Autoantibody Diversity Is Augmented in Women with Breast Cancer and Is Related to the Stage of the Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. The Study Design
2.2. Participants
2.3. Sample Size
2.4. Blood Samples
2.5. T47D Cell Line Culture
2.6. T47D Protein Extraction
2.7. SDS-PAGE and Western Blot
2.8. Image Analysis
2.9. Statistical Analysis
3. Results
3.1. Characteristics of Participants
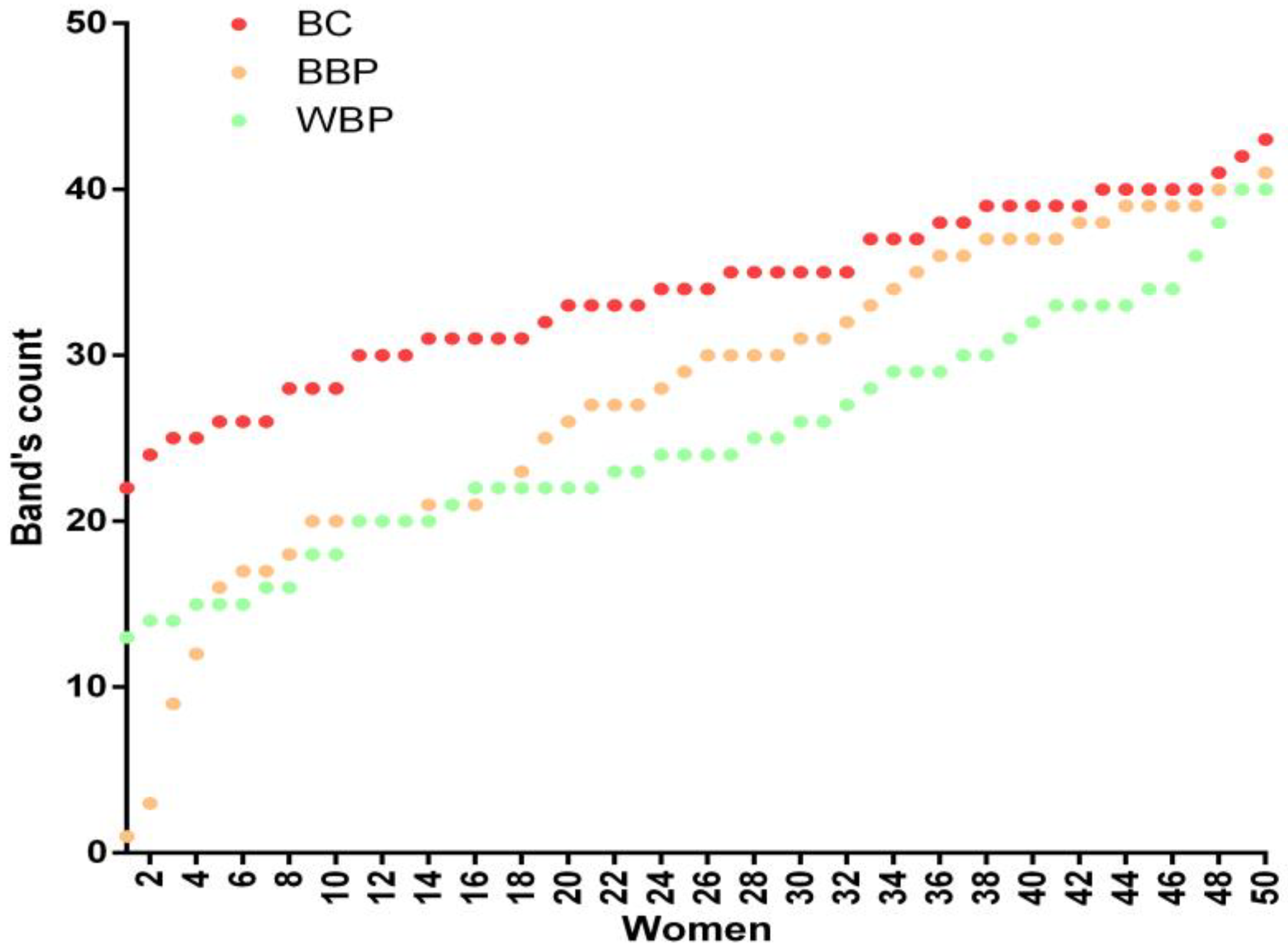
3.2. Autoantibodies from BC Patients Recognize a Larger Number of T47D Antigens vs. BBP and WBP
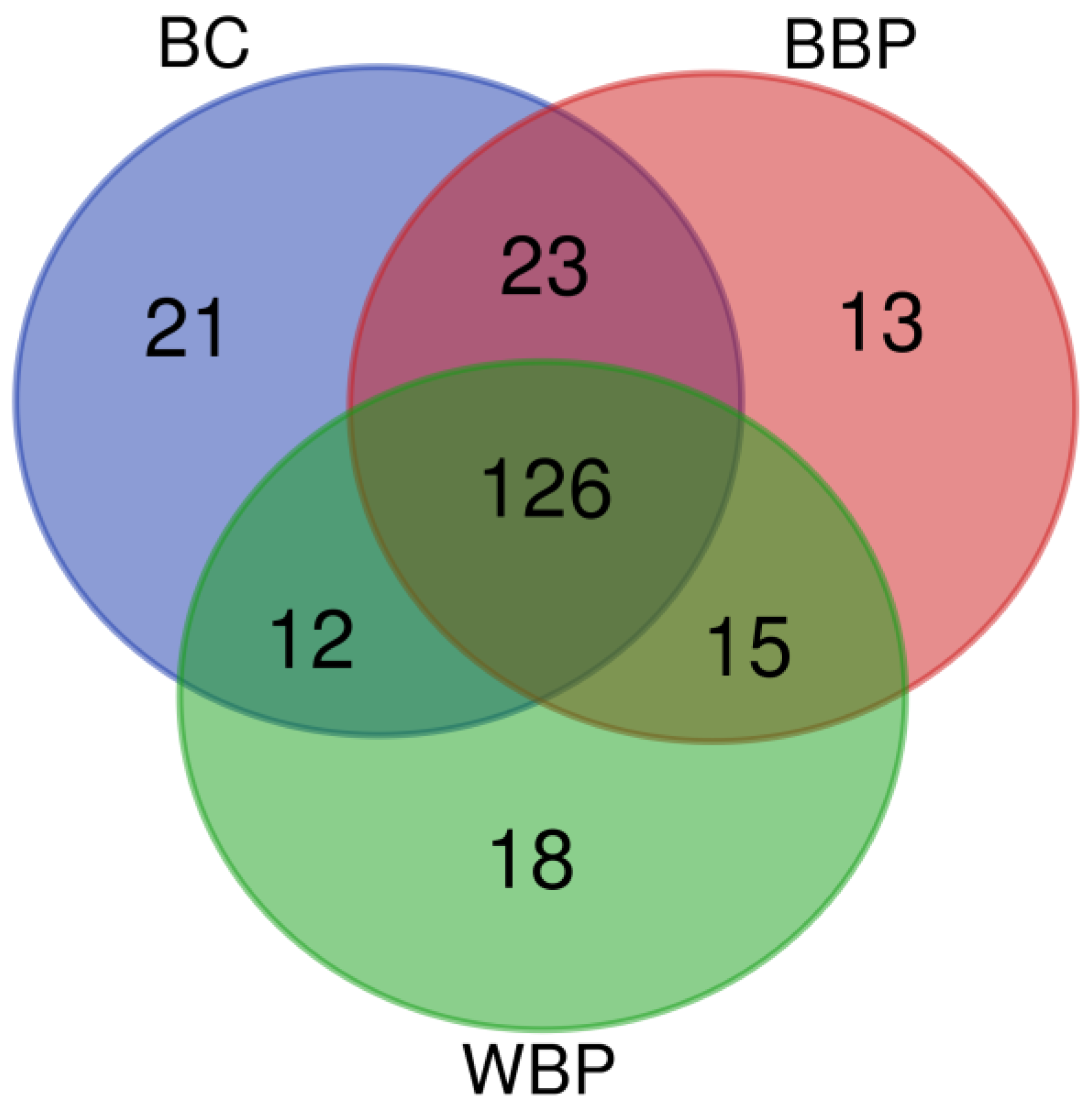
3.3. Sera Antibody Patterns of BC and BBP Groups Are Very Similar
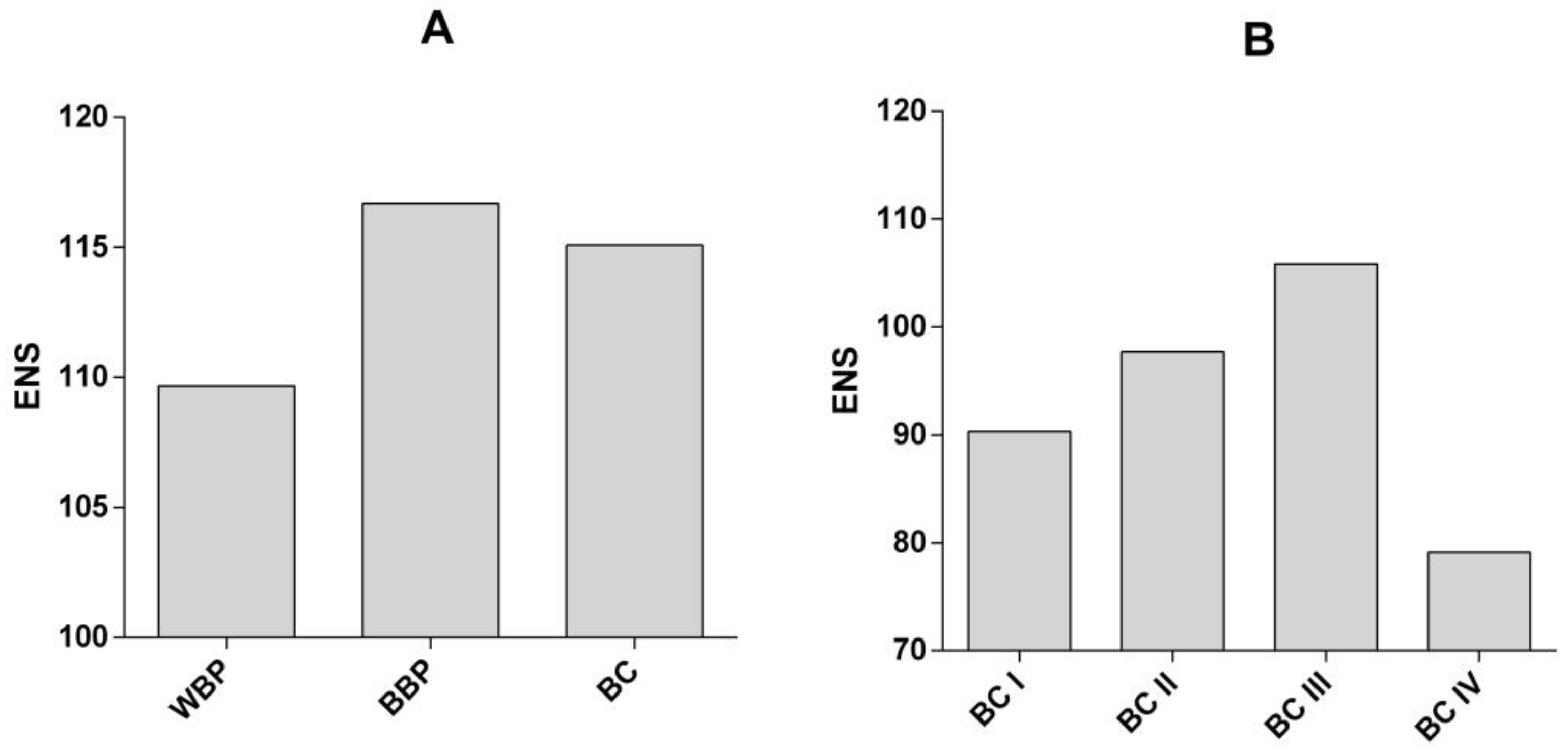
3.4. Diversity in the Antibodies Repertoire Is Increased in Patients with BBP and BC
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Global Cancer Observarory. 2023. Available online: https://gco.iarc.fr/today/online-analysis-pie?v=2020&mode=cancer&mode_population=continents&population=900&populations=900&key=total&sex=2&cancer=39&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B%5D=16&nb_items=7&group_cancer=1&include_nmsc=1&include_nmsc_other=1&half_pie=0&donut=0 (accessed on 15 March 2022).
- National Institute of Statistics, Geography and Informatics. 2021, Mexico. Statistics Regarding the World Day of the Fight Against Breast Cancer (October 19). Press Release no. 571/21. 18 October 2021. Available online: https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2021/EAP_LUCHACANCER2021.pdf (accessed on 15 March 2022).
- Mohar-Betancourt, A.; Alvarado-Miranda, A.; Torres-Domínguez, J.A.; Cabrera, P.; Lara Medina, F.; Villarreal-Gómez, Y.S.; Reynoso-Noverón, N. Prognostic factors in patients with breast cancer and brain metastasis as the first site of recurrence. Public Health Mex. 2018, 60, 141–150. [Google Scholar] [CrossRef]
- Qiu, J.; Keyser, B.; Lin, Z.T.; Wu, T. Autoantibodies as Potential Biomarkers in Breast Cancer. Biosensors 2018, 8, 67. [Google Scholar] [CrossRef] [PubMed]
- Gyurján, I.; Rosskopf, S.; Coronell, J.A.L.; Muhr, D.; Singer, C.; Weinhäusel, A. IgG based immunome analyses of breast cancer patients reveal underlying signaling pathways. Oncotarget 2019, 10, 3491–3505. [Google Scholar] [CrossRef] [PubMed]
- Kostianets, O.; Shyyan, M.; Antoniuk, S.V.; Filonenko, V.; Kiyamova, R. Panel of SEREX-defined antigens for breast cancer autoantibodies profile detection. Biomarkers 2017, 22, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Yang, R.; Han, Y.; Yi, W.; Long, Q. Autoantibodies as biomarkers for breast cancer diagnosis and prognosis. Front. Immunol. 2022, 13, 1035402. [Google Scholar] [CrossRef]
- López-Árias, E.; Aguilar-Lemarroy, A.; Jave-Suárez, F.L.; Morgan-Villela, G.; Mariscal-Ramirez, I.; Martinez Velazquez, M.; Alvarez, A.H.; Gutierrez-Ortega, A.; Hernandez-Gutierrez, R. Alpha 1-antitrypsin: A novel tumor-associated antigen identified in patients with early-stage breast cancer. Electrophoresis 2012, 33, 2130–2137. [Google Scholar] [CrossRef]
- Fernández-Grijalva, A.L.; Aguilar-Lemarroy, A.; Jave-Suarez, L.F.; Gutierrez-Ortega, A.; Godinez-Melgoza, P.A.; Herrera-Rodriguez, S.E.; Mariscal-Ramirez, I.; Martinez-Velazquez, M.; Gawinowicz, M.A.; Martinez-Silva, M.G.; et al. Alpha 2HS-glycoprotein, a tumor-associated antigen (TAA) detected in Mexican patients with early-stage breast cancer. J. Proteom. 2015, 112, 301–312. [Google Scholar] [CrossRef]
- Oaxaca-Camacho, A.R.; Ochoa-Mojica, O.R.; Aguilar-Lemarroy, A.; Jave-Suárez, L.F.; Muñoz-Valle, J.F.; Padilla-Camberos, E.; Núñez-Hernández, J.A.; Herrera-Rodríguez, S.E.; Martínez-Velázquez, M.; Carranza-Aranda, A.S.; et al. Serum Analysis of Women with Early-Stage Breast Cancer Using a Mini-Array of Tumor-Associated Antigens. Biosensors 2020, 10, 149. [Google Scholar] [CrossRef]
- Liu, H.; Perugino, C.A.; Ghebremichael, M.; Wallace, Z.S.; Montesi, S.B.; Stone, J.H.; Pillai, S. Disease Severity Linked to Increase in Autoantibody Diversity in IgG4-Related Disease. Arthritis Rheumatol. 2020, 72, 687–693. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Tamura, K.; Stecher, G.; Peterson, D.; Filipski, A.; Kumar, S. MEGA6: Molecular Evolutionary Genetics Analysis version 6.0. Mol. Biol. Evol. 2013, 30, 2725–2729. [Google Scholar] [CrossRef] [PubMed]
- Benz, C.C. Impact of aging on the biology of breast cancer. Crit. Rev. Oncol. Hematol. 2008, 66, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Chen, J.; Li, Q.; Huang, W.; Lan, H.; Jiang, H. Association between breastfeeding and breast cancer risk: Evidence from a meta-analysis. Breastfeed Med. 2015, 10, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Arceo-Martínez, M.T.; López-Meza, J.E.; Ochoa-Zarzosa, A.; Palomera-Sanchez, Z. Current status of breast cancer in Mexico: Main types and risk factors. Mex. Gaz. Oncol. 2021, 20, 101–110. [Google Scholar] [CrossRef]
- Jost, L. Entropy and diversity. Oikos 2006, 113, 363–365. [Google Scholar] [CrossRef]
- Largeot, A.; Pagano, G.; Gonder, S.; Moussay, E.; Paggetti, J. The B-side of Cancer Immunity: The Underrated Tune. Cells 2019, 8, 449. [Google Scholar] [CrossRef]
- Madrid, F.F.; Maroun, M.C.; Olivero, O.A.; Long, M.; Stark, A.; Grossman, L.I.; Binder, W.; Dong, J.; Burke, M.; Nathanson, S.D.; et al. Autoantibodies in breast cancer sera are not epiphenomena and may participate in carcinogenesis. BMC Cancer 2015, 15, 407. [Google Scholar] [CrossRef]
- Arias-Pulido, H.; Cimino-Mathews, A.; Chaher, N.; Qualls, C.; Joste, N.; Colpaert, C.; Marotti, J.D.; Foisey, M.; Prossnitz, E.R.; Emens, L.A.; et al. The combined presence of CD20 + B cells and PD-L1 + tumor-infiltrating lymphocytes in inflammatory breast cancer is prognostic of improved patient outcome. Breast Cancer Res. Treat. 2018, 171, 273–282. [Google Scholar] [CrossRef]
- Pucci, F.; Garris, C.; Lai, C.P.; Newton, A.; Pfirschke, C.; Engblom, C.; Alvarez, D.; Sprachman, M.; Evavold, C.; Magnuson, A.; et al. SCS macrophages suppress melanoma by restricting tumor-derived vesicle-B cell interactions. Science 2016, 352, 242–246. [Google Scholar] [CrossRef]
- Reddy, R.; Mintz, J.; Golan, R.; Firdaus, F.; Ponce, R.; Van Booven, D.; Manoharan, A.; Issa, I.; Blomberg, B.; Arora, H. Antibody Diversity in Cancer: Translational Implications and Beyond Vaccines. Vaccines 2022, 10, 1165. [Google Scholar] [CrossRef]
- Takai, T.; Li, M.; Sylvestre, D.; Clynes, R.; Ravetch, J.V. FcR gamma chain deletion results in pleiotrophic effector cell defects. Cell 1994, 76, 519–529. [Google Scholar] [CrossRef] [PubMed]
- Satoh, M.; Takano, S.; Sogawa, K.; Noda, K.; Yoshitomi, H.; Ishibashi, M.; Mogushi, K.; Takizawa, H.; Otsuka, M.; Shimizu, H.; et al. Immune-complex level of cofilin-1 in sera is associated with cancer progression and poor prognosis in pancreatic cancer. Cancer Sci. 2017, 108, 795–803. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.T.; Coussens, L.M. Humoral immunity, inflammation and cancer. Curr. Opin. Immunol. 2007, 19, 209–216. [Google Scholar] [CrossRef] [PubMed]
- DeNardo, D.G.; Coussens, L.M. Inflammation and breast cancer. Balancing immune response: Crosstalk between adaptive and innate immune cells during breast cancer progression. Breast Cancer Res. 2007, 9, 212. [Google Scholar] [CrossRef] [PubMed]
- Szekely, B.; Bossuyt, V.; Li, X.; Wali, V.B.; Patwardhan, G.A.; Frederick, C.; Silber, A.; Park, T.; Harigopal, M.; Pelekanou, V.; et al. Immunological differences between primary and metastatic breast cancer. Ann. Oncol. 2018, 29, 2232–2239. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, H.; Jamiyan, T.; Yamaguchi, R.; Kakumoto, A.; Abe, A.; Harada, O.; Enkhbat, B.; Masunaga, A. Prognostic value of tumor-infiltrating B lymphocytes and plasma cells in triple-negative breast cancer. Breast Cancer. 2021, 28, 904–914. [Google Scholar] [CrossRef]
- Hu, Q.; Hong, Y.; Qi, P.; Lu, G.; Mai, X.; Xu, S.; He, X.; Guo, Y.; Gao, L.; Jing, Z.; et al. Atlas of breast cancer infiltrated B-lymphocytes revealed by paired single-cell RNA-sequencing and antigen receptor profiling. Nat. Commun. 2021, 12, 2186. [Google Scholar] [CrossRef]
- Liu, M.; Wei, F.; Wang, J.; Yu, W.; Shen, M.; Liu, T.; Zhang, D.; Wang, Y.; Ren, X.; Sun, Q. Myeloid-derived suppressor cells regulate the immunosuppressive functions of PD-1(−)PD-L1(+) Bregs through PD-L1/PI3K/AKT/NF-kappaB axis in breast cancer. Cell Death Dis. 2021, 12, 465. [Google Scholar] [CrossRef]
- Shen, M.; Wang, J.; Yu, W.; Zhang, C.; Liu, M.; Wang, K.; Yang, L.; Wei, F.; Wang, S.E.; Sun, Q.; et al. A novel MDSC-induced PD-1(-)PD-L1(+) B-cell subset in breast tumor microenvironment possesses immuno-suppressive properties. Oncoimmunology 2018, 7, e1413520. [Google Scholar] [CrossRef]

| WBP | BBP | BC | p | |
|---|---|---|---|---|
| Age, years | 39.68 ± 12.33 | 40.42 ± 11.69 | 51.28 ± 13.45 | <0.001 a |
| Weight, kg | 61.75 ± 9.15 | 65.20 ± 13.56 | 66.28 ± 15.70 | 0.362 b |
| Height, m | 1.56 ± 0.06 | 1.54 ± 0.08 | 1.54 ± 0.08 | 0.335 a |
| BMI, kg/m2 | 25.51 ± 3.77 | 27.56 ± 5.46 | 27.82 ± 5.30 | 0.108 b |
| Gestations, no. | 1.36 ± 1.54 | 2.11 ± 1.82 | 3.48 ± 2.05 | <0.001 b |
| Mode of births | ||||
| Vaginal | 0.78 ± 1.26 | 0.95 ±1.29 | 2.56 ± 2.16 | <0.001 b |
| C-section | 0.34± 0.75 | 0.66 ± 1.02 | 0.54 ± 0.93 | 0.243 b |
| Abortions, no. | 0.17 ± 0.50 | 0.37 ± 0.69 | 0.38± 0.98 | 0.276 b |
| Total breastfeeding length, months | 3.89 ± 6.84 | 8.88 ± 10.32 | 11.96 ± 9.95 | <0.001 b |
| Abdominal perimeter, cm | 85.12 ± 17.92 | 93.34 ± 11.90 | 95.67 ± 13.33 | 0.003 b |
| Hip perimeter, cm | 91.90 ± 19.41 | 99.33 ± 12.32 | 102.16 ± 12.51 | 0.006 b |
| Stage | I (n = 6) | II (n = 11) | III (n = 23) | IV (n = 5) | Not Classified (n = 5) | p |
|---|---|---|---|---|---|---|
| Age, years | 50 ± 20.09 | 51.45 ± 14.96 | 51.13 ± 12.39 | 50.6 ± 13.37 | 53 ± 12.94 | 0.999 a |
| BMI, kg/m2 | 28.94 ± 8.6 | 27.09 ± 5.18 | 27.95 ± 5.01 | 28.62 ± 3.5 | 28.88 ± 5.24 | 0.944 a |
| Gestations, no. | 3.17 ± 1.17 | 3.64 ± 1.75 | 3.43 ± 2.57 | 3.4 ± 1.67 | 4 ± 1 | 0.983 a |
| Mode of births | ||||||
| Vaginal | 2.64 ± 1.63 | 2.73 ± 2.33 | 2.22 ± 2.33 | 3 ± 2.24 | 3.67 ± 1.53 | 0.814 a |
| C-section | 0.33 ± 0.82 | 0.81 ± 1.25 | 0.57 ± 0.9 | 0.4 ± 0.89 | 0.25 ± 0.5 | 0.793 a |
| Abortions, no. | 0.17 ± 0.41 | 0.09 ±0.3 | 0.65 ± 1.34 | 0.2 ± 0.45 | 0 ± 0 | 0.473 a |
| Total breastfeeding length, months | 16 ± 10.81 | 10.82 ± 7.65 | 11.75 ± 12.46 | 10 ± 5.1 | 12.67 ± 1.15 | 0.865 a |
| Histological subtypes | ||||||
| Invasive ductal carcinoma, n(%) | 3 | 8 | 16 | 5 | 3 | 0.993 c |
| Invasive lobular carcinoma, n(%) | 0 | 0 | 1 | 0 | 0 | |
| Tubular ductal carcinoma, n(%) | 0 | 0 | 1 | 0 | 0 | |
| Mucinous carcinoma, n(%) | 0 | 1 | 0 | 0 | 0 | |
| Tubulo-lobular carcinoma, n(%) | 0 | 0 | 1 | 0 | 0 | |
| Tumor molecular characteristics | ||||||
| SBR | 8.67 ± 0.58 | 6.29 ± 1.5 | 7.64 ± 1.55 | 7.33 ± 1.53 | 4 ± 0 | 0.077 b |
| ER | 15 ± 21.21 | 81.11 ± 9.28 | 44.71 ± 39.86 | 12 ± 28.63 | 70 ± 34.64 | 0.009 b |
| PR | 20 ± 28.28 | 60 ± 37.8 | 22.35 ± 30.32 | 17 ± 38.01 | 40 ± 56.57 | 0.210 b |
| Ner2/Neu | 50 ± 70.71 | 10 ± 26.46 | 31.76 ± 44.61 | 40 ± 54.77 | 66.67 ± 57.74 | 0.456 b |
| Ki67 | 27.5 ± 31.82 | 36.67 ± 28.83 | 51.47 ± 30.71 | 50 ± 23.43 | 26.67 ± 20.82 | 0.466 a |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Hernández, J.; León-Díaz, R.; Zentella, A.; Lamoyi, E.; Esquivel-Velázquez, M.; Barranca-Enríquez, A.; Romo-González, T. Autoantibody Diversity Is Augmented in Women with Breast Cancer and Is Related to the Stage of the Disease. Curr. Oncol. 2023, 30, 8793-8804. https://doi.org/10.3390/curroncol30100634
Pérez-Hernández J, León-Díaz R, Zentella A, Lamoyi E, Esquivel-Velázquez M, Barranca-Enríquez A, Romo-González T. Autoantibody Diversity Is Augmented in Women with Breast Cancer and Is Related to the Stage of the Disease. Current Oncology. 2023; 30(10):8793-8804. https://doi.org/10.3390/curroncol30100634
Chicago/Turabian StylePérez-Hernández, Jesús, Rosalba León-Díaz, Alejandro Zentella, Edmundo Lamoyi, Marcela Esquivel-Velázquez, Antonia Barranca-Enríquez, and Tania Romo-González. 2023. "Autoantibody Diversity Is Augmented in Women with Breast Cancer and Is Related to the Stage of the Disease" Current Oncology 30, no. 10: 8793-8804. https://doi.org/10.3390/curroncol30100634
APA StylePérez-Hernández, J., León-Díaz, R., Zentella, A., Lamoyi, E., Esquivel-Velázquez, M., Barranca-Enríquez, A., & Romo-González, T. (2023). Autoantibody Diversity Is Augmented in Women with Breast Cancer and Is Related to the Stage of the Disease. Current Oncology, 30(10), 8793-8804. https://doi.org/10.3390/curroncol30100634





