Web-Based Peer Navigation for Men with Prostate Cancer and Their Family Caregivers: A Pilot Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Study Participants
2.4. Intervention
2.5. Outcomes
2.6. Analysis
3. Results
3.1. Participant Characteristics
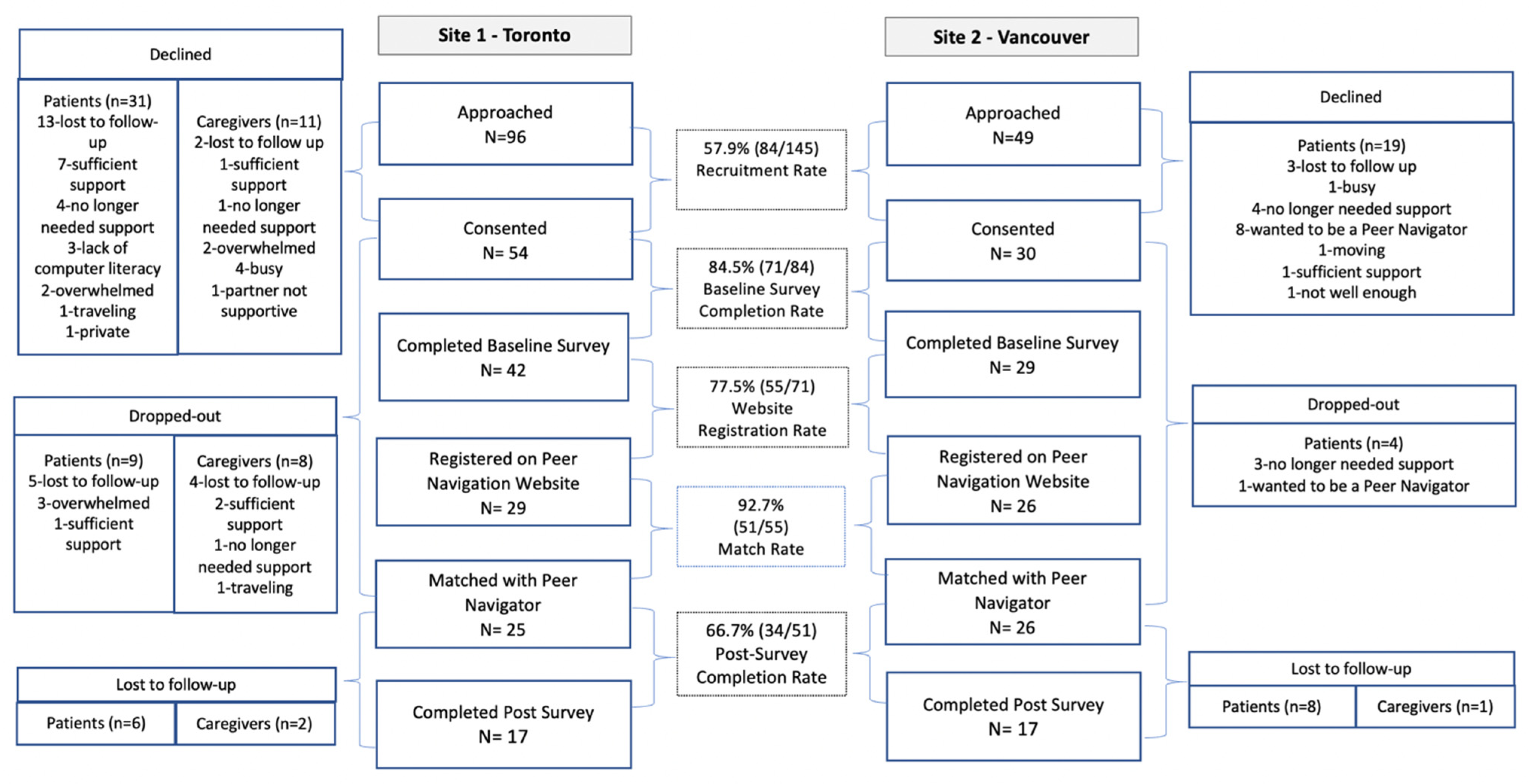
3.2. Feasibility
3.3. Acceptability
3.3.1. Satisfaction
3.3.2. Matching Preferences
3.3.3. Participant–Peer Navigator Interactions
3.3.4. Health Library Usage
3.3.5. Perceived Benefits
3.4. Possible Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Canadian Cancer Society. 2020 Canadian Cancer Statistics; Canadian Cancer Society: Toronto, ON, Canada, 2020. [Google Scholar]
- Canadian Cancer Society. Canadian Cancer Statistics: A 2018 Special Report; Canadian Cancer Society: Toronto, ON, Canada, 2018. [Google Scholar]
- Thera, R.; Carr, D.T.; Groot, D.G.; Baba, N.; Jana, D.K. Understanding Medical Decision-making in Prostate Cancer Care. Am. J. Men’s Health 2018, 12, 1635–1647. [Google Scholar] [CrossRef] [PubMed]
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; De Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S.; et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2017, 71, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.J.; Weinberger, M.I.; Nelson, C.J. Prostate cancer: Psychosocial implications and management. Future Oncol. 2008, 4, 561–568. [Google Scholar] [CrossRef] [Green Version]
- Chen, R.C.; Basak, R.; Meyer, A.M.; Kuo, T.M.; Carpenter, W.R.; Agans, R.P.; Broughman, J.R.; Reeve, B.B.; Nielsen, M.E.; Usinger, D.S.; et al. Association between choice of radical prostatectomy, external beam radiotherapy, brachytherapy, or active surveillance and patient-reported quality of life among men with localized prostate cancer. JAMA 2017, 317, 1141–1150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Resnick, M.J.; Koyama, T.; Fan, K.H.; Albertsen, P.C.; Goodman, M.; Hamilton, A.S.; Hoffman, R.M.; Potosky, A.L.; Stanford, J.L.; Stroup, A.M. Long-Term Functional Outcomes after Treatment for Localized Prostate Cancer. NEJM. 2013, 368, 436–445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canadian Partnership Against Cancer. Prostate Cancer Control in Canada: A System Performance Spotlight Report; Canadian Partnership Against Cancer: Toronto, ON, Canada, 2015. [Google Scholar]
- King, A.J.L.; Evans, M.; Moore, T.H.M.; Paterson, C.; Sharp, D.; Persad, R.; Huntley, A. Prostate cancer and supportive care: A systematic review and qualitative synthesis of men’s experiences and unmet needs. Euro. J. Cancer Care 2015, 24, 618–634. [Google Scholar] [CrossRef] [Green Version]
- Goodwin, B.C.; Ralph, N.; Ireland, M.J.; Hyde, M.K.; Oliffe, J.L.; Dunn, J.; Chambers, S. The role of masculinities in psychological and emotional help seeking by men with prostate cancer. Psycho-Oncology 2019, 29, 356–363. [Google Scholar] [CrossRef]
- Ream, E.; Quennell, A.; Fincham, L.; Faithfull, S.; Khoo, V.; Wilson-Barnett, J.; Richardson, A. Supportive care needs of men living with prostate cancer in England: A survey. Br. J. Cancer 2008, 98, 1903–1909. [Google Scholar] [CrossRef] [Green Version]
- Steginga, S.K.; Occhipinti, S.; Dunn, J.; Gardiner, R.A.; Heathcote, P.; Yaxley, J. The supportive care needs of men with prostate cancer. Psycho-Oncology 2001, 10, 66–75. [Google Scholar] [CrossRef]
- Boberg, E.W.; Gustafson, D.H.; Hawkins, R.P.; Offord, K.P.; Koch, C.; Wen, K.-Y.; Kreutz, K.; Salner, A. Assessing the unmet information, support and care delivery needs of men with prostate cancer. Patient Educ. Couns. 2003, 49, 233–242. [Google Scholar] [CrossRef]
- Ettridge, K.; Bowden, J.; Chambers, S.; Smith, D.; Murphy, M.; Evans, S.; Roder, D.; Miller, C. “Prostate cancer is far more hidden…”: Perceptions of stigma, social isolation and help-seeking among men with prostate cancer. Euro. J. Cancer Care 2018, 27, e12790. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, R.; Kendell, C.; Lethbridge, L. Prostate cancer survivors follow-up care after treatment: A population-based study in Nova Scotia, Canada. Oral Presentation at the Association of Supportive Care in Cancer (MASCC) Annual Meeting, Seville, Spain, 24–26 June 2020. [Google Scholar]
- Flora, P.; Milosevic, E.; Soheilipour, S.; Maharaj, N.; Dirlea, M.; Parvin, L.; Matthew, A.; Kazanjian, A.; Bender, J.L. “I know how difficult it can be”: A closer look at characteristics and motivations of volunteer prostate cancer peer navigators". In Proceedings of the Canadian Association of Psychosocial Oncology Conference Proceedings, Toronto, ON, Canada, 30 May–1 June 2018. [Google Scholar]
- Maharaj, N.; Soheilipour, S.; Bender, J.L.; Kazanjian, A. Understanding Prostate Cancer Patients’ Support Needs: How Do They Manage Living With Cancer? Illn. Crisis Loss 2018, 29, 51–73. [Google Scholar] [CrossRef]
- Girgis, A.; Lambert, S.; Johnson, C.; Waller, A.; Currow, D. Physical, psychosocial, relationship, and economic burden of caring for people with cancer: A review. J. Oncol. Pract. 2013, 9, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Given, B.; Sherwood, P.R. Family care for the older person with cancer. Sem. Oncol. Nurs. 2006, 22, 43–50. [Google Scholar] [CrossRef]
- Sinfield, P.; Baker, R.; Ali, S.; Richardson, A. The needs of carers of men with prostate cancer and barriers and enablers to meeting them: A qualitative study in England. Euro. J. Cancer Care 2012, 21, 527–534. [Google Scholar] [CrossRef]
- Sinfield, P.; Baker, R.; Camosso-Stefinovic, J.; Colman, A.M.; Tarrant, C.; Mellon, J.K.; Steward, W.; Kockelbergh, R.; Agarwal, S. Men’s and carers’ experiences of care for prostate cancer: A narrative literature review. Health Expect. 2009, 12, 301–312. [Google Scholar] [CrossRef] [Green Version]
- Cancer Journey Action Group. Navigation: A guide to Implementing Best Practices in Person-Centred Care. Canadian Partnership Against Cancer. 2012. Available online: https://s22457.pcdn.co/wp-content/uploads/2018/12/Implementing-Navigation-Guide-EN.pdf (accessed on 25 April 2022).
- Lopez, D.; Pratt-Chapman, M.L.; Rohan, E.A.; Sheldon, L.K.; Basen-Engquist, K.; Kline, R.; Shulman, L.N.; Flores, E.J. Establishing effective patient navigation programs in oncology. Support. Care Cancer 2019, 27, 1985–1996. [Google Scholar] [CrossRef]
- Wells, K.J.; Battaglia, T.A.; Dudley, D.J.; Garcia, R.; Greene, A.; Calhoun, E.; Mandelblatt, J.S.; Paskett, E.D.; Raich, P.C.; Patient Navigation Research Program. Patient navigation: State of the art or is it science? Cancer 2008, 113, 1999–2010. [Google Scholar] [CrossRef] [Green Version]
- Paskett, E.D.; Harrop, J.P.; Wells, K.J. Patient navigation: An update on the state of the science. CA Cancer J. Clin. 2011, 61, 237–249. [Google Scholar] [CrossRef] [Green Version]
- Ali-Faisal, S.F.; Colella, T.J.F.; Medina-Jaudes, N.; Benz Scott, L. The effectiveness of patient navigation to improve healthcare utilization outcomes: A meta-analysis of randomized controlled trials. Patient Educ. Couns. 2017, 100, 436–448. [Google Scholar] [CrossRef]
- Ustjanauskas, A.E.; Bredice, M.; Nuhaily, S.; Kath, L.; Wells, K.J. Training in Patient Navigation. Health Promot. Pract. 2016, 17, 373–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dionne-Odom, J.N.; Azuero, A.; Taylor, R.A.; Dosse, C.; Bechthold, A.C.; Currie, E.; Reed, R.D.; Harrell, E.R.; Engler, S.; Ejem, D.B.; et al. A lay navigator-led, early palliative care intervention for African American and rural family caregivers of individuals with advanced cancer (Project Cornerstone): Results of a pilot randomized trial. Cancer 2022, 128, 1321–1330. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aggarwal, R.; Ranganathan, P. Study designs: Part 4–Interventional studies. Perspect. Clin. Res. 2019, 10, 137. [Google Scholar] [CrossRef]
- Thabane, L.; Ma, J.; Chu, R.; Cheng, J.; Ismaila, A.; Rios, L.P.; Robson, R.; Thabane, M.; Giangregorio, L.; Goldsmith, C.H. A tutorial on pilot studies: The what, why and how. BMC Med. Res. Methodol. 2010, 10, 1. [Google Scholar] [CrossRef] [Green Version]
- Lazarus, S.; Folkman, R. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Cutrona, C.; Russel, D. Type of social support and specific stress: Toward a theory of optimal matching. In Social Support: An Interactional View; Sarason, B., Sarason, I., Pierce, G., Eds.; Wiley & Sons: Oxford, UK, 1990; pp. 319–366. [Google Scholar]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman and Company: New York, NY, USA, 2000. [Google Scholar]
- Flora, P.K.; Bender, J.L.; Miller, A.S.; Parvin, L.; Soheilipour, S.; Maharaj, N.; Milosevic, E.; Matthew, A.; Kazanjian, A. A core competency framework for prostate cancer peer navigation. Support. Care Cancer 2019, 28, 2605–2614. [Google Scholar] [CrossRef]
- Bender, J.; Flora, P.; Milosevic, E.; Soheilipour, S.; Maharaj, N.; Dirlea, M.; Parvin, L.; Matthew, A.; Kazanjian, A. Training in Peer Navigation: A Mixed-Methods Evaluation of a Blended Learning, Competency-Based Training Program for Prostate Cancer Peer Navigators. Support. Care Cancer 2021, 29, 1235–1244. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). JMIR 2004, 6, e132. [Google Scholar] [CrossRef]
- Eysenbach, G.; CONSORT-EHEALTH Group CE. CONSORT-EHEALTH: Improving and standardizing evaluation reports of Web-based and mobile health interventions. J. Med. Internet Res. 2011, 13, e126. [Google Scholar] [CrossRef]
- Jean-Pierre, P.; Fiscella, K.; Winters, P.C.; Post, U.; Wells, K.J.; McKoy, J.M.; Battaglia, T.; Simon, M.A.; Kilbourn, K.; Patient Navigation Research Program Group. Psychometric development and reliability analysis of a patient satisfaction with interpersonal relationship with navigator measure: A multi-site patient navigation research program study. Psycho-Oncology 2012, 21, 986–992. [Google Scholar] [CrossRef]
- Sauro, J.; Lewis, J.R. When designing usability questionnaires, does it hurt to be positive? In Proceedings of the Conference on Human Factors in Computing Systems, Vancouver, BC, Canada, 7 May 2011; ACM: New York, NY, USA, 2011; pp. 2215–2223. [Google Scholar]
- Fitch, M.I.; Pang, K.; VandeZande, D. Identifying patient-reported outcomes of telephone-based breast cancer support services. Can. Oncol. Nurs. J. 2017, 27, 115–123. [Google Scholar] [PubMed]
- Hibbard, J.H.; Mahoney, E.R.; Stockard, J.; Tusler, M. Development and testing of a short form of the patient activation measure. Health Serv. Res. 2005, 40, 1918–1930. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazanec, S.R.; Sattar, A.; Delaney, C.P.; Daly, B.J. Activation for Health Management in Colorectal Cancer Survivors and Their Family Caregivers. Wes. J. Nurs. Res. 2016, 38, 325–344. [Google Scholar] [CrossRef] [PubMed]
- Bansback, N.; Tsuchiya, A.; Brazier, J.; Anis, A. Canadian valuation of EQ-5D health states: Preliminary value set and considerations for future valuation studies. PLoS ONE 2012, 7, e31115. [Google Scholar] [CrossRef]
- Krahn, M.; Ritvo, P.; Irvine, J.; Tomlinson, G.; Bezjak, A.; Trachtenberg, J.; Naglie, G. Construction of the Patient-Oriented Prostate Utility Scale (PORPUS): A multiattribute health state classification system for prostate cancer. J. Clin. Epidemiol. 2000, 53, 920–930. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- VaglioJr, J.; Conard, M.; Poston, W.S.; O’Keefe, J.; Haddock, C.K.; House, J.; Spertus, J.A. Testing the performance of the ENRICHD Social Support Instrument in cardiac patients. Health Qual. Life Outcomes 2004, 2, 24. [Google Scholar] [CrossRef] [Green Version]
- Schofield, P.; Gough, K.; Lotfi-Jam, K.; Aranda, S. Validation of the Supportive Care Needs Survey-short form 34 with a simplified response format in men with prostate cancer. Psycho-Oncology 2012, 21, 1107–1112. [Google Scholar] [CrossRef]
- Girgis, A.; Lambert, S.; Lecathelinais, C. The supportive care needs survey for partners and caregivers of cancer survivors: Development and psychometric evaluation. Psycho-Oncology 2011, 20, 387–393. [Google Scholar] [CrossRef]
- Bender, J.L. The Internet as a Route to Health Information, Support, and Healthcare for Cancer Survivors. J. Natl. Compr. Cancer Netw. 2020, 18, 1586–1588. [Google Scholar] [CrossRef]
- Bender, J.L.; Feldman-Stewart, D.; Tong, C.; Lee, K.; Brundage, M.; Pai, H.; Robinson, J.; Panzarella, T. Health-Related Internet Use Among Men With Prostate Cancer in Canada: Cancer Registry Survey Study. J. Med. Internet Res. 2019, 21, e14241. [Google Scholar] [CrossRef] [PubMed]
- Oliffe, J. Health Behaviors, Prostate Cancer, and Masculinities. Men Masc. 2009, 11, 346–366. [Google Scholar] [CrossRef]
- Dillman, D.A.; Smyth, J.D.; Christian LMelani Dillman, D.A. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method; Wiley & Sons: Oxford, UK, 2009. [Google Scholar]
- Jean-Pierre, P.; Winters, P.C.; Clark, J.A.; Warren-Mears, V.; Wells, K.J.; Post, D.M.; LaVerda, N.; van Duyn, M.A.; Fiscella, K.; Patient Navigation Research Program Group. Do better-rated navigators improve patient satisfaction with cancer-related care? J. Cancer Educ. 2013, 28, 527–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Helgeson, V.; Gotlieb, B. Chapter 7: Support Groups. In Social Support Measurement and Intervention; Cohen, S., Underwood, L., Gottlieb, B., Eds.; Oxford University Press: New York, NY, USA, 2000. [Google Scholar]
- Pinto, A.D.; Glattstein-Young, G.; Mohamed, A.; Bloch, G.; Leung, F.H.; Glazier, R.H. Building a Foundation to Reduce Health Inequities: Routine Collection of Sociodemographic Data in Primary Care. J. Am. Board Fam. Med. 2016, 29, 348–355. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, S.; Shahid, R.K. Disparity in cancer care: A Canadian perspective. Curr. Oncol. 2012, 19, e376–e382. [Google Scholar] [CrossRef] [Green Version]
- Weber, B.A.; Roberts, B.L.; Yarandi, H.; Mills, T.L.; Chumbler, N.R.; Wajsman, Z. The Impact of Dyadic Social Support on Self-Efficacy and Depression After Radical Prostatectomy. J. Aging Health 2007, 19, 630–645. [Google Scholar] [CrossRef]
- Fiscella, K.; Ransom, S.; Jean-Pierre, P.; Cella, D.; Stein, K.; Bauer, J.E.; Crane-Okada, R.; Gentry, S.; Canosa, R.; Smith, T.; et al. Patient-reported outcome measures suitable to assessment of patient navigation. Cancer 2011, 117, 3601–3615. [Google Scholar] [CrossRef] [Green Version]
- Greene, J.; Hibbard, J.H. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Inter. Med. 2012, 27, 520–526. [Google Scholar] [CrossRef] [Green Version]
- Simard, S.; Thewes, B.; Humphris, G.; Dixon, M.; Hayden, C.; Mireskandari, S.; Ozakinci, G. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J. Cancer Surviv. 2013, 7, 300–322. [Google Scholar] [CrossRef]
- Van de Wal, M.; van Oort, I.; Schouten, J.; Thewes, B.; Gielissen, M.; Prins, J. Fear of cancer recurrence in prostate cancer survivors. Acta Oncol. 2016, 55, 821–827. [Google Scholar] [CrossRef]
- Carroll, J.K.; Humiston, S.G.; Meldrum, S.C.; Salamone, C.M.; Jean-Pierre, P.; Epstein, R.M.; Fiscella, K. Patients’ experiences with navigation for cancer care. Patient Educ. Couns. 2010, 80, 241–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Category | Count (%), Unless Otherwise Specified |
|---|---|---|
| Age (years): mean, (SD), range | 65.2 (7.1), 48–78 | |
| Participant | Patient | 29 (85.3) |
| Caregiver | 5 (14.7) | |
| Sex | Male | 29 (85.3) |
| Female | 5 (14.7) | |
| Race/Ethnicity | Caucasian | 30 (88.2) |
| Asian | 1 (2.9) | |
| Filipino | 1 (2.9) | |
| South Asian | 1 (2.9) | |
| West Indian | 1 (2.9) | |
| Relationship Status | Married/Common-Law/Dating | 31 (91.2) |
| Single/Widowed/Divorced | 3 (8.8) | |
| Sexual Orientation | Heterosexual | 31 (91.2) |
| Homosexual | 2 (5.9) | |
| Prefer not to say | 1 (2.9) | |
| Education completed | University | 21 (66.8) |
| College | 9 (26.8) | |
| Secondary school | 4 (11.8) | |
| Household Income | 40,000 or less | 2 (5.8) |
| 40,001–80,999 | 10 (29.4) | |
| 80,001–100,000 | 5 (14.7) | |
| More than 100,001 | 13 (38.2) | |
| Prefer not to say | 4 (11.8) | |
| Type of disease | Localized | 30 (88.2) |
| Metastatic | 3 (8.8) | |
| Not sure | 1 (2.9) | |
| Stage of Journey | Deciding on Treatment | 8 (24.2) |
| Active Surveillance | 4 (12.1) | |
| In-treatment | 5 (15.2) | |
| In- recovery/follow-up | 12 (36.4) | |
| In-recurrence | 4 (12.1) |
| Item | Mean (SD) | ||
|---|---|---|---|
| Total (n = 34) | Patient (n = 29) | Caregiver (n = 5) | |
| 1. Is courteous and respectful to me | 8.9 (1.7) | 8.9 (1.7) | 8.8 (1.3) |
| 2. Is easy to talk to | 8.7 (2.0) | 8.8 (1.9) | 8.2 (2.5) |
| 3. Makes me feel comfortable | 8.6 (2.1) | 8.6 (2.2) | 8.4 (1.5) |
| 4. Gives me enough time | 8.5 (2.2) | 8.6 (2.1) | 7.8 (2.5) |
| 5. Listens to my problems | 8.5 (2.4) | 8.6 (2.4) | 8 (2.5) |
| 6. Is dependable | 8.3 (2.4) | 8.4 (2.5) | 8 (2.1) |
| 7. Cares about me personally | 8.2 (2.6) | 8.3 (2.7) | 8 (2.4) |
| 8. Is easy for me to reach | 8.2 (2.4) | 8.3 (2.4) | 8 (2.1) |
| 9. Figures out important issues in my healthcare | 7.8 (2.6) | 7.9 (2.7) | 7.2 (2.2) |
| Mean satisfaction | 8.4 (2.5) | 8.4 (2.2) | 7.9 (2.1) |
| Item | Mean (SD) | ||
|---|---|---|---|
| Total (n = 34) | Patient (n = 29) | Caregiver (n = 5) | |
| 1. Online matching process | 7.4 (3.2) | 7.8 (3) | 4.8 (3.3) |
| 2. Process of registering on website | 7.3 (3.0) | 7.5 (3) | 6.6 (3.6) |
| 3. Support received from your navigator | 7.0 (3.7) | 7.3 (3.7) | 5.8 (3.7) |
| 4. Interactions with your navigator | 6.8 (3.6) | 7.3 (3.4) | 3.6 (3.5) |
| 5. Overall program satisfaction | 6.8 (2.9) | 7 (2.9) | 5.6 (3.5) |
| 6. Availability of your navigator | 6.4 (3.9) | 7 (3.8) | 3.6 (3.5) |
| 7. Interactions with your program staff | 6.1 (3.7) | 6.6 (3.6) | 3.6 (3.6) |
| 8. Support received from program staff | 5.3 (4.2) | 5.7 (4.3) | 3.6 (4.2) |
| 9. Length of the program | 5.3 (3.9) | 5.5 (4.1) | 4 (2.9) |
| 10. Messaging chat feature on website | 5.3 (4.2) | 5.8 (4.3) | 2.6 (2.8) |
| 11. Health library on website | 4.0 (4.1) | 4.1 (4.2) | 3.6 (3.9) |
| 12. Availability of program staff for program questions | 3.7 (4.2) | 4 (4.4) | 2 (2.3) |
| 13. Availability of program staff for technical questions | 3.4 (4.0) | 3.7 (4.3) | 1.4 (1.5) |
| Item (As a Result of My Interactions with My Navigator…) | Mean (SD) | ||
|---|---|---|---|
| Total (n = 34) | Patient (n = 29) | Caregiver (n = 5) | |
| Informational Support | 7.0 (3.03) | 7.2 (3) | 5.4 (3.5) |
| 1. I feel more informed about prostate cancer and its treatment | 6.9 (3.1) | 7.1 (3) | 5.8 (3.8) |
| 2. I feel more informed about resources and services | 6.7 (3.1) | 7 (3) | 4.8 (3.5) |
| 3. I feel more informed about the road ahead and what to expect | 7.1 (3.1) | 7.2 (3) | 5.8 (3.8) |
| 4. I have the information to move forward | 7.2 (2.8) | 7.5 (2.8) | 5.3 (3) |
| Emotional Support | 7.6 (2.6) | 7.8 (2.5) | 6.2 (3.2) |
| 5. I feel less anxious | 7.4 (2.8) | 7.7 (2.6) | 5.5 (3.7) |
| 6. I feel less down or depressed | 7.3 (2.7) | 7.6 (2.5) | 5.8 (3.8) |
| 7. I feel less alone | 7.6 (2.7) | 7.9 (2.5) | 5.8 (3.7) |
| 8. I feel that my peer navigator cares about me | 8.0 (2.5) | 8.1 (2.5) | 7.6 (2.3) |
| 9. I feel more hopeful about the road ahead | 7.4 (2.6) | 7.6 (2.6) | 6.3 (2.6) |
| Validation Support | 7.8 (2.4) | 8 (2.3) | 6.5 (2.6) |
| 10. I feel that my peer navigator and I have a similar understanding | 7.6 (2.6) | 7.8 (2.6) | 6.5 (2.5) |
| 11. I feel that my peer navigator understands me | 7.8 (2.6) | 7.9 (2.7) | 6.8 (2.5) |
| 12. I feel that my peer navigator listens to me and is interested in what I have to say | 8.1 (2.3) | 8.1 (2.3) | 8 (2.4) |
| 13. I feel less anxious talking to someone who has been in my shoes | 7.7 (2.4) | 8 (2.2) | 5.3 (2.9) |
| 14. I feel that my thoughts and feelings are normal | 8.1 (2.1) | 8.3 (1.8) | 6 (2.9) |
| Autonomy Support | 7.5 (2.5) | 7.7 (2.3) | 6.1 (3.6) |
| 15. I have found new ways of looking at my situation | 7.4 (2.4) | 7.4 (2.2) | 7 (3.8) |
| 16. I feel more in control | 7.4 (2.3) | 7.4 (2.1) | 7 (3.8) |
| 17. I feel more assured and comfortable with my choice of treatment | 7.8 (2.3) | 7.9 (2.1) | 6.8 (3.9) |
| 18. I feel more confident that I can manage emotional distress | 7.3 (2.7) | 7.7 (2.4) | 4.5 (3.4) |
| 19. I feel more confident talking to my healthcare provider about my concerns | 7.7 (2.5) | 7.8 (2.4) | 6.5 (3.7) |
| 20. I feel more confident coping with my cancer | 7.4 (2.6) | 7.7 (2.3) | 4.8 (3.1) |
| Variable | Pre-Test Mean (SD) | Post-Test Mean (SD) | Mean Difference (SE) | Paired t-Test | p-Value | |
|---|---|---|---|---|---|---|
| Patient/Caregiver Activation (PAM-PT/CG), | ||||||
| Patient (n = 28) | 62.2 (20.93) | 74.06 (16.45) | −11.86 (3.87) | −3.1 | <0.01 * | |
| Caregiver (n = 4) | 51.38 (8.22) | 59.3 (6.45) | −7.93 (1.65) | −4.79 | 0.02 * | |
| Total (n = 34) | 60.84 (20.03) | 72.2 (16.2) | −11.37 (3.39) | −3.4 | <0.01 * | |
| Health Quality of Life (EQ5D-5L) | ||||||
| Patient (n = 29) | 0.85 (0.1) | 0.87 (0.14) | −0.02 (0.02) | −0.78 | 0.45 | |
| Caregiver (n = 5) | 0.87 (0.08) | 0.87 (0.1) | −0.01 (0.06) | −0.1 | 0.93 | |
| Total (n = 34) | 0.8 (0.1) | 0.9 (0.1) | −0.1 (0.1) | −0.8 | 0.45 | |
| PC Quality of Life (PORPUS) | ||||||
| Patient (n =28) | 97.1 (1.39) | 98.23 (0.99) | −1.13 (0.2) | −5.6 | <0.01 * | |
| Anxiety (HADS-Anxiety) | ||||||
| Patient (n = 29) | 4.97 (3.31) | 4.66 (3.93) | 0.31 (0.52) | 0.6 | 0.55 | |
| Caregiver (n = 5) | 9.6 (5.32) | 9.4 (6.02) | 0.2 (1.53) | 0.13 | 0.9 | |
| Total (n = 34) | 5.6 (3.9) | 5.3 (4.5) | 0.3 (0.48) | 0.6 | 0.55 | |
| Depression (HADS-Depression) | ||||||
| Patient (n = 29) | 2.59 (2.31) | 3.31 (3.5) | −0.72 (0.46) | −1.57 | 0.13 | |
| Caregiver (n = 5) | 7 (3.94) | 6.2 (5.22) | 0.8 (1.83) | 0.44 | 0.68 | |
| Total (n = 34) | 3.2 (3.0) | 3.7 (3.8) | −0.5 (0.47) | −1.1 | 0.29 | |
| Social Support (ESSI) | ||||||
| Patient | ||||||
| Total (n = 29) | 28.35 (4.92) | 29.24 (5.11) | −0.9 (0.88) | −1.02 | 0.32 | |
| Informational (n = 29) | 3.62 (0.94) | 4.07 (0.88) | −0.45 (0.19) | −2.37 | 0.03 * | |
| Practical (n = 28) | 3.93 (1.33) | 4.21 (1.29) | −0.29 (0.26) | −1.11 | 0.28 | |
| Caregiver (n = 5) | ||||||
| Total | 19.8 (7.4) | 23.2 (8.44) | −3.4 (1.57) | −2.17 | 0.1 | |
| Informational | 2.8 (1.48) | 2.8 (1.48) | 0 (0.32) | 0 | 1 | |
| Practical | 1.2 (0.84) | 3 (1.41) | −1.8 (0.49) | −3.67 | 0.02 * | |
| Total, n = 34 | 27.1 (6.0) | 28.3 (5.9) | −1.2 (0.79) | −1.6 | 0.12 | |
| Informational Support, n = 34 | 3.50 (1.0) | 3.9 (1.1) | −0.4 (0.17) | −2.3 | 0.03 * | |
| Practical Support, n = 34 | 3.51 (1.6) | 4.0 (1.3) | −0.5 (0.25) | −2.1 | 0.045 * | |
| Supportive Care Needs | ||||||
| Patient | Total Met Needs, n = 28 | 30.0 (11.1) | 31.9 (10.5) | −1.9 (2.4) | −0.8 | 0.45 |
| Total Unmet Needs, n = 28 | 11.7 (11.1) | 9.9 (10.3) | 1.8 (2.4) | 0.7 | 0.47 | |
| Fear of Recurrence Unmet Need, n = 28 | 1.5 (1.3) | 1.1 (1.0) | 0.4 (0.19) | 2.3 | 0.03 * | |
| Caregiver | Total Met Needs, n = 5 | 19.0 (10.9) | 27.0 (13.5) | −8 (3.0) | −2.6 | 0.05 * |
| Total Unmet Needs, n = 5 | 25.8 (10.8) | 18.0 (13.5) | 7.8 (3.0) | 2.6 | 0.06 | |
| Support to look after own health Unmet Need, n = 5 | 3.6 (0.5) | 1.6 (1.3) | 2. (0.55) | 3.6 | 0.02 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bender, J.L.; Flora, P.K.; Soheilipour, S.; Dirlea, M.; Maharaj, N.; Parvin, L.; Matthew, A.; Catton, C.; Jamnicky, L.; Pollock, P.; et al. Web-Based Peer Navigation for Men with Prostate Cancer and Their Family Caregivers: A Pilot Feasibility Study. Curr. Oncol. 2022, 29, 4285-4299. https://doi.org/10.3390/curroncol29060343
Bender JL, Flora PK, Soheilipour S, Dirlea M, Maharaj N, Parvin L, Matthew A, Catton C, Jamnicky L, Pollock P, et al. Web-Based Peer Navigation for Men with Prostate Cancer and Their Family Caregivers: A Pilot Feasibility Study. Current Oncology. 2022; 29(6):4285-4299. https://doi.org/10.3390/curroncol29060343
Chicago/Turabian StyleBender, Jacqueline L., Parminder K. Flora, Shimae Soheilipour, Mihaela Dirlea, Nandini Maharaj, Lisa Parvin, Andrew Matthew, Charles Catton, Leah Jamnicky, Philip Pollock, and et al. 2022. "Web-Based Peer Navigation for Men with Prostate Cancer and Their Family Caregivers: A Pilot Feasibility Study" Current Oncology 29, no. 6: 4285-4299. https://doi.org/10.3390/curroncol29060343
APA StyleBender, J. L., Flora, P. K., Soheilipour, S., Dirlea, M., Maharaj, N., Parvin, L., Matthew, A., Catton, C., Jamnicky, L., Pollock, P., Kwan, W., Finelli, A., & Kazanjian, A. (2022). Web-Based Peer Navigation for Men with Prostate Cancer and Their Family Caregivers: A Pilot Feasibility Study. Current Oncology, 29(6), 4285-4299. https://doi.org/10.3390/curroncol29060343






