Case Report
A 25-year-old woman with recurrent palpitations and documented drug-refractory narrow complex tachycardia was referred to our clinic for treatment. The surface ECG during sinus rhythm and transthoracic echocardiography showed unremarkable findings. Based on the ECG tracings during the tachycardia, AT was suspected to be the underlying rhythm disorder.
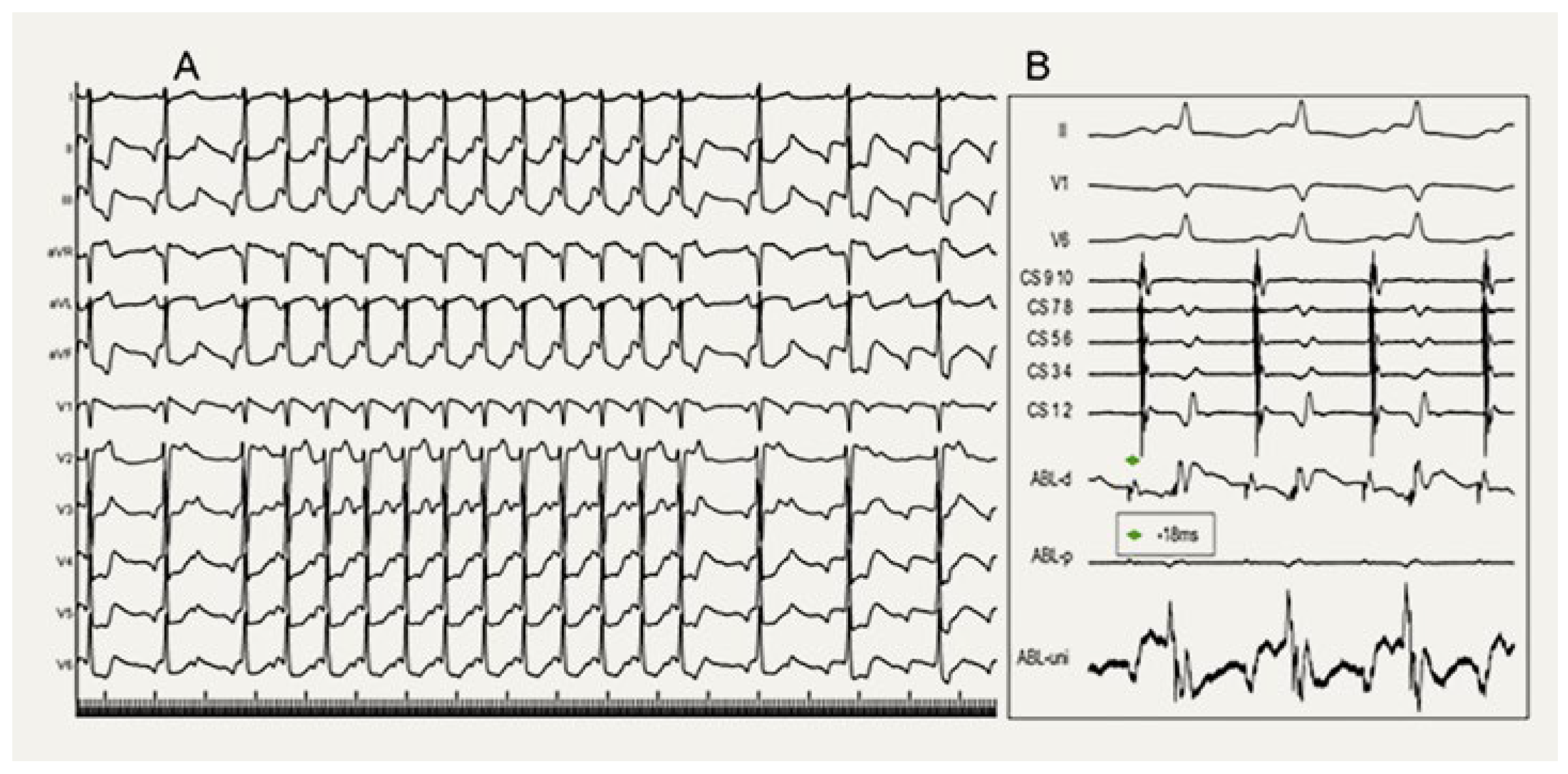
After obtaining written informed consent, an electrophysiologic study was performed, which revealed a spontaneously occurring narrow complex tachycardia alternating with sinus rhythm (
Figure 1A). The CARTO™-3D mapping system (Biosense Webster, Irvine, CA, USA) was used with a 7-French, 4-mm tip ablation catheter (Navistar
®, Biosense Webster) and a steerable, decapolar coronary sinus catheter (Decanav
®, Biosense Webster).
The baseline intracardiac intervals were within normal limits (atrial-His bundle [AH] interval: 102 ms, His bundle-ventricular [HV] interval: 50 ms). A SVT with a cycle length of 490 ms was spontaneously and repeatedly induced by premature atrial beats with an AH interval of 180 ms. Programmed atrial stimulation could not be performed because the tachycardia turned into an incessant form. The veno-arterio-venous entrainment maneuver was inconclusive because short ventricular pacing sequences terminated the tachycardia, indicating that an AT was unlikely [
1]. On the other hand, premature ventricular contractions while the His bundle was refractory did not advance atrial activation, ruling out a retrograde accessory pathway. The intracardiac measurements during the tachycardia (AH: 180 ms, His bundle-atrial [HA] interval: 360 ms, ventriculoatrial [VA] interval: 310 ms) favored an atypical (fast-slow type) AVNRT (
Figure 1B) [
2,
3]. Slow pathway ablation was performed at the typical location using radiofrequency energy with a Navistar
® catheter at a target temperature of 52 °C and a maximum power output of 50 W during the tachycardia. Radiofrequency treatment terminated the tachycardia immediately. After 60 seconds of ablation, during which multiple slow junctional beats were observed, AVNRT was no longer inducible, and no AH-jump was detected during programmed atrial pacing.
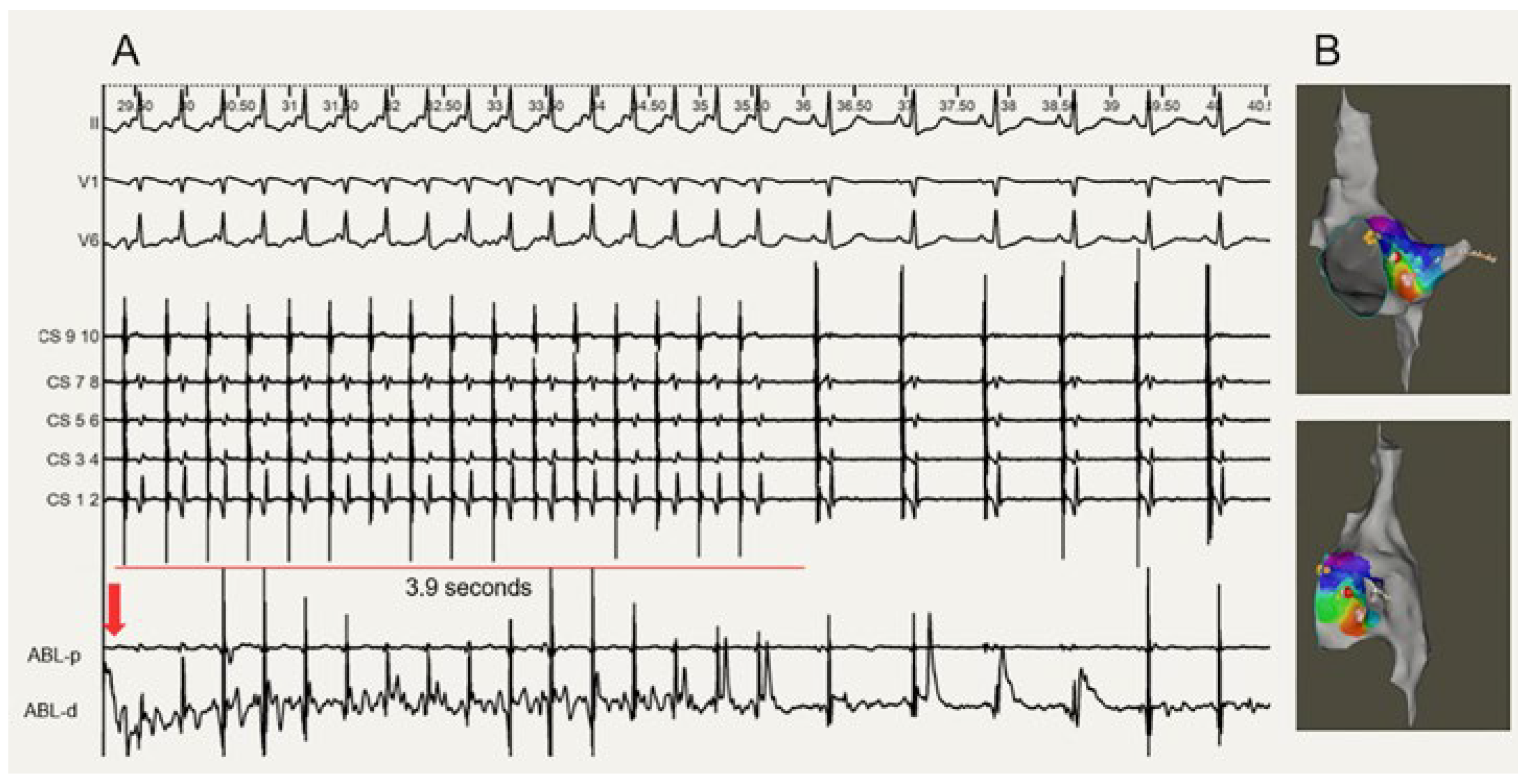
Following successful ablation of the atypical AVNRT, a second tachycardia with similar P wave morphology was induced by atrial burst pacing under isoprenaline infusion during the waiting period. However, this tachycardia started without an AH-jump and showed VA unlinking with intermittent 2:1 or 3:1 conduction, which is consistent with an AT diagnosis (
Figure 2). A high-density mapping of the local area revealed a focal origin anteroinferior to the slow pathway region, with a strong local activation signal at the distal pole of the ablation catheter (16 mm distance) (
Figure 3B). The tachycardia was successfully terminated via ablation within five seconds (
Figure 3A). There was no evidence of junctional rhythm or atrioventricular (AV) block during the application of radiofrequency. No tachycardias were inducible thereafter, and the patient reported no recurrences during the 3-month follow-up period (
Figure 5).
Discussion
This case report demonstrates the occurrence of two different types of SVTs occurring in the same patient, both of which could be successfully ablated in adjacent but clearly distinct areas within the right atrium. In clinical practice, the coexistence of AVNRT with other types of arrhythmia is not uncommon, with atrial fibrillation and atrial flutter being the most common [
4]. However, coexisting symptomatic focal AT is rare, especially if it originates adjacent to the slow-pathway region. We diagnosed both an atypical AVNRT induced by spontaneous atrial premature beats and a focal AT located anteroinferior to the slow-pathway location.
A premature atrial beat, caused by the same focus of the AT with the same P wave morphology, followed by a significant AH-jump, provided a critical hint for the identification of the slow pathway [
2,
3]. Characteristic findings of an atypical fast-slow AVNRT include a HA interval >70 ms, AH <200 ms, and AH<HV [
6]. Nevertheless, the presence of a slow pathway does not necessarily imply that it is a component of a tachycardia circuit. Ventricular pacing maneuvers, such as measuring the post-pacing interval minus tachycardia cycle length, were reported to be useful in diagnosing the involvement of slow pathways in the tachycardia circuit [
6]. However, in our case, due to the termination of the tachycardia, we were unable to perform them successfully. Our observation that premature ventricular contractions while the His bundle was refractory did not advance atrial activation nevertheless excluded a retrograde accessory pathway. In addition, we consistently documented the termination of the fast-slow AVNRT with a QRS signal, i.e., in the retrograde limb of the presumed reentry tachycardia, an observation that is common with fast-slow AVNRT but does not exclude AT. Nevertheless, ablation at the typical slow-pathway location terminated the fast-slow tachycardia, induced multiple junctional beats, and eliminated the AH-jump, supporting the diagnosis and treatment efficacy [
7].
Atrial tachycardia was revealed after successful slow-pathway ablation during the waiting period on isoprenaline infusion. Criteria supporting this diagnosis were: 1) Automatic AT could be neither initiated nor terminated by programmed stimulation; 2) changes in atrial-atrial interval and VA unlinking with a wide range of coupling intervals with AV 2:1 or 3:1 conduction were demonstrated; 3) local atrial activation recorded from the tip of the ablation catheter preceded P wave onset by at least 18 ms.
The AT in our case originated near the slow-pathway region.
Figure 4 shows that the slow pathway was captured antidromically in the first beat and orthodromically during the clinical tachycardia. It is possible that the atrial ectopic beats collided into the reentry circuit and terminated the fast-slow reentry, leading to an AV node refractoriness resulting in the termination of the AVNRT [
7]. Alternatively, the AV node fatigue phenomenon may explain the termination, which is more commonly thought to be rate-dependent [
8]. However, the tachycardia cycle length in our case was rather long, and therefore, AV node fatigue was unlikely. As a result, we strongly suspect that the atrial focus that caused the AT both triggered and terminated the AVNRT in our case.
Figure 1.
Fast-slow atrioventricular-nodal reentrant tachycardia (AVNRT) induced by spontaneous premature atrial beats. (A) Twelve-lead electrocardiogram (ECG) of an AVNRT episode (tracing speed 25 mm/s). Two premature atrial beats induced AVNRT; the first premature atrial complex (PAC) caused a significant PR prolongation, indicating the presence of a slow pathway; the second PAC conducted antegrade over the fast pathway and induced the long RP tachycardia, which was proved to be a fast-slow AVNRT by ECG tracing shown in B. (B) Surface ECG leads II, V1, and V6 and endocardial recordings during atrial tachycardia (recording speed 100 mm/s). CS: Decapolar catheter (CS 1-10) in the coronary sinus. HBE: Quadripolar electrode placed at the His bundle site, recording an atrial-His bundle interval-jump of 85 ms following the first atrial premature beat. AA: atrial-atrial interval; AH: Atrial-His bundle interval; HA: His bundle-atrial interval.
Figure 1.
Fast-slow atrioventricular-nodal reentrant tachycardia (AVNRT) induced by spontaneous premature atrial beats. (A) Twelve-lead electrocardiogram (ECG) of an AVNRT episode (tracing speed 25 mm/s). Two premature atrial beats induced AVNRT; the first premature atrial complex (PAC) caused a significant PR prolongation, indicating the presence of a slow pathway; the second PAC conducted antegrade over the fast pathway and induced the long RP tachycardia, which was proved to be a fast-slow AVNRT by ECG tracing shown in B. (B) Surface ECG leads II, V1, and V6 and endocardial recordings during atrial tachycardia (recording speed 100 mm/s). CS: Decapolar catheter (CS 1-10) in the coronary sinus. HBE: Quadripolar electrode placed at the His bundle site, recording an atrial-His bundle interval-jump of 85 ms following the first atrial premature beat. AA: atrial-atrial interval; AH: Atrial-His bundle interval; HA: His bundle-atrial interval.
Figure 2.
Atrial tachycardia (AT) induced by atrial extrastimuli during isoprenaline infusion after successful slow-pathway ablation. (A) Twelve-lead electrocardiogram (ECG) of the AT episode (tracing speed 25 mm/s). Note that AT started with no significant PR prolongation. (B) Surface ECG leads I, aVF, and V1 and endocardial recordings during AT (recording speed 50 mm/s). CS: Decapolar catheter (CS 1-10) in the coronary sinus. ABL-d: Ablation distal. ABL-p: Ablation proximal. ABL-uni: Ablation unipolar.
Figure 2.
Atrial tachycardia (AT) induced by atrial extrastimuli during isoprenaline infusion after successful slow-pathway ablation. (A) Twelve-lead electrocardiogram (ECG) of the AT episode (tracing speed 25 mm/s). Note that AT started with no significant PR prolongation. (B) Surface ECG leads I, aVF, and V1 and endocardial recordings during AT (recording speed 50 mm/s). CS: Decapolar catheter (CS 1-10) in the coronary sinus. ABL-d: Ablation distal. ABL-p: Ablation proximal. ABL-uni: Ablation unipolar.
Figure 3.
Successful ablation of the atrial tachycardia (AT) focus. (A) Endocardial recording of the successful ablation in the target region. Red arrow: Ablation start; ABL-d: Ablation distal; ABL-p: Ablation proximal; ABL-uni: Ablation unipolar. (B). Electroanatomical endocardial mapping demonstrated the distinct AT focus adjacent to but clearly different from the slow pathway ablation location. Upper: Left anterior oblique projection; Lower: Right anterior oblique projection.
Figure 3.
Successful ablation of the atrial tachycardia (AT) focus. (A) Endocardial recording of the successful ablation in the target region. Red arrow: Ablation start; ABL-d: Ablation distal; ABL-p: Ablation proximal; ABL-uni: Ablation unipolar. (B). Electroanatomical endocardial mapping demonstrated the distinct AT focus adjacent to but clearly different from the slow pathway ablation location. Upper: Left anterior oblique projection; Lower: Right anterior oblique projection.
Figure 4.
Slow pathway responded to spontaneous premature atrial beats during onset and termination, a schematic speculation. Blue lines show the conduction through the atrium (A), atrioventricular node (AVN), His bundle, and ventricle (V). A1 is a spontaneous premature atrial complex. It conducted through the slow pathway during the first beat and through the fast pathway during the second beat. The atypical atrioventricular-nodal reentrant tachycardia was terminated, as speculated by the same spontaneous atrial premature beat collision with the AVN reentry.
Figure 4.
Slow pathway responded to spontaneous premature atrial beats during onset and termination, a schematic speculation. Blue lines show the conduction through the atrium (A), atrioventricular node (AVN), His bundle, and ventricle (V). A1 is a spontaneous premature atrial complex. It conducted through the slow pathway during the first beat and through the fast pathway during the second beat. The atypical atrioventricular-nodal reentrant tachycardia was terminated, as speculated by the same spontaneous atrial premature beat collision with the AVN reentry.
Figure 5.
Timeline. AVNRT: Atrioventricular-nodal reentrant tachycardia; AT: Atrial tachycardia; ECG: Electrocardiogram; EPS: Electrophysiology study; SVT: Supraventricular tachycardia; UCG: Ultrasonic cardiogram.
Figure 5.
Timeline. AVNRT: Atrioventricular-nodal reentrant tachycardia; AT: Atrial tachycardia; ECG: Electrocardiogram; EPS: Electrophysiology study; SVT: Supraventricular tachycardia; UCG: Ultrasonic cardiogram.
Of note, the HV interval in this young patient was 50 ms, which is within the normal range but unusually long for his age. Although there were no clinical symptoms or signs of AV block, the patient will continue to be closely monitored, considering previous observations [
9]. Furthermore, low-voltage areas are frequently seen in reentrant ATs [
10]. In our case, however, no localized low-voltage substrate was found around the tachycardia origin.