Infective Endocarditis: Prevention and Antibiotic Prophylaxis
What is new compared to the 2008 recommendations?
Population at high risk for infective endocarditis
- 1.
- Patients with a previous episode of infective endocarditis.
- 2.
- Patients with any prosthetic valve (biological or mechanical), including a transcatheter valve (transcatheter valve implantation), or those in whom any prosthetic material was used for cardiac valve repair.
- 3.
- Patients with congenital heart disease (CHD).
- (a)
- Any type of cyanotic CHD (i.e., unrepaired CHD).
- (b)
- Any type of CHD repaired with prosthetic material, whether placed surgically or by percutaneous techniques. ⇒ At risk up to 6 months after the procedure.
- (c)
- Any type of CHD repaired with prosthetic material, whether placed surgically or by percutaneous techniques. ⇒ At risk for life if residual shunt persists or if residual finding persists after the procedure (for example incomplete tissue ingrowth of prosthetic material).
- 4.
- There is no evidence to recommend antimicrobial prophylaxis for cardiac transplant recipients who develop cardiac valvulopathy. The indication should be discussed on a case-by-case basis. The patient should contact their transplant specialist to evaluate the indication prior to an elective intervention.
Dental and non-dental interventions
Dental procedures
- –
- manipulation of the gingival or periapical region of the teeth.
- –
- perforation of the oral mucosa.
Antibiotic prophylaxis prior to dental intervention and dental hygiene*
- –
- Adults: 2 g orally (p.o.)
- –
- Children: 50 mg/kg (maximum dose 2 g) p.o.
- –
- Adults: cefuroxime axetil 1 g p.o. in patients with delayed hypersensitivity reaction
- –
- Children: cefuroxime axetil 50 mg/kg p.o. (maximum dose 1 g) in patients with delayed hypersensitivity reaction
- –
- Adults: clindamycin 600 mg p.o. in patients with immediate hypersensitivity reaction
- –
- Children: clindamycin 20 mg/kg p.o. (maximum dose 600 mg) in patients with immediate hypersensitivity reaction
- –
- Adults: amoxicillin 2 g intravenously (i.v.)
- –
- Children: amoxicillin 50 mg/kg i.v. (maximum dose 2 g)
- –
- Adults: cefazolin 1 g i.v. or ceftriaxone 2 g i.v. in patients with delayed hypersensitivity reaction
- –
- Children: cefazolin 25 mg/kg i.v. (maximum dose 1 g) or ceftriaxone 50 mg/kg i.v. (maximum dose 2 g) in patients with delayed hypersensitivity reaction
- –
- Adults: clindamycin 600 mg i.v. or vancomycin 1 g i.v. in patients with immediate hypersensitivity reaction
- –
- Children: clindamycin 20 mg/kg i.v. (maximum dose 600 mg) or vancomycin 20 mg/kg i.v. (maximum dose 1 g) in patients with immediate hypersensitivity reaction
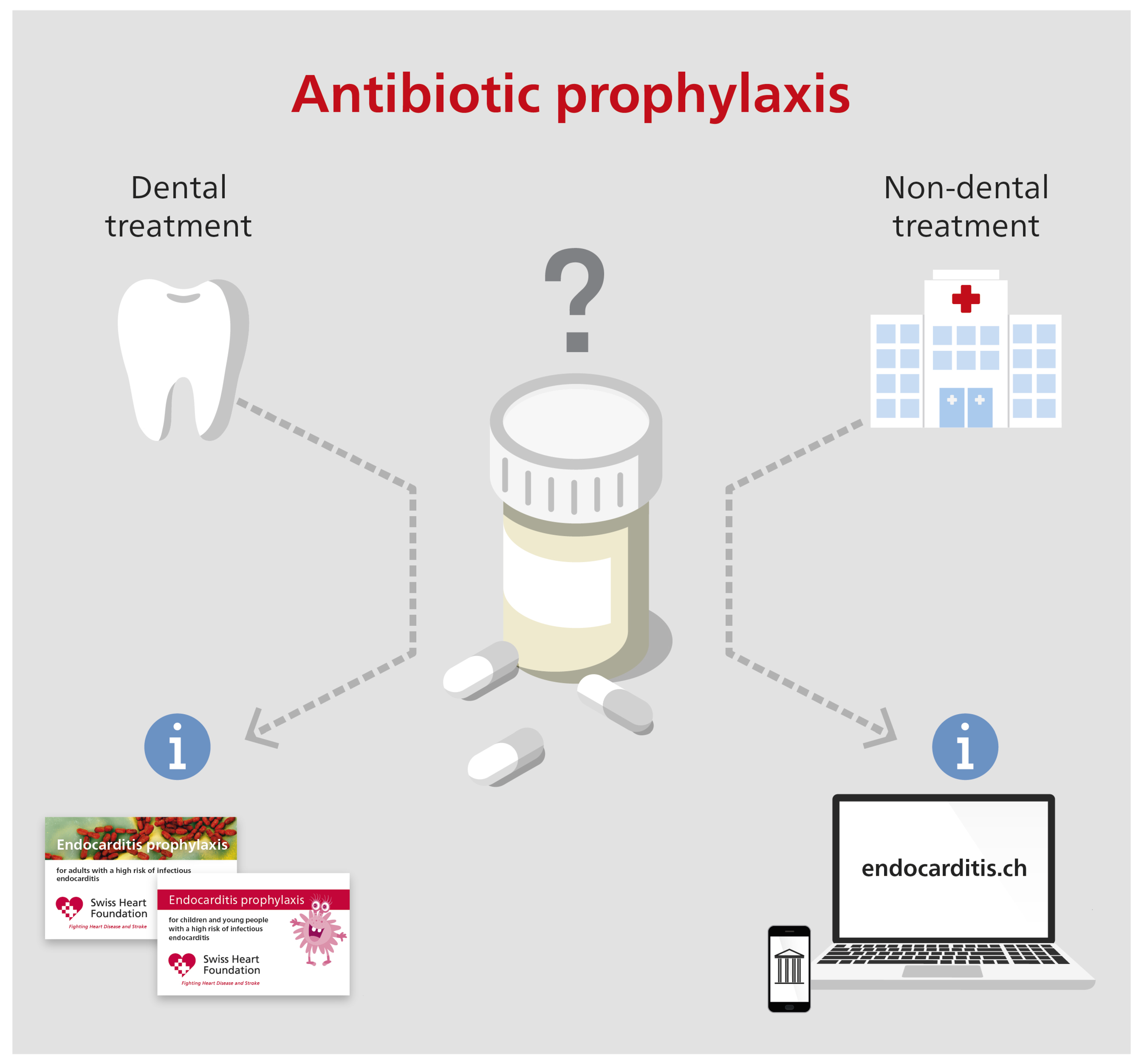
Non-dental interventions
- –
- Perioperative antimicrobial prophylaxis is not recommended for tonsillectomy in patients not at risk for infective endocarditis. There is no evidence-based recommendation for perioperative antimicrobial prophylaxis in patients with risk for infective endocarditis.
- –
- Tonsillectomy is associated with bacteremia in a considerable proportion of patients undergoing this procedure. There is no evidence that perioperative antimicrobial prophylaxis prevents infective endocarditis in patients at risk. The majority of the expert group favor perioperative antimicrobial prophylaxis for tonsillectomy in patients at risk for infective endocarditis. The agent should contain activity against microorganisms belonging to the oral microbiom.
- –
- The expert group clearly categorizes this statement as an expression of opinion and not as a guideline recommendation. The expert group states also that the number of opinions does not correlate with the level of evidence.
- –
- Antibiotic prophylaxis is not recommended for bronchoscopy, laryngoscopy, or transnasal or endotracheal intubation.
- –
- For invasive procedures to treat an established infection (i.e., drainage of abscesses), an empiric antibiotic regimen containing anti-staphylococcal activity (S. aureus) should be used.
- –
- Antibiotic prophylaxis is not recommended for gastroscopy, colonoscopy, low risk laparoscopic biliary tract procedures (see also the 2015 recommendations for perioperative antimicrobial prophylaxis of Swissnoso), cystoscopy, vaginal or caesarean delivery, or transesophageal echocardiography.
- –
- In the case of an established infection, an empiric antibiotic regimen containing anti-enterococcal activity should be used.
- –
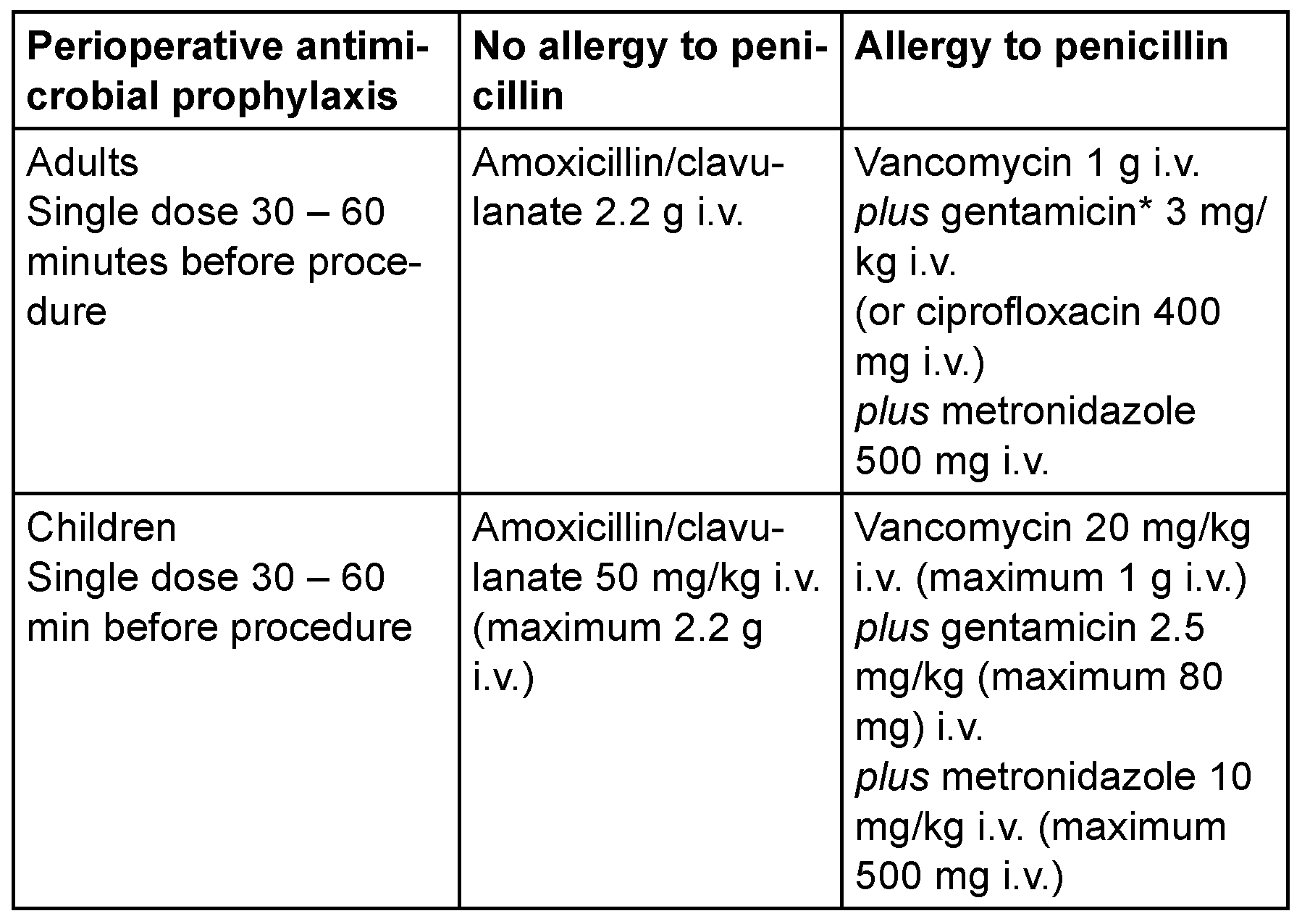
- If antibiotic therapy is indicated to prevent wound infection or sepsis associated with a gastrointestinal or genitourinary tract procedure, perioperative or peri-interventional antimicrobial prophylaxis containing antienterococcal activity should be used (see Table 1, dose recommendations are based on normal renal and liver function).
- –
- Antibiotic prophylaxis is not recommended for any procedure.
- –
- For surgical procedures on infected skin/skin structure (e.g., incision of skin abscess): an empiric antibiotic regimen should contain an agent with activity against staphylococci and beta-hemolytic streptococci.
- –
- Preoperative screening for nasal carriage of Staphylococcus aureus is recommended before elective cardiac surgery in order to treat carriers.
- –
- Local treatment without screening for S. aureus is not recommended.
- –
- Potential sources of infection (e.g., dental foci) should be treated/removed ≥2 weeks prior to the intervention.
- –
- Perioperative antibiotic prophylaxis is recommended before placement of a pacemaker or implantable cardioverter defibrillator.
- –
- Perioperative antibiotic prophylaxis should be administered in patients undergoing surgical or transcatheter implantation of a prosthetic valve, intravascular prosthetic or other foreign material (for example graft implantation for endovascular aneurysm repair).
- –
- Prophylaxis should be started immediately before the procedure and repeated if the procedure is prolonged. Prophylaxis should not be prolonged for longer than 48 hours.
Areas of uncertainty
Heart transplantation
Tonsillectomy
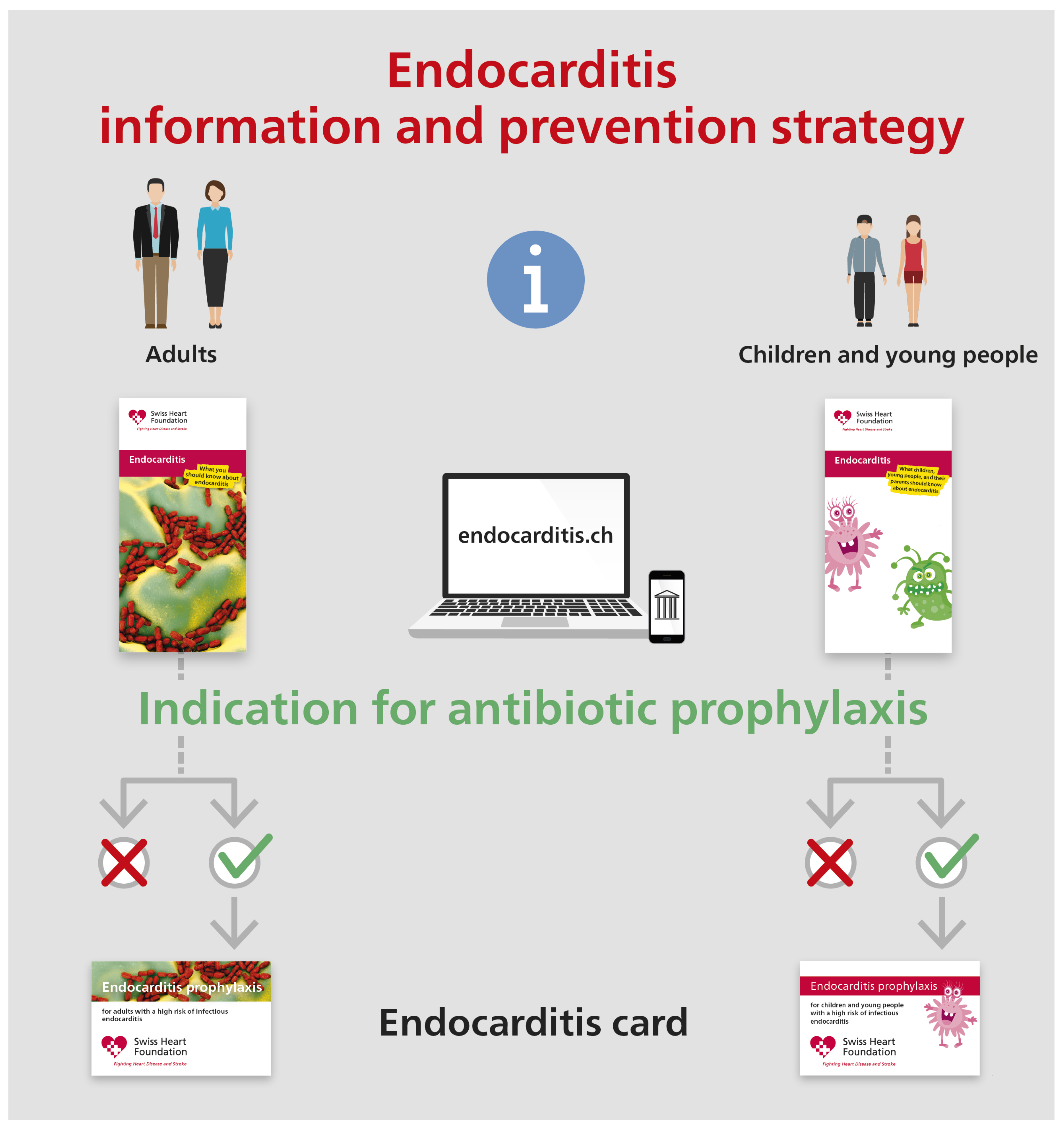
Information and communication strategy
- –
- Knowledge transfer to increase awareness for good dental and skin hygiene
- –
- Education on symptoms consistent with infective endocarditis and the appropriate steps when these symptoms occur (i.e., get in contact with the doctor, obtain blood culture prior to administration of antibiotic therapy)
Funding
Acknowledgments
References
- Jaussi, A.; Flückiger, U. Revidierte schweizerische Richtlinien für die Endokarditis- Prophylaxe. Kardiovaskuläre Medizin. 2008, 11, 392–400. [Google Scholar] [CrossRef]
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; et al.; ESC Scientific Document Group 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015, 36, 3075–3128. [Google Scholar] [CrossRef] [PubMed]
- Swissnoso. Nationales Zentrum für Infektionsprävention. Sample- Guideline: perioperative Antibiotikaprophylaxe. Available online: https://www.swissnoso.ch/fileadmin/module/ssi_intervention/Dokumente_D/4_Sample_Guidelines/180816_Sample-Guideline_AMP_de.pdf.
- Schweizerische Gesellschaft für Gastroenterologie; Société Suisse de Gastroentérologie; Societa Svizzera di Gastroenterologia. Antibiotic Prophylaxis for Gastrointestinal Endoscopy. Available online: https://sggssg.ch/fileadmin/user_upload/Antibiotikaprophylaxe_ in_der_Gastroenterologie_2018.pdf.
- François, M.; Bingen, E.H.; Lambert-Zechovsky, N.Y.; Mariani-Kurkdjian, P.; Nottet, J.B.; Narcy, P. Bacteremia during tonsillectomy. Arch Otolaryngol Head Neck Surg. 1992, 118, 1229–1231. [Google Scholar] [CrossRef] [PubMed]
- Kaygusuz, I.; Gök, U.; Yalçin, S.; Keleş, E.; Kizirgil, A.; Demirbağ, E. Bacteremia during tonsillectomy. Int J Pediatr Otorhinolaryngol. 2001, 58, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, I.; Okur, E.; Ciragil, P.; Aral, M.; Kilic, M.A.; Gul, M. Bacteraemia during tonsillectomy. J Laryngol Otol. 2003, 117, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Klug, T.E.; Henriksen, J.J.; Rusan, M.; Fuursted, K.; Ovesen, T. Bacteremia during quinsy and elective tonsillectomy: an evaluation of antibiotic prophylaxis recommendations for patients undergoing tonsillectomy. J Cardiovasc Pharmacol Ther. 2012, 17, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Milder, E.A.; Rizzi, M.D.; Morales, K.H.; Ross, R.K.; Lautenbach, E.; Gerber, J.S. Impact of a new practice guideline on antibiotic use with pediatric tonsillectomy. JAMA Otolaryngol Head Neck Surg. 2015, 141, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Wilson, W.; Taubert, K.A.; Gewitz, M.; Lockhart, P.B.; Baddour, L.M.; Levison, M.; et al.; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Surgery and Anesthesia; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation. 2007, 116, 1736–1754. [Google Scholar] [CrossRef] [PubMed]
 |
© 2022 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Swiss expert group on infective endocarditis prevention; Parham, S.; Barbara, H.; Michelle, F.; Ursula, F.; Katia, B.; Benoit, G.; Raban, J.; Stephan, Z.; Philipp, A.; et al. Infective Endocarditis: Prevention and Antibiotic Prophylaxis. Cardiovasc. Med. 2021, 24, 42. https://doi.org/10.4414/cvm.2021.02144
Swiss expert group on infective endocarditis prevention, Parham S, Barbara H, Michelle F, Ursula F, Katia B, Benoit G, Raban J, Stephan Z, Philipp A, et al. Infective Endocarditis: Prevention and Antibiotic Prophylaxis. Cardiovascular Medicine. 2021; 24(1):42. https://doi.org/10.4414/cvm.2021.02144
Chicago/Turabian StyleSwiss expert group on infective endocarditis prevention, Sendi Parham, Hasse Barbara, Frank Michelle, Flückiger Ursula, Boggian Katia, Guery Benoit, Jeger Raban, Zbinden Stephan, Agyeman Philipp, and et al. 2021. "Infective Endocarditis: Prevention and Antibiotic Prophylaxis" Cardiovascular Medicine 24, no. 1: 42. https://doi.org/10.4414/cvm.2021.02144
APA StyleSwiss expert group on infective endocarditis prevention, Parham, S., Barbara, H., Michelle, F., Ursula, F., Katia, B., Benoit, G., Raban, J., Stephan, Z., Philipp, A., Walter, K., & Matthias, G. (2021). Infective Endocarditis: Prevention and Antibiotic Prophylaxis. Cardiovascular Medicine, 24(1), 42. https://doi.org/10.4414/cvm.2021.02144




