Abstract
We present the case of a 50-year-old woman with a chemotherapeutically treated primary mediastinal lymphoma and circumferential pericardial effusion, whose echocardiogram revealed unusual intrapericardial colour and pulsed-wave Doppler flow signals. Insights on workup and hypotheses are discussed.
Case Description
A 50-year-old woman with a 2-year history of primary mediastinal large B-cell lymphoma treated with six chemotherapy cycles EPOCH-R (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin and rituximab) underwent follow-up thoracic computed tomography (CT). A moderately sized circumferential pericardial effusion was visualised but no lymphoma recurrence was detected. Past medical history included surgical closure of a type 2 atrial septal defect (ASD) more than 20 years ago.
The patient presented herself in good general condition with no clinical signs of tamponade or heart failure. A broad laboratory workup turned out normal and the electrocardiogram showed a sinus rhythm, low QRS and voltage biphasic T waves in I, aVL and V5-V6.
Transthoracic echocardiogram (TTE) confirmed a moderately sized circumferential serous pericardial effusion with no features of tamponade. Unusual prominent colour Doppler signals were seen within the pericardial space adjacent to the right ventricle free wall and directed towards the apex in systole (Figure 1, supplementary material: video clips). There was no evidence for communication with adjacent cardiac chambers. Flow signals were confirmed on pulsed-wave Doppler with maximal flow velocity of 100 cm/s. (Figure 2). Left ventricular dimensions and ejection fraction were normal while the right atrium and right ventricle were mildly dilated.
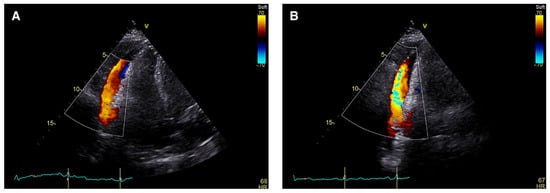
Figure 1.
Transthoracic echocardiogram: apical 4-chamber view, colour Doppler signal within the pericardial effusion adjacent to the free wall of the right ventricle during ventricular systole.
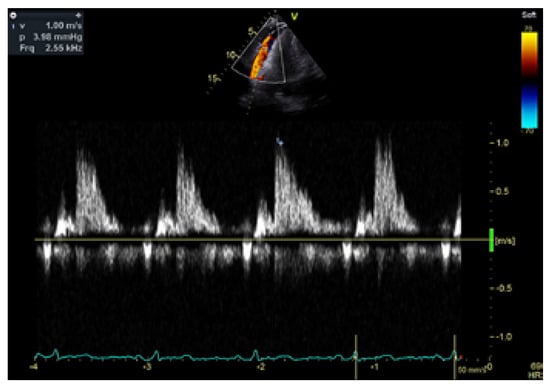
Figure 2.
Pulsed-wave Doppler of the intrapericardial flow from a modified apical view. The sample volume is placed laterally to the right ventricle.
Cardiac magnetic resonance imaging (CMR) with cine, flow and tissue characterisation sequences excluded any disease of the parietal or visceral pericardium, right ventricular wall anomalies, myocardial oedema or relevant late gadolinium enhancement (Figure 3 and Figure 4), but confirmed a mild circular pericardial effusion without evidence of pericardial haematoma or myocardial rupture. Myocardial extracellular volume by native and post-contrast T1-mapping was normal with 24%. Qp/ Qs was 0.95 calculated by aortic flow and flow across the pulmonary trunk by phase contrast flow velocity mapping. A gated coronary angio-CT did not find any coronary artery fistula or anomalous communication.
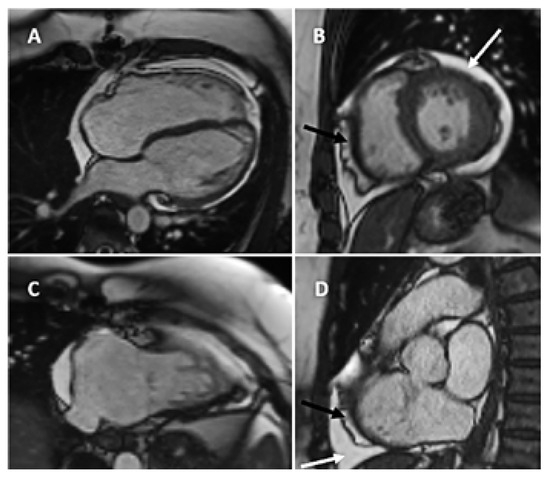
Figure 3.
CMR steady-state free precession cine still frames. (A) Four chamber view enddiastolic; (B) midventricular short axis; (C) RV 2-chamber view; (D) Right ventricular outflow tract with circular pericardial effusion (white arrow) and epicardial fat (black arrow).
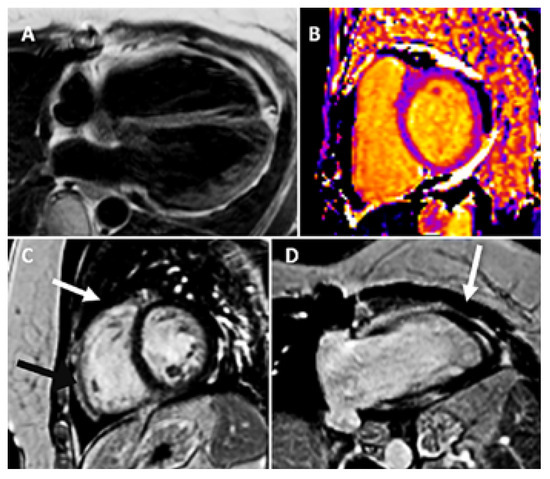
Figure 4.
CMR tissue characterization. (A) T1weighted turbo spin-echo (TSE); (B) native T1mapping epicardial fat (black) and pericardial effusion (white); (C) and (D) late gadolinium T1weighted imaging pictures showing pericardial effusion (white arrow), epicardial fat (black arrow) and only non-specific myocardial enhancement (late gadolinium enhancement) of the inferior insertion point.
Echocardiographic follow-up at one and four months showed no increase of the pericardial effusion and unchanged intrapericardial Doppler flows. To date, there is a complete remission of the lymphoma on oncological and radiological follow-up.
Discussion
Pericardial effusion is common in patients with neoplasia and particularly with mediastinal lymphoma [1] and can be the first manifestation of malignancy with important prognostic and therapeutic consequences [2,3]. While it may arise from direct tumour involvement, chemotherapy and radiation can also induce pericardial effusion. In our case, the patient presented with pericardial effusion at time of diagnosis of the lymphoma and the effusion was seen on positron emission tomographycomputed tomography (PET-CT).
Intrapericardial Doppler flow signal is rare and should raise the question of abnormal vascular communication with the cardiac cavities or the aorta [4,5]. To the best of our knowledge, this is the first case report describing intrapericardial Doppler flow signals in the absence of cardiac cavity communications in a patient without a recent cardiac procedure. Similar phenomena have been described in patients post coronary artery bypass grafting, aortic root replacement and radiofrequency ablation for atrial fibrillation [6,7,8]. In our case, the more than 20-year prior surgical ASD closure was certainly not related to the pericardial effusion. The presence of colour and pulsed wave Doppler signals inside the pericardial cavity implies the scattering of the ultrasound beam by small-sized particles, most commonly red blood cells and fibrin, moving towards and away from the ultrasound beam. Given the absence of haemodynamic compromise and reassuring radiological follow-up, diagnostic pericardiocentesis was not performed. We hypothesise that the movement of the right ventricle during systole, associated with a potentially rigid parietal pericardium due to the history of cardiac surgery and oncological treatments, could generate a suction effect with a localised shift of pericardial fluid, creating the observed Doppler signals.
Doppler examination of the intrapericardial space searching for colour or pulsed Doppler flow signals should be performed as it could be useful to detect abnormal communications with the pericardium and hint at the presence of haematic effusion.
Disclosure Statement
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Burazor, I.; Imazio, M.; Markel, G.; Adler, Y. Malignant Pericardial Effusion. Cardiology. 2013, 124, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Maisch, B.; Ristic, A.; Pankuweit, S. Evaluation and Management of Pericardial Effusion in Patients with Neoplastic Disease. Progress in Cardiovascular Diseases. 2010, 53, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Izutsu, K.; Suzuki, R.; et al. Prognostic significance of pleural or pericardial effusion and the implication of optimal treatment in primary mediastinal large B-cell lymphoma: A multicenter retrospective study in Japan. Haematologica. 2014, 99, 1817–1825. [Google Scholar] [CrossRef] [PubMed]
- Ozeki, S.; Utsunomiya, T.; Kishi, T.; et al. Coronary arteriovenous fistula presenting as chronic pericardial effusion. Circ J. 2002, 66, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, H.; Serdar Küçükoğlu, M.; Ozhan, H.; et al. A case of coronary artery fistula draining into the pericardium causing hematoma. Cardiovasc Surg. 2001, 9, 201203. [Google Scholar] [CrossRef]
- Gerber, T.C.; Safford, R.E. Intrapericardial Doppler-flow signals in cardiac tamponade. Clin Cardiol. 1999, 22, 231–232. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, L.; Camarda, P.; Mancuso, A.; Valerio, E.; Rebulla, E. Intrapericardial Doppler Flow Signals in a Patient with Postsurgical Pericardial Effusion. J Med Ultrasound. 2017, 25, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.P.; Lee, A.P.-W.; Yang, X.S.; Yu, C.M. Doppler flow signals in small amount pericardial effusion after radiofrequency ablation. Intern J Cardiol. 2014, 171, 447–448. [Google Scholar] [CrossRef] [PubMed]
© 2023 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.