The Role of the Sol-Gel Synthesis Process in the Biomedical Field and Its Use to Enhance the Performance of Bioabsorbable Magnesium Implants
Abstract
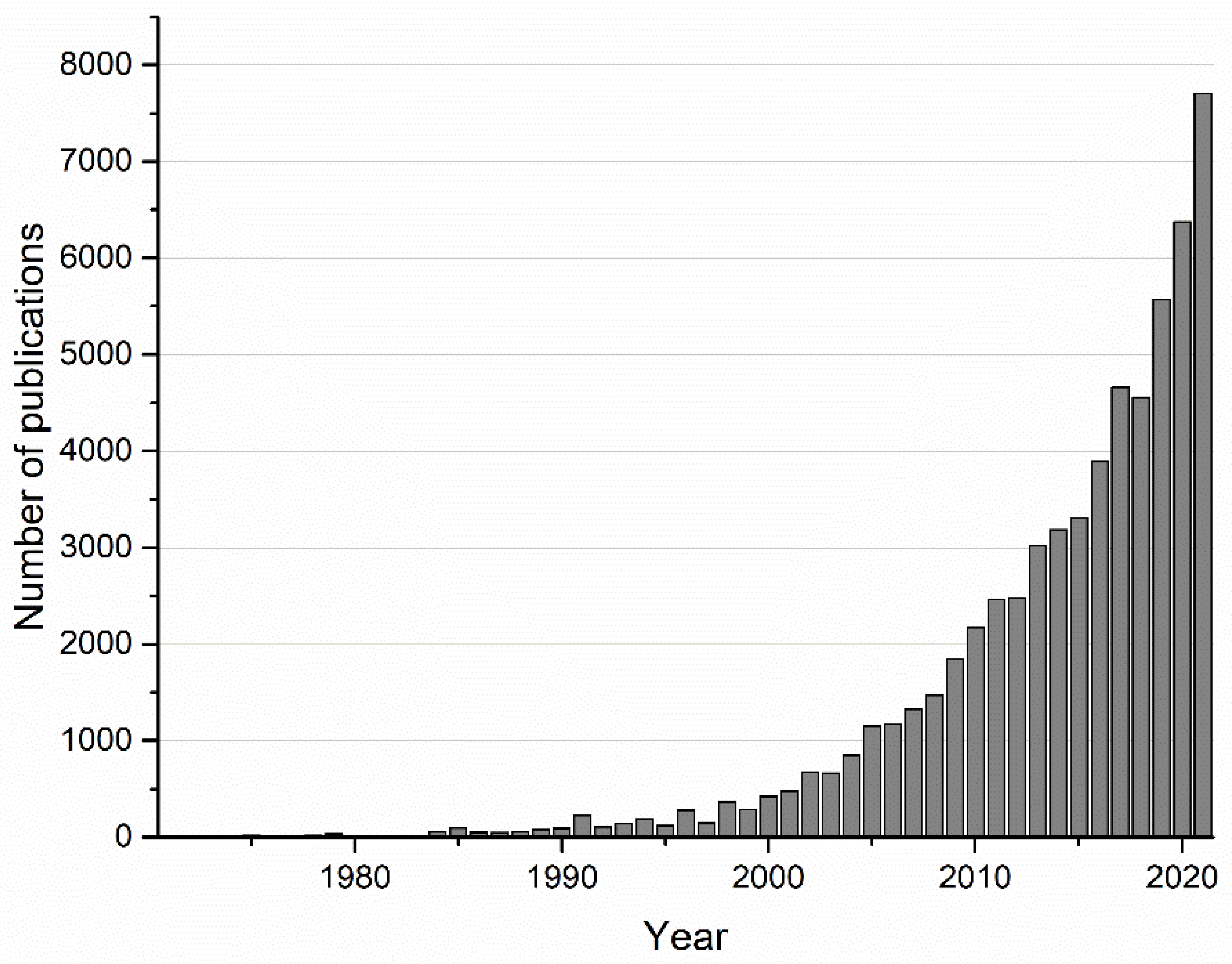
:1. Introduction
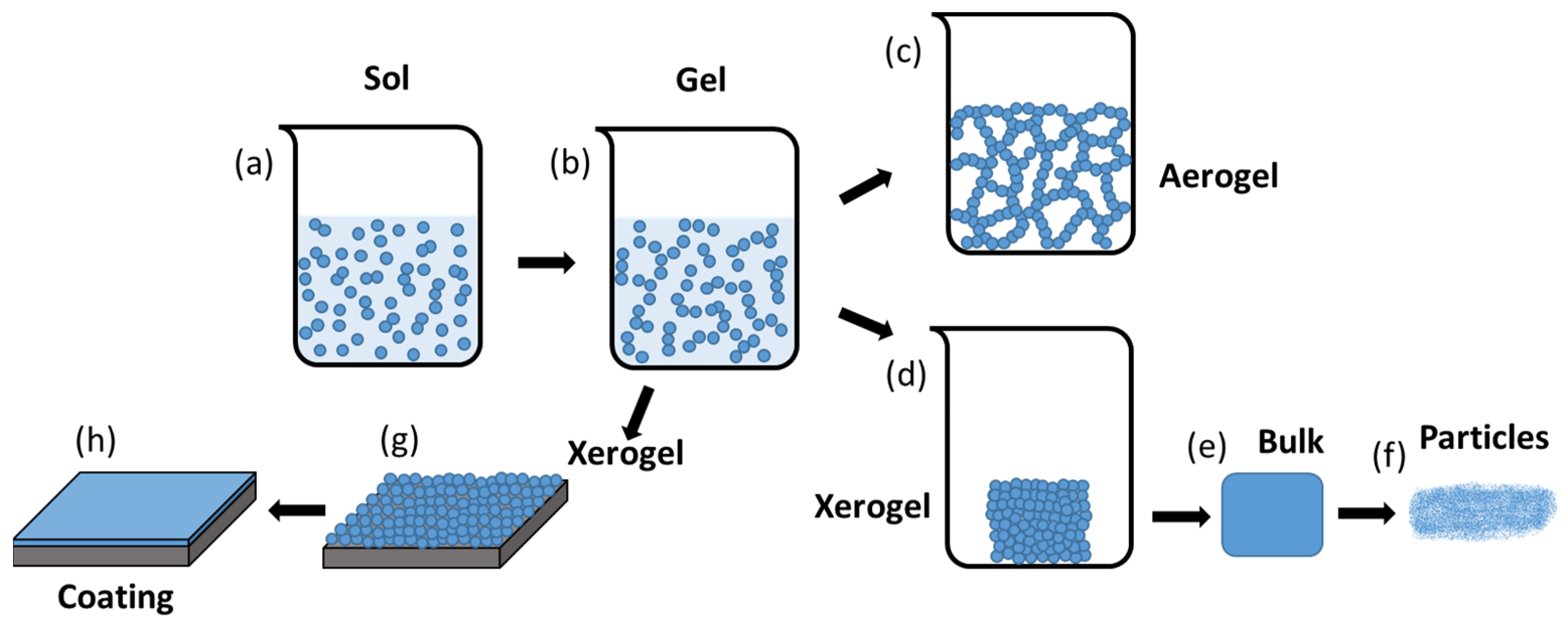
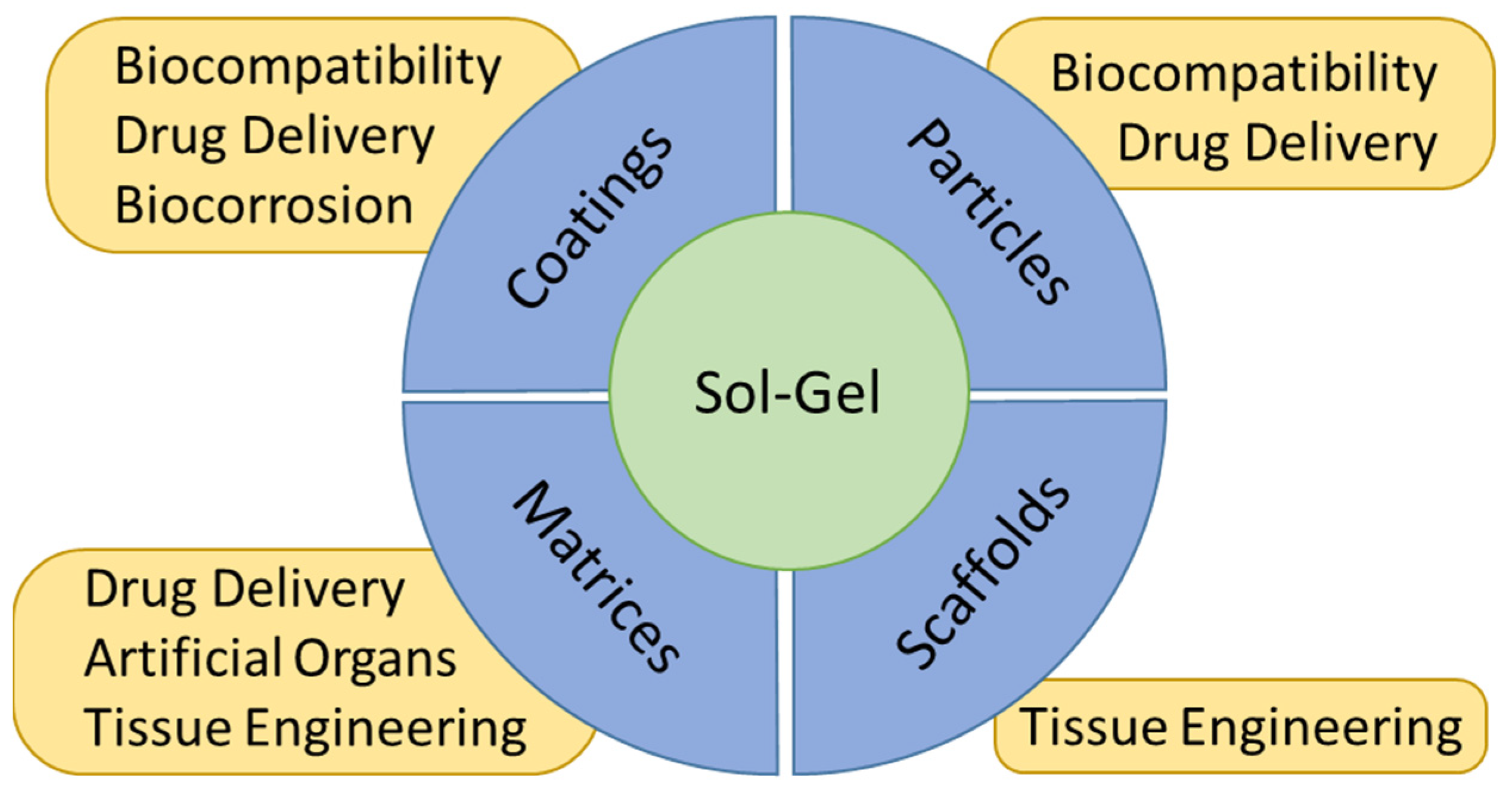
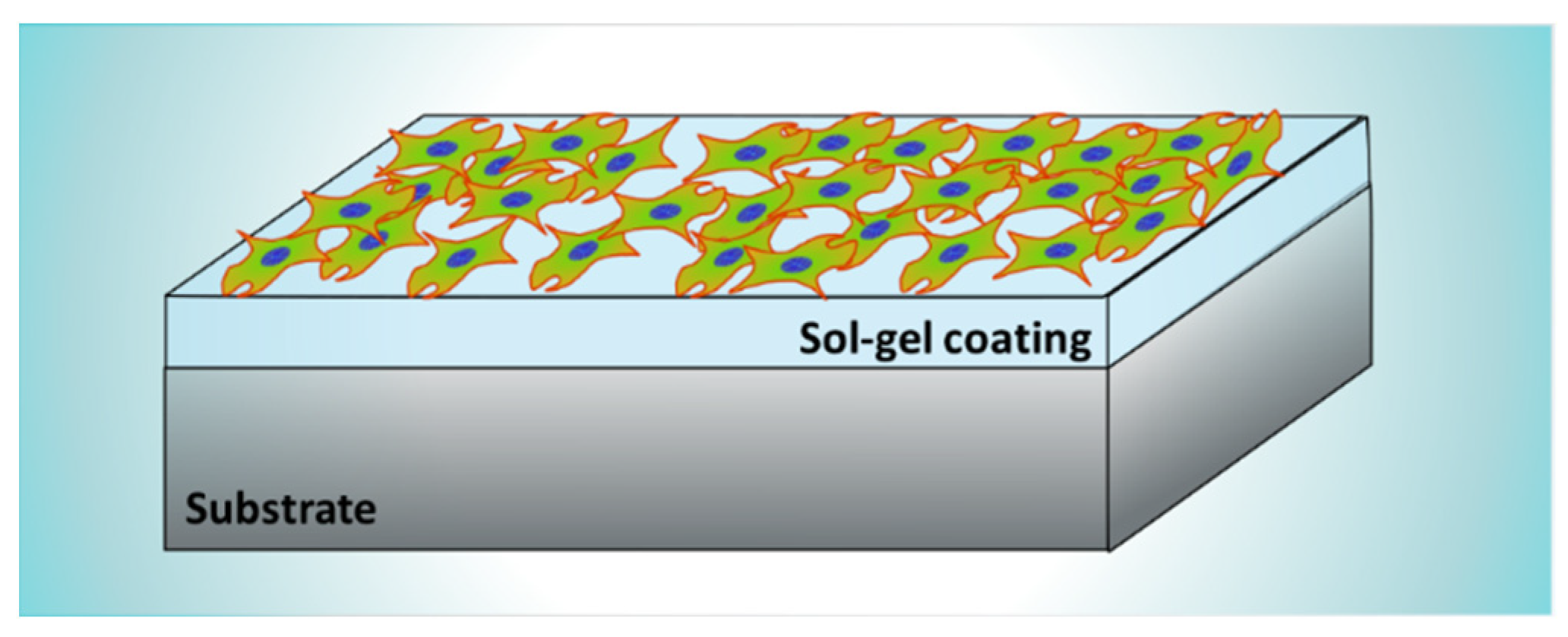
2. Sol-Gel Coatings for Biomedical Applications
2.1. General Considerations
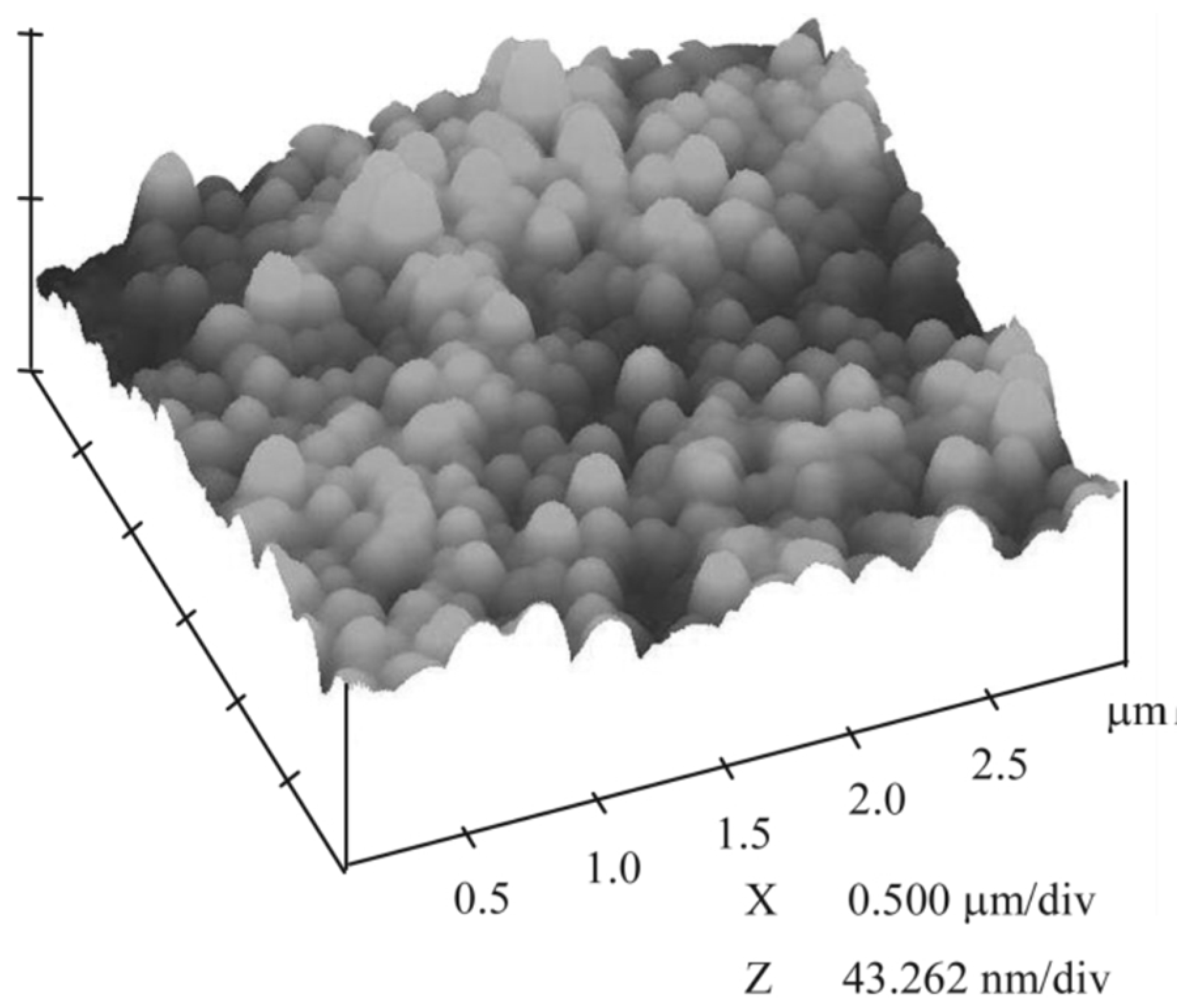
2.2. Coatings for Biocompatibility Improvement
2.3. Coatings for Biocorrosion Protection
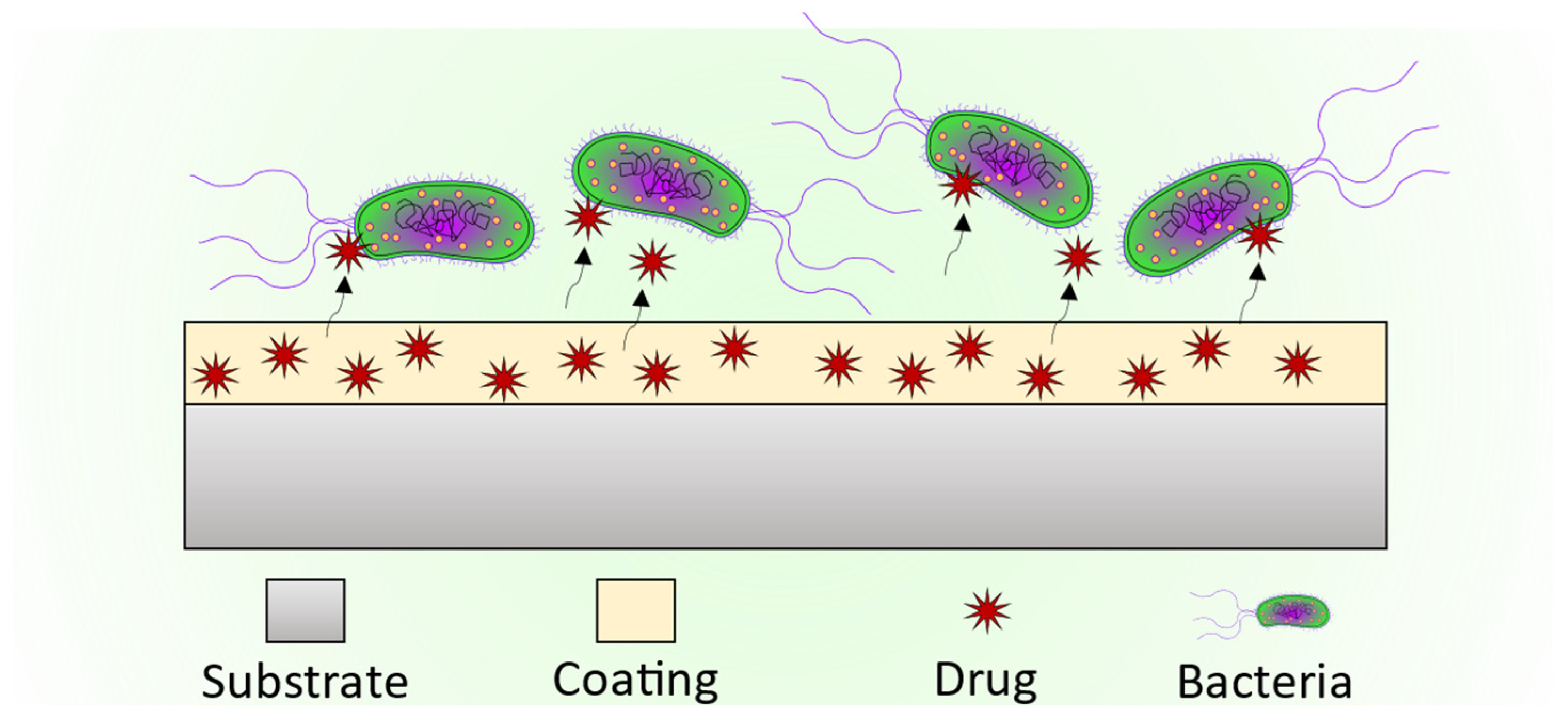
2.4. Coatings as Drug Delivery Systems
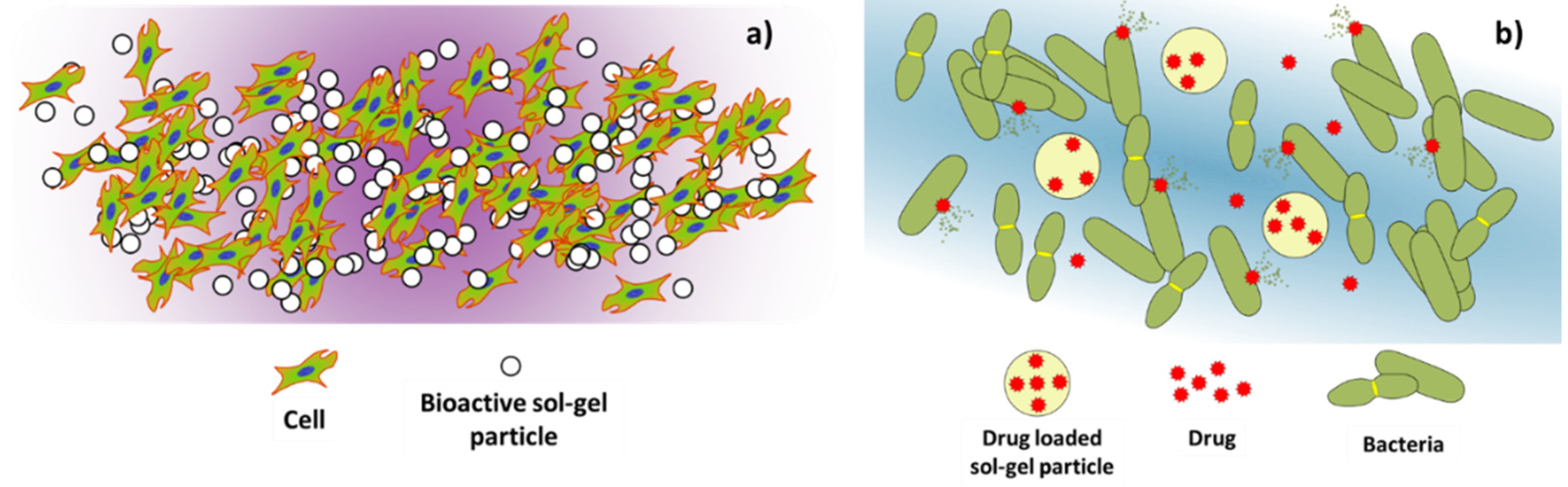
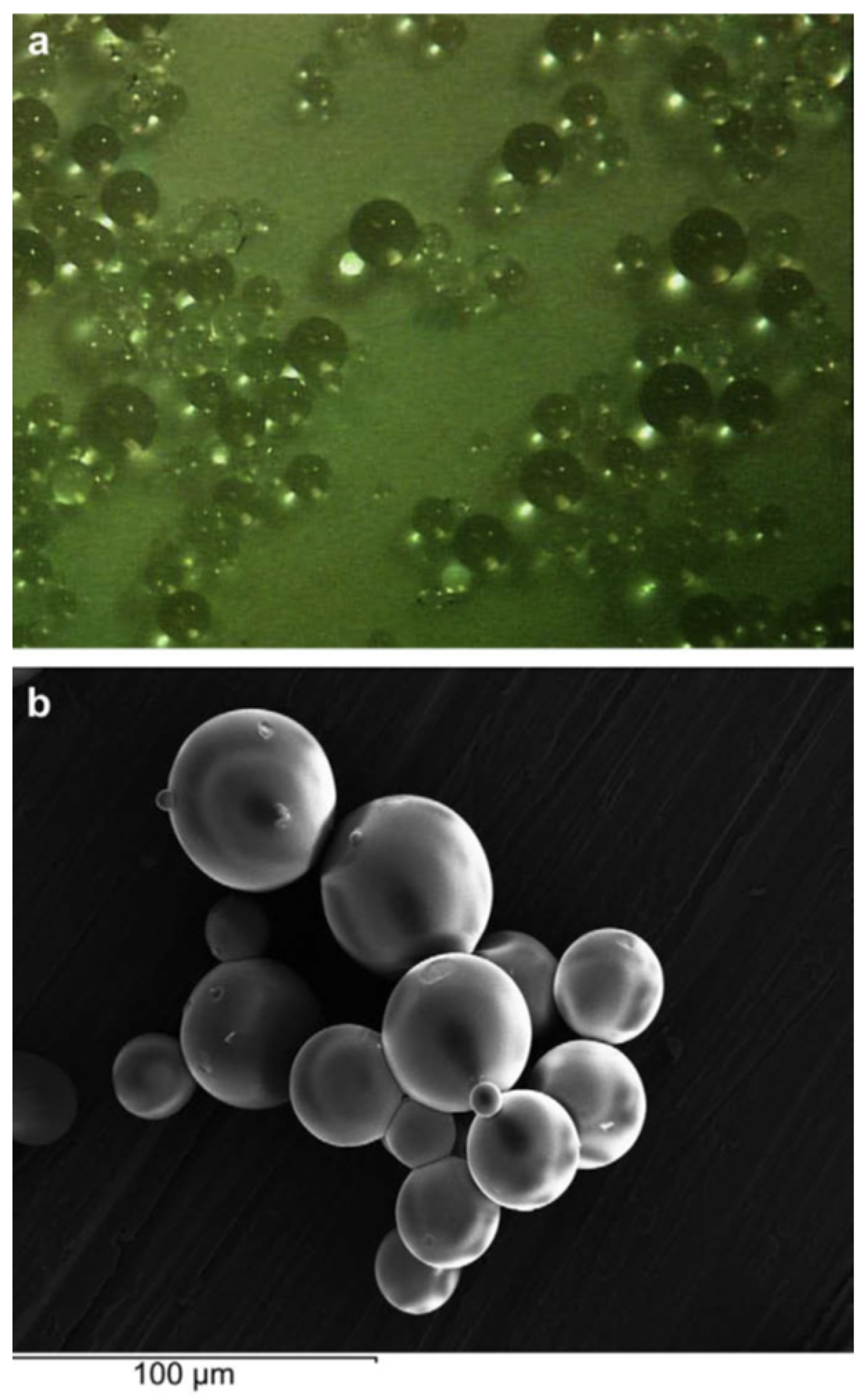
3. Sol-Gel Particles for Biomedical Applications
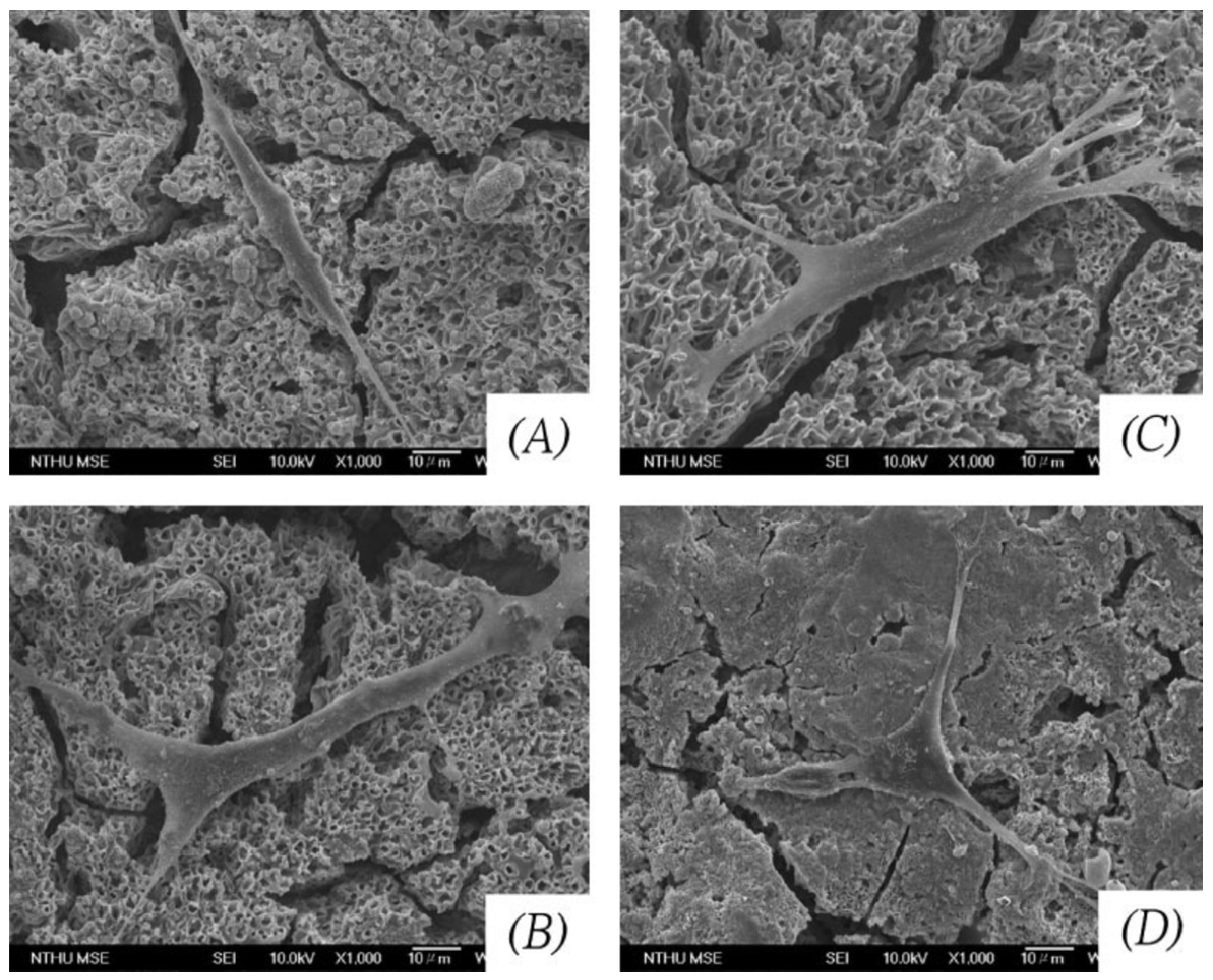
3.1. Particles for Biocompatibility Improvement

3.2. Particles as Drug Delivery Systems
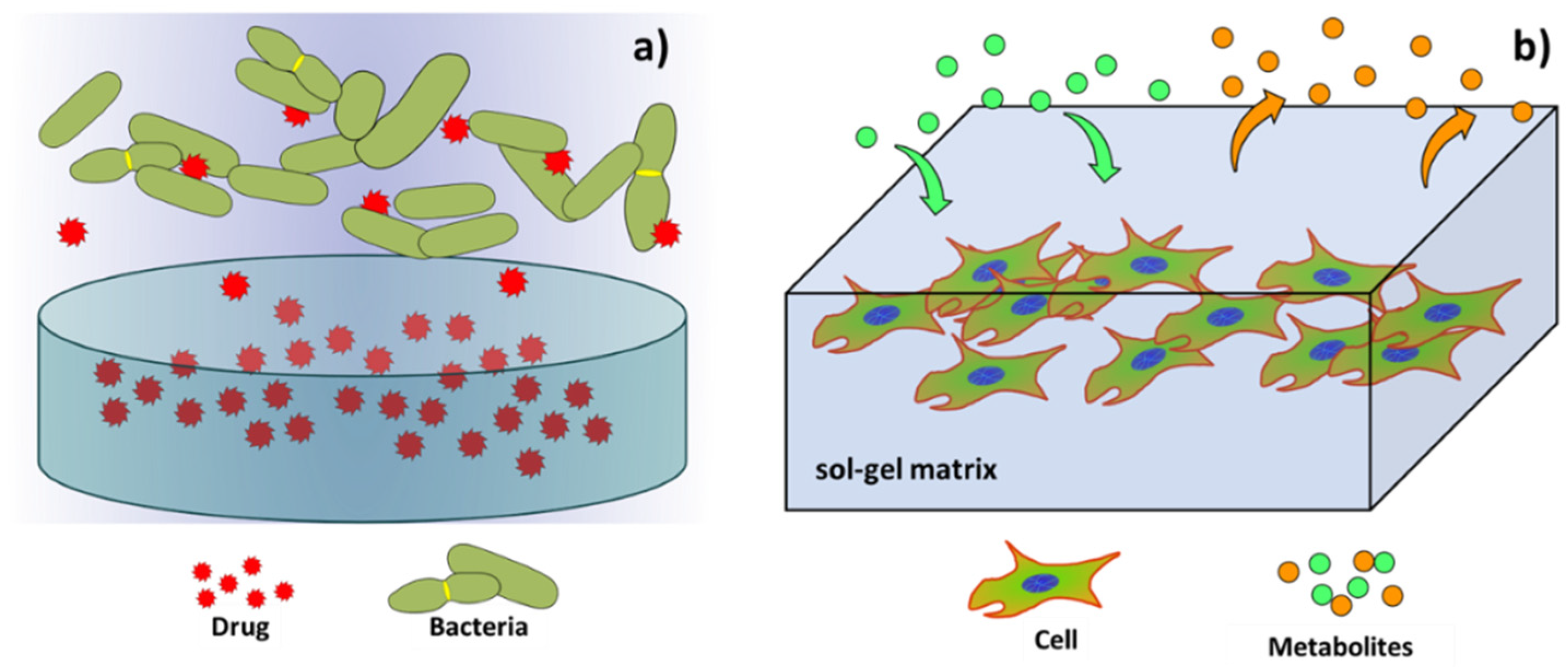
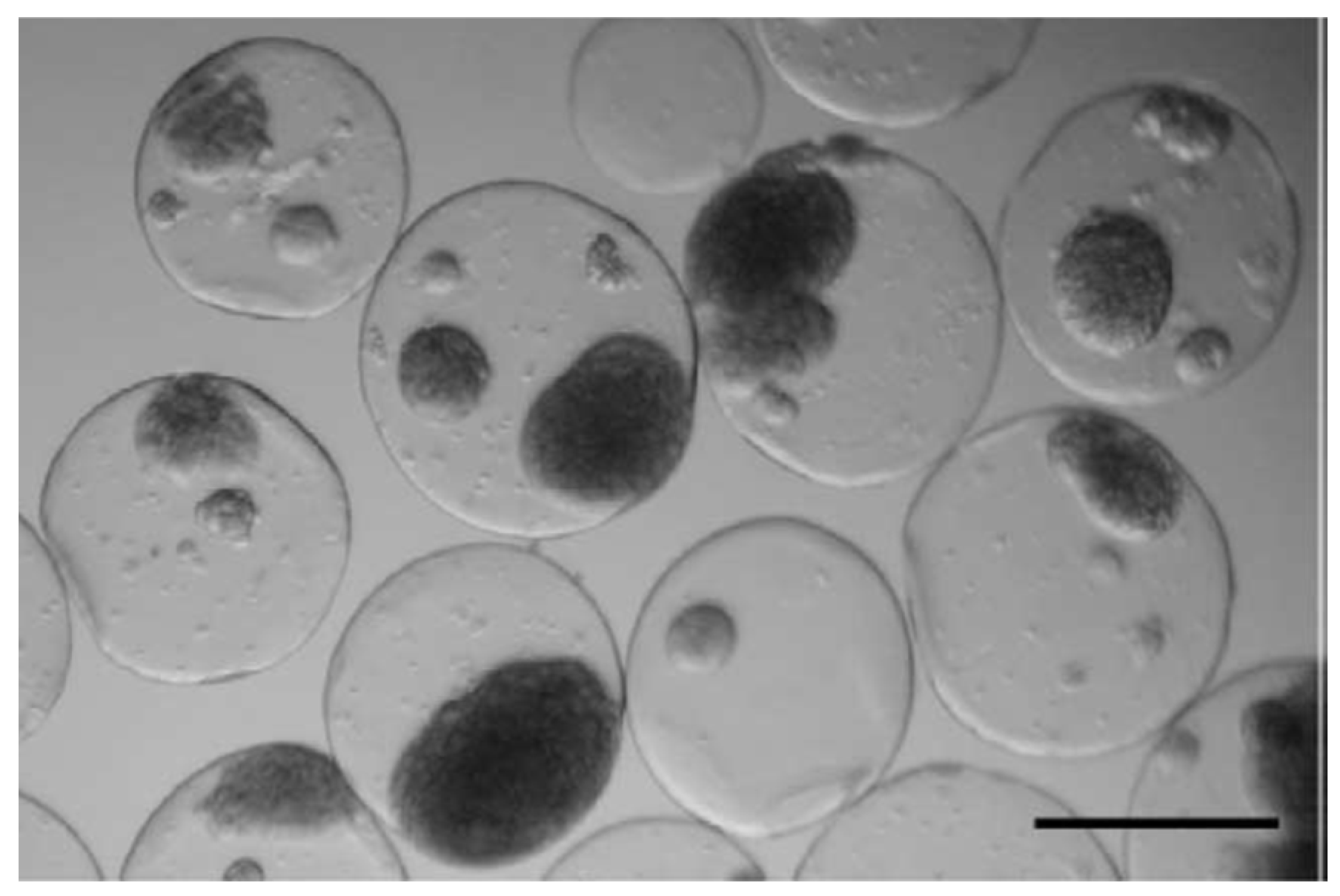
4. Sol-Gel Matrices
4.1. Sol-Gel Matrices for Drug Delivery Systems
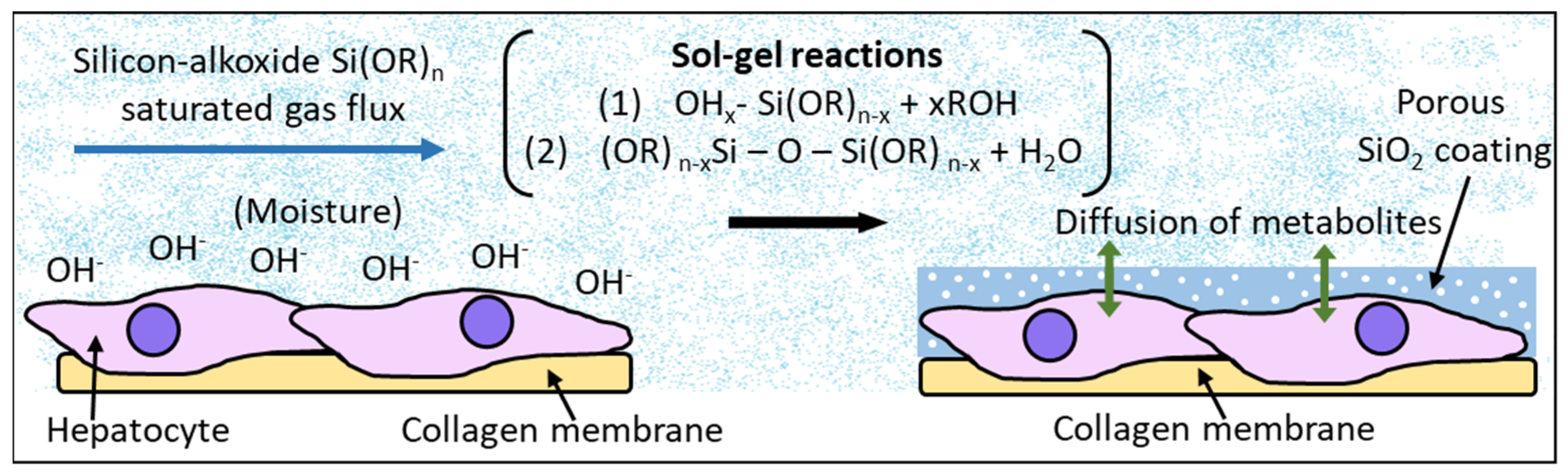
4.2. Sol-Gel Matrices for Tissue Engineering
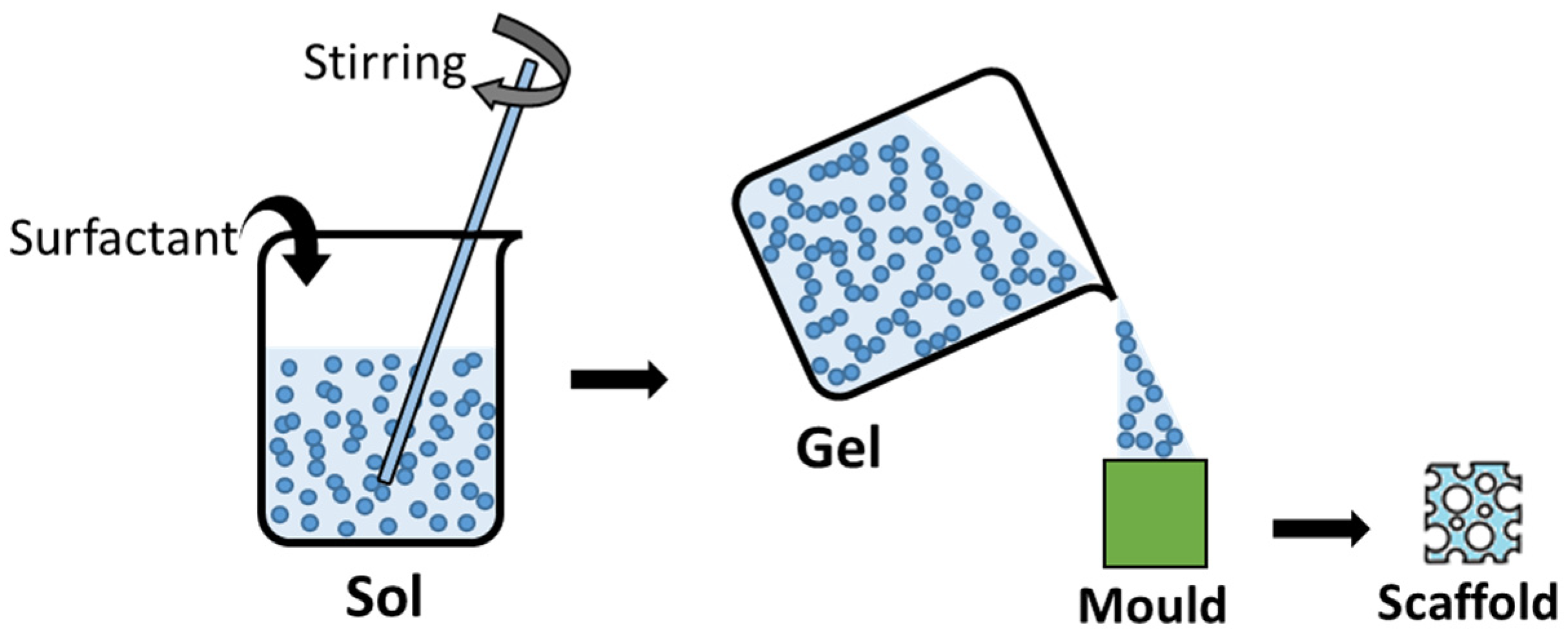
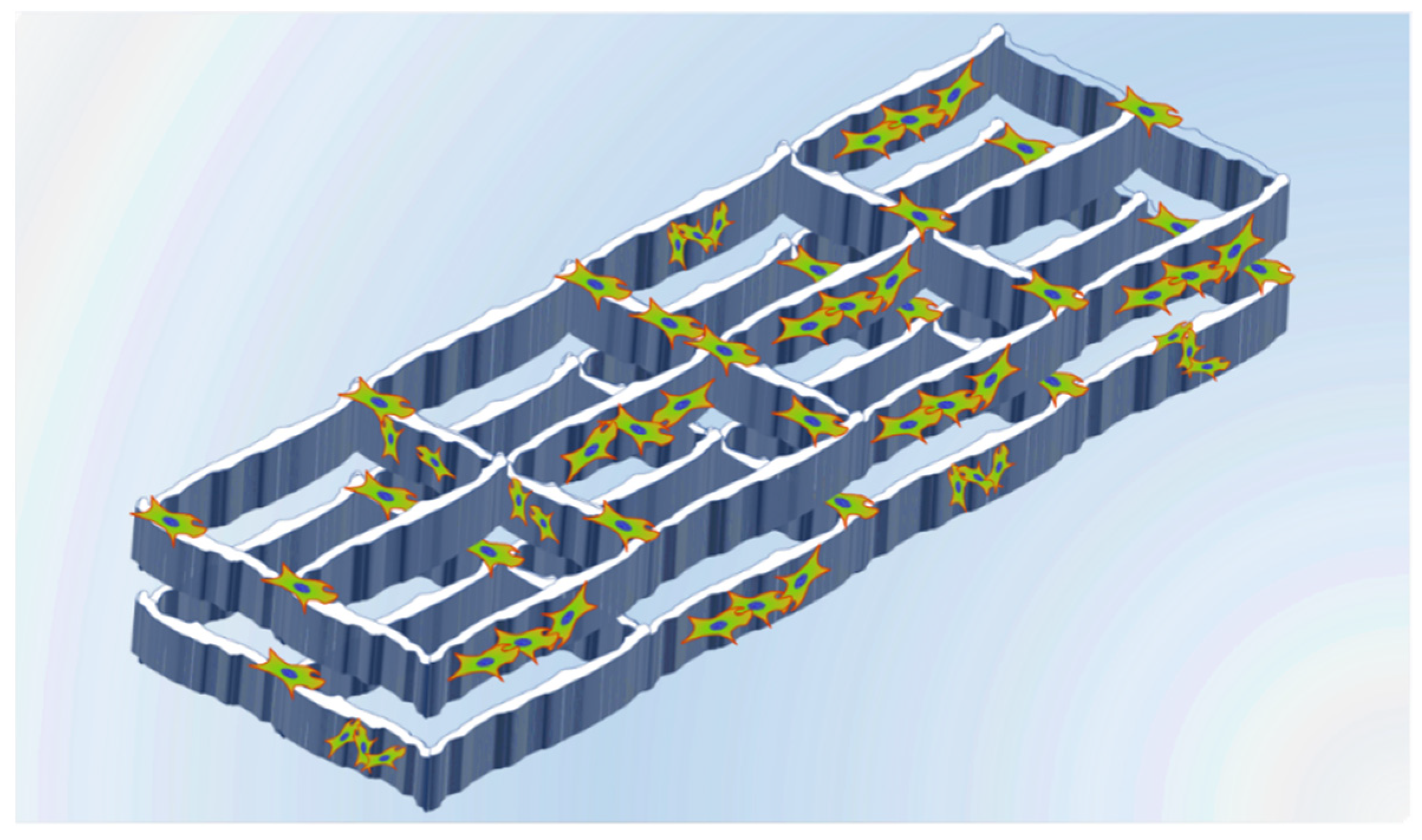
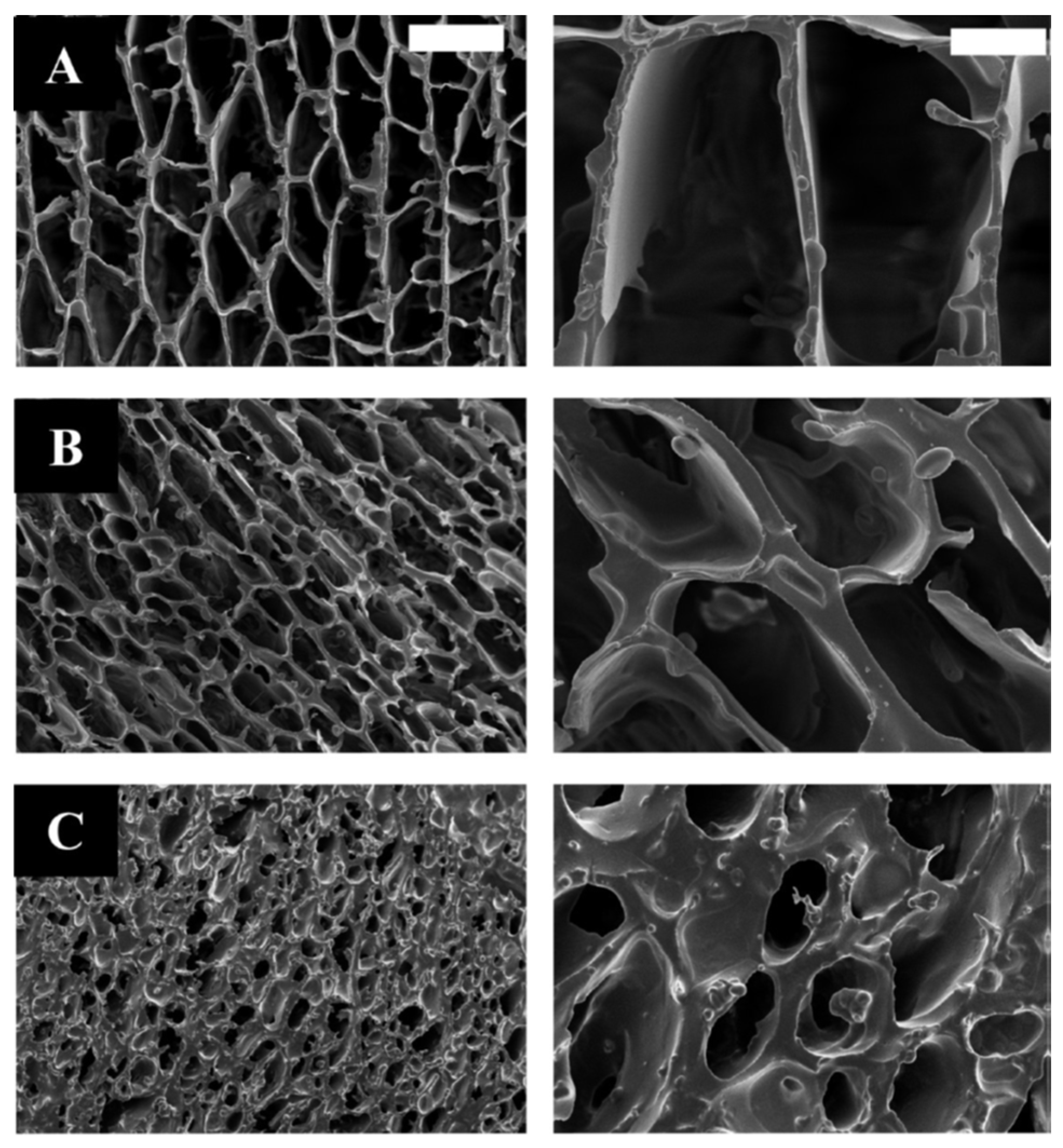
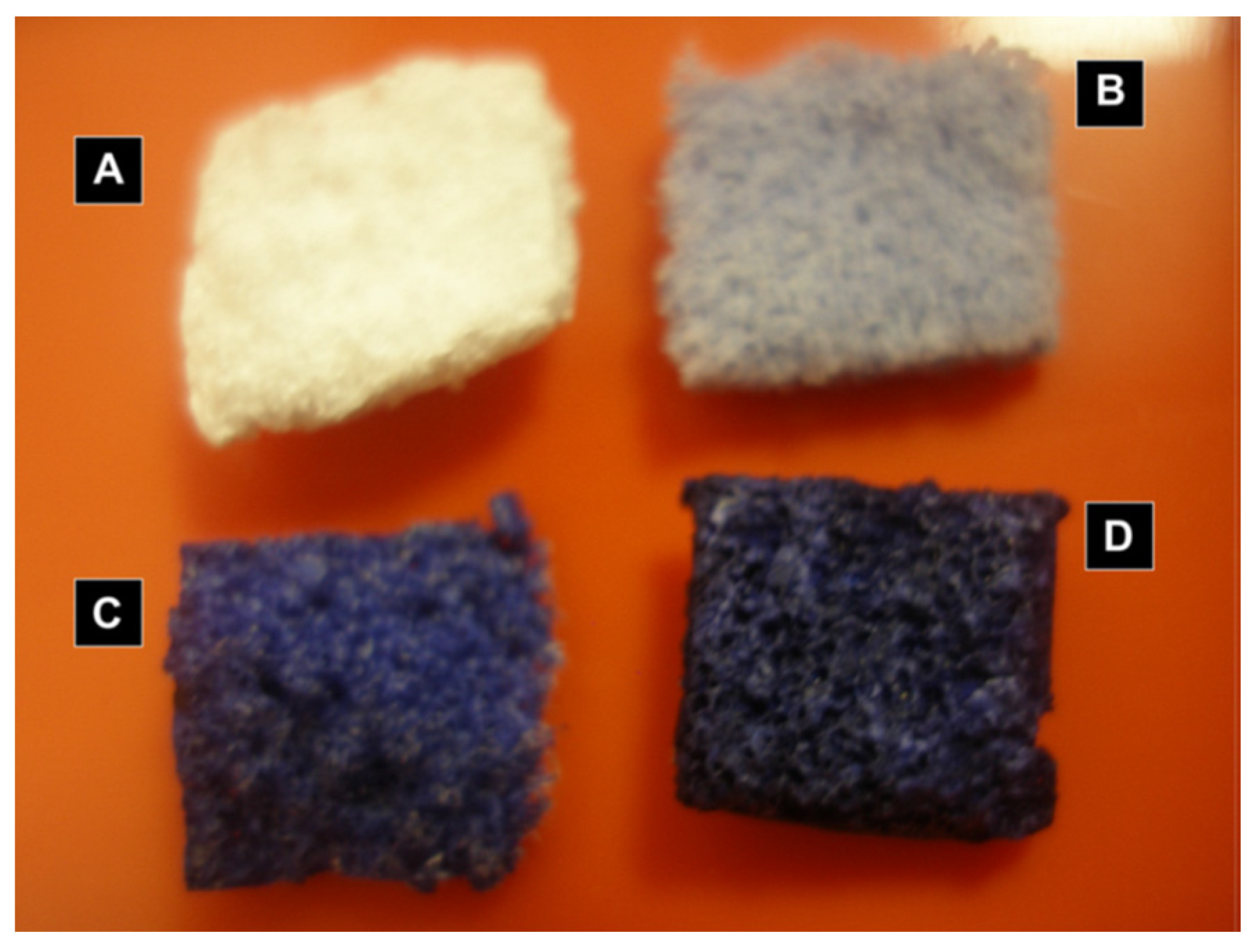
5. Sol-Gel Scaffolds for Tissue Engineering
6. Innovative Applications of the Sol-Gel Technique in the Biomedical Field
7. The Sol-Gel Process in the Biocompatibility Improvement of Magnesium Alloys
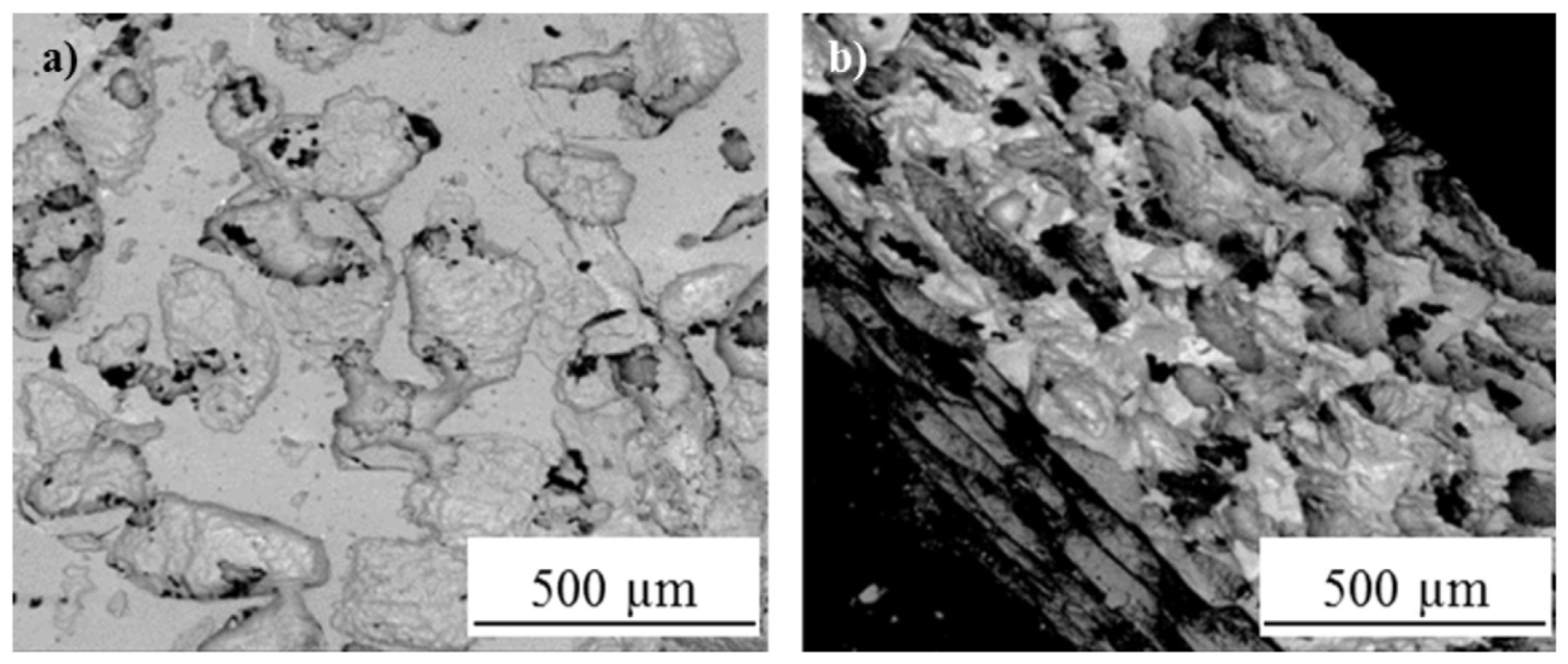
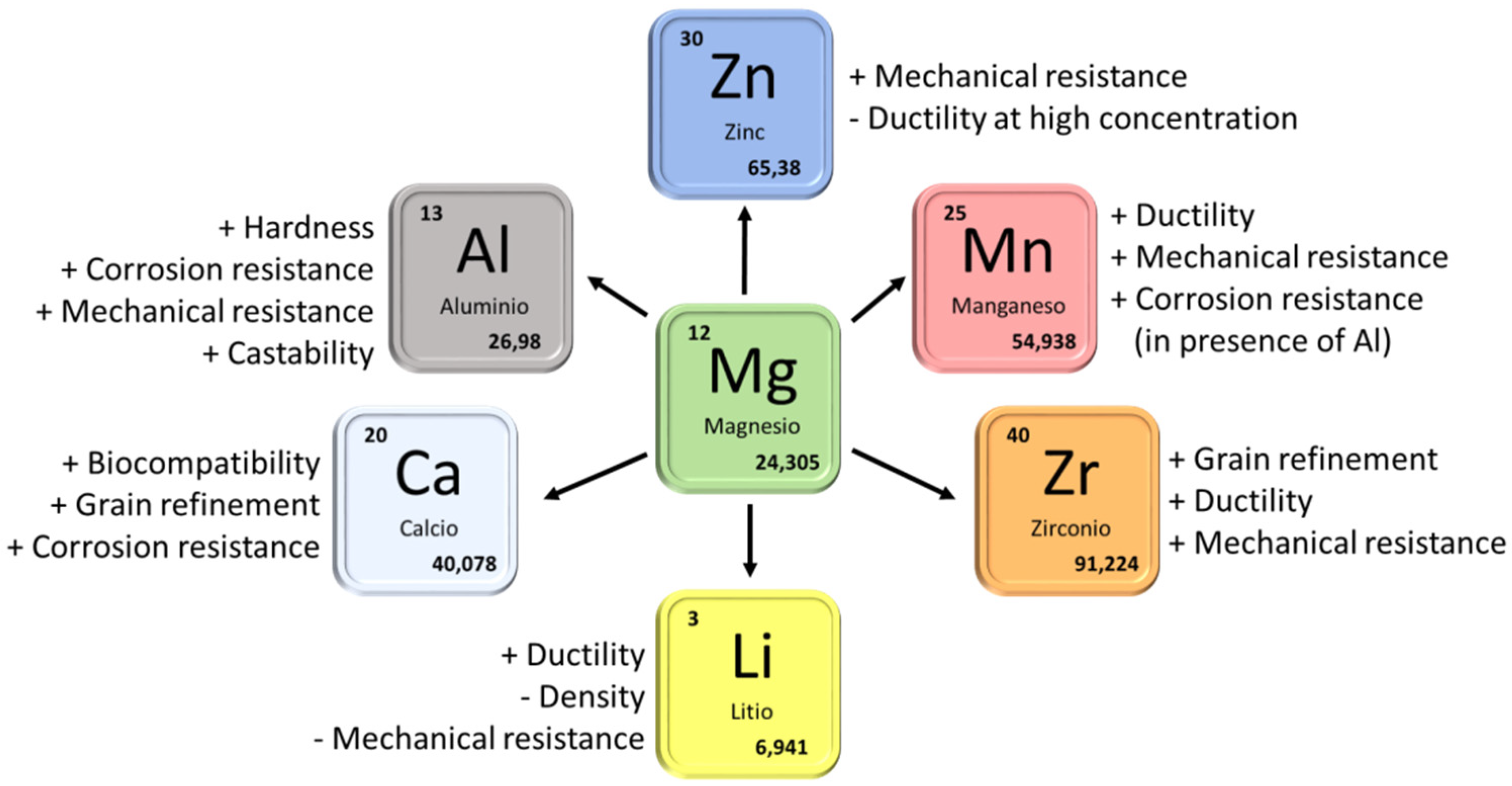
7.1. General Considerations
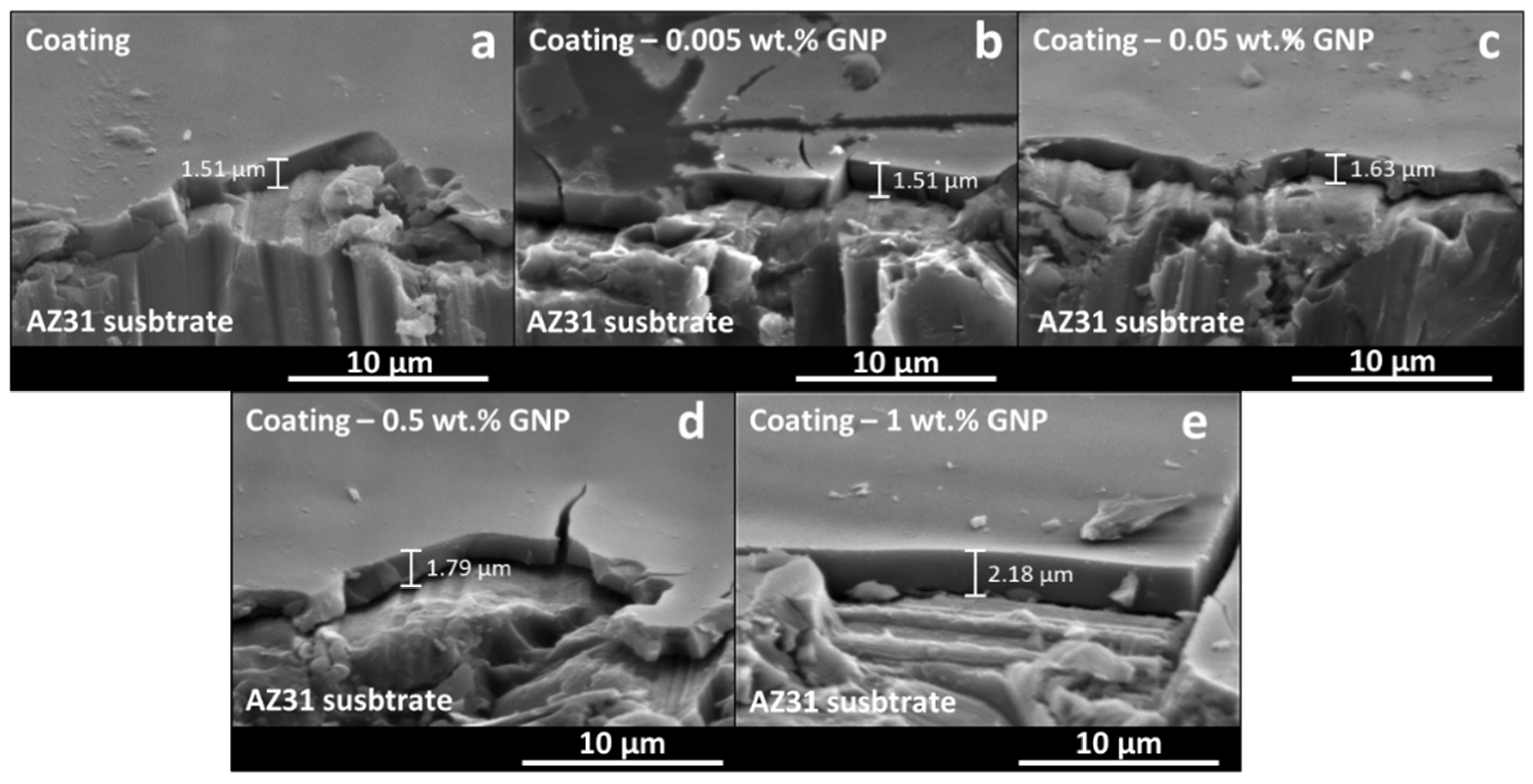
7.2. Sol-Gel Coatings on Mg-Al Alloys
7.3. Sol-Gel Coatings on Mg-Zn, Mg-Ca, and Mg-Rare Earth
8. Concluding Remarks and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Navarro, M.; Michiardi, A.; Castaño, O.; Planell, J.A. Biomaterials in orthopaedics. J. R. Soc. Interface 2008, 5, 1137–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hench, L.L. Biomaterials. Science 1980, 208, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Hench, L.L.; Polak, J.M. Third-Generation Biomedical Materials. Science 2002, 295, 1014–1017. [Google Scholar] [CrossRef] [Green Version]
- Ning, C.; Zhou, L.; Tan, G. Fourth-generation biomedical materials. Mater. Today 2016, 19, 2–3. [Google Scholar] [CrossRef]
- Sidane, D.; Rammal, H.; Beljebbar, A.; Gangloff, S.; Chicot, D.; Velard, F.; Khireddine, H.; Montagne, A.; Kerdjoudj, H. Biocompatibility of sol-gel hydroxyapatite-titania composite and bilayer coatings. Mater. Sci. Eng. C 2017, 72, 650–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Catauro, M.; Bollino, F.; Giovanardi, R.; Veronesi, P. Modification of Ti6Al4V implant surfaces by biocompatible TiO2/PCL hybrid layers prepared via sol-gel dip coating: Structural characterization, mechanical and corrosion behavior. Mater. Sci. Eng. C 2017, 74, 501–507. [Google Scholar] [CrossRef]
- Li, W.; Su, Y.; Ma, L.; Zhu, S.; Zheng, Y.; Guan, S. Sol-gel coating loaded with inhibitor on ZE21B Mg alloy for improving corrosion resistance and endothelialization aiming at potential cardiovascular application. Colloids Surf. B Biointerfaces 2021, 207, 111993. [Google Scholar] [CrossRef]
- Ballarre, J.; Ceré, S.M. Sol-gel coatings for protection and biofunctionalization of stainless-steel prosthetic intracorporeal devices in Latin-America. J. Sol-Gel Sci. Technol. 2022, 102, 96–104. [Google Scholar] [CrossRef]
- Dong, Y.; Wang, T.; Xu, Y.; Guo, Y.; Li, G.; Lian, J. A polydopamine-based calcium phosphate/graphene oxide composite coating on magnesium alloy to improve corrosion resistance and biocompatibility for biomedical applications. Materialia 2022, 21, 101315. [Google Scholar] [CrossRef]
- Sieminska, L.; Zerda, T.W. Diffusion of Steroids from Sol−Gel Glass. J. Phys. Chem. 1996, 100, 4591–4597. [Google Scholar] [CrossRef]
- Radin, S.; Ducheyne, P.; Kamplain, T.; Tan, B.H. Silica sol-gel for the controlled release of antibiotics. I. Synthesis, characterization, andin vitro release. J. Biomed. Mater. Res. 2001, 57, 313–320. [Google Scholar] [CrossRef]
- Zirak, N.; Maadani, A.; Salahinejad, E.; Abbasnezhad, N.; Shirinbayan, M. Fabrication, drug delivery kinetics and cell viability assay of PLGA-coated vancomycin-loaded silicate porous microspheres. Ceram. Int. 2021, 48, 48–54. [Google Scholar] [CrossRef]
- Pope, E.J.A.; Braun, K.; Peterson, C.M. Bioartificial Organs I: Silica Gel Encapsulated Pancreatic Islets for the Treatment of Diabetes Mellitus. J. Sol-Gel Sci. Technol. 1997, 639, 635–639. [Google Scholar] [CrossRef]
- Carturan, G.; Dellagiacoma, G.; Rossi, M.; Monte, R.D.; Muraca, M. Encapsulation of viable animal cells for hybrid bioartificial organs by the Biosil method. Sol-Gel Opt. IV 1997, 3136, 366–373. [Google Scholar] [CrossRef]
- Brinker, C.J.; Scherer, G.W. Sol-Gel Science: The Physics and Chemistry of Sol-Gel Processing; American Press: San Diego, CA, USA, 1990. [Google Scholar]
- Innocenzi, P.; Guglielmi, M.; Gobbin, M.; Colombo, P. Coating of metals by the sol-gel dip-coating method. J. Eur. Ceram. Soc. 1992, 10, 431–436. [Google Scholar] [CrossRef]
- Fernández-Hernán, J.; López, A.; Torres, B.; Rams, J. Silicon oxide multilayer coatings doped with carbon nanotubes and graphene nanoplatelets for corrosion protection of AZ31B magnesium alloy. Prog. Org. Coat. 2020, 148, 105836. [Google Scholar] [CrossRef]
- Fernández-Hernán, J.; López, A.; Torres, B.; Rams, J. Influence of roughness and grinding direction on the thickness and adhesion of sol-gel coatings deposited by dip-coating on AZ31 magnesium substrates. A Landau–Levich equation revision. Surf. Coat. Technol. 2021, 408, 126798. [Google Scholar] [CrossRef]
- Ramires, P.A.; Wennerberg, A.; Johansson, C.B.; Cosentino, F.; Tundo, S.; Milella, E. Biological behavior of sol-gel coated dental implants. J. Mater. Sci. Mater. Electron. 2003, 14, 539–545. [Google Scholar] [CrossRef]
- Catauro, M.; Barrino, F.; Bononi, M.; Colombini, E.; Giovanardi, R.; Veronesi, P.; Tranquillo, E. Coating of Titanium Substrates with ZrO2 and ZrO2-SiO2 Composites by Sol-Gel Synthesis for Biomedical Applications: Structural Characterization, Mechanical and Corrosive Behavior. Coatings 2019, 9, 200. [Google Scholar] [CrossRef] [Green Version]
- Velten, D.; Eisenbarth, E.; Schanne, N.; Breme, J. Biocompatible Nb2O5 thin films prepared by means of the sol–gel process. J. Mater. Sci. Mater. Med. 2004, 15, 457–461. [Google Scholar] [CrossRef]
- Zhang, J.; Zhou, J.; Huang, X.; Wang, L.; Liu, G.; Cheng, J. In situ preparation of hierarchically porous β-tricalcium phosphate bioceramic scaffolds by the sol-gel method combined with F127. Ceram. Int. 2020, 46, 6396–6405. [Google Scholar] [CrossRef]
- Baino, F.; Fiume, E.; Miola, M.; Leone, F.; Onida, B.; Verné, E. Fe-doped bioactive glass-derived scaffolds produced by sol-gel foaming. Mater. Lett. 2019, 235, 207–211. [Google Scholar] [CrossRef]
- Mohammadi, I.; Shahrabi, T.; Mahdavian, M.; Izadi, M. A novel corrosion inhibitive system comprising Zn-Al LDH and hybrid sol-gel silane nanocomposite coating for AA2024-T3. J. Alloy. Compd. 2022, 909, 164755. [Google Scholar] [CrossRef]
- Khalil, H.P.S.A.; Yahya, E.B.; Tajarudin, H.A.; Balakrishnan, V.; Nasution, H. Insights into the Role of Biopolymer-Based Xerogels in Biomedical Applications. Gels 2022, 8, 334. [Google Scholar] [CrossRef]
- Yang, X.; Jiang, P.; Xiao, R.; Fu, R.; Liu, Y.; Ji, C.; Song, Q.; Miao, C.; Yu, H.; Gu, J.; et al. Robust Silica—Agarose Composite Aerogels with Interpenetrating Network Structure by In Situ Sol-Gel Process. Gels 2022, 8, 303. [Google Scholar] [CrossRef]
- Liu, D.-M.; Yang, Q.; Troczynski, T. Sol–gel hydroxyapatite coatings on stainless steel substrates. Biomaterials 2002, 23, 691–698. [Google Scholar] [CrossRef]
- Domínguez-Trujillo, C.; Peón, E.; Chicardi, E.; Pérez, H.; Rodríguez-Ortiz, J.A.; Pavón, J.; García-Couce, J.; Galvan, J.C.; García-Moreno, F.; Torres, Y. Sol-gel deposition of hydroxyapatite coatings on porous titanium for biomedical applications. Surf. Coat. Technol. 2018, 333, 158–162. [Google Scholar] [CrossRef]
- Hosseinalipour, S.; Ershad-Langroudi, A.; Hayati, A.N.; Nabizade-Haghighi, A. Characterization of sol–gel coated 316L stainless steel for biomedical applications. Prog. Org. Coat. 2010, 67, 371–374. [Google Scholar] [CrossRef]
- Durán, A.; Conde, A.; Coedo, A.G.; Dorado, T.; García, C.; Ceré, S. Sol–gel coatings for protection and bioactivation of metals used in orthopaedic devices. J. Mater. Chem. 2004, 14, 2282–2290. [Google Scholar] [CrossRef] [Green Version]
- Devi, K.B.; Singh, K.; Rajendran, N. Sol–gel synthesis and characterisation of nanoporous zirconium titanate coated on 316L SS for biomedical applications. J. Sol-Gel Sci. Technol. 2011, 59, 513–520. [Google Scholar] [CrossRef]
- Śmieszek, A.; Donesz-Sikorska, A.; Grzesiak, J.; Krzak, J.; Marycz, K. Biological effects of sol–gel derived ZrO2 and SiO2/ZrO2 coatings on stainless steel surface—In vitro model using mesenchymal stem cells. J. Biomater. Appl. 2014, 29, 699–714. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, B.; Feldmann, M.; Ziegler, G. Sol–gel and precursor-derived coatings with cover function on medical alloys. J. Mater. Chem. 2007, 17, 4034–4040. [Google Scholar] [CrossRef]
- Castro, Y.; Durán, A. Control of degradation rate of Mg alloys using silica sol–gel coatings for biodegradable implant materials. J. Sol-Gel Sci. Technol. 2018, 90, 198–208. [Google Scholar] [CrossRef]
- Balamurugan, A.; Balossier, G.; Kannan, S.; Rajeswari, S. Elaboration of sol–gel derived apatite films on surgical grade stainless steel for biomedical applications. Mater. Lett. 2006, 60, 2288–2293. [Google Scholar] [CrossRef]
- Agrawal, K.; Singh, G.; Puri, D.; Prakash, S. Synthesis and Characterization of Hydroxyapatite Powder by Sol-Gel Method for Biomedical Application. J. Miner. Mater. Charact. Eng. 2011, 10, 727–734. [Google Scholar] [CrossRef]
- Regina, S.; Conceição, V. Sol-Gel SiO2-CaO-P2O5 Biofilm with Surface Engineered for Medical Application 3. Results and Discussion. Mater. Res. 2007, 10, 177–181. [Google Scholar]
- Catauro, M.; Papale, F.; Sapio, L.; Naviglio, S. Biological influence of Ca/P ratio on calcium phosphate coatings by sol-gel processing. Mater. Sci. Eng. C 2016, 65, 188–193. [Google Scholar] [CrossRef] [PubMed]
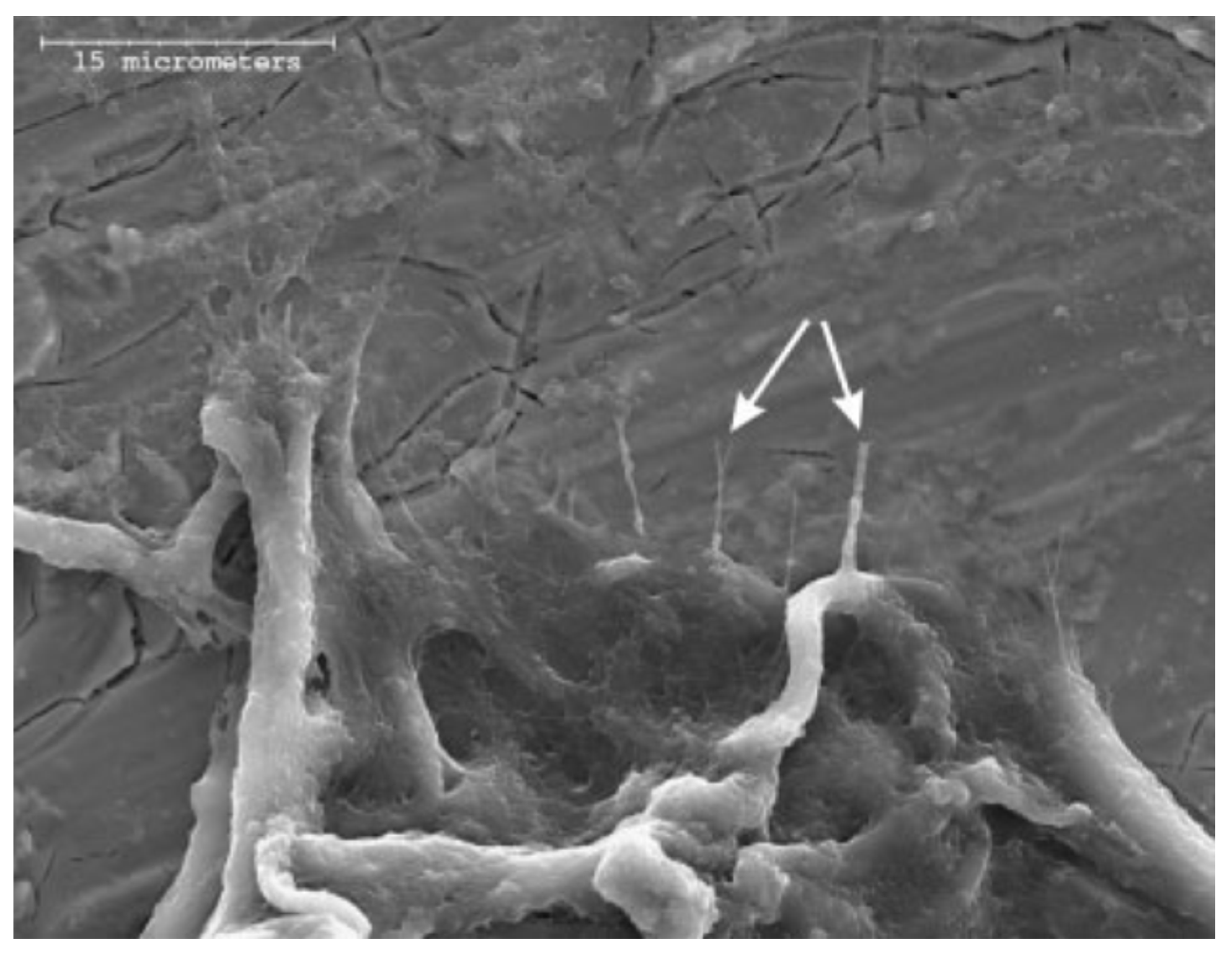
- Pierce, A.L.; Sommakia, S.; Rickus, J.L.; Otto, K.J. Thin-film silica sol–gel coatings for neural microelectrodes. J. Neurosci. Methods 2009, 180, 106–110. [Google Scholar] [CrossRef]
- Haddow, D.; James, P.; Van Noort, R. Sol-Gel Derived Calcium Phosphate Coatings for Biomedical Applications. J. Sol-Gel Sci. Technol. 1998, 13, 261–265. [Google Scholar] [CrossRef]
- Zhou, H.; Lee, J. Nanoscale hydroxyapatite particles for bone tissue engineering. Acta Biomater. 2011, 7, 2769–2781. [Google Scholar] [CrossRef]
- Chung, R.-J.; Hsieh, M.-F.; Huang, C.-W.; Perng, L.-H.; Wen, H.-W.; Chin, T.-S. Antimicrobial effects and human gingival biocompatibility of hydroxyapatite sol-gel coatings. J. Biomed. Mater. Res. Part B Appl. Biomater. 2006, 76, 169–178. [Google Scholar] [CrossRef] [PubMed]
- Kawashita, M.; Tsuneyama, S.; Miyaji, F.; Kokubo, T.; Kozuka, H.; Yamamoto, K. Antibacterial silver-containing silica glass prepared by sol–gel method. Biomaterials 2000, 21, 393–398. [Google Scholar] [CrossRef]
- Gallardo, J.; Galliano, P.; Durán, A. Bioactive and Protective Sol-Gel Coatings on Metals for Orthopaedic Prostheses. J. Sol-Gel Sci. Technol. 2001, 21, 65–74. [Google Scholar] [CrossRef]
- Galliano, P.; de Damborenea, J.; Pascual, M.J.; Durán, A. Sol-Gel Coatings on 316L Steel for Clinical Applications. J. Sol-Gel Sci. Technol. 1998, 13, 723–727. [Google Scholar] [CrossRef]
- Ääritalo, V.; Meretoja, V.; Tirri, T.; Areva, S.; Jämsä, T.; Tuukkanen, J.; Rosling, A.; Närhi, T. Development of a Low Temperature Sol-Gel-Derived Titania-Silica Implant Coating. Mater. Sci. Appl. 2010, 01, 118–126. [Google Scholar] [CrossRef] [Green Version]
- Gartner, M.; Trapalis, C.; Todorova, N.; Giannakopoulou, T.; Dobrescu, G.; Anastasescu, M.; Osiceanu, P.; Ghita, A.; Enache, M.; Dumitru, L.; et al. Doped Sol-gel TiO2Films for Biological Applications. Bull. Korean Chem. Soc. 2008, 29, 1038–1042. [Google Scholar] [CrossRef] [Green Version]
- Catauro, M.; Bollino, F.; Papale, F. Biocompatibility improvement of titanium implants by coating with hybrid materials synthesized by sol-gel technique. J. Biomed. Mater. Res. Part A 2014, 102, 4473–4479. [Google Scholar] [CrossRef] [PubMed]
- Kayani, Z.N.; Anwar, M.; Saddiqe, Z.; Riaz, S.; Naseem, S. Biological and optical properties of sol–gel derived ZnO using different percentages of silver contents. Colloids Surf. B Biointerfaces 2018, 171, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Areva, S.; Paldan, H.; Peltola, T.; Närhi, T.; Jokinen, M.; Lindén, M. Use of sol-gel-derived titania coating for direct soft tissue attachment. J. Biomed. Mater. Res. Part A 2004, 70, 169–178. [Google Scholar] [CrossRef]
- Liu, J.-X.; Yang, D.-Z.; Shi, F.; Cai, Y.-J. Sol–gel deposited TiO2 film on NiTi surgical alloy for biocompatibility improvement. Thin Solid Films 2003, 429, 225–230. [Google Scholar] [CrossRef]
- Gerritsen, M.; Kros, A.; Sprakel, V.; Lutterman, J.A.; Nolte, R.J.M.; Jansen, J.A. Biocompatibility evaluation of sol–gel coatings for subcutaneously implantable glucose sensors. Biomaterials 2000, 21, 71–78. [Google Scholar] [CrossRef]
- Kennady, M.C.; Tucker, M.R.; Lester, G.E.; Buckley, M.J. Stress shielding effect of rigid internal fixation plates on mandibular bone grafts. A photon absorption densitometry and quantitative computerized tomographic evaluation. Int. J. Oral Maxillofac. Surg. 1989, 18, 307–310. [Google Scholar] [CrossRef]
- Kanayama, M.; Cunningham, B.W.; Haggerty, C.J.; Abumi, K.; Kaneda, K.; McAfee, P.C. In vitro biomechanical investigation of the stability and stress-shielding effect of lumbar interbody fusion devices. J. Neurosurg. 2000, 93, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, T.; Price, J.S.; Lanyon, L.E. Functional adaptation to mechanical loading in both cortical and cancellous bone is controlled locally and is confined to the loaded bones. Bone 2010, 46, 314–321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turner, C. Three rules for bone adaptation to mechanical stimuli. Bone 1998, 23, 399–407. [Google Scholar] [CrossRef]
- Mellon, S.J.; Tanner, E. Bone and its adaptation to mechanical loading: A review. Int. Mater. Rev. 2012, 57, 235–255. [Google Scholar] [CrossRef] [Green Version]
- Xin, Y.; Hu, T.; Chu, P.K. In vitro studies of biomedical magnesium alloys in a simulated physiological environment: A review. Acta Biomater. 2011, 7, 1452–1459. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.N.; Li, X.L.; Zhou, W.R.; Cheng, Y.; Zheng, Y. Microstructure, biocorrosion and cytotoxicity evaluations of rapid solidified Mg–3Ca alloy ribbons as a biodegradable material. Biomed. Mater. 2010, 5, 3–9. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Gu, X.; Lou, S.; Zheng, Y. The development of binary Mg–Ca alloys for use as biodegradable materials within bone. Biomaterials 2008, 29, 1329–1344. [Google Scholar] [CrossRef]
- Zhang, B.; Hou, Y.; Wang, X.; Wang, Y.; Geng, L. Mechanical properties, degradation performance and cytotoxicity of Mg–Zn–Ca biomedical alloys with different compositions. Mater. Sci. Eng. C 2011, 31, 1667–1673. [Google Scholar] [CrossRef]
- Gu, X.; Zheng, Y.; Cheng, Y.; Zhong, S.; Xi, T. In vitro corrosion and biocompatibility of binary magnesium alloys. Biomaterials 2009, 30, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Byun, S.-H.; Lim, H.-K.; Lee, S.-M.; Kim, H.-E.; Kim, S.-M.; Lee, J.-H. Biodegradable Magnesium Alloy (ZK60) with a Poly(l-lactic)-Acid Polymer Coating for Maxillofacial Surgery. Metals 2020, 10, 724. [Google Scholar] [CrossRef]
- Amaravathy, P.; Sowndarya, S.; Sathyanarayanan, S.; Rajendran, N. Novel sol gel coating of Nb2O5 on magnesium alloy for biomedical applications. Surf. Coat. Technol. 2014, 244, 131–141. [Google Scholar] [CrossRef]
- Hu, J.; Zhang, C.; Cui, B.; Bai, K.; Guan, S.; Wang, L.; Zhu, S. In vitro degradation of AZ31 magnesium alloy coated with nano TiO2 film by sol–gel method. Appl. Surf. Sci. 2011, 257, 8772–8777. [Google Scholar] [CrossRef]
- Catauro, M.; Papale, F.; Roviello, G.; Ferone, C.; Bollino, F.; Trifuoggi, M.; Aurilio, C. Synthesis of SiO2 and CaO rich calcium silicate systems via sol-gel process: Bioactivity, biocompatibility, and drug delivery tests. J. Biomed. Mater. Res. Part A 2014, 102, 3087–3092. [Google Scholar] [CrossRef] [PubMed]
- Ou, S.-F.; Chung, R.-J.; Lin, L.-H.; Chiang, Y.-C.; Huang, C.-F.; Ou, K.-L. A mechanistic study on the antibacterial behavior of silver doped bioceramic. J. Alloy. Compd. 2015, 629, 362–367. [Google Scholar] [CrossRef]
- Liao, K.-H.; Ou, K.-L.; Cheng, H.-C.; Lin, C.-T.; Peng, P.-W. Effect of silver on antibacterial properties of stainless steel. Appl. Surf. Sci. 2010, 256, 3642–3646. [Google Scholar] [CrossRef]
- Hetrick, E.M.; Schoenfisch, M.H. Reducing implant-related infections: Active release strategies. Chem. Soc. Rev. 2006, 35, 780–789. [Google Scholar] [CrossRef]
- Kortesuo, P.; Ahola, M.; Kangas, M.; Kangasniemi, I.; Yli-Urpo, A.; Kiesvaara, J. In vitro evaluation of sol–gel processed spray dried silica gel microspheres as carrier in controlled drug delivery. Int. J. Pharm. 2000, 200, 223–229. [Google Scholar] [CrossRef]
- Chawla, A.; Taylor, K.; Newton, J.; Johnson, M. Production of spray dried salbutamol sulphate for use in dry powder aerosol formulation. Int. J. Pharm. 1994, 108, 233–240. [Google Scholar] [CrossRef]
- He, P.; Davis, S.S.; Illum, L. Chitosan microspheres prepared by spray dying method. Eur. J. Pharm. Sci. 1996, 4, S173. [Google Scholar] [CrossRef]
- Oh, S.-A.; Kim, S.-H.; Won, J.-E.; Kim, J.-J.; Shin, U.S.; Kim, H.-W. Effects on Growth and Osteogenic Differentiation of Mesenchymal Stem Cells by the Zinc-Added Sol-Gel Bioactive Glass Granules. J. Tissue Eng. 2010, 1, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Raucci, M.G.; Giugliano, D.; Alvarez-Perez, M.A.; Ambrosio, L. Effects on growth and osteogenic differentiation of mesenchymal stem cells by the strontium-added sol–gel hydroxyapatite gel materials. J. Mater. Sci. Mater. Med. 2015, 26, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Bosetti, M.; Cannas, M. The effect of bioactive glasses on bone marrow stromal cells differentiation. Biomaterials 2005, 26, 3873–3879. [Google Scholar] [CrossRef] [PubMed]
- Nablo, B.J.; Chen, T.-Y.; Schoenfisch, M.H. Sol−Gel Derived Nitric-Oxide Releasing Materials that Reduce Bacterial Adhesion. J. Am. Chem. Soc. 2001, 123, 9712–9713. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharyya, S.; Agrawal, A.; Knabe, C.; Ducheyne, P. Sol–gel silica controlled release thin films for the inhibition of methicillin-resistant Staphylococcus aureus. Biomaterials 2014, 35, 509–517. [Google Scholar] [CrossRef]
- Hench, L.L.; Jones, J.R. Bioactive Glasses: Frontiers and Challenges. Front. Bioeng. Biotechnol. 2015, 3, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Luz, G.M.; Mano, J. Preparation and characterization of bioactive glass nanoparticles prepared by sol–gel for biomedical applications. Nanotechnology 2011, 22, 494014. [Google Scholar] [CrossRef]
- Moshaverinia, A.; Ansari, S.; Moshaverinia, M.; Roohpour, N.; Darr, J.A.; Rehman, I. Effects of incorporation of hydroxyapatite and fluoroapatite nanobioceramics into conventional glass ionomer cements (GIC). Acta Biomater. 2008, 4, 432–440. [Google Scholar] [CrossRef]
- Liu, W.C.; Wang, H.-Y.; Chen, L.-C.; Huang, S.-W.; Wu, C.; Chung, R.-J. Hydroxyapatite/tricalcium silicate composites cement derived from novel two-step sol-gel process with good biocompatibility and applications as bone cement and potential coating materials. Ceram. Int. 2019, 45, 5668–5679. [Google Scholar] [CrossRef]
- Thampi, V.A.; Prabhu, M.; Kavitha, K.; Manivasakan, P.; Prabu, P.; Rajendran, V.; Shankar, S.; Kulandaivelu, P. Hydroxyapatite, alumina/zirconia, and nanobioactive glass cement for tooth-restoring applications. Ceram. Int. 2014, 40, 14355–14365. [Google Scholar] [CrossRef]
- Radin, S.; Chen, T.; Ducheyne, P. The controlled release of drugs from emulsified, sol gel processed silica microspheres. Biomaterials 2009, 30, 850–858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melville, A.J.; Rodríguez-Lorenzo, L.M.; Forsythe, J.S. Effects of calcination temperature on the drug delivery behaviour of Ibuprofen from hydroxyapatite powders. J. Mater. Sci. Mater. Electron. 2008, 19, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- Chung, R.-J.; Hsieh, M.-F.; Huang, K.-C.; Perng, L.-H.; Chou, F.-I.; Chin, T.-S. Anti-Microbial Hydroxyapatite Particles Synthesized by a Sol? Gel Route. J. Sol-Gel Sci. Technol. 2005, 33, 229–239. [Google Scholar] [CrossRef] [Green Version]
- Kortesuo, P.; Ahola, M.; Karlsson, S.; Kangasniemi, I.; Kiesvaara, J.; Yli-Urpo, A. Sol-gel-processed sintered silica xerogel as a carrier in controlled drug delivery. J. Biomed. Mater. Res. 1999, 44, 162–167. [Google Scholar] [CrossRef]
- Hernández-Escolano, M.; Juan-Díaz, M.; Martinez-Ibañez, M.; Jiménez-Morales, A.; Goñi, I.; Gurruchaga, M.; Suay, J. The design and characterisation of sol–gel coatings for the controlled-release of active molecules. J. Sol-Gel Sci. Technol. 2012, 64, 442–451. [Google Scholar] [CrossRef] [Green Version]
- Sakai, S.; Ono, T.; Ijima, H.; Kawakami, K. In vitro and in vivo evaluation of alginate/sol–gel synthesized aminopropyl-silicate/alginate membrane for bioartificial pancreas. Biomaterials 2002, 23, 4177–4183. [Google Scholar] [CrossRef]
- Sglavo, V.M.; Carturan, G.; Monte, R.D.; Muraca, M. SiO2 Entrapment of animal cells Part I Mechanical featurs of sol-gel SiO2 coatings. J. Mater. Sci. 1999, 34, 3587–3590. [Google Scholar] [CrossRef]
- Muraca, M.; Vilei, M.T.; Zanusso, G.E.; Ferraresso, C.; Boninsegna, S.; Monte, R.D.; Carraro, P.; Carturan, G. SiO2 Entrapment of Animal Cells: Liver-Specific Metabolic Activities in Silica-Overlaid Hepatocytes. Artif. Organs 2002, 26, 664–669. [Google Scholar] [CrossRef]
- Chen, Q.-Z.; Thouas, G.A. Fabrication and characterization of sol–gel derived 45S5 Bioglass®–ceramic scaffolds. Acta Biomater. 2011, 7, 3616–3626. [Google Scholar] [CrossRef]
- Minaberry, Y.; Jobbágy, M. Macroporous Bioglass Scaffolds Prepared by Coupling Sol–Gel with Freeze Drying. Chem. Mater. 2011, 23, 2327–2332. [Google Scholar] [CrossRef]
- Raucci, M.G.; Guarino, V.; Ambrosio, L. Hybrid composite scaffolds prepared by sol–gel method for bone regeneration. Compos. Sci. Technol. 2010, 70, 1861–1868. [Google Scholar] [CrossRef] [Green Version]
- Bielby, R.C.; Pryce, R.S.; Hench, L.L.; Polak, J.M. Enhanced Derivation of Osteogenic Cells from Murine Embryonic Stem Cells after Treatment with Ionic Dissolution Products of 58S Bioactive Sol–Gel Glass. Tissue Eng. 2005, 11, 479–488. [Google Scholar] [CrossRef]
- Mosqueira, L.; Barrioni, B.R.; Martins, T.; Melo, F.G.; Ocarino, N.M.; Serakides, R.; Pereira, M.M. Strontium-releasing sol–gel bioactive glass spheres and their ability to stimulate osteogenic differentiation in osteoporotic bone marrow mesenchymal stem cells. J. Mater. Res. 2021, 36, 459–474. [Google Scholar] [CrossRef]
- Mano, J.F. Stimuli-Responsive Polymeric Systems for Biomedical Applications. Adv. Eng. Mater. 2008, 10, 515–527. [Google Scholar] [CrossRef]
- Carrasquilla, C.; Kapteyn, E.; Li, Y.; Brennan, J.D. Sol-Gel-Derived Biohybrid Materials Incorporating Long-Chain DNA Aptamers. Angew. Chem. Int. Ed. 2017, 56, 10686–10690. [Google Scholar] [CrossRef]
- Maier, P.; Hort, N. Magnesium Alloys for Biomedical Applications. Metals 2020, 10, 1328. [Google Scholar] [CrossRef]
- Kamrani, S.; Fleck, C. Biodegradable magnesium alloys as temporary orthopaedic implants: A review. BioMetals 2019, 32, 185–193. [Google Scholar] [CrossRef]
- Chen, J.; Tan, L.; Yu, X.; Etim, I.P.; Ibrahim, M.; Yang, K. Mechanical properties of magnesium alloys for medical application: A review. J. Mech. Behav. Biomed. Mater. 2018, 87, 68–79. [Google Scholar] [CrossRef]
- Agarwal, S.; Curtin, J.; Duffy, B.; Jaiswal, S. Biodegradable magnesium alloys for orthopaedic applications: A review on corrosion, biocompatibility and surface modifications. Mater. Sci. Eng. C 2016, 68, 948–963. [Google Scholar] [CrossRef] [Green Version]
- Du, Z.; Leng, H.; Guo, L.; Huang, Y.; Zheng, T.; Zhao, Z.; Liu, X.; Zhang, X.; Cai, Q.; Yang, X. Calcium silicate scaffolds promoting bone regeneration via the doping of Mg2+ or Mn2+ ion. Compos. Part B Eng. 2020, 190, 107937. [Google Scholar] [CrossRef]
- Van der Wijst, J.; Bindels, R.J.; Hoenderop, J.G. Mg2+ homeostasis. Curr. Opin. Nephrol. Hypertens. 2014, 23, 361–369. [Google Scholar] [CrossRef]
- Hofstetter, J.; Martinelli, E.; Pogatscher, S.; Schmutz, P.; Povoden-Karadeniz, E.; Weinberg, A.; Uggowitzer, P.; Löffler, J. Influence of trace impurities on the in vitro and in vivo degradation of biodegradable Mg–5Zn–0.3Ca alloys. Acta Biomater. 2015, 23, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Uggowitzer, P.J.; Nagasekhar, A.; Schmutz, P.; Easton, M.; Song, G.-L.; Atrens, A. Calculated phase diagrams and the corrosion of die-cast Mg–Al alloys. Corros. Sci. 2009, 51, 602–619. [Google Scholar] [CrossRef]
- Mohamed, S.R.; Friedrich, S.; Friedrich, B. Refining Principles and Technical Methodologies to Produce Ultra-Pure Magnesium for High-Tech Applications. Metals 2019, 9, 85. [Google Scholar] [CrossRef] [Green Version]
- Witte, F.; Hort, N.; Vogt, C.; Cohen, S.; Kainer, K.U.; Willumeit, R.; Feyerabend, F. Degradable biomaterials based on magnesium corrosion. Curr. Opin. Solid State Mater. Sci. 2008, 12, 63–72. [Google Scholar] [CrossRef] [Green Version]
- Esmaily, M.; Svensson, J.E.; Fajardo, S.; Birbilis, N.; Frankel, G.S.; Virtanen, S.; Arrabal, R.; Thomas, S.; Johansson, L.G. Fundamentals and advances in magnesium alloy corrosion. Prog. Mater. Sci. 2017, 89, 92–193. [Google Scholar] [CrossRef]
- Khramov, A.; Balbyshev, V.; Kasten, L.; Mantz, R. Sol–gel coatings with phosphonate functionalities for surface modification of magnesium alloys. Thin Solid Films 2006, 514, 174–181. [Google Scholar] [CrossRef]
- Reyes, Y.; Durán, A.; Castro, Y. Glass-like cerium sol-gel coatings on AZ31B magnesium alloy for controlling the biodegradation of temporary implants. Surf. Coat. Technol. 2016, 307, 574–582. [Google Scholar] [CrossRef]
- Su, Y.; Lu, C.; Hu, X.; Guo, Y.; Xun, X.; Zhang, Z.; Li, G.; Lian, J.; Ren, L. Improving the Degradation Resistance and Surface Biomineralization Ability of Calcium Phosphate Coatings on a Biodegradable Magnesium Alloy via a Sol-Gel Spin Coating Method. J. Electrochem. Soc. 2018, 165, C155–C161. [Google Scholar] [CrossRef]
- Phani, A.R.; Gammel, F.J.; Hack, T.; Haefke, H. Enhanced corrosioon resistance by sol-gel-based ZrO2-CeO2 coatings on magnesium alloys. Mater. Corros. 2005, 56, 77–82. [Google Scholar] [CrossRef]
- Fernández-Hernán, J.; Torres, B.; López, A.; Martínez-Campos, E.; Rams, J. Sol-gel coatings doped with graphene nanoplatelets for improving the degradation rate and the cytocompatibility of AZ31 alloy for biomedical applications. Surf. Coat. Technol. 2021, 426, 127745. [Google Scholar] [CrossRef]
- Nezamdoust, S.; Seifzadeh, D.; Rajabalizadeh, Z. Application of novel sol–gel composites on magnesium alloy. J. Magnes. Alloy. 2019, 7, 419–432. [Google Scholar] [CrossRef]
- Nezamdoust, S.; Seifzadeh, D. Application of CeH–V/ sol–gel composite coating for corrosion protection of AM60B magnesium alloy. Trans. Nonferr. Met. Soc. China 2017, 27, 352–362. [Google Scholar] [CrossRef]
- Nezamdoust, S.; Seifzadeh, D.; Rajabalizadeh, Z. PTMS/OH-MWCNT sol-gel nanocomposite for corrosion protection of magnesium alloy. Surf. Coat. Technol. 2018, 335, 228–240. [Google Scholar] [CrossRef]
- Nezamdoust, S.; Seifzadeh, D.; Habibi-Yangjeh, A. Nanodiamond incorporated sol−gel coating for corrosion protection of magnesium alloy. Trans. Nonferr. Met. Soc. China 2020, 30, 1535–1549. [Google Scholar] [CrossRef]
- Samadianfard, R.; Seifzadeh, D.; Habibi-Yangjeh, A.; Jafari-Tarzanagh, Y. Oxidized fullerene/sol-gel nanocomposite for corrosion protection of AM60B magnesium alloy. Surf. Coat. Technol. 2020, 385, 125400. [Google Scholar] [CrossRef]
- Huang, K.; Cai, S.; Xu, G.; Ren, M.; Wang, X.; Zhang, R.; Niu, S.; Zhao, H. Sol–gel derived mesoporous 58S bioactive glass coatings on AZ31 magnesium alloy and in vitro degradation behavior. Surf. Coat. Technol. 2014, 240, 137–144. [Google Scholar] [CrossRef]
- Galio, A.; Lamaka, S.; Zheludkevich, M.; Dick, L.; Müller, I.; Ferreira, M. Inhibitor-doped sol–gel coatings for corrosion protection of magnesium alloy AZ31. Surf. Coat. Technol. 2010, 204, 1479–1486. [Google Scholar] [CrossRef]
- Tang, H.; Xin, T.; Wang, F. Calcium Phosphate/Titania Sol-Gel Coatings on AZ31 Magnesium Alloy for Biomedical Applications. Int. J. Electrochem. Sci. 2013, 8, 8115–8125. [Google Scholar]
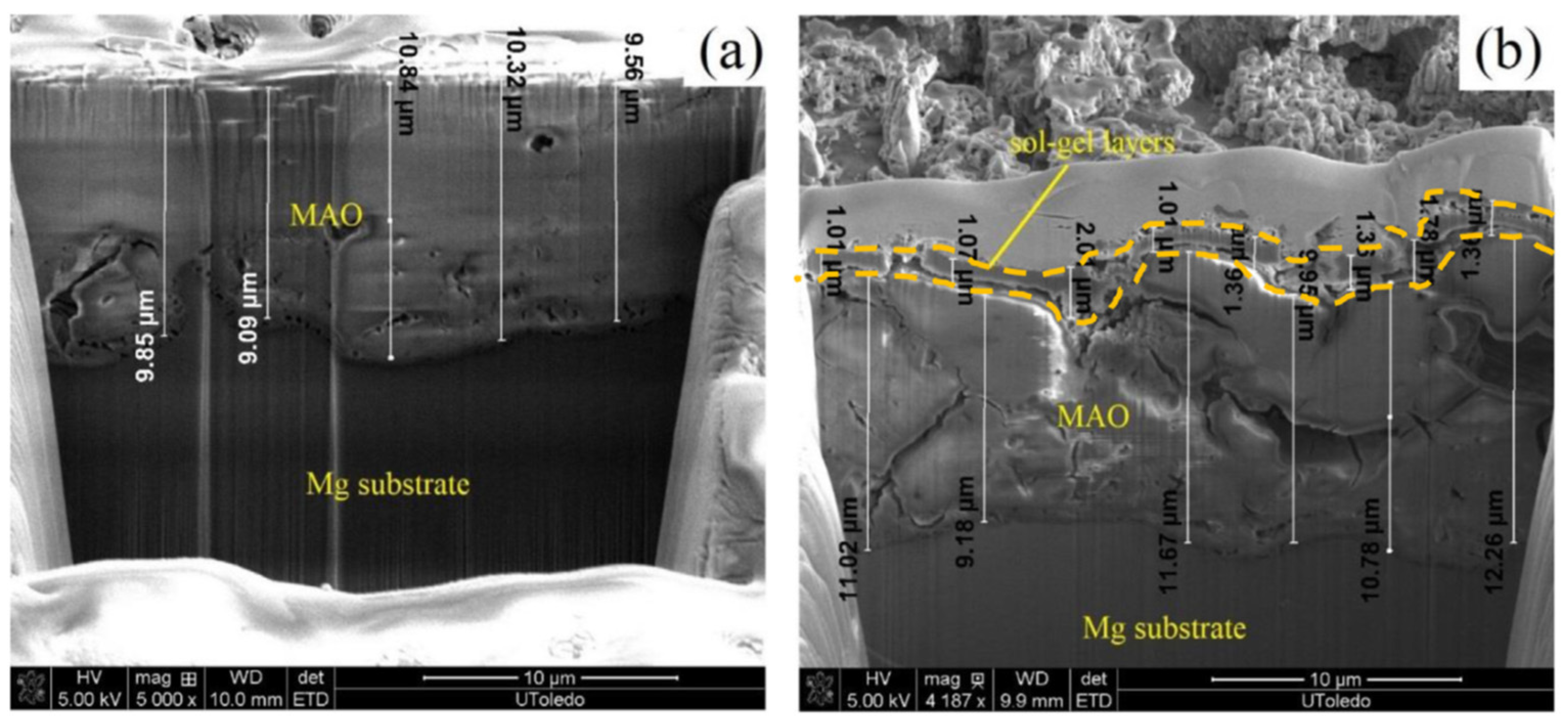
- Pezzato, L.; Rigon, M.; Martucci, A.; Brunelli, K.; Dabalà, M. Plasma Electrolytic Oxidation (PEO) as pre-treatment for sol-gel coating on aluminum and magnesium alloys. Surf. Coat. Technol. 2019, 366, 114–123. [Google Scholar] [CrossRef]
- Rojaee, R.; Fathi, M.; Raeissi, K. Controlling the degradation rate of AZ91 magnesium alloy via sol–gel derived nanostructured hydroxyapatite coating. Mater. Sci. Eng. C 2013, 33, 3817–3825. [Google Scholar] [CrossRef] [PubMed]
- Maret, W. Zinc in Cellular Regulation: The Nature and Significance of “Zinc Signals”. Int. J. Mol. Sci. 2017, 18, 2285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rueda, L.M.; Nieves, C.; Barrios, C.A.H.; Coy, A.E.; Viejo, F. Design of TEOS-GPTMS sol-gel coatings on rare-earth magnesium alloys employed in the manufacture of orthopaedic implants. J. Phys. Conf. Ser. 2016, 687, 012013. [Google Scholar] [CrossRef]
- Chmielewska, A.; MacDonald, T.; Ibrahim, H.; McManus, T.; Lindemann, J.L.; Smith, P.; Rong, L.; Luo, A.; Advincula, R.; Swieszkowski, W.; et al. Biocompatibility of a novel heat-treated and ceramic-coated magnesium alloy (Mg–1.2Zn–0.5Ca–0.5Mn) for resorbable skeletal fixation devices. MRS Commun. 2020, 10, 467–474. [Google Scholar] [CrossRef]
- Ibrahim, H.; Dehghanghadikolaei, A.; Advincula, R.; Dean, D.; Luo, A.; Elahinia, M. Ceramic coating for delayed degradation of Mg-1.2Zn-0.5Ca-0.5Mn bone fixation and instrumentation. Thin Solid Films 2019, 687, 137456. [Google Scholar] [CrossRef]
- Li, M.; Chen, Q.; Zhang, W.; Hu, W.; Su, Y. Corrosion behavior in SBF for titania coatings on Mg–Ca alloy. J. Mater. Sci. 2011, 46, 2365–2369. [Google Scholar] [CrossRef]
- Roy, A.; Singh, S.S.; Datta, M.K.; Lee, B.; Ohodnicki, J.; Kumta, P.N. Novel sol–gel derived calcium phosphate coatings on Mg4Y alloy. Mater. Sci. Eng. B Solid-State Mater. Adv. Technol. 2011, 176, 1679–1689. [Google Scholar] [CrossRef]


| Generation | Year | Properties | Biomaterials |
|---|---|---|---|
| First | ~1960 | Bioinert, Non-toxic. | Stainless steel, Cr-Co-Mo, NiTi, Ti6Al4V. |
| Second | 1970–1990 | Bioactive, Biodegradable. | Hydroxyapatite, Bioactive Glass, Magnesium alloys. |
| Third | ~2000 | Bioactive, Biodegradable, Cause specific cellular response. | Bioglass®, Biosilicates. |
| Fourth | ~2015 | Interactions with cellular signals. | Carbon-based materials, Conductive polymers. |
| Morphology | Synthesized Material | Applications | References |
|---|---|---|---|
| Coating | Hydroxyapatite (Ca5(PO4)3OH) | Biocompatibility improvement, Osseointegration, Antimicrobial. | [5,19,27,28,35,40,42] |
| Bioactive glass (SiO2-CaO-P2O5) | Biocompatibility improvement, Osseointegration. | [19,37,38] | |
| SiO2 | Biocompatibility improvement, Biocorrosion protection, Drug delivery. | [30,34,52,66] | |
| TiO2 | Biocorrosion protection, Biocompatibility improvement, Osseointegration. | [50,51,65] | |
| ZnO | Antimicrobial. | [49] | |
| Nb2O5 | Biocorrosion protection, Biocompatibility improvement. | [21,64] | |
| Particles | Bioactive glass (SiO2-CaO-P2O5) | Biocompatibility improvement. | [79,82] |
| Hydroxyapatite (Ca5(PO4)3OH) | Antimicrobial, Drug delivery, Biocompatibility improvement. | [80,81,82,85] | |
| SiO2 | Drug delivery. | [70,83] | |
| Matrix | SiO2 | Drug delivery. | [10,86] |
| Alginate/SiO2 | Drug delivery, Bio-artificial organ. | [88] | |
| Collagen/SiO2 | Drug delivery, Bio-artificial organ. | [90] | |
| Scaffold | Bioglass® | Tissue engineering, Osseointegration. | [91,92] |
| Hydroxyapatite/Polycaprolactone | Tissue engineering, Osseointegration. | [93] |
| Alloy Elements | Alloy | Composition |
|---|---|---|
| Mg–Al | AM60B | Al (5.5–6.5%), Mn (0.24–0.6%), Zn (0.22%) and <0.05% Si, Cu, Fe, Ni |
| AZ31 | Al (2.5–3.5%), Zn (0.6–1.4%), Mn (0.2%) and <0.1% Si, Cu, Ca, Fe, Ni | |
| AZ60 | Al (5.8–7.2%), Zn (0.4–1.5%), Mn (0.15%) and <0.1% Si, Cu, Ni, Fe | |
| AZ80 | Al (7.8–9.2%), Zn (0.2–0.8%), Mn (0.12%) and <0.1% Si, Cu, Fe, Ni | |
| AZ91D | Al (8.3–9.7%), Zn (0.35–1%), Mn (≥0.13%) and <0.1% Si, Cu, Fe, Ni | |
| Mg–Zn | ZE41 | Zn (3.5–5%), Zr (0.4–1%), Rare Earths (La, Ce, Ga 0.75–1.75%), 0.15% Mn |
| ZK30 | Zn (3%) and Zr (≥0.45%) | |
| ZK60 | Zn (6%) and Zr (≥0.45%) | |
| Mg3Zn | Zn (3%) | |
| Mg2Zn | Zn (2%) | |
| Mg–Ca | Mg–1.0Ca | Ca (1%) |
| Mg–0.6Ca | Ca (0.6%) | |
| Mg–Zn–Ca | Mg–0.5Zn–0.3Ca | Zn (0.5%), Ca (0.3%) |
| Mg–Rare Earths | Mg4Y | Y (4%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Hernán, J.P.; Torres, B.; López, A.J.; Rams, J. The Role of the Sol-Gel Synthesis Process in the Biomedical Field and Its Use to Enhance the Performance of Bioabsorbable Magnesium Implants. Gels 2022, 8, 426. https://doi.org/10.3390/gels8070426
Fernández-Hernán JP, Torres B, López AJ, Rams J. The Role of the Sol-Gel Synthesis Process in the Biomedical Field and Its Use to Enhance the Performance of Bioabsorbable Magnesium Implants. Gels. 2022; 8(7):426. https://doi.org/10.3390/gels8070426
Chicago/Turabian StyleFernández-Hernán, Juan Pablo, Belén Torres, Antonio Julio López, and Joaquín Rams. 2022. "The Role of the Sol-Gel Synthesis Process in the Biomedical Field and Its Use to Enhance the Performance of Bioabsorbable Magnesium Implants" Gels 8, no. 7: 426. https://doi.org/10.3390/gels8070426
APA StyleFernández-Hernán, J. P., Torres, B., López, A. J., & Rams, J. (2022). The Role of the Sol-Gel Synthesis Process in the Biomedical Field and Its Use to Enhance the Performance of Bioabsorbable Magnesium Implants. Gels, 8(7), 426. https://doi.org/10.3390/gels8070426









