The Quality in Psychiatric Care–Inpatient Staff Instrument: A Psychometric Evaluation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants and Procedures
2.3. The QPC-IPS Instrument
2.4. Data Analysis
3. Results
3.1. Sample Description
3.2. Factor Structure of the QPC-IPS
3.3. Internal Consistency
3.4. Test Retest
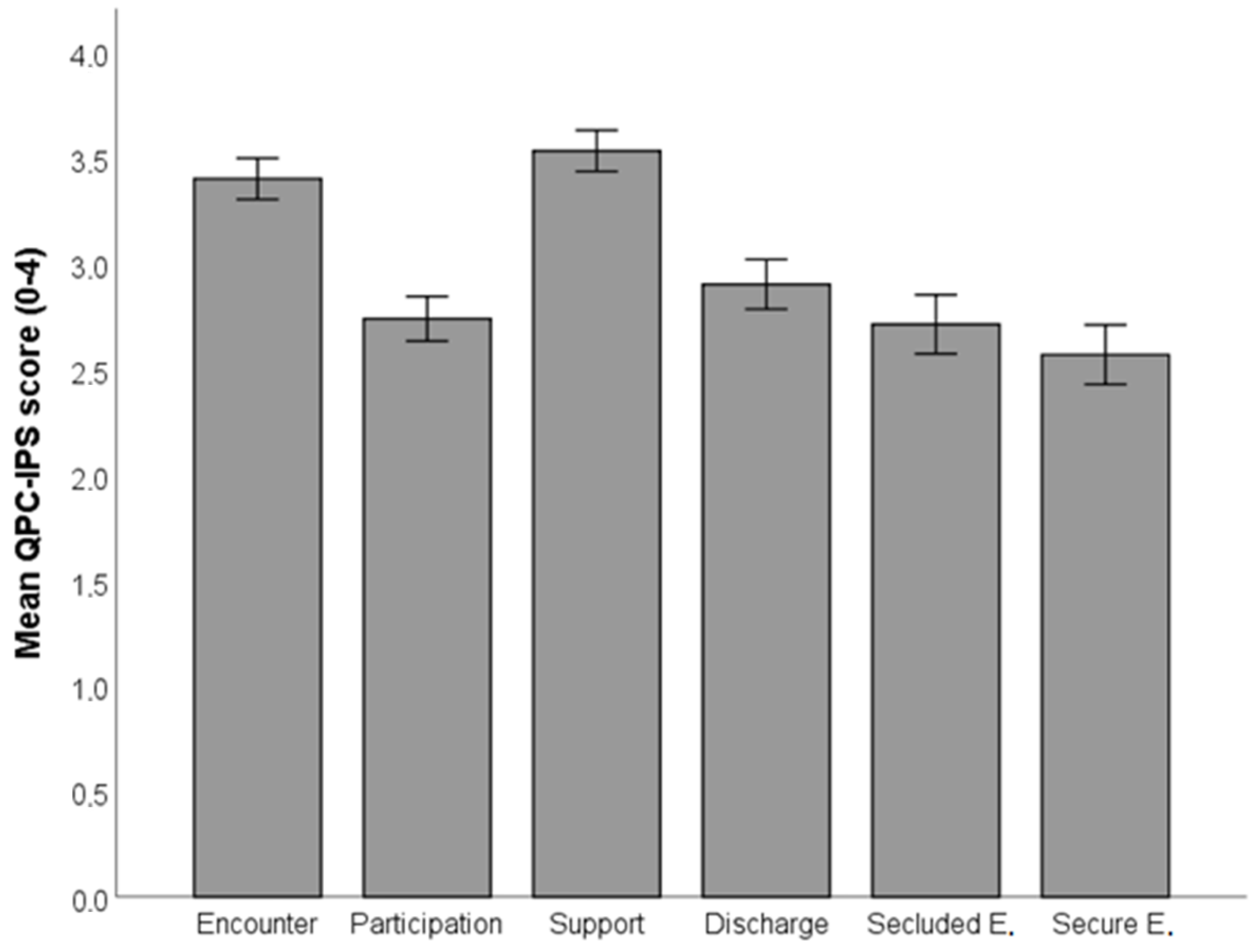
3.5. Description of Staff View of Inpatient Quality of Care
4. Discussion
4.1. Limitations
4.2. Implications for Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statements
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parameswaran, S.G.; Spaeth–Rublee, B.; Pincus, H.A. Measuring the quality of mental health care: Consensus perspectives from selected industrialized countries. Adm. Policy Ment. Health 2015, 42, 288–295. [Google Scholar] [CrossRef] [PubMed]
- Konderding, U. Which kind of psychometrics is adequate for patient satisfaction questionnaires? Patient Prefer. Adherence 2016, 10, 2083–2090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, D.E.; Tsugawa, Y.; Figueroa, J.F.; Jha, A.K. Association between the Centers for Medicare and Medicaid Services hospital star rating and patient outcomes. JAMA Intern. Med. 2016, 176, 848–850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnetz, B.B. Staff perception of the impact of health care transformation on quality of care. Int. J. Qual. Health Care 1999, 11, 345–351. [Google Scholar] [CrossRef] [Green Version]
- Farr, M.; Cressey, P. Understanding staff perspectives of quality of care in practice in healthcare. BMC Health Serv. Res. 2015, 15, 123. [Google Scholar] [CrossRef] [Green Version]
- Sanchez-Balcells, S.; Callarisa Roca, M.; Rodriguez-Zunino, N.; Puig-Llobert, M.; Lluch-Canut, M.-T.; Roldan-Merino, J.F. Psychometric properties of instruments measuring quality and satisfaction in mental health: A systematic review. J. Adv. Nurs. 2018, 74, 2497–2510. [Google Scholar] [CrossRef]
- Delaney, K.R.; Johnson, M.E.; Fogg, L. Development and testing of the combined assessment of psychiatric environments. A patient-centered quality measure for inpatient psychiatric treatment. J. Am. Psychiatr. Nurses Assoc. 2015, 21, 134–147. [Google Scholar] [CrossRef]
- Danielson, C.K.; Borckardt, J.J.; Grubaugh, A.L.; Pelic, C.G.; Hardesty, S.J.; Frueh, B.C. Quantifying staff and patient perceptions of quality of care improvements in the psychiatric inpatient setting: Preliminary psychometrics of a new measure. Psychol. Serv. 2008, 5, 1–10. [Google Scholar] [CrossRef]
- Schröder, A.; Lundqvist, L.-O. The Quality in Psychiatric Care–Forensic In-Patient Staff (QPC-FIPS) instrument: Psychometric properties and staff views of the quality of forensic psychiatric services in Sweden. Open J. Nurs. 2013, 3, 330–341. [Google Scholar] [CrossRef] [Green Version]
- Luther, L.; Fukui, S.; Garabrant, J.M.; Rollins, A.L.; Morse, G.; Henry, N.; Shimp, D.; Gearhart, T.; Salyers, M. Measuring quality of care in community mental health: Validation of concordant clinician and client quality-of-care scales. J. Behav. Health Serv. Res. 2019, 46, 64–79. [Google Scholar] [CrossRef]
- Granger, B.B.; Sandelowski, M.; Tahshjain, H.; Swedberg, K.; Ekman, I. A qualitative descriptive study of the work of adherence to chronic heart failure regimen: Patient and physician perspectives. J. Cardiovasc. Nurs. 2009, 24, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Sitzia, J.; Wood, N. Patient satisfaction: A review of issues and concepts. Soc. Sci. Med. 1997, 45, 1829–1843. [Google Scholar] [CrossRef]
- Boyer, L.; Baumstarck-Barrau, K.; Cano, N.; Zendjidjian, X.; Belzeaux, R.; Limousin, S.; Magalon, D.; Samuelian, J.C.; Lancon, C.; Auquier, P. Assessment of psychiatric inpatient satisfaction: A systematic review of self-reported instruments. Eur. Psychiatry 2009, 24, 540–549. [Google Scholar] [CrossRef] [PubMed]
- Shiva, A.; Haden, S.C.; Brooks, J. Psychiatric civil and forensic inpatient satisfaction with care: The impact of provider and recipient characteristics. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 979–987. [Google Scholar] [CrossRef]
- Schröder, A.; Wilde-Larsson, B.; Ahlström, G.; Lundqvist, L.-O. Psychometric properties of the instrument Quality in Psychiatric Care and descriptions of quality of care among in-patients. Int. Health Care Qual. Assur. 2010, 23, 554–570. [Google Scholar] [CrossRef]
- Lundqvist, L.-O.; Schröder, A. Patient and staff views of quality in forensic psychiatric in-patient care. J. Forensic Nurs. 2015, 11, 51–58. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A practical guide to their development and use, 2nd ed.; Oxford University Press: Oxford, UK, 2003. [Google Scholar]
- Lundqvist, L.-O.; Suryani; Anna, N.; Rafiyah, I.; Schröder, A. Indonesian adaptation of the Quality in Psychiatric Care–In-patient (QPC-IP) instrument: Psychometric properties and factor structure. Asian J. Psychiatr. 2018, 34, 1–5. [Google Scholar] [CrossRef]
- Lundqvist, L.-O.; Suryani; Hermiati, D.; Sutini, T.; Schröder, A. A psychometric evaluation of the Indonesian version of the Quality in Psychiatric Care–Inpatient Staff (QPC-IPS) instrument. Asian J. Psychiatr. 2019, 46, 29–33. [Google Scholar] [CrossRef]
- Sanchez-Balcells, S.; Lundqvist, L.-O.; Roldan-Merino, J.F.; Lluch-Canut, M.-T.; Calarisa Roca, M.; Rodriguez Zunino, N.; Tomas Jimenez, M.; Schröder, A.; Puig-Llobet, M. A Spanish adaptation of the Quality in Psychiatric Care–Inpatient Staff (QPC-IPS) instrument: Psychometric properties and factor structure. An. Sist. Sanit. Navar. 2020, 43, 307–321. [Google Scholar]
- Lundqvist, L.-O.; Riiskjaer, E.; Lorentzen, K.; Schröder, A. Factor structure and psychometric properties of the Danish adaptation of the Quality in Psychiatric Care–Forensic In-patient Staff (QPC-FIPS). Open J. Nurs. 2014, 4, 878–885. [Google Scholar] [CrossRef] [Green Version]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef] [Green Version]
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw–Hill: New York, NY, USA, 1994. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. LISREL 8: User’s Reference Guide, 2nd ed.; Scientific Software International: Chicago, IL, USA, 1996. [Google Scholar]
- Jöreskog, K.G.; Sörbom, D. PRELIS—A Program for Multivariate Data Screening and Data Summarization. A Preprocessor for LISREL, 2nd ed.; Scientific Software Inc.: Chicago, IL, USA, 1988. [Google Scholar]
- Satorra, A.; Bentler, P.M. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika 2001, 66, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Cangur, S.; Ercan, I. Comparison of model fit indices used in structural equation modeling under multivariate normality. J. Mod. App. Stat. Methods 2015, 14, 52–167. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Jones, J.; Nolan, P.; Bowers, L.; Simpson, A.; Hackney, D.; Bhui, K. Psychiatric wards: Places of safety? J. Psychiatr. Ment. Health Nurs. 2010, 17, 124–130. [Google Scholar] [CrossRef]
- Stenhouse, R.C. “Safe enough in here?”: Patients’ expecations and experinces of feeling safe in an acute psychiatric inpatient ward. J. Clin. Nurs. 2013, 22, 3109–3119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Samartzis, L.; Talias, M.A. Assessing and improving the quality in mental health services. Int. J. Environ. Res. Public Health 2020, 17, 249. [Google Scholar] [CrossRef] [Green Version]
- Pelto-Piri, V.; Wallsten, T.; Hylén, U.; Nikban, I.; Kjellin, L. Feeling safe or unsafe in the psychiatric inpatient care, a hospital-based qualitative interview study with inpatients in Sweden. Int. J. Ment. Health Syst. 2019, 13, 23. [Google Scholar] [CrossRef]
- Melnyk, B.; Gallagher-Ford, L.; Long, L.E.; Fineout-Overholt, E. The establishment of evidence-based practice competencies for practicing registered nurses and advanced practice nurses in real-world clinical settings: Proficiencies to improve healthcare quality, reliability, patient outcomes, and costs. Worldviews Evid.-Based Nurs. 2014, 11, 5–15. [Google Scholar] [CrossRef]
- Aiken, L.H.; Sloane, D.M.; Bruyneel, L.; Van den Heede, K.; Griffiths, P.; Busse, R.; Diomidus, M.; Kinnunen, J.; Kózka, M.; Lesaffre, E.; et al. Nurse staffing and education and hospital mortality in nine European countries: A retrospective observational study. Lancet 2014, 383, 1824–1830. [Google Scholar] [CrossRef] [Green Version]
- Tibaut, B.; Dewa, L.H.; Ramtale, S.C.; D’Lima, D.; Adam, S.; Ashrafian, H.; Darzi, A.; Archer, S. Patient safety in inpatient mental health settings: A systematic review. BMJ Open 2019, 9, e030230. [Google Scholar] [CrossRef] [PubMed]
- Hair, J.F.; Anderson, R.E.; Tatham, R.L.; Black, W.C. Multivariate Data Analysis with Readings; Prentice Hall: Hoboken, NJ, USA, 1995. [Google Scholar]
- Rindfuss, R.R.; Choe, M.K.; Tsuya, N.O.; Bumpass, L.L.; Tamaki, E. Do low survey response rates bias results? Evidence from Japan. Demogr. Res. 2015, 32, 797–828. [Google Scholar] [CrossRef] [Green Version]
- Shannon, S.E.; Mitchell, P.H.; Cain, K.C. Patients, nurses, and physicians have differing views of quality of critical care. J. Nurs. Scholarsh. 2002, 34, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, B.; Dunn, L. The declaration of Helsinki on medical research involving human subjects: A review of seventh revision. J. Nepal Health Res. Counc. 2019, 17, 548–552. [Google Scholar] [CrossRef] [PubMed]
| QPC-IPS Dimension | MT1 | SDT1 | MT2 | SDT2 | ICC | 95% CI | |
|---|---|---|---|---|---|---|---|
| 1. | Encounter | 3.39 | 0.43 | 3.45 | 0.38 | 0.89 | 0.84–0.94 |
| 2. | Participation | 2.65 | 0.56 | 2.64 | 0.48 | 0.92 | 0.87–0.95 |
| 3. | Discharge | 2.82 | 0.60 | 2.80 | 0.57 | 0.82 | 0.72–0.89 |
| 4. | Support | 3.53 | 0.50 | 3.53 | 0.46 | 0.89 | 0.84–0.94 |
| 5. | Secluded Environment | 2.63 | 0.70 | 2.67 | 0.60 | 0.75 | 0.61–0.86 |
| 6. | Secure Environment | 2.58 | 0.63 | 2.64 | 0.61 | 0.84 | 0.75–0.91 |
| Total QPC | 2.98 | 0.42 | 3.00 | 0.36 | 0.95 | 0.93–0.97 |
| QPC-IPS Items | Loadings | Alpha | Mean | SD | ||
|---|---|---|---|---|---|---|
| Total QPC-IPS (30 items) | 0.94 | 3.03 | 0.46 | |||
| 1. Encounter (8 items) | 0.90 | 3.40 | 0.50 | |||
| 7. | Patients have the opportunity to talk when needed | 0.67 | 3.29 | 0.72 | ||
| 10. | Staff are involved | 0.83 | 3.44 | 0.68 | ||
| 11. | Staff treat the patients with warmth and consideration | 0.88 | 3.48 | 0.64 | ||
| 12. | Staff care if the patients get angry | 0.88 | 3.37 | 0.71 | ||
| 15. | Staff respect the patients | 0.89 | 3.58 | 0.57 | ||
| 18. | Staff show they understand the patients’ feelings | 0.81 | 3.28 | 0.66 | ||
| 20. | Staff have time to listen to the patients | 0.69 | 3.14 | 0.73 | ||
| 25. | Staff are concerned about the patients’ care | 0.86 | 3.64 | 0.54 | ||
| 2. Participation (8 items) | 0.87 | 2.74 | 0.55 | |||
| 1. | Patients can influence their own care and treatment | 0.75 | 2.60 | 0.70 | ||
| 5. | Patients’ opinion of the right care is respected | 0.76 | 2.70 | 0.71 | ||
| 6. | Patients are involved in decisions about their care | 0.75 | 2.67 | 0.74 | ||
| 13. | Benefit drawn from earlier experience of treatment | 0.64 | 2.80 | 0.76 | ||
| 14. | Patients get to recognise signs of deterioration | 0.75 | 2.65 | 0.76 | ||
| 27. | Patients receive information in a way that they can understand | 0.80 | 2.96 | 0.72 | ||
| 29. | Patients are informed about their mental health problems | 0.79 | 2.83 | 0.74 | ||
| 30. | Patients receive information about treatment alternatives | 0.67 | 2.71 | 0.88 | ||
| 3. Discharge (4 items) | 0.82 | 2.90 | 0.61 | |||
| 8. | Patients are offered planning of their continued treatment | 0.81 | 2.94 | 0.80 | ||
| 16. | Patients are offered a follow-up after discharge | 0.66 | 3.15 | 0.79 | ||
| 17. | Patients are given help in finding an occupation | 0.76 | 2.31 | 0.88 | ||
| 21. | Patients know where to turn after discharge | 0.67 | 3.21 | 0.73 | ||
| 4. Support (4 items) | 0.75 | 3.54 | 0.50 | |||
| 19. | Staff prevent the patients from hurting each other | 0.66 | 3.52 | 0.61 | ||
| 22. | Staff prevent the patients from hurting themselves | 0.73 | 3.47 | 0.61 | ||
| 23. | Nothing shameful about having mental problems | 0.98 | 3.64 | 0.61 | ||
| 24. | Staff tell patients shame must not interfere with seeking treatment | 0.87 | 3.51 | 0.67 | ||
| 5. Secluded environment (3 items) | 0.65 | 2.71 | 0.72 | |||
| 3. | Patients have access to a place that is private | 0.71 | 2.83 | 1.05 | ||
| 26. | Patients have their own room | 0.66 | 2.25 | 0.79 | ||
| 28. | Private place where patients can receive visits from family | 0.68 | 3.07 | 0.96 | ||
| 6. Secure environment (3 items) | 0.76 | 2.57 | 0.73 | |||
| 2. | Security is high at the ward | 0.66 | 2.75 | 1.00 | ||
| 4. | Patients feel secure with fellow patients | 0.93 | 2.73 | 0.82 | ||
| 9. | Patients are not disturbed by fellow patients | 0.79 | 2.23 | 0.82 | ||
| QPC-IPS Dimension | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|
| 1. | Encounter | 1.00 | |||||
| 2. | Participation | 0.67 | 1.00 | ||||
| 3. | Discharge | 0.58 | 0.78 | 1.00 | |||
| 4. | Support | 0.70 | 0.56 | 0.44 | 1.00 | ||
| 5. | Secluded environment | 0.46 | 0.67 | 0.57 | 0.31 | 1.00 | |
| 6. | Secure environment | 0.54 | 0.59 | 0.48 | 0.34 | 0.55 | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, A.; Lundqvist, L.-O. The Quality in Psychiatric Care–Inpatient Staff Instrument: A Psychometric Evaluation. Healthcare 2022, 10, 1213. https://doi.org/10.3390/healthcare10071213
Schröder A, Lundqvist L-O. The Quality in Psychiatric Care–Inpatient Staff Instrument: A Psychometric Evaluation. Healthcare. 2022; 10(7):1213. https://doi.org/10.3390/healthcare10071213
Chicago/Turabian StyleSchröder, Agneta, and Lars-Olov Lundqvist. 2022. "The Quality in Psychiatric Care–Inpatient Staff Instrument: A Psychometric Evaluation" Healthcare 10, no. 7: 1213. https://doi.org/10.3390/healthcare10071213
APA StyleSchröder, A., & Lundqvist, L.-O. (2022). The Quality in Psychiatric Care–Inpatient Staff Instrument: A Psychometric Evaluation. Healthcare, 10(7), 1213. https://doi.org/10.3390/healthcare10071213






