Should We Hastily Adopt Public Access Defibrillation?
Gedanken zum Artikel «Laiendefibrillation–häufig propagiert, aber zu selten eingesetzt» Kardiovaskuläre Medizin 2006;2:54–67
References
- Stiell, I.G.; Wells, G.A.; Field, B.J.; et al. Improved out-of-hospital cardiac arrest survival through the inexpensive optimization of an existing defibrillation program: OPALS study phase II. Ontario Prehospital Advanced Life Support. JAMA 1999, 281, 1175–1181. [Google Scholar] [CrossRef]
- Katz, E.; Horstmann, M.; Kehtari, R.; et al. Frühzeitige Defibrillation durch Rettungsassistenten bei kardialen Notfällen mit externen halbautomatischen Defibrillatoren. Der Notartzt 2001, 17, 167–170. [Google Scholar] [CrossRef]
- Stotz, M.; Albrecht, R.; Zwicker, G.; et al. EMS defibrillation-first policy may not improve outcome in out-of-hospital cardiac arrest. Resuscitation 2003, 58, 277–282. [Google Scholar] [CrossRef] [PubMed]
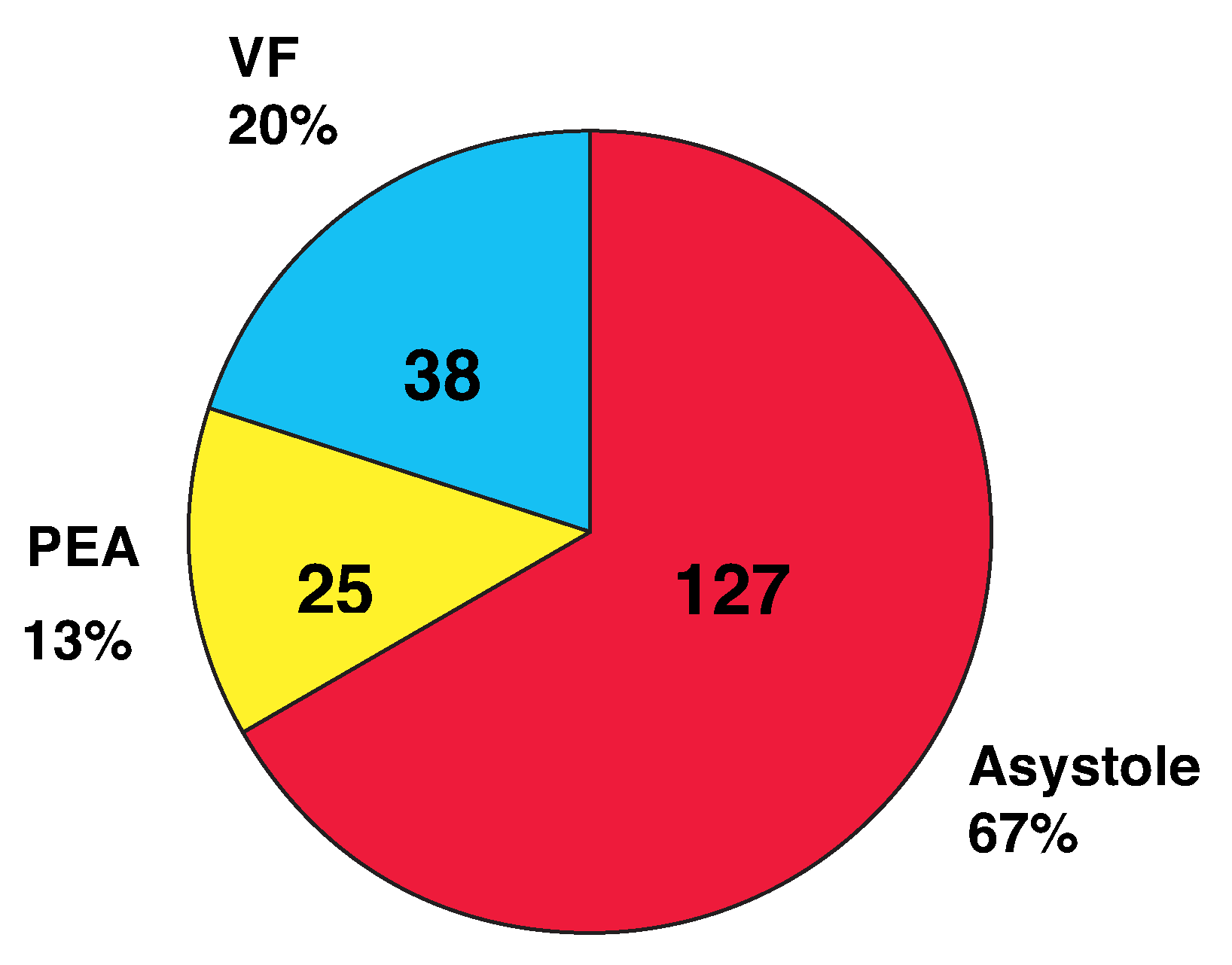
- Katz, E.; Metzger, J.T.; Kappenberger, L.; et al. Is ventricular fibrillation the most common initial rhythm in out-of-hospital cardiac arrest? Resuscitation 2004, 62, 403. [Google Scholar]
- Vilke, G.M.; Chan, T.C.; Dunford, J.V.; et al. M.; Chan, T.C.; Dunford, J.V.; et al. The three-phase model of cardiac arrest as applied to ventricular fibrillation in a large, urban emergency medical services system. Resuscitation 2005, 64, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Wik, L.; Hansen, T.B.; Fylling, F.; et al. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with outof-hospital ventricular fibrillation: A randomized trial. JAMA 2003, 289, 1389–1395. [Google Scholar] [CrossRef] [PubMed]
- Bruesch, M. Reanimationsdatenbank Schweiz nach Utsteinstyle. SAEZ 2005, 86, 2429–2433. [Google Scholar]
© 2006 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Katz, E.; Sierro, C.; Metzger, J.-T.; Fishmann, D.; Kehtari, R.; Kappenberger, L. Should We Hastily Adopt Public Access Defibrillation? Cardiovasc. Med. 2006, 9, 243. https://doi.org/10.4414/cvm.2006.01181
Katz E, Sierro C, Metzger J-T, Fishmann D, Kehtari R, Kappenberger L. Should We Hastily Adopt Public Access Defibrillation? Cardiovascular Medicine. 2006; 9(6):243. https://doi.org/10.4414/cvm.2006.01181
Chicago/Turabian StyleKatz, E., C. Sierro, J. -T. Metzger, D. Fishmann, R. Kehtari, and L. Kappenberger. 2006. "Should We Hastily Adopt Public Access Defibrillation?" Cardiovascular Medicine 9, no. 6: 243. https://doi.org/10.4414/cvm.2006.01181
APA StyleKatz, E., Sierro, C., Metzger, J.-T., Fishmann, D., Kehtari, R., & Kappenberger, L. (2006). Should We Hastily Adopt Public Access Defibrillation? Cardiovascular Medicine, 9(6), 243. https://doi.org/10.4414/cvm.2006.01181



