Radiotherapy or Surgery? Comparative, Qualitative Assessment of Online Patient Education Materials on Prostate Cancer
Abstract
:1. Introduction
2. Materials and Methods
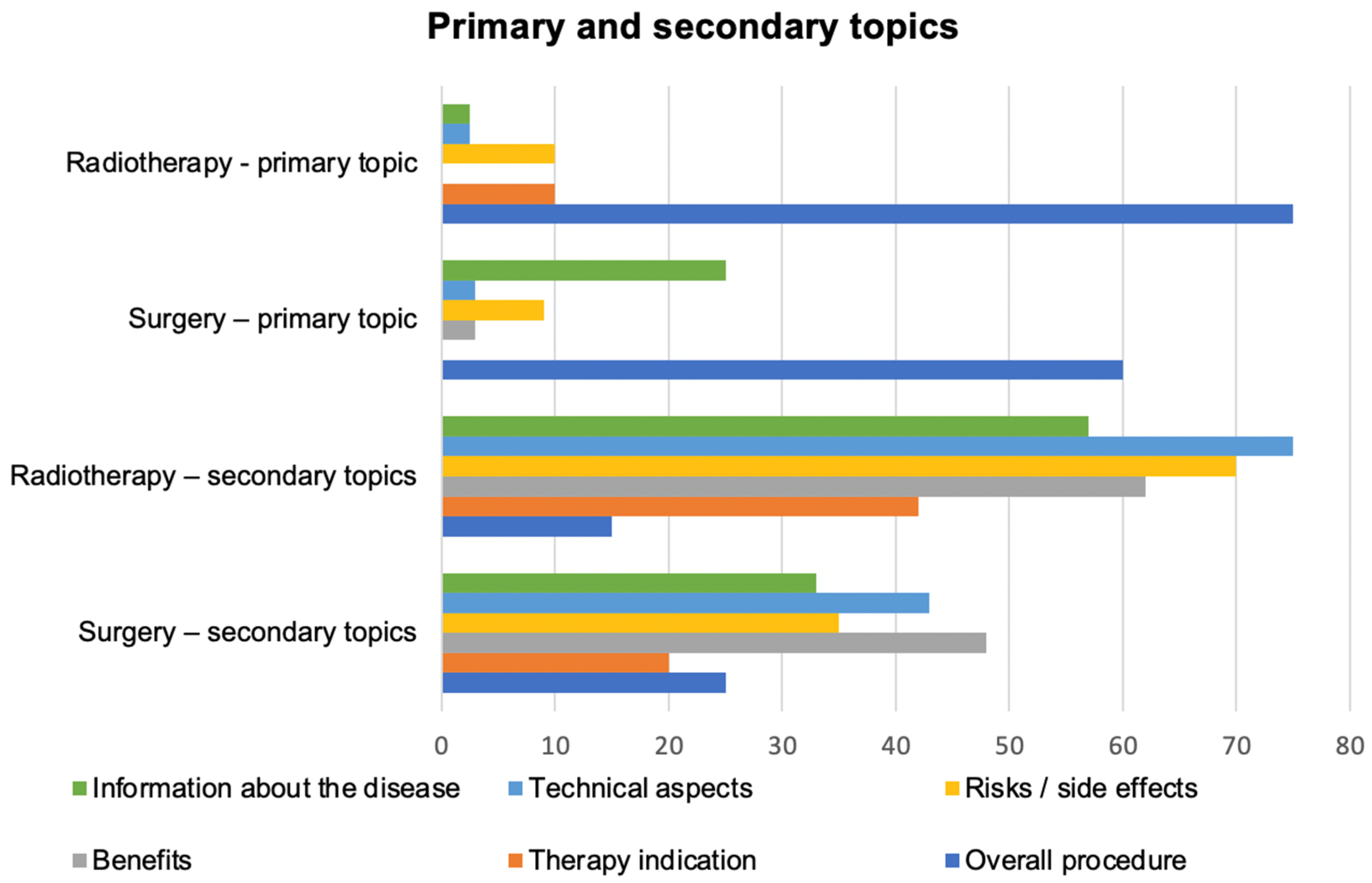
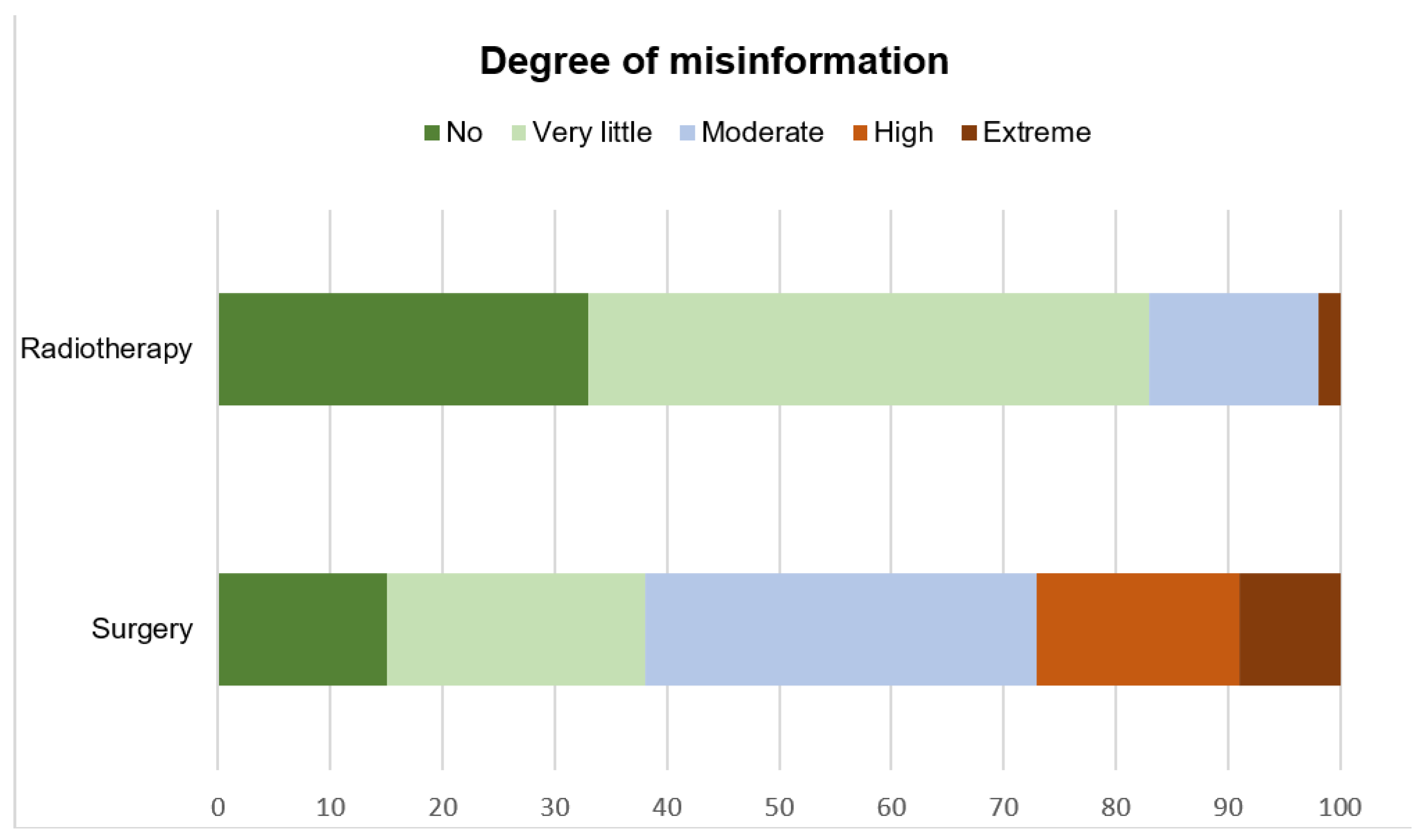
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Culp, M.B.B.; Soerjomataram, I.; Efstathiou, J.A.; Bray, F.; Jemal, A. Recent global patterns in prostate cancer incidence and mortality rates. Eur. Urol. 2020, 77, 38–52. [Google Scholar] [CrossRef]
- Mottet, N.; van den Bergh, R.C.; Briers, E.; van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on prostate cancer—2020 Update. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur. Urol. 2020, 79, 243–262. [Google Scholar] [CrossRef]
- Cornford, P.; van den Bergh, R.C.; Briers, E.; van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S.; et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on prostate cancer. Part II—2020 Update: Treatment of relapsing and metastatic prostate cancer. Eur. Urol. 2021, 79, 263–282. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-S.; Sul, C.-K.; Song, K.-H.; Na, Y.-G.; Shin, J.H.; Oh, T.-H.; Kim, Y.-H. Changes in urinary symptoms and tolerance due to long-term ureteral double-j stenting. Int. Neurourol. J. 2010, 14, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Donovan, J.L.; Hamdy, F.C.; Lane, J.A.; Mason, M.; Metcalfe, C.; Walsh, E.; Blazeby, J.; Peters, T.; Holding, P.; Bonnington, S.; et al. Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N. Engl. J. Med. 2016, 375, 1425–1437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wallis, C.J.; Saskin, R.; Choo, R.; Herschorn, S.; Kodama, R.T.; Satkunasivam, R.; Shah, P.S.; Danjoux, C.; Nam, R.K. Surgery versus radiotherapy for clinically-localized prostate cancer: A systematic review and meta-analysis. Eur. Urol. 2016, 70, 21–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinberg, P.L.; Wason, S.; Stern, J.M.; Deters, L.; Kowal, B.; Seigne, J. YouTube as source of prostate cancer information. Urology 2010, 75, 619–622. [Google Scholar] [CrossRef]
- Betschart, P.; Pratsinis, M.; Müllhaupt, G.; Rechner, R.; Herrmann, T.R.; Gratzke, C.; Schmid, H.-P.; Zumstein, V.; Abt, D. Information on surgical treatment of benign prostatic hyperplasia on YouTube is highly biased and misleading. BJU Int. 2020, 125, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Sood, A.; Sarangi, S.; Pandey, A.; Murugiah, K. YouTube as a source of information on kidney stone disease. Urology 2011, 77, 558–562. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Pei, S.; Chen, B.; Song, Y.; Zhang, T.; Yang, W.; Shaman, J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science 2020, 368, 489–493. [Google Scholar] [CrossRef] [Green Version]
- Schrag, D.; Hershman, D.L.; Basch, E. Oncology practice during the COVID-19 pandemic. JAMA 2020, 323, 2005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jazieh, A.R.; Akbulut, H.; Curigliano, G.; Rogado, A.; Alsharm, A.A.; Razis, E.D.; Mula-Hussain, L.; Errihani, H.; Khattak, A.; De Guzman, R.B.; et al. Impact of the COVID-19 pandemic on cancer care: A global collaborative study. JCO Glob. Oncol. 2020, 6, 1428–1438. [Google Scholar] [CrossRef] [PubMed]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef] [PubMed]
- Spolverato, G.; Capelli, G.; Restivo, A.; Bao, Q.R.; Pucciarelli, S.; Pawlik, T.M.; Gronchi, A. The management of surgical patients during the coronavirus disease 2019 (COVID-19) pandemic. Surgery 2020, 168, 4–10. [Google Scholar] [CrossRef]
- Shoemaker, S.J.; Wolf, M.S.; Brach, C. Development of the patient education materials assessment tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Educ. Couns. 2014, 96, 395–403. [Google Scholar] [CrossRef] [Green Version]
- Moorhead, S.A.; Hazlett, D.E.; Harrison, L.; Carroll, J.K.; Irwin, A.; Hoving, C. A new dimension of health care: Systematic review of the uses, benefits, and limitations of social media for health communication. J. Med. Internet Res. 2013, 15, e85. [Google Scholar] [CrossRef] [Green Version]
- Dutta, A.; Beriwal, N.; Van Breugel, L.M.; Sachdeva, S.; Barman, B.; Saikia, H.; Nelson, U.-A.; Mahdy, A.; Paul, S. YouTube as a source of medical and epidemiological information during COVID-19 pandemic: A cross-sectional study of content across six languages around the globe. Cureus 2020, 12, e8622. [Google Scholar] [CrossRef]
- Charnock, D.; Shepperd, S.; Needham, G.; Gann, R. DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. J. Epidemiol. Community Health 1999, 53, 105–111. [Google Scholar] [CrossRef] [Green Version]
- Dahn, J.R.; Penedo, F.J.; Gonzalez, J.S.; Esquiabro, M.; Antoni, M.H.; Roos, B.A.; Schneiderman, N. Sexual functioning and quality of life after prostate cancer treatment: Considering sexual desire. Urology 2004, 63, 273–277. [Google Scholar] [CrossRef]
- Posielski, N.; Frankel, J.; Kuo, H.-C.; Ho, O.; Elsamanoudi, S.; Nousome, D.; Speir, R.; Stroup, S.; Musser, J.; Ernest, A.; et al. Impact of age and race on health-related quality of life outcomes in patients undergoing radical prostatectomy for localized prostate cancer. Urology 2021, 7, 34. [Google Scholar] [CrossRef]
- Kaicker, J.; Wu, K.; Athreya, S. Assessing the reliability and quality of online uterine fibroid embolization resources. Cardiovasc. Interv. Radiol. 2012, 36, 385–394. [Google Scholar] [CrossRef]
- Vishnevetsky, J.; Walters, C.B.; Tan, K.S. Interrater reliability of the patient education materials assessment tool (PEMAT). Patient Educ. Couns. 2018, 101, 490–496. [Google Scholar] [CrossRef]
- Mohler, J.; Bahnson, R.R.; Boston, B.; Busby, J.E.; D’Amico, A.; Eastham, J.A.; Enke, C.A.; George, D.; Horwitz, E.M.; Huben, R.P.; et al. NCCN clinical practice guidelines in oncology: Prostate cancer. J. Natl. Compr. Canc. Netw. 2010, 8, 162–200. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, A.V.; Manola, J.; Loffredo, M.; Renshaw, A.A.; DellaCroce, A.; Kantoff, P.W. 6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer: A randomized controlled trial. JAMA 2004, 292, 821–827. [Google Scholar] [CrossRef] [Green Version]
- Sanda, M.G.; Dunn, R.L.; Michalski, J.; Sandler, H.M.; Northouse, L.; Hembroff, L.; Lin, X.; Greenfield, T.K.; Litwin, M.S.; Saigal, C.S.; et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N. Engl. J. Med. 2008, 358, 1250–1261. [Google Scholar] [CrossRef]
- Albertsen, P.C.; Hanley, J.A.; Fine, J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 2005, 293, 2095–2101. [Google Scholar] [CrossRef] [Green Version]
- Stephenson, A.J.; Kattan, M.W.; Eastham, J.A.; Bianco, F.J., Jr.; Yossepowitch, O.; Vickers, A.J.; Klein, E.A.; Wood, D.P.; Scardino, P.T. Prostate cancer–Specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J. Clin. Oncol. 2009, 27, 4300–4305. [Google Scholar] [CrossRef] [Green Version]
- Hu, J.C.; Gu, X.; Lipsitz, S.R.; Barry, M.J.; D’Amico, A.V.; Weinberg, A.C.; Keating, N.L. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA 2009, 302, 1557–1564. [Google Scholar] [CrossRef] [PubMed]
- Hardcastle, N.; Tomé, W.A.; Foo, K.; Miller, A.; Carolan, M.; Metcalfe, P. Comparison of prostate IMRT and VMAT biologically optimised treatment plans. Med. Dosim. 2011, 36, 292–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel Coronavirus from patients with pneumonia in China. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. COVID-19—Implications for the health care system. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef]
- Lal, A.; Erondu, N.A.; Heymann, D.L.; Gitahi, G.; Yates, R. Fragmented health systems in COVID-19: Rectifying the misalignment between global health security and universal health coverage. Lancet 2021, 397, 61–67. [Google Scholar] [CrossRef]
- Stensland, K.D.; Morgan, T.M.; Moinzadeh, A.; Lee, C.T.; Briganti, A.; Catto, J.W.; Canes, D. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur. Urol. 2020, 77, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Ribal, M.J.; Cornford, P.; Briganti, A.; Knoll, T.; Gravas, S.; Babjuk, M.; Harding, C.; Breda, A.; Bex, A.; Rassweiler, J.J.; et al. European association of urology guidelines office rapid reaction group: An organisation-wide collaborative effort to adapt the european association of urology guidelines recommendations to the Coronavirus disease 2019 Era. Eur. Urol. 2020, 78, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Roach, M.; Moughan, J.; Lawton, C.A.F.; Dicker, A.P.; Zeitzer, K.L.; Gore, E.M.; Kwok, Y.; Seider, M.J.; Hsu, I.-C.; Hartford, A.C.; et al. Sequence of hormonal therapy and radiotherapy field size in unfavourable, localised prostate cancer (NRG/RTOG 9413): Long-term results of a randomised, phase 3 trial. Lancet Oncol. 2018, 19, 1504–1515. [Google Scholar] [CrossRef]
- Dee, E.C.; Mahal, B.A.; Arega, M.A.; D’Amico, A.V.; Mouw, K.W.; Nguyen, P.L.; Muralidhar, V. Relative timing of radiotherapy and androgen deprivation for prostate cancer and implications for treatment during the COVID-19 pandemic. JAMA Oncol. 2020, 6, 1630–1632. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.-Y.; Desai, A.; Lopes, G.D.L.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Ueda, M.; Martins, R.; Hendrie, P.C.; McDonnell, T.; Crews, J.R.; Wong, T.L.; McCreery, B.; Jagels, B.; Crane, A.; Byrd, D.R.; et al. Managing cancer care during the COVID-19 pandemic: Agility and collaboration toward a common goal. J. Natl. Compr. Cancer Netw. 2020, 18, 366–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S.; et al. Shared decision making: A model for clinical practice. J. Gen. Intern. Med. 2012, 27, 1361–1367. [Google Scholar] [CrossRef] [Green Version]
- Page, A.E. Safety in surgery: The role of shared decision-making. Patient Saf. Surg. 2015, 9, 24. [Google Scholar] [CrossRef] [Green Version]
- European Association of Urology YouTube Channel. Available online: https://www.youtube.com/channel/UCuBt1xdv2n7GPawh7lcqDRA (accessed on 1 March 2021).
- American Urology Association YouTube Channel. Available online: https://www.youtube.com/user/AmerUrological (accessed on 1 March 2021).
- American Society for Radiation Oncology YouTube Channel. Available online: https://www.youtube.com/user/ASTROTargetingCancer (accessed on 1 March 2021).
- Pratsinis, M.; Abt, D.; Müllhaupt, G.; Langenauer, J.; Knoll, T.; Schmid, H.-P.; Zumstein, V.; Betschart, P. Systematic assessment of information about surgical urinary stone treatment on YouTube. World J. Urol. 2021, 39, 935–942. [Google Scholar] [CrossRef] [PubMed]
- Tanwar, R.; Khattar, N.; Sood, R.; Makkar, A. Benign prostatic hyperplasia related content on YouTube: Unregulated and concerning. Recenti Prog Med. 2015, 106, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.Y.; Hevelone, N.D.; Lipsitz, S.R.; Kowalczyk, K.J.; Hu, J.C. Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J. Urol. 2012, 187, 1392–1398. [Google Scholar] [CrossRef] [PubMed]
| . | Range of Upload (Month/Year) | Median Length of Video (min:s) | Median No. of Views | Median Thumbs Up | Median Thumbs Down | Median No. of Comments | Median Audio Quality [1 (Bad)–5 (Excellent)] | Median Video Quality [1 (Bad)–5 (Excellent)] |
|---|---|---|---|---|---|---|---|---|
| Radiotherapy | 11/2008–09/2019 | 06:30 [1:37–31:00] | 20′848 [8077–1′291′081] | 355 [20–640] | 292.5 [3–582] | 12 [3–21] | 3.5 [3–4] | 4 [3–5] |
| Surgery | 02/2008–09/2019 | 04:04 [00:35–10:54] | 33′123 [13′942–4′986′282] | 119.5 [6–8400] | 10.5 [0–1700] | 13 [0–326] | 5 [2–5] | 5 [2–5] |
| DISCERN Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Radiotherapy | 4 | 3.5 | 3.25 | 3 | 2.5 | 2 | 2.25 | 2 | 2.5 | 2.5 | 3 | 1.5 | 2.5 | 2.75 | 3 | 3 |
| [2–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–4.5] | [1–5] | [1–0.5] | [1–5] | [1–5] | [1–5] | [1–5] | |
| Surgery | 3 | 3 | 2.5 | 2 | 2 | 3 | 2 | 2.5 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 |
| [2–5] | [2–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] | [1–5] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, E.; Pratsinis, M.; Plasswilm, L.; Schmid, H.-P.; Panje, C.; Betschart, P. Radiotherapy or Surgery? Comparative, Qualitative Assessment of Online Patient Education Materials on Prostate Cancer. Curr. Oncol. 2021, 28, 3420-3429. https://doi.org/10.3390/curroncol28050296
Vu E, Pratsinis M, Plasswilm L, Schmid H-P, Panje C, Betschart P. Radiotherapy or Surgery? Comparative, Qualitative Assessment of Online Patient Education Materials on Prostate Cancer. Current Oncology. 2021; 28(5):3420-3429. https://doi.org/10.3390/curroncol28050296
Chicago/Turabian StyleVu, Erwin, Manolis Pratsinis, Ludwig Plasswilm, Hans-Peter Schmid, Cédric Panje, and Patrick Betschart. 2021. "Radiotherapy or Surgery? Comparative, Qualitative Assessment of Online Patient Education Materials on Prostate Cancer" Current Oncology 28, no. 5: 3420-3429. https://doi.org/10.3390/curroncol28050296
APA StyleVu, E., Pratsinis, M., Plasswilm, L., Schmid, H.-P., Panje, C., & Betschart, P. (2021). Radiotherapy or Surgery? Comparative, Qualitative Assessment of Online Patient Education Materials on Prostate Cancer. Current Oncology, 28(5), 3420-3429. https://doi.org/10.3390/curroncol28050296





