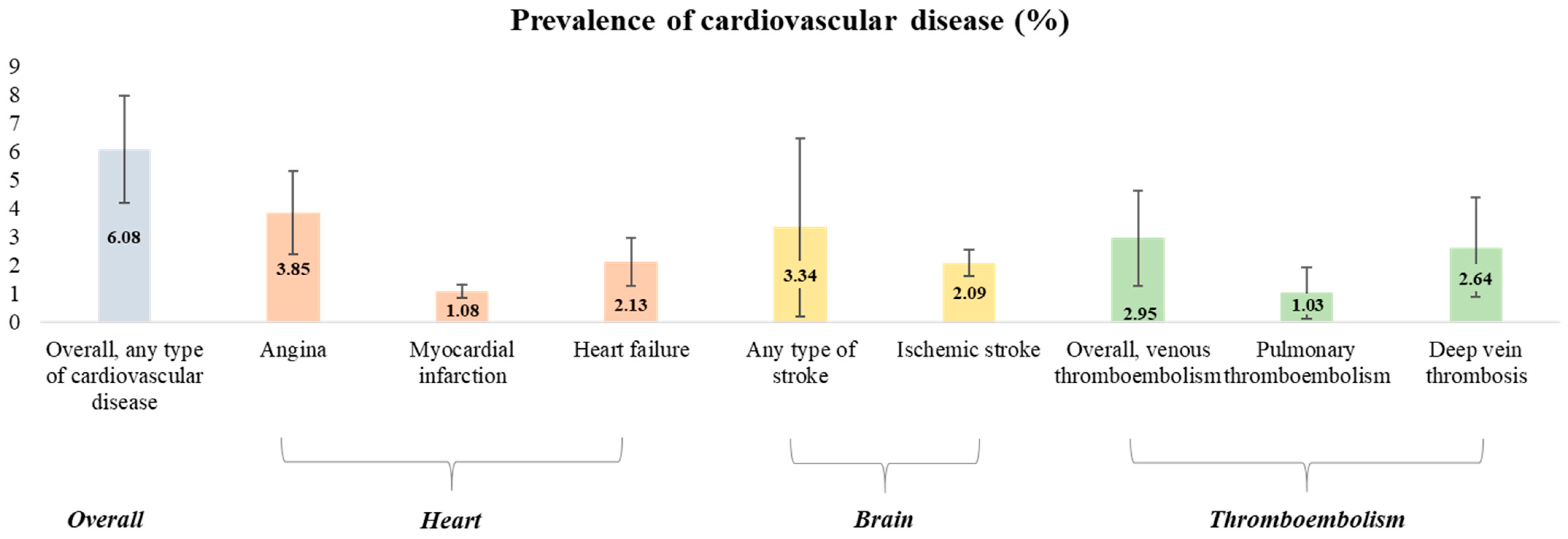
3.2. AI Use and the Prevalence of Various Cardiovascular Outcomes
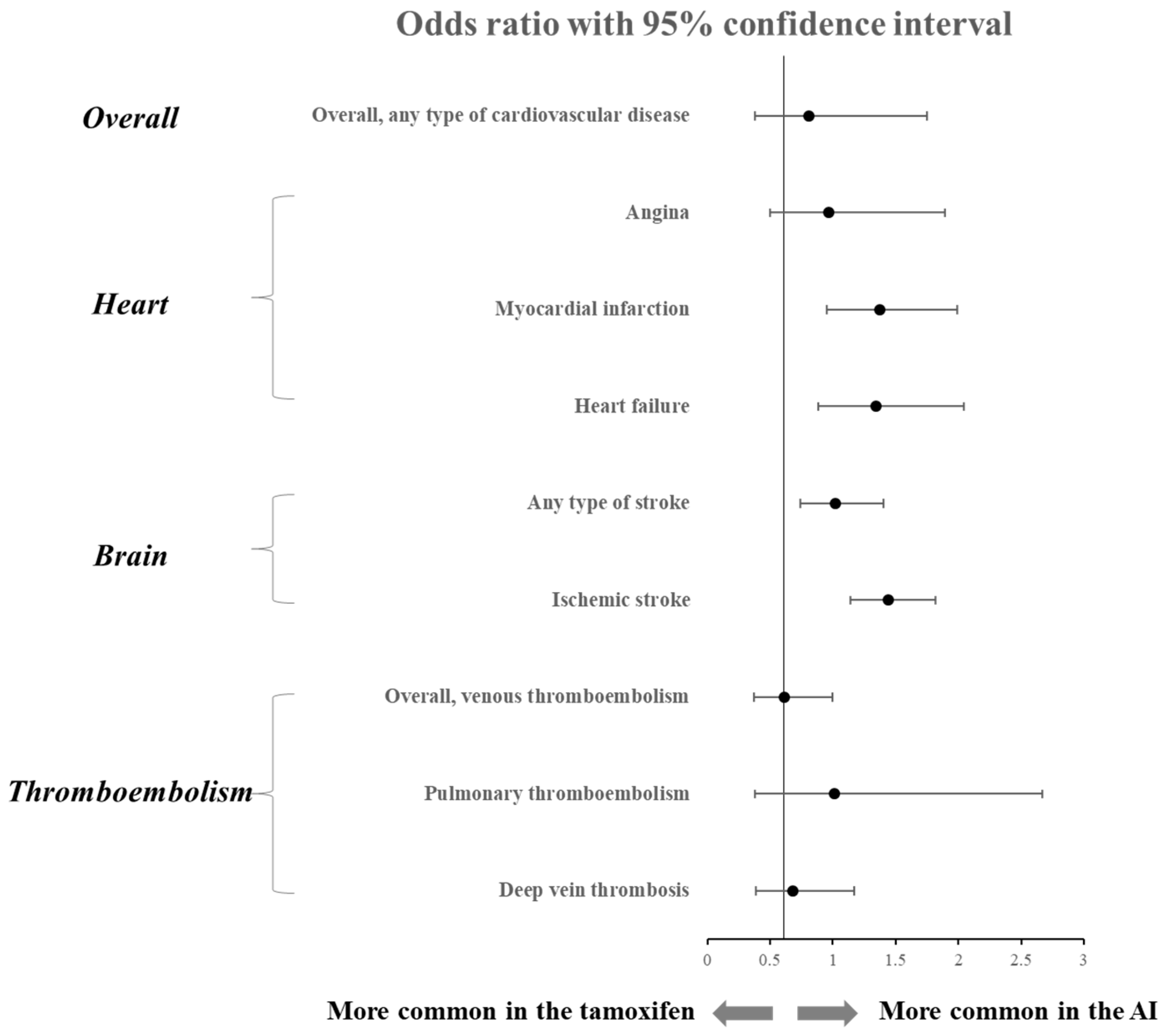
3.3. Comparison of Various Cardiovascular Outcomes between AI and Tamoxifen
3.4. Change in Lipid Profile during AI Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Huang, J.; Chan, P.S.; Lok, V.; Chen, X.; Ding, H.; Jin, Y.; Yuan, J.; Lao, X.Q.; Zheng, Z.J.; Wong, M.C. Global incidence and mortality of breast cancer: A trend analysis. Aging 2021, 13, 5748–5803. [Google Scholar] [CrossRef]
- Lei, S.; Zheng, R.; Zhang, S.; Wang, S.; Chen, R.; Sun, K.; Zeng, H.; Zhou, J.; Wei, W. Global patterns of breast cancer incidence and mortality: A population-based cancer registry data analysis from 2000 to 2020. Cancer Commun. 2021, 41, 1183–1194. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Hendrick, R.E.; Helvie, M.A.; Monticciolo, D.L. Breast Cancer Mortality Rates Have Stopped Declining in U.S. Women Younger than 40 Years. Radiology 2021, 299, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Mehta, L.S.; Watson, K.E.; Barac, A.; Beckie, T.M.; Bittner, V.; Cruz-Flores, S.; Dent, S.; Kondapalli, L.; Ky, B.; Okwuosa, T.; et al. Cardiovascular Disease and Breast Cancer: Where These Entities Intersect: A Scientific Statement From the American Heart Association. Circulation 2018, 137, e30–e66. [Google Scholar] [CrossRef] [PubMed]
- Patnaik, J.L.; Byers, T.; DiGuiseppi, C.; Dabelea, D.; Denberg, T.D. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: A retrospective cohort study. Breast Cancer Res. 2011, 13, R64. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative, G. Aromatase inhibitors versus tamoxifen in premenopausal women with oestrogen receptor-positive early-stage breast cancer treated with ovarian suppression: A patient-level meta-analysis of 7030 women from four randomised trials. Lancet Oncol. 2022, 23, 382–392. [Google Scholar] [CrossRef]
- Khosrow-Khavar, F.; Filion, K.B.; Bouganim, N.; Suissa, S.; Azoulay, L. Aromatase Inhibitors and the Risk of Cardiovascular Outcomes in Women With Breast Cancer: A Population-Based Cohort Study. Circulation 2020, 141, 549–559. [Google Scholar] [CrossRef]
- Khosrow-Khavar, F.; Bouganim, N.; Filion, K.B.; Suissa, S.; Azoulay, L. Cardiotoxicity of Use of Sequential Aromatase Inhibitors in Women With Breast Cancer. Am. J. Epidemiol. 2020, 189, 1086–1095. [Google Scholar] [CrossRef]
- Sund, M.; Garcia-Argibay, M.; Garmo, H.; Ahlgren, J.; Wennstig, A.K.; Fredriksson, I.; Lindman, H.; Valachis, A. Aromatase inhibitors use and risk for cardiovascular disease in breast cancer patients: A population-based cohort study. Breast 2021, 59, 157–164. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A.; et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Park, J.E.; Lee, Y.J.; Seo, H.J.; Sheen, S.S.; Hahn, S.; Jang, B.H.; Son, H.J. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J. Clin. Epidemiol. 2013, 66, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Sawada, S.; Sato, K.; Kusuhara, M.; Ayaori, M.; Yonemura, A.; Tamaki, K.; Hiraide, H.; Mochizuki, H.; Ohsuzu, F. Effect of anastrozole and tamoxifen on lipid metabolism in Japanese postmenopausal women with early breast cancer. Acta Oncol. 2005, 44, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Lonning, P.E.; Geisler, J.; Krag, L.E.; Erikstein, B.; Bremnes, Y.; Hagen, A.I.; Schlichting, E.; Lien, E.A.; Ofjord, E.S.; Paolini, J.; et al. Effects of exemestane administered for 2 years versus placebo on bone mineral density, bone biomarkers, and plasma lipids in patients with surgically resected early breast cancer. J. Clin. Oncol. 2005, 23, 5126–5137. [Google Scholar] [CrossRef]
- Atalay, G.; Dirix, L.; Biganzoli, L.; Beex, L.; Nooij, M.; Cameron, D.; Lohrisch, C.; Cufer, T.; Lobelle, J.P.; Mattiaci, M.R.; et al. The effect of exemestane on serum lipid profile in postmenopausal women with metastatic breast cancer: A companion study to EORTC Trial 10951, ‘Randomized phase II study in first line hormonal treatment for metastatic breast cancer with exemestane or tamoxifen in postmenopausal patients’. Ann. Oncol. 2004, 15, 211–217. [Google Scholar] [CrossRef]
- Wojtacki, J.; Kraszewski, W.; Leśniewski-Kmak, K.; Śliwińska, M.; Czyżewska, K.; Kruszewska, E.; Rachoń, D. Short-term effects of anastrozole therapy on serum lipid profile in patients with breast cancer, previously treated with tamoxifen. Preliminary report. Nowotwory. J. Oncol. 2001, 51, 43. [Google Scholar]
- Markopoulos, C.; Dafni, U.; Misitzis, J.; Zobolas, V.; Tzoracoleftherakis, E.; Koukouras, D.; Xepapadakis, G.; Papadiamantis, J.; Venizelos, B.; Antonopoulou, Z.; et al. Extended adjuvant hormonal therapy with exemestane has no detrimental effect on the lipid profile of postmenopausal breast cancer patients: Final results of the ATENA lipid substudy. Breast Cancer Res. 2009, 11, R35. [Google Scholar] [CrossRef]
- Tian, W.; Wu, M.; Deng, Y. Comparison of Changes in the Lipid Profiles of Eastern Chinese Postmenopausal Women with Early-Stage Breast Cancer Treated with Different Aromatase Inhibitors: A Retrospective Study. Clin. Pharmacol. Drug Dev. 2018, 7, 837–843. [Google Scholar] [CrossRef]
- Santa-Maria, C.A.; Blackford, A.; Nguyen, A.T.; Skaar, T.C.; Philips, S.; Oesterreich, S.; Rae, J.M.; Desta, Z.; Robarge, J.; Henry, N.L.; et al. Association of Variants in Candidate Genes with Lipid Profiles in Women with Early Breast Cancer on Adjuvant Aromatase Inhibitor Therapy. Clin. Cancer Res. 2016, 22, 1395–1402. [Google Scholar] [CrossRef]
- Abdel-Qadir, H.; Amir, E.; Fischer, H.D.; Fu, L.; Austin, P.C.; Harvey, P.J.; Rochon, P.A.; Lee, D.S.; Anderson, G.M. The risk of myocardial infarction with aromatase inhibitors relative to tamoxifen in post-menopausal women with early stage breast cancer. Eur. J. Cancer 2016, 68, 11–21. [Google Scholar] [CrossRef]
- Pineda-Moncusi, M.; Garcia-Giralt, N.; Diez-Perez, A.; Tusquets, I.; Servitja, S.; Albanell, J.; Prieto-Alhambra, D.; Nogues, X. Thromboembolic, cardiovascular and overall mortality risks of aromatase inhibitors, compared with tamoxifen treatment: An outpatient-register-based retrospective cohort study. Ther. Adv. Med. Oncol. 2020, 12, 1758835920909660. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chlebowski, R.T.; Shi, J.; Barac, A.; Haque, R. Aromatase inhibitor and tamoxifen use and the risk of venous thromboembolism in breast cancer survivors. Breast Cancer Res. Treat. 2019, 174, 785–794. [Google Scholar] [CrossRef]
- Markopoulos, C.; Polychronis, A.; Zobolas, V.; Xepapadakis, G.; Papadiamantis, J.; Koukouras, D.; Lappas, H.; Gogas, H. The effect of exemestane on the lipidemic profile of postmenopausal early breast cancer patients: Preliminary results of the TEAM Greek sub-study. Breast Cancer Res. Treat. 2005, 93, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Matthews, A.A.; Peacock Hinton, S.; Stanway, S.; Lyon, A.R.; Smeeth, L.; Lund, J.L.; Bhaskaran, K. Endocrine therapy use and cardiovascular risk in postmenopausal breast cancer survivors. Heart 2021, 107, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- Rabaglio, M.; Sun, Z.; Maibach, R.; Giobbie-Hurder, A.; Ejlertsen, B.; Harvey, V.J.; Neven, P.; Lang, I.; Bonnefoi, H.; Wardley, A.; et al. Cumulative incidence of cardiovascular events under tamoxifen and letrozole alone and in sequence: A report from the BIG 1-98 trial. Breast Cancer Res. Treat. 2021, 185, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Seruga, B.; Zadnik, V.; Kuhar, C.G.; Marinko, T.; Cufer, T.; Zakotnik, B.; Zorman, D.; Ocana, A.; Amir, E. Association of aromatase inhibitors with coronary heart disease in women with early breast cancer. Cancer Investig. 2014, 32, 99–104. [Google Scholar] [CrossRef]
- Kamaraju, S.; Shi, Y.; Smith, E.; Nattinger, A.B.; Laud, P.; Neuner, J. Are aromatase inhibitors associated with higher myocardial infarction risk in breast cancer patients? A Medicare population-based study. Clin. Cardiol. 2019, 42, 93–100. [Google Scholar] [CrossRef]
- Choi, S.H.; Kim, K.E.; Park, Y.; Ju, Y.W.; Jung, J.G.; Lee, E.S.; Lee, H.B.; Han, W.; Noh, D.Y.; Yoon, H.J.; et al. Effects of tamoxifen and aromatase inhibitors on the risk of acute coronary syndrome in elderly breast cancer patients: An analysis of nationwide data. Breast 2020, 54, 25–30. [Google Scholar] [CrossRef]
- Ligibel, J.A.; James O’Malley, A.; Fisher, M.; Daniel, G.W.; Winer, E.P.; Keating, N.L. Risk of myocardial infarction, stroke, and fracture in a cohort of community-based breast cancer patients. Breast Cancer Res. Treat. 2012, 131, 589–597. [Google Scholar] [CrossRef]
- Faiz, A.S.; Guo, S.; Kaveney, A.; Philipp, C.S. Risk of venous thromboembolism and endocrine therapy in older women with breast cancer in the United States. Blood Coagul. Fibrinolysis. 2021, 32, 373–381. [Google Scholar] [CrossRef]
- Franchi, M.; Tritto, R.; Tarantini, L.; Navazio, A.; Corrao, G. Adjuvant Hormonotherapy and Cardiovascular Risk in Post-Menopausal Women with Breast Cancer: A Large Population-Based Cohort Study. Cancers 2021, 13, 2254. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.T.; Chen, P.W.; Lin, H.W.; Kuo, Y.H.; Lin, S.H.; Li, Y.H. Risks of Aromatase Inhibitor-Related Cardiotoxicity in Patients with Breast Cancer in Asia. Cancers 2022, 14, 508. [Google Scholar] [CrossRef] [PubMed]
- Breast International Group 1-98 Collaborative, G.; Thurlimann, B.; Keshaviah, A.; Coates, A.S.; Mouridsen, H.; Mauriac, L.; Forbes, J.F.; Paridaens, R.; Castiglione-Gertsch, M.; Gelber, R.D.; et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N. Engl. J. Med. 2005, 353, 2747–2757. [Google Scholar] [CrossRef]
- Haque, R.; Shi, J.; Schottinger, J.E.; Chung, J.; Avila, C.; Amundsen, B.; Xu, X.; Barac, A.; Chlebowski, R.T. Cardiovascular Disease after Aromatase Inhibitor Use. JAMA Oncol. 2016, 2, 1590–1597. [Google Scholar] [CrossRef] [PubMed]
- Khosrow-Khavar, F.; Filion, K.B.; Al-Qurashi, S.; Torabi, N.; Bouganim, N.; Suissa, S.; Azoulay, L. Cardiotoxicity of aromatase inhibitors and tamoxifen in postmenopausal women with breast cancer: A systematic review and meta-analysis of randomized controlled trials. Ann. Oncol. 2017, 28, 487–496. [Google Scholar] [CrossRef] [PubMed]
- Yu, Q.; Xu, Y.; Yu, E.; Zheng, Z. Risk of cardiovascular disease in breast cancer patients receiving aromatase inhibitors vs. tamoxifen: A systematic review and meta-analysis. J. Clin. Pharm. Ther. 2022, 47, 575–587. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Zhang, J.; Shen, G.; Liu, L.; Zhao, Q.; Lu, X.; Yang, H.; Hong, D. Aromatase inhibitors and risk of cardiovascular events in breast cancer patients: A systematic review and meta-analysis. BMC Pharmacol. Toxicol 2019, 20, 62. [Google Scholar] [CrossRef]
- Hemingway, H.; Langenberg, C.; Damant, J.; Frost, C.; Pyorala, K.; Barrett-Connor, E. Prevalence of angina in women versus men: A systematic review and meta-analysis of international variations across 31 countries. Circulation 2008, 117, 1526–1536. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Alonso, A.; Beaton, A.Z.; Bittencourt, M.S.; Boehme, A.K.; Buxton, A.E.; Carson, A.P.; Commodore-Mensah, Y.; et al. Heart Disease and Stroke Statistics-2022 Update: A Report from the American Heart Association. Circulation 2022, 145, e153–e639. [Google Scholar] [CrossRef] [PubMed]
- Mehta, P.A.; Cowie, M.R. Gender and heart failure: A population perspective. Heart 2006, 92 (Suppl. 3), iii14–iii18. [Google Scholar] [CrossRef]
- North, B.J.; Sinclair, D.A. The intersection between aging and cardiovascular disease. Circ. Res. 2012, 110, 1097–1108. [Google Scholar] [CrossRef] [PubMed]
- Cuppone, F.; Bria, E.; Verma, S.; Pritchard, K.I.; Gandhi, S.; Carlini, P.; Milella, M.; Nisticò, C.; Terzoli, E.; Cognetti, F.; et al. Do adjuvant aromatase inhibitors increase the cardiovascular risk in postmenopausal women with early breast cancer? Meta-analysis of randomized trials. Cancer 2008, 112, 260–267. [Google Scholar] [CrossRef] [PubMed]
- Meier, C.R.; Jick, H. Tamoxifen and risk of idiopathic venous thromboembolism. Br. J. Clin. Pharmacol. 1998, 45, 608–612. [Google Scholar] [CrossRef] [PubMed]
- Decensi, A.; Maisonneuve, P.; Rotmensz, N.; Bettega, D.; Costa, A.; Sacchini, V.; Salvioni, A.; Travaglini, R.; Oliviero, P.; D’Aiuto, G.; et al. Effect of tamoxifen on venous thromboembolic events in a breast cancer prevention trial. Circulation 2005, 111, 650–656. [Google Scholar] [CrossRef]
- Hernandez, R.K.; Sorensen, H.T.; Pedersen, L.; Jacobsen, J.; Lash, T.L. Tamoxifen treatment and risk of deep venous thrombosis and pulmonary embolism: A Danish population-based cohort study. Cancer 2009, 115, 4442–4449. [Google Scholar] [CrossRef]
- Heit, J.A. Epidemiology of venous thromboembolism. Nat Rev Cardiol 2015, 12, 464–474. [Google Scholar] [CrossRef]
- White, R.H. The epidemiology of venous thromboembolism. Circulation 2003, 107, I4–I8. [Google Scholar] [CrossRef]
- Severino, P.; D’Amato, A.; Pucci, M.; Infusino, F.; Birtolo, L.I.; Mariani, M.V.; Lavalle, C.; Maestrini, V.; Mancone, M.; Fedele, F. Ischemic Heart Disease and Heart Failure: Role of Coronary Ion Channels. Int. J. Mol. Sci. 2020, 21, 3167. [Google Scholar] [CrossRef]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef]
- Perrone-Filardi, P.; Paolillo, S.; Costanzo, P.; Savarese, G.; Trimarco, B.; Bonow, R.O. The role of metabolic syndrome in heart failure. Eur. Heart J. 2015, 36, 2630–2634. [Google Scholar] [CrossRef]
- Monnier, A. Effects of adjuvant aromatase inhibitor therapy on lipid profiles. Expert Rev. Anticancer Ther. 2006, 6, 1653–1662. [Google Scholar] [CrossRef] [PubMed]
- Boccardo, F.; Rubagotti, A.; Puntoni, M.; Guglielmini, P.; Amoroso, D.; Fini, A.; Paladini, G.; Mesiti, M.; Romeo, D.; Rinaldini, M.; et al. Switching to anastrozole versus continued tamoxifen treatment of early breast cancer: Preliminary results of the Italian Tamoxifen Anastrozole Trial. J. Clin. Oncol. 2005, 23, 5138–5147. [Google Scholar] [CrossRef] [PubMed]
- Coombes, R.C.; Paridaens, R.; Jassem, J.; Van de Velde, C.J.; Delozier, T.; Jones, S.E.; Hall, E.; Kilburn, L.S.; Snowdon, C.F.; Bliss, J.M. First mature analysis of the Intergroup Exemestane Study. J. Clin. Oncol. 2006, 24, LBA527. [Google Scholar] [CrossRef]
- Elisaf, M.S.; Bairaktari, E.T.; Nicolaides, C.; Kakaidi, B.; Tzallas, C.S.; Katsaraki, A.; Pavlidis, N.A. Effect of letrozole on the lipid profile in postmenopausal women with breast cancer. Eur. J. Cancer 2001, 37, 1510–1513. [Google Scholar] [CrossRef] [PubMed]
- Zidan, J.; Chetver, L.; Hussein, O.; Zucker, M. Effect of letrozole on plasma lipids, triglycerides, and estradiol in postmenopausal women with metastatic breast cancer. Oncologist 2010, 15, 1159–1163. [Google Scholar] [CrossRef] [PubMed]
- Ruhstaller, T.; Giobbie-Hurder, A.; Colleoni, M.; Jensen, M.B.; Ejlertsen, B.; de Azambuja, E.; Neven, P.; Lang, I.; Jakobsen, E.H.; Gladieff, L.; et al. Adjuvant Letrozole and Tamoxifen Alone or Sequentially for Postmenopausal Women with Hormone Receptor-Positive Breast Cancer: Long-Term Follow-Up of the BIG 1-98 Trial. J. Clin. Oncol. 2019, 37, 105–114. [Google Scholar] [CrossRef]
- Cuzick, J.; Sestak, I.; Baum, M.; Buzdar, A.; Howell, A.; Dowsett, M.; Forbes, J.F.; investigators, A.L. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer: 10-year analysis of the ATAC trial. Lancet Oncol. 2010, 11, 1135–1141. [Google Scholar] [CrossRef]
- Dziewulska-Bokiniec, A.; Wojtacki, J.; Skokowski, J.; Kortas, B. The effect of tamoxifen treatment on serum cholesterol fractions in breast cancer women. Neoplasma 1994, 41, 13–16. [Google Scholar]
- Thangaraju, M.; Kumar, K.; Gandhirajan, R.; Sachdanandam, P. Effect of tamoxifen on plasma lipids and lipoproteins in postmenopausal women with breast cancer. Cancer 1994, 73, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Love, R.R.; Wiebe, D.A.; Feyzi, J.M.; Newcomb, P.A.; Chappell, R.J. Effects of tamoxifen on cardiovascular risk factors in postmenopausal women after 5 years of treatment. J. Natl. Cancer Inst. 1994, 86, 1534–1539. [Google Scholar] [CrossRef]
- Grey, A.B.; Stapleton, J.P.; Evans, M.C.; Reid, I.R. The effect of the anti-estrogen tamoxifen on cardiovascular risk factors in normal postmenopausal women. J. Clin. Endocrinol. Metab. 1995, 80, 3191–3195. [Google Scholar] [CrossRef] [PubMed]
- Decensi, A.; Bonanni, B.; Guerrieri-Gonzaga, A.; Gandini, S.; Robertson, C.; Johansson, H.; Travaglini, R.; Sandri, M.T.; Tessadrelli, A.; Farante, G.; et al. Biologic activity of tamoxifen at low doses in healthy women. J. Natl. Cancer Inst. 1998, 90, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Vrbanec, D.; Reiner, Z.; Belev, B.; Plestina, S. Changes in serum lipid and lipoprotein levels in postmenopausal patients with node-positive breast cancer treated with tamoxifen. Tumori 1998, 84, 687–690. [Google Scholar] [CrossRef] [PubMed]
- Cushman, M.; Costantino, J.P.; Tracy, R.P.; Song, K.; Buckley, L.; Roberts, J.D.; Krag, D.N. Tamoxifen and cardiac risk factors in healthy women: Suggestion of an anti-inflammatory effect. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 255–261. [Google Scholar] [CrossRef]
| Study | Study Type | Country | Cancer Stage | Age (Median) | Menopause | Treatment Duration | No. Group | Treatment | Control | No. Treatment | No. Control |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sawada 2005 [13] | Prospective RCT | Japan | early | 58.7 | postmenopausal | 12 wks | 2 | anastrozole | TAM | 22 | 22 |
| Lonning 2005 [14] | Prospective RCT | Norway | early | 60 | postmenopausal | 2 yrs | 2 | exemestane | placebo | 58 | 65 |
| Atalay 2004 [15] | Prospective RCT | Europe | non-metastatic | 64 | postmenopausal | 48 wks | 2 | exemestane | TAM | 36 | 36 |
| Khosrow-Khavar 2020 [8] | Retrospective cohort | UK | non-metastatic | 70.8 | postmenopausal | >1 year | 2 | AI | TAM | 8139 | 9783 |
| Wojtacki 2001 [16] | Retrospective cohort | Poland | non-metastatic | 61.6 | postmenopausal | 16.2 weeks | 1 | anastrozole | 44 | ||
| Markopoulos 2009 [17] | Prospective RCT | Greece | non-metastatic | 62.6 | postmenopausal | 5 years | 2 | exemestane | placebo | 211 | 200 |
| Tian 2018 [18] | Retrospective cohort | China | early breast cancer | 59.5 | postmenopausal | 2 years | 1 | letrozole | 38 | ||
| Santa-Maria 2016 [19] | Prospective cohort | USA | early breast cancer | 59 | postmenopausal | 3 months | 1 | AI | 422 | ||
| Abdel-Qadir 2016 [20] | Retrospective cohort | Canada | early breast cancer | 71 | postmenopausal | at least 1 year | 2 | AI | TAM | 7409 | 1941 |
| Pineda-Moncusi 2020 [21] | Retrospective cohort | UK, Spain | early breast cancer | 67 | postmenopausal | 29 months | 2 | AI | TAM | 18,455 | 3082 |
| Xu 2019 [22] | Prospective cohort | USA | non-metastatic | 65 | postmenopausal | 3.2 years | 2 | AI | TAM | 3837 | 4062 |
| Markopoulos 2005 [23] | Prospective RCT | Greece | early breast cancer | 65 | postmenopausal | 12 months | 2 | exemestane | TAM | 90 | 86 |
| Matthews 2021 [24] | Retrospective cohort | USA, UK | early breast cancer | 76 | postmenopausal | 2.2 years | 2 | AI | placebo | 15,074 | 4667 |
| Rabaglio 2021 [25] | Prospective RCT | Europe, USA | early breast cancer | NA | postmenopausal | 5 years | 2 | letrozole | TAM | 1535 | 1541 |
| Khosrow-Khavar 2020 [9] | Retrospective cohort | Canada | early breast cancer | 67.7 | postmenopausal | 5 years | 2 | AI | TAM | 1962 | 3874 |
| Seruga 2014 [26] | Retrospective cohort | Slovenia | early breast cancer | 69 | postmenopausal | NA | 2 | AI | TAM | 33 | 41 |
| Kamaraju 2019 [27] | Retrospective cohort | USA | early breast cancer | NA | postmenopausal | 12 months | 2 | AI | TAM | 4690 | 958 |
| Choi 2020 [28] | Retrospective cohort | Korea | all stage | 63.3 | postmenopausal | 3 years | 2 | AI | placebo | 19,584 | 18,807 |
| Ligibel 2012 [29] | Retrospective cohort | USA | all stage | 67 | NA | 30 months | 2 | AI | placebo | 9069 | 30,255 |
| Faiz 2021 [30] | Retrospective cohort | USA | all stage | 74.8 | postmenopausal | 2 years | 2 | AI | TAM | 64,384 | 22,042 |
| Franchi 2021 [31] | Retrospective cohort | Italy | early breast cancer | NA | postmenopausal | NA | 2 | AI | TAM | 7881 | 7881 |
| Chang 2022 [32] | Retrospective cohort | Taiwan | all stage | 62.53 | mixed | NA | 2 | AI | TAM | 11,728 | 16,730 |
| Thurlimann 2005 [33] | Prospective RCT | worldwide | early breast cancer | 61 | postmenopausal | 25.8 months | 2 | letrozole | TAM | 3975 | 3988 |
| Sund 2021 [10] | Retrospective cohort | Sweden | early breast cancer | 66 | postmenopausal | 46.8 months | 2 | AI | placebo | 1481 | 3668 |
| Haque 2016 [34] | Retrospective cohort | USA | all stage | 66.8 | postmenopausal | 2.3 years | 2 | AI | TAM | 3807 | 4207 |
| Outcome | No. of Studies | No. of Patients Events/Total | Pooled Event Rate (per 100 Person) | 95% CI | I2 | p for Heterogeneity |
|---|---|---|---|---|---|---|
| Overall, any type of cardiovascular disease | 6 [21,25,31,32,33,34] | 2453/47,381 | 6.08 | 2.91 to 10.31 | 100% | <0.01 |
| Heart | ||||||
| Coronary artery disease including angina | 6 [21,24,25,26,33,34] | 1499/42,879 | 3.85 | 1.48 to 7.18 | 99% | <0.01 |
| Myocardial infarction | 9 [8,9,20,24,26,28,31,32,34] | 977/75,617 | 1.08 | 0.61 to 1.65 | 97% | <0.01 |
| Heart failure | 8 [8,9,24,25,31,32,33,34] | 2338/54,101 | 2.13 | 0.79 to 4.48 | 100% | 0 |
| Brain | ||||||
| Any type of stroke | 2 [24,28] | 1287/34,658 | 3.34 | 0 to 12.81 | 100% | <0.01 |
| Ischemic stroke | 5 [8,9,28,31,32] | 1293/49,294 | 2.09 | 1.21 to 3.21 | 98% | <0.01 |
| Thromboembolism | ||||||
| Overall, venous thromboembolism | 6 [21,22,24,25,30,33] | 7503/107,260 | 2.95 | 0.55 to 7.12 | 100% | 0 |
| Pulmonary thromboembolism | 4 [21,22,24,30] | 2701/101,750 | 1.03 | 0.01 to 3.61 | 100% | 0 |
| Deep vein thrombosis | 4 [21,22,24,30] | 5866/101,750 | 2.64 | 0.30 to 7.19 | 100% | 0 |
| Outcome | No. of Studies | No. of Patients, Events/Total (AI) | No. of Patients, Events/Total (Tamoxifen) | OR | 95% CI | I2 | p for Heterogeneity |
|---|---|---|---|---|---|---|---|
| Overall, any type of cardiovascular disease | 6 [21,25,31,32,33,34] | 2453/47,381 | 3361/37,429 | 0.81 | 0.38 to 1.75 | 99% | <0.01 |
| Heart | |||||||
| Coronary artery disease including angina | 6 [21,24,25,26,33,34] | 1499/42,879 | 523/15,145 | 0.97 | 0.50 to 1.89 | 95% | <0.01 |
| Myocardial infarction | 9 [8,9,20,24,26,28,31,32,34] | 977/75,617 | 412/53,824 | 1.30 | 0.88 to 1.93 | 88% | <0.01 |
| Heart failure | 8 [8,9,24,25,31,32,33,34] | 2338/54,101 | 1234/50,290 | 1.20 | 0.78 to 1.86 | 96% | <0.01 |
| Brain | |||||||
| Any type of stroke | 2 [24,28] | 1287/34,658 | 237/9367 | 1.02 | 0.74 to 1.40 | 69% | 0.07 |
| Ischemic stroke | 5 [8,9,28,31,32] | 1293/49,294 | 833/45,349 | 1.39 | 1.07 to 1.81 | 85% | <0.01 |
| Thromboembolism | |||||||
| Overall, venous thromboembolism | 6 [21,22,24,25,30,33] | 7503/107,260 | 2893/37,001 | 0.61 | 0.37 to 1.00 | 97% | <0.01 |
| Pulmonary thromboembolism | 4 [21,22,24,30] | 2701/101,750 | 991/31,472 | 1.01 | 0.38 to 2.67 | 94% | <0.01 |
| Deep vein thrombosis | 4 [21,22,24,30] | 5866/101,750 | 2060/31,472 | 0.68 | 0.39 to 1.17 | 96% | <0.01 |
| Outcome | No. of Studies | Mean Difference | 95% CI | I2 | p for Heterogeneity | |
|---|---|---|---|---|---|---|
| Comparison with baseline | ||||||
| HDL-cholesterol | 6-month | 5 [15,17,18,23] | −2.47 | −4.26 to −0.69 | 81% | <0.01 |
| 12-month | 4 [17,18,23] | 1.16 | −3.18 to 5.49 | 94% | <0.01 | |
| LDL-cholesterol | 6-month | 5 [17,18,23] | 10.48 | −2.95 to 23.92 | 87% | <0.01 |
| 12-month | 5 [17,18,23] | 8.05 | −3.68 to 19.79 | 87% | <0.01 | |
| Total cholesterol | 6-month | 6 [15,17,18,23] | 5.16 | −2.07 to 12.40 | 83% | <0.01 |
| 12-month | 5 [17,18,23] | 4.62 | −4.00 to 13.24 | 99% | <0.01 | |
| Comparison with tamoxifen | ||||||
| HDL-cholesterol | 6-month | 2 [15,23] | −3.67 | −12.31 to 4.97 | 99% | <0.01 |
| 12-month | 2 [17,23] | −1.52 | −4.79 to 7.75 | 99% | <0.01 | |
| LDL-cholesterol | 6-month | 2 [17,23] | 6.48 | 0.64 to 16.32 | 99% | <0.01 |
| 12-month | 2 [17,23] | 11.87 | −15.77 to 39.50 | 100% | <0.01 | |
| Total cholesterol | 6-month | 3 [15,17,23] | 1.28 | −14.97 to 17.53 | 100% | <0.01 |
| 12-month | 2 [17,23] | 6.89 | −20.75 to 34.52 | 100% | <0.01 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, J.-J.; Jung, E.-A.; Kim, Z.; Kim, B.-Y. Risk of Cardiovascular Events and Lipid Profile Change in Patients with Breast Cancer Taking Aromatase Inhibitor: A Systematic Review and Meta-Analysis. Curr. Oncol. 2023, 30, 1831-1843. https://doi.org/10.3390/curroncol30020142
Yoo J-J, Jung E-A, Kim Z, Kim B-Y. Risk of Cardiovascular Events and Lipid Profile Change in Patients with Breast Cancer Taking Aromatase Inhibitor: A Systematic Review and Meta-Analysis. Current Oncology. 2023; 30(2):1831-1843. https://doi.org/10.3390/curroncol30020142
Chicago/Turabian StyleYoo, Jeong-Ju, Eun-Ae Jung, Zisun Kim, and Bo-Yeon Kim. 2023. "Risk of Cardiovascular Events and Lipid Profile Change in Patients with Breast Cancer Taking Aromatase Inhibitor: A Systematic Review and Meta-Analysis" Current Oncology 30, no. 2: 1831-1843. https://doi.org/10.3390/curroncol30020142
APA StyleYoo, J.-J., Jung, E.-A., Kim, Z., & Kim, B.-Y. (2023). Risk of Cardiovascular Events and Lipid Profile Change in Patients with Breast Cancer Taking Aromatase Inhibitor: A Systematic Review and Meta-Analysis. Current Oncology, 30(2), 1831-1843. https://doi.org/10.3390/curroncol30020142





