Introduction
Hypertension accounts for about 20% of deaths in women worldwide and is a major modifiable risk factor for cardiovascular diseases. Cardiovascular diseases are the number one killer in Switzerland [
1], however, one o bserves a historical blindness concerning cardiovascular diseases and their complications in women, despite the fact that more hypertensive women than men develop target organ damage and complications. Women’s health in general has been reduced to their “bikini”, that is mammary glands and reproductive organs, for a long time. This results in only a few specific recommendations focusing on cardiovascular health in women.
Epidemiology
The prevalence of arterial hypertension increases steadily with age, reaching 70% in patients over 70 years old. With age and as women live longer, there is a more important proportion of hypertensive women than men in the elderly [
1].
A recent article published in the
Lancet tried to ascertain the prevalence, detection rate, treatment and control rates of arterial hypertension on a global scale [
2]. In high income countries (including Switzerland), the situation is better than the global average, but it is still suboptimal: 27% of hypertensive men and 31% of hypertensive women are still not diagnosed. Moreover, 10% of diagnosed men and 11% of diagnosed women are not treated and 21% of treated patients are not sufficiently controlled, with similar rates in both sexes. It is noteworthy, that the detection and treatment rates are slightly better in women, which holds true in lower income countries as well. We hypothesise that this is due to differences in health related behaviours, with women being generally more inclined to seek medical attention and to be more compliant with their medications [
3,
4]. However, if we specifically look at blood pressure (BP) control rates in patients over 65 years old, the trend reverses: the Framingham heart study showed that BP control rates were a lot worse in woman than in men over 60 years. Some studies also report more frequent resistant arterial hypertension in women after 49 years [
4,
5].
In Geneva, a study by the «Bus Santé» (Health Bus) published in 2012 reported that 62% of hypertensive women and 50% of hypertensive men had well controlled BP. Women were also more frequently aware of being hypertensive [
4,
6].
Moreover, the ischemic stroke risk increases at a lower BP level in women than in men, with a higher risk for women at every BP level [
7].
Sex bias in clinical research
Women have been largely excluded in clinical research for fear of damage to the unborn foetus. It is not uncommon in research protocols of trials with medications that a pregnancy test is mandatory to be included, even if it concerns post menopausal women.
Many scientific instances like the National Institutes of Health (NIH) at the end of the 1990’s, have risen against this, advocating parity of 50% for the inclusion of women in clinical studies. However it has been shown in 2009 that the proportion of women in large randomised cardiovascular clinical trials was only 38% and that only 68% of those trials included subgroup analyses based on sex [
8].
The SPRINT study was a large randomised trial, including more than 9000 nondiabetic patients with high cardiovascular risk [
9]. It compared systolic BP targets of <140 mm Hg (standard group) versus <120 mm Hg (intensive group). The intensive treatment group showed superior results regarding mortality and primary composite cardiovascular outcome reduction. The SPRINT study had a big echo in the United States and worldwide. Despite some criticism bearing on the unattended BP measurement used, it completely changed the target of systolic BP we aim to attain in all sub groups of patients, including patients with diabetes, renal failure and older patients. This study drastically impacted the American Heart Association 2017 guidelines, which recommend a target of less than 130 mm Hg of systolic BP for everyone. Yes, everyone, including women! However, in the trial, only 36% of included patients were women [
8]. The study was prematurely stopped because of a significant reduction of mortality, but this reduction was only statistically significant in men. The “women subgroup” did not show any significant difference between the two different blood pressure targets, due to a lack of statistical power. So there is a lack of evidence to apply this guideline to women.
Recently (2021), still only 25–30% of patients included in main clinical studies were women. For example, in another field, among 155 studies on Covid 19 treatment, 80% have excluded pregnant women [
10]. This exclusion is totally unjustified, for numerous medications that were evaluated have an established safety during pregnancies (e.g. ritonavir, lopinavir, interferon b, corticosteroids).
Pathophysiology across women’s life cycle
There is scarce high quality scientific data on the pathophysiological mechanisms of arterial hypertension, its management and its treatment in the female population. Indeed, epidemiology and response to drugs differ based on sex, but this is an understudied field.
During their reproductive life, women are relatively protected from essential arterial hypertension. Oestrogen and progesterone influence the activity of the renin angiotensinaldosterone system (RAAS), oxidative stress and endothelial function.
Pregnancy
Women are affected in this period of their lives by hypertensive disorders of pregnancy: preeclampsia (5–10% of pregnancies), gestational arterial hypertension and worsening of preexisting arterial hypertension during pregnancy. The frequency of these disorders increases related to later age of first gestation, “diabesity” and social factors. International guidelines on BP goals, antihypertensive medications and level of BP at which antihypertensive treatment has to be started during pregnancy differ widely or even contradict one another. There is a real deficit of clinical research in this field. Moreover, hypertensive disorders of pregnancy have been recently recognised as an ulterior cardiovascular and renal risk factor in their own right and the last guidelines of European societies of hypertension and cardiology recommend taking the obstetrical history in all hypertensive women.
Hypertensive troubles of pregnancy, including prematurity and intrauterine growth retardation, are associated with increased cardiovascular, renal and metabolic risks later in life and emerge as a marker of future risk that we have to consider and prevent.
Moreover, it has been shown that hypertensive disorders of pregnancy are associated with cognitive impairment in later life (poorer working memory and verbal learning 15 years after the pregnancy compared to women with normotensive pregnancies) [
11].
Menstrual cycle, oral contraceptives, menopause
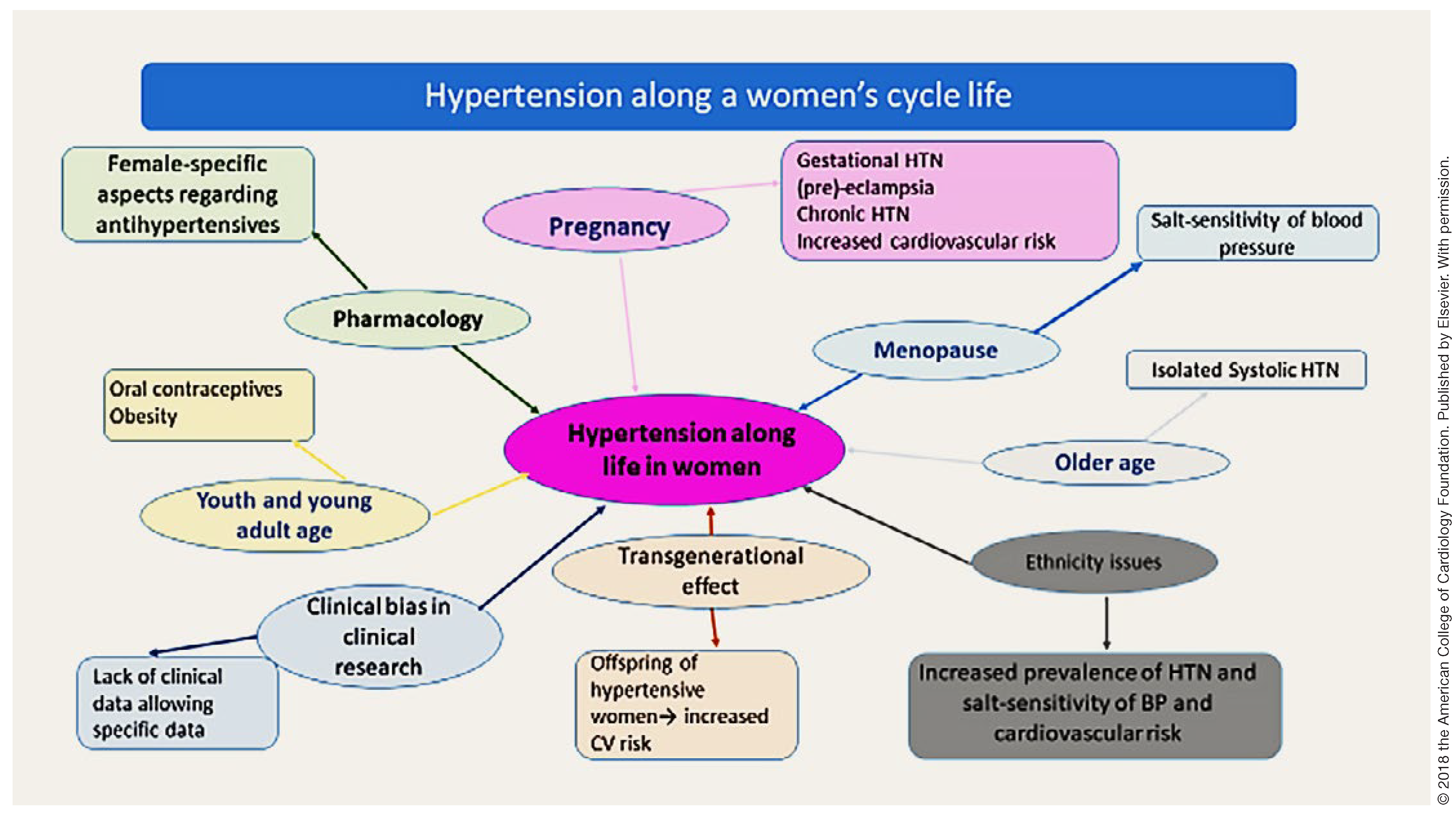
Women represent a heterogeneous group that is not easy to study, due to cyclic hormonal fluctuations (
Figure 1). Women have a lower blood pressure (BP) than men during their adolescence and reproductive life related to their female sex hormones. Endogenous female sex steroids influence the blood pressure, which drops slightly in the luteal phase of the menstrual cycle compared to the follicular phase. The increased progesterone level observed in the second phase of the menstrual cycle acts as an antagonist of the mineralocorticoid receptor [
4,
12]. The blood pressure rises slightly with oral contraceptives (even in normotensive women)[
12]. The episodes of malignant hypertension observed in the 60’s are actually rare, because doses of oestrogens have been greatly reduced in the preparations. Nevertheless, blood pressure has to be carefully controlled in hypertensive women taking oral contraceptives (OC) and the choice of the OC has to be discussed with the gynaecologist. Concomitant smoking must be stopped in hypertensive women taking OC because of the increased cardiovascular (CV) risk.
It is noteworthy that topical hormonal replacement therapy (with natural oestradiol and progesterone) does not result in an increase in BP [
4].
Approximately ten years after the menopause, the blood pressure starts to increase and prevalence of women’s systolic hypertension surpasses men’s [
13]. Complex pathophysiological mechanisms are set in motion, including an increase of the androgen/oestrogen ratio, activation of the sympathetic nervous system, activation of RAAS, decrease of NO mediated vasodilation and increase in endothelin 1 levels [
14]. The complete disappearance of the female sex hormones influence and interaction with testosterone and the sympathetic system at old age increase the arterial stiffness.
Moreover, post menopausal women present with a specific arterial hypertension phenotype. Their BP is more sensitive to salt intake [
12]. They are more prone to isolated systolic hypertension and increased pulse pressure due to arterial rigidity. In 24 hour ambulatory blood pressure monitoring, post menopausal women are more prone than men to have an abolished nocturnal dipping, which predisposes them to more frequent left ventricular hypertrophy [
14].
The variability of the BP is a newly recognised risk factor and is frequently observed in older women, whether it be visit to visit variability or stated in a 24h ambulatory blood pressure monitoring (ABPM) showing a high standard deviation. Anxiety and arterial stiffness may play a role in lability of the BP and would favour calcium channel blockers and stress management. White coat effect is more often observed in women and can also be considered as a form of variability.
Cardiovascular risk factors are different in women
In addition to hypertension as a classical cardiovascular risk factor, one has to consider other cardiovascular risk factors specific to women. Hypertensive women are more often affected by depression, stress at home plus stress at work (“double hat”), low social support, lower income, lower level of education and anxiety [
15]. They are more prone to an insufficient sleeping time, to the metabolic syndrome with an increase in waist circumference and android obesity. Other emerging non traditional cardiovascular risk factors are preterm delivery and hypertensive troubles during pregnancy.
Pharmacology of anti-hypertensive drugs in women
Numerous studies show that men and women respond differently to antihypertensive medications. In pharmacokinetics, drug absorption is generally lower in women due to a higher gastric pH, lower gastric emptying time and longer intestinal transit, resulting in higher bioavailability [
4,
16]. There also exist differences in cytochromes P450 activity, resulting for example in higher clearance of drugs metabolised by CYP3A4 (calcium channel blockers (CCBs), losartan) and CYP2D6 (labetalol, metoprolol) in young women. The clearance decreases with age, which explains why older women experience a higher blood pressure drop than younger women and men with CCBs [
16]. Moreover, women have lower activity of CYP1A2 and CYP2E1 than men [
1,
15]. In terms of bodily distribution, body weight is proportionally higher in women, which explains why lipophilic drugs (e.g. metoprolol) have a larger distribution volume, whereas hydrophilic drugs (e.g. angiotensin converting enzyme inhibitors [ACEI]) have a smaller distribution volume and therefore an increased effect [
15]. Furthermore, renal clearance is lower in women, due to the glomerular filtration rate being on average 10 15% lower than men’s for the same body surface area [
16]. This last point, as well as women being on average of lower weight, explains why drug exposure is higher in women and exposes them to more side effects [
4,
16].
Currently, guidelines on antihypertensive medications don’t take sex into account, because of the knowledge gap we already discussed.
Of note, even in animal research and despite well established sex differences in pharmacokinetics and pharmacodynamics and attempts to draw attention to sex dependent drug effects, the majority of rodent researchers continue to use males exclusively [
17]. As in human research, rules have been edited to systematically include more females in animal models.
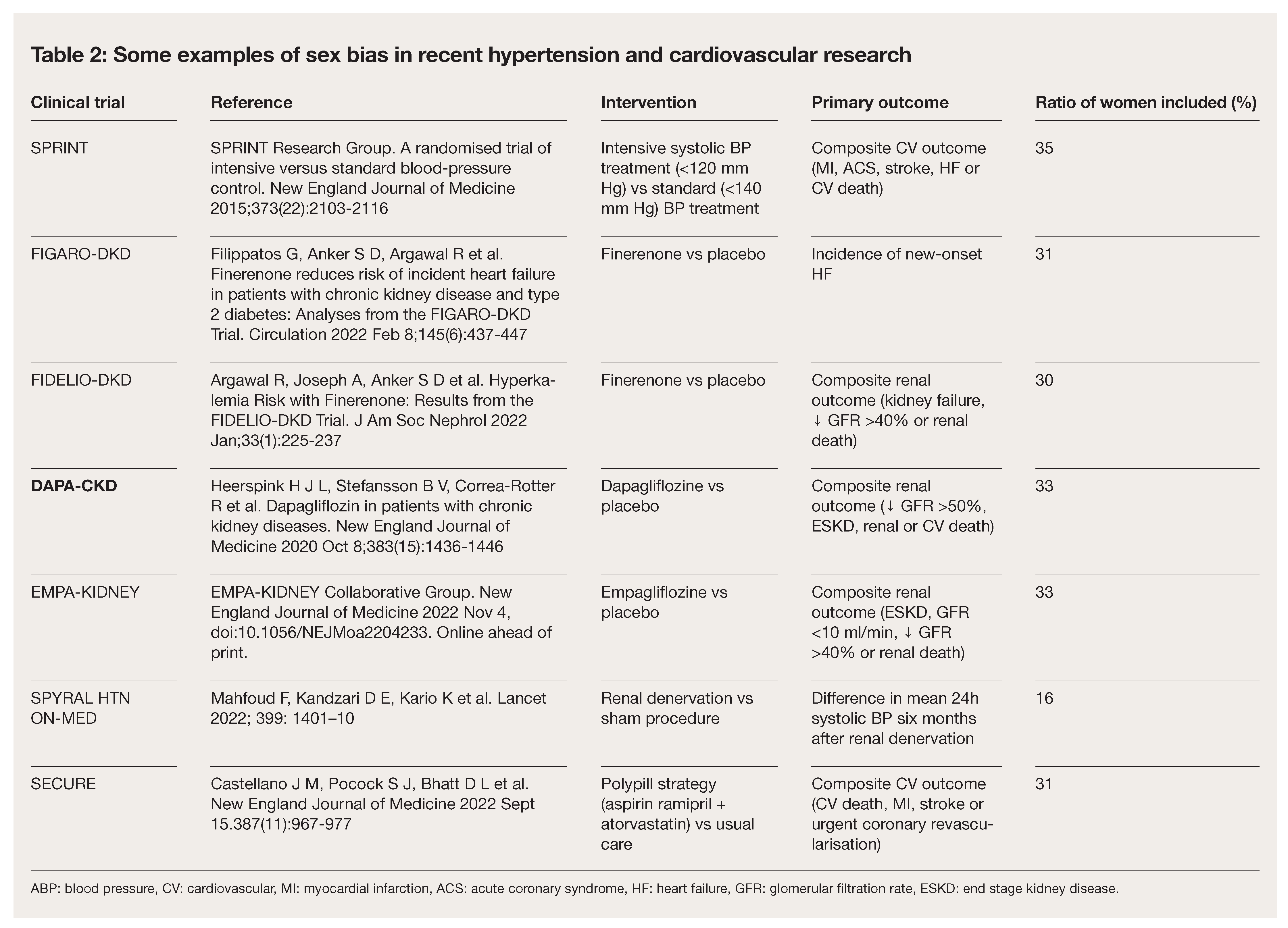
There is data suggesting sex specific diffe rences in response to antihypertensive medi cations, which we have summarised in
Table 1 [
4].
Empirically, we note that the most prescribed antihypertensive medications in men are ACEIs and angiotensin receptor blockers (ARB), whereas in women, they are diuretics and CCBs [
16]. This is probably linked to an avoidance of ACEIs and ARBs in women of childbearing age due to teratogenic risks. Salt sensitivity of the BP seems to be more frequent in women. Perimenopausal women are more prone to this phenotype [
12], which is associated with a lower plasma renin activity, therefore explaining a larger drop in blood pressure with diuretics and CCBs compared with beta blockers and blockers of the renin system. This encourages us to use a combination of diff erent antihypertensive classes at low dose, in order to benefit from the organ protection offered by the ACEIs and ARBs as is recommended by the 2018 ESC/ESH guidelines [
4]. An increased salt sensitivity of the BP is also observed 10 15 years after a preeclampsia [
18].
Available data show a similar efficiency of ACEIs and ARBs on blood pressure in men and women [
16]. Pharmacokinetic studies have revealed that the area under the curve (AUC) for ARBs is higher in women. This difference disappears after adjustment for body surface area [
4,
16].
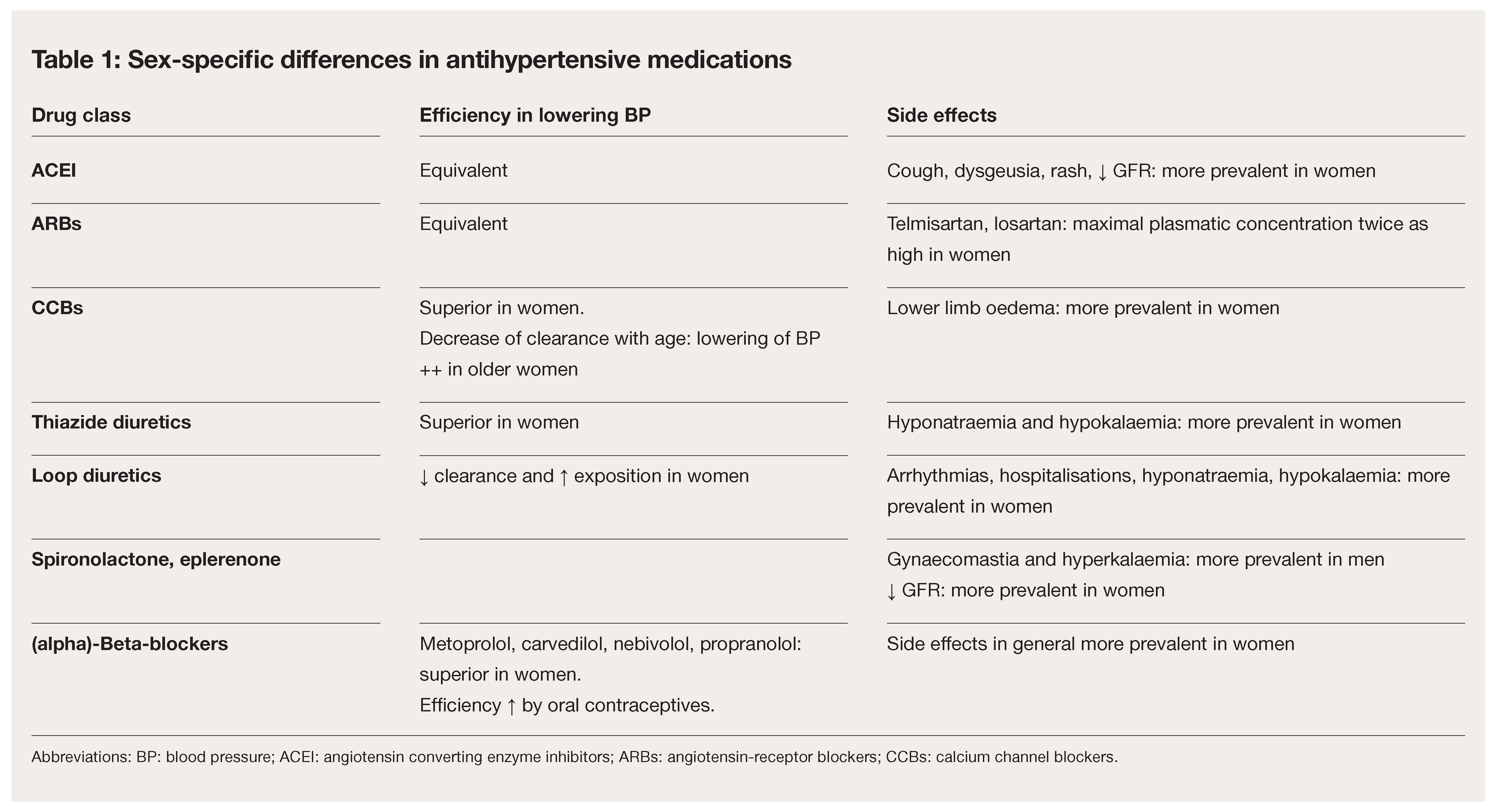
Table 2.
Some examples of sex bias in recent hypertension and cardiovascular research.
Table 2.
Some examples of sex bias in recent hypertension and cardiovascular research.
Similarly, the AUC for amlodipine is higher in women, but there is no difference in weight adjusted analyses. Furthermore, a 1996 study found that amlodipine in monotherapy led to a higher blood pressure reduction in women [
4,
19].
We can also cite the Accomplish study which showed the superiority of the ACEI/ CCB combination versus ACEI/thiazide diuretic to lower blood pressure [
20]. The results were however not significant in the women subgroup [
4].
Older women are often intolerant to all drugs with undefined malaises. If we turn to side effects, cough due to ACEI and hyponatraemia due to thiazide diuretics are both more frequent in women [
16]. Women are also more prone to lower limb oedema due to CCBs [
4,
16].
To summarize, for the treatment of hypertensive women we recommend to lower the doses of CCBs and thiazide diuretics. We also recommend an extra awareness to side effects (cough for ACEI, lower limb oedema for CCBs and hyponatraemia for thiazide diuretics).
Conclusion
Hypertension affects women in all phases of their life. It is now well known that there are differences between male and female arterial hypertension in terms of epidemiology, pathophysiology and response to antihypertensive medication. This field is understudied and the current knowledge gap leads to the absence of evidence based sex specific guidelines. Future cardiovascular clinical trials will need to enrol at least 50% women, with sex specific analyses on efficiency and safety of medications. It is necessary that more female researchers put in place “women oriented” projects, which implies having more women in academic positions.
As potential solution we propose a reflection on barriers limiting women participation in clinical trials and strategies to increase their enrolment, for example refusing to publish studies in which sex equality is not achieved.
The general practitioner should be aware of sex related differences in efficiency and safety of antihypertensive medications. We propose to prescribe lower doses of antihypertensive medications in women and that the doses be weight adjusted, knowing that side effects are more common in women [
4].