Abstract
Dual antiplatelet therapy (DAPT) is the evidence-based standard of care in patients with acute coronary syndrome (ACS) managed invasively or noninvasively, as well as for secondary prevention of coronary artery disease (CAD). The optimal treatment duration and composition of DAPT, however, remains a major challenge. Very low-dose (VLD) anticoagulation with rivaroxaban combined with antiplatelet therapy showed better outcomes in patients with ACS or stable CAD who were at high risk for ischaemic events and low bleeding risk. Current guidelines highlight patient risk stratification to individualise DAPT composition and duration. These personalised risk assessments, and implications for ischaemic events and bleeding complications are essential in decision making for adequate antithrombotic therapy and treatment decisions.
Introduction
Coronary artery disease (CAD) is characterised by the progressive development of coronary atherosclerotic plaques and their rupture. Myocardial perfusion is gradually impaired as a result of advancing stenosis of the blood vessel, and plaque rupture will result in complete vascular obliteration and myocardial ischaemia. The activation of platelets and the coagulation system are crucial in the pathophysiology.
Cardiovascular disease, particularly acute coronary syndrome (ACS), remains the major cause of mortality in the Western hemisphere, in spite of significant progress in treatment standards over the last decades [1]. Recent trials have shown that the implementation of new evidence-based treatments has resulted in significantly lower mortality rates [2].
Dual antiplatelet therapy (DAPT) is well established for secondary prevention in patients with coronary artery disease following percutaneous coronary intervention (PCI) [3,4]. Of note, DAPT is also indicated in patients with ACS without PCI if medical treatment only is pre-ferred. DAPT, consisting of aspirin and a P2Y12 inhibitor, is essential in preventing coronary and cerebrovascular thrombotic events. The optimal duration and combination of pharmaceuticals in DAPT aher PCI is still a controversial issue, weighing the prevention of ischaemic events against the risk of bleeding complications. Novel potent P2Y12 inhibitors are more effective in preventing ischaemic events, but do carry an increased risk of bleeding complications that are associated with substantial morbidity and mortality [5]. Newer generation stents are associated with fewer events and may need less intense therapies. Clinicians are challenged with balancing the bleeding and ischaemic risks on an individual basis when choosing the optimal duration and composition of the antithrombotic regimen.
Antiplatelet medication
DAPT, combining aspirin and a P2Y12 inhibitor such as clopidogrel, prasugrel or ticagrelor, is the current standard treatment aher a diagnosis of ACS. Multiple clinical trials demonstrated its effectiveness in prevention of thrombotic events, at the price of a higher bleeding risk. Current guidelines favour more potent P2Y12 inhibitors, such as prasugrel or ticagrelor, over clopidogrel because of an even greater reduction of ischaemic events (Figure 1) [5,6].

Figure 1.
Overview of platelet inhibition. Antithrombotic treatments and anticoagulants such as warfarin, rivaroxaban, apixaban, edoxaban and dabigatran further synergise with antiplatelet agents as shown in the Compass trial [6].Modified from Beer et al., artwork in collaboration with Dr. Nicole Bonetti is acknowledged [6]. 5-HT: 5-hydroxy tryptamine (serotonin); ADP: adenosine diphosphate; GP: glycoprotein; PAR: protease-activated receptor; TP: platelet thromboxane A2 receptor
Clopidogrel is a second generation P2Y12 inhibitor, a thienopyridine prodrug that requires hepatic metabolism to produce its active form [7]. Notably, cytochrome P450 2C19 (CYP2C19) is involved in this transformation. The function of this enzyme may be reduced in some individuals owing to a loss-of-function variant of the CYP2C19 or multiple other factors (e.g., drug interactions). This may decrease the effect on platelet inhibition and therefore result in a potentially higher risk for thrombotic events [8,9]. Routine genotype testing for P2Y12 inhibition is debated, but still lacks a pragmatic strategy for clinical practice and has not entered the guidelines [10,11,12].
Prasugrel is also a thienopyridine prodrug, but unlike clopidogrel, its conversion to an active metabolite only requires a one-step activation [13]. Compared with clopidogrel, prasugrel ensures more rapid and effective platelet inhibition.
Ticagrelor is one of a newer generation of P2Y12 inhibitors, which, like prasugrel, does not require special metabolism for drug activity. Furthermore, ticagrelor provides more reliable and rapid platelet inhibition than clopidogrel [14]. A common side-effect of ticagrelor is dyspnoea, which affects 10–20% of the patients. This side effect affects tolerability and may lead to a change in medication [15].
Prasugrel and ticagrelor have both been compared with clopidogrel in the following large, randomised trials. The TRITON-TIMI 38 trial (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) compared prasugrel with clopidogrel in patients with ACS undergoing PCI. Compared with clopidogrel, the group treated with prasugrel showed a significant reduction in the composite ischaemic endpoint of cardiovascular death, myocardial infarction or stroke [16]. The PLATO-trial (PLATelet inhibiton and patient Outcomes) showed a benefit of ticagrelor over clopidogrel with a significant reduction in the composite of vascular death, myocardial infarction or stroke with or without revascularisation [17]. The recent 2020 European Society of Cardiology (ESC) guidelines for treatment in patients with non ST-segment elevation ACS favour prasugrel or ticagrelor as a standard therapy (Figure 2andFigure 3) [4]. Direct comparison between prasugrel and ticagrelor was investigated in the randomised ISAR-REACT 5 trial (Intracoronary Stenting and Antithrombotic Regimen: Rapid Early Action for Coronary Treatment), which showed that prasugrel was associated with a lower rate of death, myocardial infarction or stroke at 1 year compared with ticagrelor. The mechanism behind these results is not yet fully elucidated, although partly compromised patient adherence in the ticagrelor group (due to side-effects) could be a possible reason [18]. The results of the ISAR-REACT study have several limitations, as one third of the patients were not treated with the assigned drug because of the open design of the study.
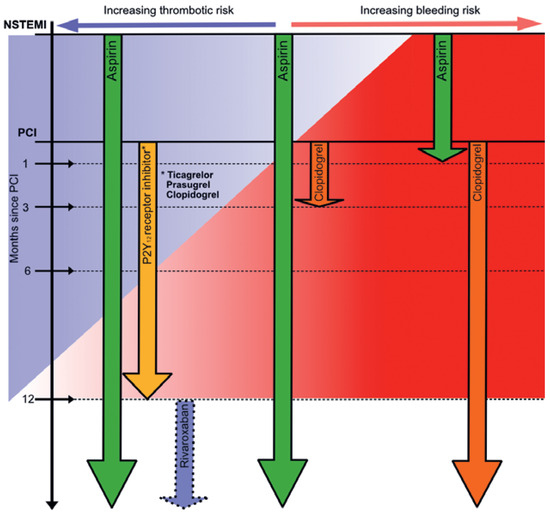
Figure 2.
Antithrombotic therapy for non-ST-segment elevation myocardial infarction. Colours represents the overlapping thrombotic risk (blue) and bleeding risk (red). Aspirin is usually given as a lifelong therapy with additional P2Y12 inhibitor for a period of 12 months after percutaneous coronary intervention. Additional therapy with low-dose rivaroxaban (2 × 2.5 mg) can be discussed 12 months after PCI in cases of low bleeding risk. In patients with increased bleeding risk duration of dual antithrombotic therapy might be shortened. In cases of very high bleeding risk dual antithrombotic therapy might be shortened to even 1 month with consecutive lifelong therapy of clopidogrel and discontinuation aspirin 1 month after PCI.ACS: acute coronary syndrome; PCI: percutaneous coronary intervention; NSTEMI: non-ST-segment elevation myocardial infarction
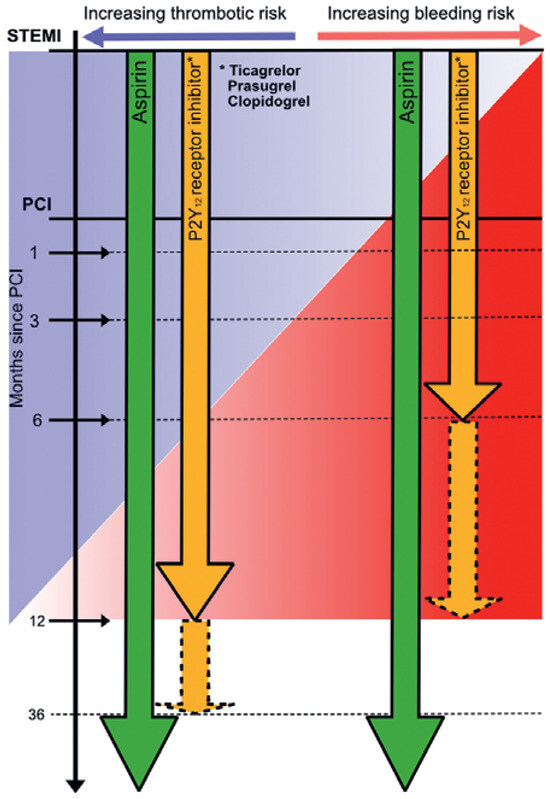
Figure 3.
Antithrombotic therapy for ST-segment elevation myocardial infarction. Colours represents the overlapping thrombotic risk (blue) and bleeding risk (red). Aspirin is usually given as lifelong therapy with additional P2Y12 inhibitor for a period of 12 months after percutaneous coronary intervention. In patients with high bleeding risk, duration of dual antithrombotic therapy might be shortened to 6 months with subsequent lifelong aspirin monotherapy.ACS: acute coronary syndrome; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction
Treatment duration
Despite various trials, the ideal duration of DAPT is still the subject of ongoing debate. The recommended standard duration of DAPT for most patients with ACS is 12 months in patients with low bleeding risk. Several trials evaluated a shorter DAPT regimen (3–6 months) [19,20,21,22]. The SMART-DATE trial compared 6-month and 12-month DAPT regimens, with clopidogrel used as the P2Y12 inhibitor in most cases [21]. Results showed an in-creased risk of myocardial infarction in the 6-month DAPT group [21]. Interestingly, some trials reported no significant difference in ischaemic events but a substantial decrease in bleeding complications with a shorter period of treatment. However, the majority of patients within the study population had a relatively low thrombotic risk [19,20,22]. These trials suggest that patients with a low risk for ischaemic events and a high risk for bleeding might benefit from a shorter DAPT regimen. Nonetheless, whether a shorter DAPT regimen is truly beneficial in patients at high thrombotic risk is yet to be further investigated. Bleeding risk is one of the key aspects for determining DAPT treatment duration, which is included in current guidelines [3,4].
The discontinuation of aspirin followed by P2Y12 inhibitor monotherapy was investigated in recent studies [23,24,25,26]. The background for challenging aspirin is that, despite all its benefits, it is associated with a higher bleeding risk and the fact that new potent antithrombotic agents with more consistent characteristics are available [27,28,29]. In the TWILIGHT trial, DAPT with aspirin and ticagrelor was compared with ticagrelor monotherapy aher 3 months DAPT. The results showed lower rates of clinically relevant bleeding and no increase of ischaemic events in the group with ticagrelor monotherapy [23]. Several TWILIGHT sub-studies confirmed these results in an experimental design [30,31]. However, the ischaemic event rate in TWILIGHT was lower than in other trials for high-risk PCI patients, as patients with ST-segment elevation myocardial infarction were excluded [4]. Since there are currently no randomised trials comparing aspirin monotherapy with P2Y12 inhibitor monotherapy aher DAPT, aspirin remains an important integral component of antithrombotic therapy. The PEGASUS-TIMI 54 trial showed that, among patients with prior myocardial infarction on aspirin therapy, the addition of ticagrelor was beneficial. Ticagrelor compared with placebo reduced the risk of cardiovascular death, myocardial infarction or stroke with higher rates of major bleeding [48].
Extended DAPT duration beyond 12 months showed a lower risk of ischaemic events at the cost of an increased bleeding risk. The pivotal DAPT trial, which compared long DAPT (30 months) with standard DAPT (12 months) aher coronary stenting, demonstrated a significant risk reduction for stent thrombosis and major adverse cardiovascular and cerebrovascular events, but was also associated with an increased risk of bleeding [32]. Thus, patients with an elevated thrombotic risk who are not at high risk for bleeding may be considered for a longer duration of DAPT [3,4]. Furthermore, PCI complexity is an important determinant for extended DAPT [4]. Technical aspects of PCI complexity are implantation of three or more stents, three or more lesions treated, total stent length >60 mm, complex PCI (leh main, bifurcation stenting with ≥2 stents implanted, chronic total occlusion, stenting of last patent vessel) and history of stent thrombosis on antiplatelet treatment [4].
Concomitant anticoagulant therapy
Due to the not negligible recurrence rate of major adverse cardiovascular events in ACS patients despite DAPT treatment, combination of DAPT and low-dose anticoagulant therapy for long-term management after hospital discharge has been the subject of renewed research interest. Oral inhibitors of factor Xa (rivaroxaban, apixaban and edoxaban) are competitive inhibitors of factor Xa and thus inhibit the formation of thrombin, which plays an essential role in platelet and coagulation activation [33]. Dabigatran is a direct oral thrombin inhibitor, stopping thrombin from converting fibrin to fibrinogen [34].
The ATLAS ACS 2-TIMI 51 trial investigated VLD rivaroxaban (2.5 mg or 5 mg twice daily) versus placebo in patients with ACS, mostly with concomitant DAPT therapy. The results showed that treatment with rivaroxaban was associated with a reduced risk of death, myocardial infarction and stroke, at the expense of an increased risk for bleeding complications [35]. Of note, a very low rivaroxaban dosage of 2.5 mg twice daily significantly reduced the risk of cardiovascular and allcause mortality compared with the 5 mg dose (twice daily). Hence, a ceiling effect of antithrombotic impact with this indication might be suggestive. In the subsequent COMPASS trial, low-dose anticoagulation (rivaroxaban 2.5 mg twice daily) in addition to aspirin compared with aspirin monotherapy was associated with a significant reduction in the primary composite outcome of cardiovascular death, myocardial infarction or stroke in patients with stable CAD or peripheral artery disease at higher ischaemic risk [36]. Importantly, these were stable patients (not ACS patients) with atherosclerosis in two vascular beds. Consistent with previous results, patients on low-dose rivaroxaban and aspirin had more bleeding complications [36]. Interestingly, VLD rivaroxaban had an important impact in reducing the incidence of stroke. Based on the available evidence, trials show a possible benefit of adding low-dose rivaroxaban in patients with ACS. However, current guidelines underline the importance of careful patient selection (high ischaemic risk and low bleeding risk) for treatment with low-dose rivaroxaban on top of aspirin for long-term secondary prevention [4].
The number of patients with atrial fibrillation (AF) referred for coronary angiography (with or without PCI) has increased over past decades (5% to 10%) [37,38]. AF patients who are treated with a triple therapy (aspirin, a P2Y12 inhibitor and an oral anticoagulant) aher ACS are at high risk for bleeding and therefore higher mortality [39,40]. The initiator for a subsequent series of important trials was the ground-breaking WOEST trial (What Is the Optimal Antiplatelet and Anticoagulant Therapy in Patients with Oral Anticoagulation and Coronary Stenting), which compared warfarin combined with clopidogrel against triple therapy (DAPT and warfarin) [41]. This trial showed decreased bleeding complications by foregoing aspirin, but was not sufficiently powered to detect differences in the secondary outcome of stent thrombosis. Nevertheless, the trial implied that dual therapy (warfarin and clopidogrel) without aspirin could be more favourable in balancing ischaemic versus bleeding risks in patients with AF and a recent ACS. In the PIONEER AF-PCI (Multicenter Study Exploring Two Treatment Strategies of Rivaroxaban and One of Oral Vitamin K Antagonist in Patients With Atrial Fibrillation Who Underwent Percutaneous Coronary Intervention) patients were randomly divided into three groups: one group treated with low-dose rivaroxaban (15 mg once daily) plus a P2Y12 inhibitor, the second group with VLD (2.5 mg twice daily) rivaroxaban plus a P2Y12 inhibitor and aspirin, and the third group with DAPT with warfarin [42]. Aher completion of DAPT therapy of 1 or 6 months, patients in groups 2 or 3 received only oral anticoagulants with aspirin. The results showed a lower rate of bleeding in each rivaroxaban treatment arm compared with triple therapy. Subsequently, the RE-DUAL PCI (Evaluation of Dual Therapy With Dabigatran vs Triple Therapy With Warfarin in Patients With AF That Undergo a PCI With Stenting) trial randomised patients to either dabigatran plus a P2Y12 inhibitor or triple therapy with warfarin [43]. The primary endpoint of major bleeding was significantly reduced in both trials in the direct oral anticoagulant (DOAC) group (oral anticoagulant plus P2Y12 inhibitor alone) compared with triple therapy.
The recent and important AUGUSTUS (Antithrombotic Therapy aher ACS or PCI in Atrial Fibrillation) trial investigated in a 2 × 2 factorial design the effect of apixaban and aspirin in patients with AF and recent ACS or PCI [44]. The key finding was that combined treatment with apixaban and a P2Y12-inhibitor resulted in lower rates of bleeding, death and rehospitalisation compared with the warfarin regimen. The addition of aspirin led to a higher bleeding rate without any difference in ischaemic events [44].
The ENTRUST-AF PCI (Edoxaban Treatment Versus Vitamin K Antagonist in Patients with Atrial Fibrillation Undergoing Percutaneous Coronary Intervention) trial showed once again the superiority of DOACs by comparing edoxaban and clopidogrel with vitamin K antagonist-based triple therapy [45].
In summary, the use of DOACs showed reduced rates of bleeding when compared with vitamin K antagonists. The current ESC Guidelines for patients with ACS and AF undergoing an uncomplicated PCI recommend triple therapy with aspirin, clopidogrel and a DOAC in reduced dose for a duration of 1 week up to 1 month (depending on the risk of stent thrombosis and bleeding risk), and a continuation of dual therapy with a DOAC and a P2Y12 inhibitor (preferably clopidogrel) for up to 12 months (or 6 months in chronic coronary syndrome) [12]. Thereaher, DOAC monotherapy is to be continued.
Risk scores and individualised antiplatelet therapy
Risk stratification based on clinical judgement and risk scores are essential for determining the optimal DAPT duration. Risk scores are important tools, which can guide the clinician by estimating the ischaemic and bleeding risks in a patient. Over the past few years several risk scores have been derived from randomised DAPT trials. The DAPT score, for example, was developed from the DAPT trial, where the trial cohort tolerated DAPT over a year [46]. It consists of nine clinical and procedural variables and is designed to predict which patients might benefit from an extended DAPT duration (as far as 30 months). Patients with a high score (2 points or more) benefitted from extended DAPT treatment (12–30 months) resulting in a reduction in ischaemic events. On the other hand, patients with a score lower than 2 did not have a net clinical benefit from an extension of DAPT treatment [46].
The PRECISE-DAPT score has been developed from a collaborative dataset comprised of eight randomised trials with 14,963 patients undergoing PCI and subsequent DAPT therapy (Table 1) [47]. Used at the time of PCI, the score is defined by five variables (age, kidney function, haemoglobin, white blood cell count, prior bleeding) and evaluates the risk and benefit of short (3–6 months) vs prolonged (12–24 months) DAPT. The score ranges from 0–100 points. In patients with a score of ≥25 points, longer DAPT was associated with no reduction in ischaemic events, but an increase in bleeding complications. On the other hand, patients with a score of less than 25 points had no increase in bleeding but had a significant reduction in ischaemic events, thus supporting longer use of DAPT in this population [47].

Table 1.
Risk score for clinical guidance of optimal dual antiplatelet therapy duration.
It is important to keep in mind that these scores are derived from randomised study cohorts and many “real world” patients do not fully meet trial inclusion criteria and may have other special characteristics. Therefore, further cohort studies and individualised clinical judgment are essential in assessing individual ischaemic versus bleeding risk with these scores.
Conclusions and future directions
Careful assessment of ischaemic versus bleeding risks is the key factor in tailoring the optimal DAPT treatment for a patient with ACS. Risk scores are useful in deciding who benefits most from treatment. With improvements in stent technology and potent P2Y12 inhibitors, the optimal DAPT duration will continue to be refined over time.
Disclosure statement
No financial support and no other potential conflict of interest relevant to this article was reported. JHB has received grant support from the Swiss National Foundation of Science (grant no. 310030_144152), the Swiss Heart Foundation, the Kardio Foundation and he has received grant support and consultancy fees to the institution from Bayer, Daitchii and Sanofi.
References
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J. 2016, 37, 3232–45. [Google Scholar] [CrossRef] [PubMed]
- Szummer, K.; Wallentin, L.; Lindhagen, L.; Alfredsson, J.; Erlinge, D.; Held, C.; et al. Improved outcomes in patients with ST-elevation myocardial infarction during the last 20 years are related to implementation of evidence-based treatments: experiences from the SWEDEHEART registry 1995-2014. Eur Heart J. 2017, 38, 3056–65. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Bueno, H.; Byrne, R.A.; Collet, J.P.; Costa, F.; Jeppsson, A.; et al. ESC Scientific Document Group. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2018, 53, 34–78. [Google Scholar] [CrossRef]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; et al. ESC Scientific Document Group. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021, 42, 1289–367. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; et al. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018, 39, 119–77. [Google Scholar] [CrossRef]
- Beer, J.H.; Bonetti, N. A COMPASS to REACH the right patients with thrombocardiology: benefits, risks, and future of the new concept. Eur Heart J. 2018, 39, 758–61. [Google Scholar] [CrossRef]
- Yang, Y.; Lewis, J.P.; Hulot, J.S.; Scott, S.A. The pharmacogenetic control of antiplatelet response: candidate genes and CYP2C19. Expert Opin Drug Metab Toxicol. 2015, 11, 1599–617. [Google Scholar] [CrossRef]
- Mega, J.L.; Close, S.L.; Wiviott, S.D.; Shen, L.; Hockett, R.D.; Brandt, J.T.; et al. Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med. 2009, 360, 354–62. [Google Scholar] [CrossRef]
- Simon, T.; Verstuyh, C.; Mary-Krause, M.; Quteineh, L.; Drouet, E.; Méneveau, N.; et al. French Registry of Acute ST-Elevation and Non-ST-Elevation Myocardial Infarction (FAST-MI) Investigators. Genetic determinants of response to clopidogrel and cardiovascular events. N Engl J Med. 2009, 360, 363–75. [Google Scholar] [CrossRef]
- Paré, G.; Mehta, S.R.; Yusuf, S.; Anand, S.S.; Connolly, S.J.; Hirsh, J.; et al. Effects of CYP2C19 genotype on outcomes of clopidogrel treatment. N Engl J Med. 2010, 363, 1704–14. [Google Scholar] [CrossRef]
- Hulot, J.S.; Chevalier, B.; Belle, L.; Cayla, G.; Khalife, K.; Funck, F.; et al. GIANT Investigators. Routine CYP2C19 Genotyping to Adjust Thienopyridine Treatment Aher Primary PCI for STEMI: results of the GIANT Study. JACC Cardiovasc Interv. 2020, 13, 621–30. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; et al. ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Storey, R.F. Development and clinical use of prasugrel and ticagrelor. Curr Pharm Des. 2012, 18, 5240–60. [Google Scholar] [CrossRef] [PubMed]
- Storey, R.F.; Bliden, K.P.; Ecob, R.; Karunakaran, A.; Butler, K.; Wei, C.; et al. Earlier recovery of platelet function aher discontinuation of treatment with ticagrelor compared with clopidogrel in patients with high antiplatelet responses. J Thromb Haemost. 2011, 9, 1730–7. [Google Scholar] [CrossRef]
- Parodi, G.; Storey, R.F. Dyspnoea management in acute coronary syndrome patients treated with ticagrelor. Eur Heart J Acute Cardiovasc Care. 2015, 4, 555–60. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Braunwald, E.; McCabe, C.H.; Montalescot, G.; Ruzyllo, W.; Gottlieb, S.; et al. TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007, 357, 2001–15. [Google Scholar] [CrossRef]
- Wallentin, L.; Becker, R.C.; Budaj, A.; Cannon, C.P.; Emanuelsson, H.; Held, C.; et al. PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009, 361, 1045–57. [Google Scholar] [CrossRef]
- Schüpke, S.; Neumann, F.J.; Menichelli, M.; Mayer, K.; Bernlochner, I.; Wöhrle, J.; et al. ISAR-REACT 5 Trial Investigators. Ticagrelor or Prasugrel in Patients with Acute Coronary Syndromes. N Engl J Med. 2019, 381, 1524–34. [Google Scholar] [CrossRef]
- Schulz-Schüpke, S.; Byrne, R.A.; Ten Berg, J.M.; Neumann, F.J.; Han, Y.; Adriaenssens, T.; et al. Intracoronary Stenting and Antithrombotic Regimen: Safety And EFficacy of 6 Months Dual Antiplatelet Therapy Aher Drug-Eluting Stenting (ISAR-SAFE) Trial Investigators. ISAR-SAFE: a randomized, double-blind, placebo-controlled trial of 6 vs. 12 months of clopidogrel therapy aher drug-eluting stenting. Eur Heart J. 2015, 36, 1252–63. [Google Scholar] [CrossRef]
- Colombo, A.; Chieffo, A.; Frasheri, A.; Garbo, R.; Masotti-Centol, M.; Salvatella, N.; et al. Second-generation drug-eluting stent implantation followed by 6versus 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol. 2014, 64, 2086–97. [Google Scholar] [CrossRef]
- Hahn, J.Y.; Song, Y.B.; Oh, J.H.; Cho, D.K.; Lee, J.B.; Doh, J.H.; et al. SMARTDATE investigators. 6-month versus 12-month or longer dual antiplatelet therapy aher percutaneous coronary intervention in patients with acute coronary syndrome (SMARTDATE): a randomised, open-label, non-inferiority trial. Lancet 2018, 391, 1274–84. [Google Scholar] [CrossRef]
- Feres, F.; Costa, R.A.; Abizaid, A.; Leon, M.B.; Marin-Neto, J.A.; Botelho, R.V.; et al. OPTIMIZE Trial Investigators. Three vs twelve months of dual antiplatelet therapy aher zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013, 310, 2510–22. [Google Scholar] [CrossRef] [PubMed]
- Mehran, R.; Baber, U.; Sharma, S.K.; Cohen, D.J.; Angiolillo, D.J.; Briguori, C.; et al. Ticagrelor with or without Aspirin in High-Risk Patients aher PCI. N Engl J Med. 2019, 381, 2032–42. [Google Scholar] [CrossRef] [PubMed]
- O’Donoghue, M.L.; Murphy, S.A.; Sabatine, M.S. The Safety and Efficacy of Aspirin Discontinuation on a Background of a P2Y12 Inhibitor in Patients Aher Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. Circulation. 2020, 142, 538–45. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, H.; Domei, T.; Morimoto, T.; Natsuaki, M.; Shiomi, H.; Toyota, T.; et al. STOPDAPT-2 Investigators. Effect of 1-Month Dual Antiplatelet Therapy Followed by Clopidogrel vs 12-Month Dual Antiplatelet Therapy on Cardiovascular and Bleeding Events in Patients Receiving PCI: The STOPDAPT-2 Randomized Clinical Trial. JAMA 2019, 321, 2414–27. [Google Scholar] [CrossRef]
- Vranckx, P.; Valgimigli, M.; Jüni, P.; Hamm, C.; Steg, P.G.; Heg, D.; et al. GLOBAL LEADERS Investigators. Ticagrelor plus aspirin for 1 month, followed by ticagrelor monotherapy for 23 months vs aspirin plus clopidogrel or ticagrelor for 12 months, followed by aspirin monotherapy for 12 months aher implantation of a drug-eluting stent: a multicentre, open-label, randomised superiority trial. Lancet 2018, 392, 940–9. [Google Scholar] [CrossRef]
- Gargiulo, G.; Windecker, S.; Vranckx, P.; Gibson, C.M.; Mehran, R.; Valgimigli, M. A Critical Appraisal of Aspirin in Secondary Prevention: Is Less More? Circulation. 2016, 134, 1881–906. [Google Scholar] [CrossRef]
- Moon, J.Y.; Franchi, F.; Rollini, F.; Angiolillo, D.J. The quest for safer antithrombotic treatment regimens in patients with coronary artery disease: new strategies and paradigm shihs. Expert Rev Hematol. 2018, 11, 5–12. [Google Scholar] [CrossRef]
- Capodanno, D.; Mehran, R.; Valgimigli, M.; Baber, U.; Windecker, S.; Vranckx, P.; et al. Aspirin-free strategies in cardiovascular disease and cardioembolic stroke prevention. Nat Rev Cardiol. 2018, 15, 480–96. [Google Scholar] [CrossRef]
- Dangas, G.; Baber, U.; Sharma, S.; Giustino, G.; Mehta, S.; Cohen, D.J.; et al. Ticagrelor With or Without Aspirin Aher Complex PCI. J Am Coll Cardiol. 2020, 75, 2414–24. [Google Scholar] [CrossRef]
- Baber, U.; Zafar, M.U.; Dangas, G.; Escolar, G.; Angiolillo, D.J.; Sharma, S.K.; et al. Ticagrelor With or Without Aspirin Aher PCI: The TWILIGHT Platelet Substudy. J Am Coll Cardiol. 2020, 75, 578–86. [Google Scholar] [CrossRef]
- Mauri, L.; Kereiakes, D.J.; Yeh, R.W.; Driscoll-Shempp, P.; Cutlip, D.E.; Steg, P.G.; et al. DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy aher drug-eluting stents. N Engl J Med. 2014, 371, 2155–66. [Google Scholar] [CrossRef] [PubMed]
- Weitz, J.I.; Bates, S.M. New anticoagulants. J Thromb Haemost. 2005, 3, 1843–53. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, R.J.; Flaker, G.C.; Saxonhouse, S.J.; Doherty, J.U.; Birtcher, K.K.; Cuker, A.; et al. Practical management of anticoagulation in patients with atrial fibrillation. J Am Coll Cardiol. 2015, 65, 1340–60. [Google Scholar] [CrossRef] [PubMed]
- Mega, J.L.; Braunwald, E.; Wiviott, S.D.; Bassand, J.P.; Bhatt, D.L.; Bode, C.; et al. ATLAS ACS 2–TIMI 51 Investigators. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med. 2012, 366, 9–19. [Google Scholar] [CrossRef]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; et al. COMPASS Investigators. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N Engl J Med. 2017, 377, 1319–30. [Google Scholar] [CrossRef]
- Ruiz-Nodar, J.M.; Marín, F.; Hurtado, J.A.; Valencia, J.; Pinar, E.; Pineda, J.; et al. Anticoagulant and antiplatelet therapy use in 426 patients with atrial fibrillation undergoing percutaneous coronary intervention and stent implantation implications for bleeding risk and prognosis. J Am Coll Cardiol. 2008, 51, 818–25. [Google Scholar] [CrossRef]
- Michniewicz, E.; Mlodawska, E.; Lopatowska, P.; Tomaszuk-Kazberuk, A.; Malyszko, J. Patients with atrial fibrillation and coronary artery disease Double trouble. Adv Med Sci. 2018, 63, 30–5. [Google Scholar] [CrossRef]
- Lamberts, M.; Olesen, J.B.; Ruwald, M.H.; Hansen, C.M.; Karasoy, D.; Kristensen, S.L.; et al. Bleeding aher initiation of multiple antithrombotic drugs, including triple therapy, in atrial fibrillation patients following myocardial infarction and coronary intervention: a nationwide cohort study. Circulation. 2012, 126, 1185–93. [Google Scholar] [CrossRef]
- Hess, C.N.; Peterson, E.D.; Peng, S.A.; de Lemos, J.A.; Fosbol, E.L.; Thomas, L.; et al. Use and Outcomes of Triple Therapy Among Older Patients With Acute Myocardial Infarction and Atrial Fibrillation. J Am Coll Cardiol. 2015, 66, 616–27. [Google Scholar] [CrossRef]
- Dewilde, W.J.; Oirbans, T.; Verheugt, F.W.; Kelder, J.C.; De Smet, B.J.; Herrman, J.P.; et al. WOEST study investigators. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013, 381, 1107–15. [Google Scholar] [CrossRef]
- Gibson, C.M.; Mehran, R.; Bode, C.; Halperin, J.; Verheugt, F.W.; Wildgoose, P.; et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N Engl J Med. 2016, 375, 2423–34. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Bhatt, D.L.; Oldgren, J.; Lip, G.Y.; Ellis, S.G.; Kimura, T.; et al. RE-DUAL PCI Steering Committee and Investigators. Dual Antithrombotic Therapy with Dabigatran aher PCI in Atrial Fibrillation. N Engl J Med. 2017, 377, 1513–24. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; et al. AUGUSTUS Investigators. Antithrombotic Therapy aher Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med. 2019, 380, 1509–24. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, P.; Valgimigli, M.; Eckardt, L.; Tijssen, J.; Lewalter, T.; Gargiulo, G.; et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen aher successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet 2019, 394, 1335–43. [Google Scholar] [CrossRef]
- Yeh, R.W.; Secemsky, E.A.; Kereiakes, D.J.; Normand, S.L.; Gershlick, A.H.; Cohen, D.J.; et al. DAPT Study Investigators. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year Aher Percutaneous Coronary Intervention. JAMA 2016, 315, 1735–49. [Google Scholar] [CrossRef]
- Costa, F.; van Klaveren, D.; James, S.; Heg, D.; Räber, L.; Feres, F.; et al. PRECISE-DAPT Study Investigators. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 2017, 389, 1025–34. [Google Scholar] [CrossRef]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; et al. PEGASUS-TIMI 54 Steering Committee and Investigators. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med. 2015, 372, 1791–800. [Google Scholar] [CrossRef]
© 2021 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.