Soluble ST2—A New Biomarker in Heart Failure
Summary
Introduction
Heart Failure—A Rapidly Advancing Field
Biomarkers in Heart Failure Patients: Strengths and Limitations
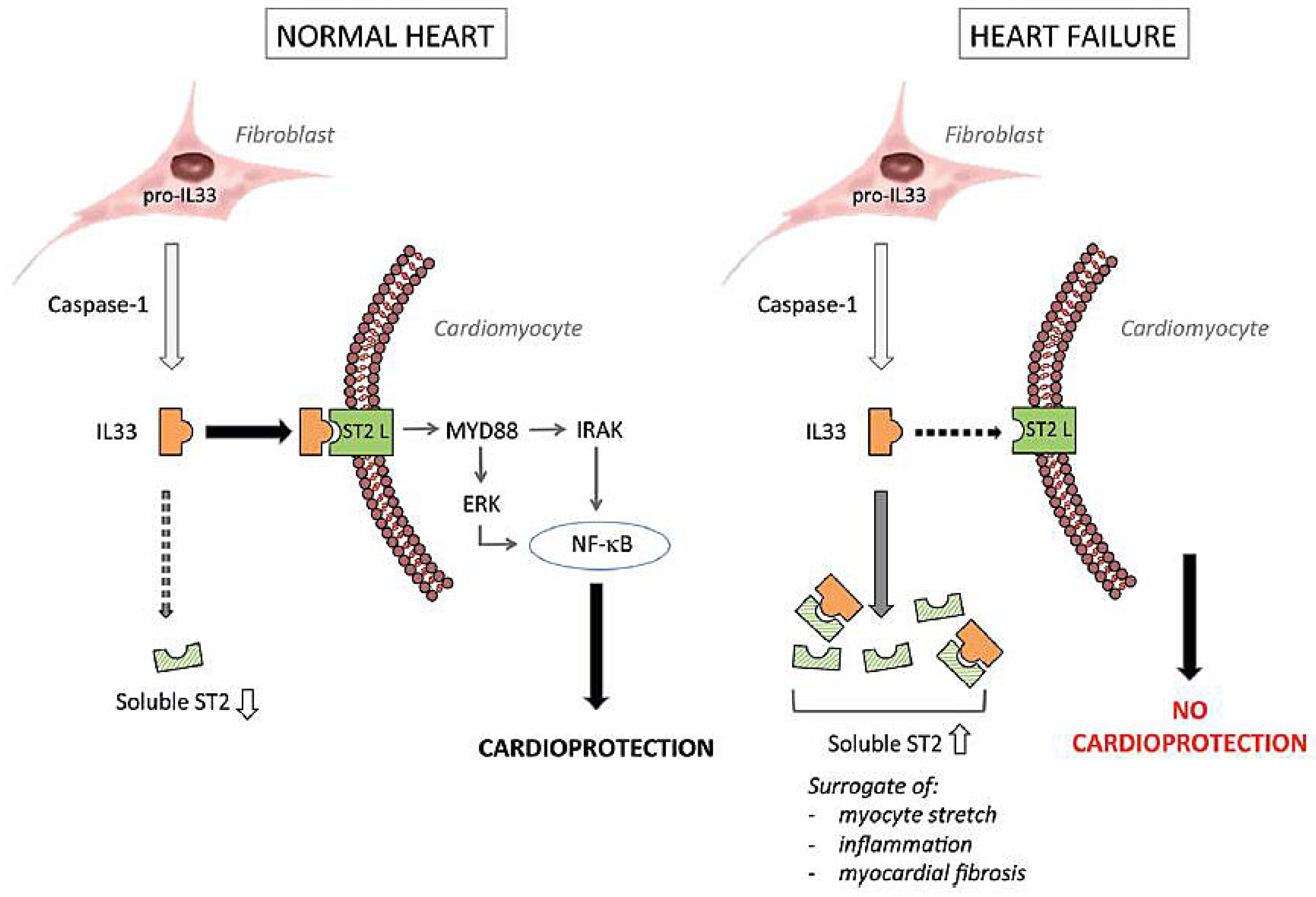
ST2 (Suppression of Tumourigenicity 2)
Measurement of sST2
Soluble ST2 in Clinical Settings
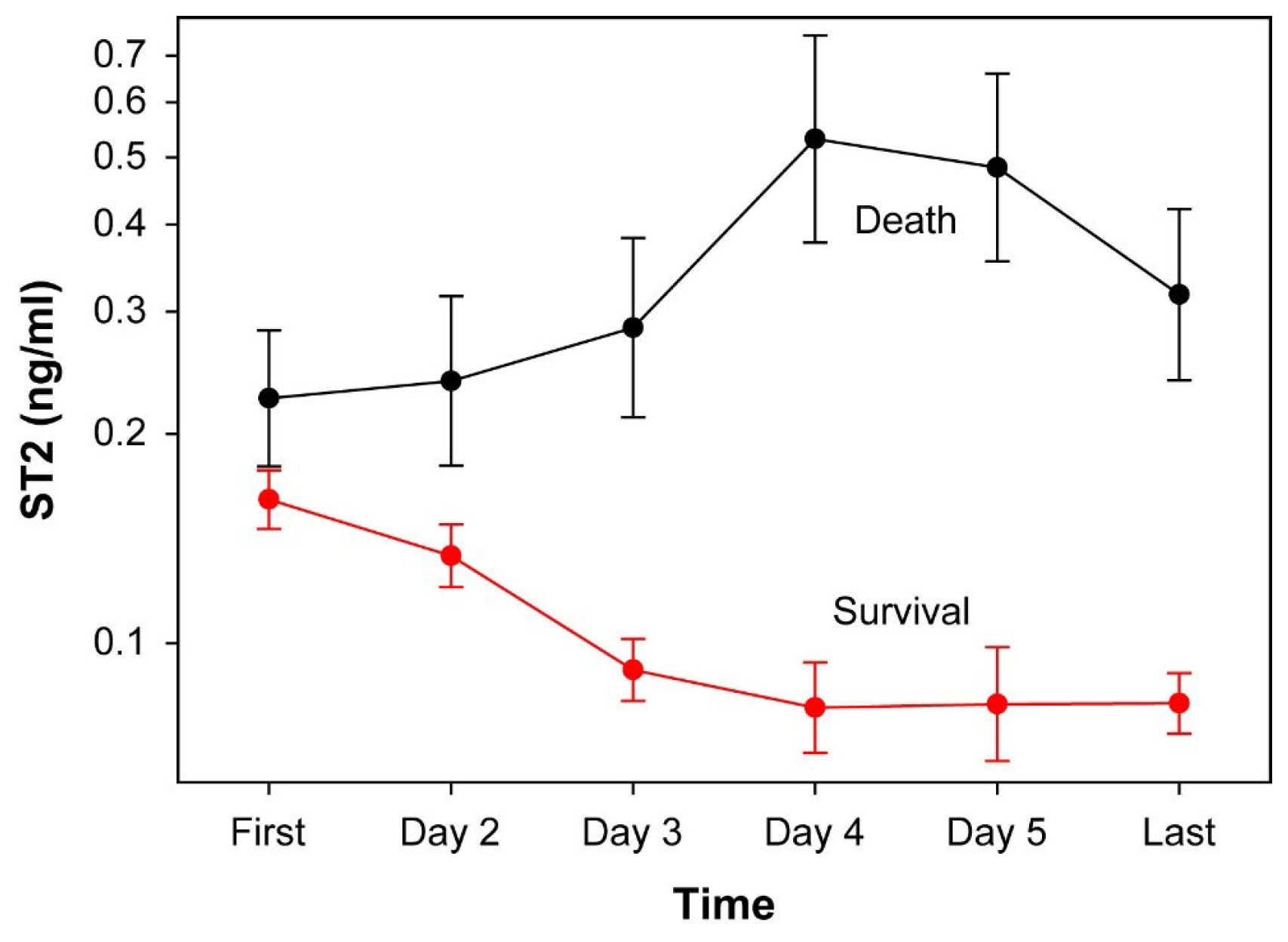
Acute Heart Failure
Chronic Heart Failure
The Swiss Experience
Areas of Uncertainty
Conclusions
Disclosure statement
Appendix A
| Title | Name | First Name | Address | City |
| Cand. med. | Ammann | Camille | HerzKlinik Hirslanden | Zurich, CH |
| Dr. med. | Arrigo | Mattia | USZ Universitäres Herzzentrum | Zurich, CH |
| PD Dr. med. | Biaggi | Patric | HerzKlinik Hirslanden | Zurich, CH |
| Dr. med. | Blümel | Sena | Universitätsspital Zürich | Zurich, CH |
| PD Dr. med. | Breidthardt | Tobias | Universitätsspital Basel | Basel, CH |
| Dumert | Werner | Bestbion | Köln, D | |
| Ph.D. | Gawinecka | Joanna | Universitätsspital Zürich | Zurich, CH |
| Dr. med. | Hammerer-Lercher | Angelika | Kantonsspital Aarau AG | Aarau, CH |
| Dr.phil.nat. | Horn | Michael P. | Inselspital Bern, ZLM | Bern, CH |
| Prof. Dr. med. | Hullin | Roger | Centre hospitalier universitaire Vaudois | Lausanne, CH |
| PD Dr. med. | Hunziker Munsch | Lukas | Inselspital Bern | Bern, CH |
| Dr.sc.nat. | Imperiali | Mauro | Centro medicina di laboratorio Dr. Risch | Pregassona, CH |
| Dr. med. | Krull | Nora | Unilabs LAS Ticino | Breganzona, CH |
| Dr. | Lüscher | Dieter | Zurich, CH | |
| Prof. Dr. med. | Maisel | Alan | University of California San Diego | San Diego, USA |
| Dr. med. | Mertens | Joachim C. P. | Universitätsspital Zürich | Zurich, CH |
| Prof. Dr. med. | Moccetti | Tiziano | Cardiocentro Ticino | Lugano, CH |
| Prof. Dr. med. | Müller | Christian | Universitätsspital Basel | Basel, CH |
| Prof. Dr. med. | Noll | Georg | HerzKlinik Hirslanden | Zurich, CH |
| Dr. med. | Pasotti | Elena | Cardiocentro Ticino | Lugano, Ch |
| Prof. Dr. med. | Risch | Lorenz | Labormedizinisches Zentrum Dr. Risch | Liebefeld, CH |
| Prof. Dr. med. | Ruschitzka | Frank | Universitätsspital Zürich | Zurich, CH |
| Dr.rer.nat. | Saleh | Lanja | Universitätsspital Zürich | Zurich, CH |
| Dr. med. | Scopigni | Francesca | Cardiocentro Ticino | Lugano, CH |
References
- Chow, S.L.; Maisel, A.S.; Anand, I.; Bozkurt, B.; de Boer, R.A.; Felker, G.M.; et al. American Heart Association Clinical Pharmacology Committee of the Council on Clinical Cardiology; Council on Basic Cardiovascular Sciences; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Epidemiology and Prevention; Council on Functional Genomics and Translational Biology; and Council on Quality of Care and Outcomes Research. Role of Biomarkers for the Prevention, Assessment, and Management of Heart Failure: A Scientific Statement From the American Heart Association Circulation 2017, 135, e1054–e1091. [Google Scholar] [CrossRef]
- Ammar, K.A.; Jacobsen, S.J.; Mahoney, D.W.; Kors, J.A.; Redfield, M.M.; Burnett, J.C., Jr.; et al. Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation 2007, 115, 1563–1570. [Google Scholar] [CrossRef]
- Desta, L.; Jernberg, T.; Löfman, I.; Hofman-Bang, C.; Hagerman, I.; Spaak, J.; et al. Incidence, temporal trends, and prognostic impact of heart failure complicating acute myocardial infarction. The SWEDEHEART Registry (Swedish Web-System for Enhancement and Development of Evidence- Based Care in Heart Disease Evaluated According to Recommended Therapies): A study of 199,851 patients admitted with index acute myocardial infarctions, 1996 to 2008. JACC Heart Fail. 2015, 3, 234–242. [Google Scholar] [CrossRef]
- Durand, E.; Doutriaux, M.; Bettinger, N.; Tron, C.; Fauvel, C.; Bauer, F.; et al. Incidence, Prognostic Impact, and Predictive Factors of Readmission for Heart Failure After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2017, 10, 2426–2436. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J.; Rowin, E.J.; Udelson, J.E.; Maron, M.S. Clinical Spectrum and Management of Heart Failure in Hypertrophic Cardiomyopathy. JACC Heart Fail. 2018, 6, 353–363. [Google Scholar] [CrossRef]
- Stewart, S.; MacIntyre, K.; Hole, D.J.; Capewell, S.; McMurray, J.J. More ‘malignant’ than cancer? Five-year survival following a first admission for heart failure. Eur. J. Heart Fail. 2001, 3, 315–322. [Google Scholar] [CrossRef]
- Group CTS; CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). N. E. J. Med. 1987, 316, 1429–1435. [Google Scholar] [CrossRef] [PubMed]
- Hjalmarson, A.; Goldstein, S.; Fagerberg, B.; Wedel, H.; Waagstein, F.; Kjek- shus, J.; et al. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999, 353, 2001–2007. [Google Scholar] [CrossRef]
- Pitt, B.; Zannad, F.; Remme, W.J.; Cody, R.; Castaigne, A.; Perez, A.; et al. Randomized Aldactone Evaluation Study Investigators. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N. E. J. Med. 1999, 341, 709–717. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; et al. PARADIGM-HF Investigators and Committees. Angiotensinneprilysin inhibition versus enalapril in heart failure. N. E. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef]
- Cleland, J.G.; Daubert, J.C.; Erdmann, E.; Freemantle, N.; Gras, D.; Kappen-berger, L.; et al.; Cardiac Resynchronization-Heart Failure (CARE-HF) Study Investigators The effect of cardiac resynchronization on morbidi- ty and mortality in heart failure. N. E. J. Med. 2005, 352, 1539–1549. [Google Scholar] [CrossRef]
- Bardy, G.H.; Lee, K.L.; Mark, D.B.; Poole, J.E.; Packer, D.L.; Boineau, R.; et al. Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N. E. J. Med. 2005, 352, 225–237. [Google Scholar] [CrossRef]
- Køber, L.; Thune, J.J.; Nielsen, J.C.; Haarbo, J.; Videbæk, L.; Korup, E. DANISH Investigators. Defibrillator Implantation in Patients with Nonischemic Systolic Heart Failure. N. E. J. Med. 2016, 375, 1221–1230. [Google Scholar] [CrossRef]
- Koehler, F.; Koehler, K.; Deckwart, O.; Prescher, S.; Wegscheider, K.; Kirwan, B.A.; et al. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet 2018, 392, 1047–1057. [Google Scholar] [CrossRef]
- Herrmann, H.C.; Pibarot, P.; Hueter, I.; Gertz, Z.M.; Stewart, W.J.; Kapadia, S.; et al. Predictors of mortality and outcomes of therapy in low-flow severe aortic stenosis: a Placement of Aortic Transcatheter Valves (PARTNER) trial analysis. Circulation 2013, 127, 2316–2326. [Google Scholar] [CrossRef] [PubMed]
- Mack, M.J.; Leon, M.B.; Smith, C.R.; Miller, D.C.; Moses, J.W.; Tuzcu, E.M.; et al. PARTNER 1 trial investigators. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): A randomised controlled trial. Lancet 2015, 385, 2477–2784. [Google Scholar] [CrossRef] [PubMed]
- Obadia, J.F.; Messika-Zeitoun, D.; Leurent, G.; Iung, B.; Bonnet, G.; Piriou, N.; et al. MITRA-FR Investigators. Percutaneous Repair or Medical Treat- ment for Secondary Mitral Regurgitation. N. E. J. Med. 2018, 379, 2297–2306. [Google Scholar] [CrossRef] [PubMed]
- Stone, G.W.; Lindenfeld, J.; Abraham, W.T.; Kar, S.; Lim, D.S.; Mishell, J.M.; et al. COAPT Investigators. Transcatheter Mitral-Valve Repair in Patients with Heart Failure. N. E. J. Med. 2018, 379, 2307–2318. [Google Scholar] [CrossRef]
- Januzzi, J.L.; Jr Filippatos, G.; Nieminen, M.; Gheorghiade, M. Troponin elevation in patients with heart failure: on behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur. Heart J. 2012, 33, 2265–2271. [Google Scholar] [CrossRef]
- Anand, I.S.; Latini, R.; Florea, V.G.; Kuskowski, M.A.; Rector, T.; Masson, S.; et al. Val-HeFT Investigators. C-reactive protein in heart failure: prognos- tic value and the effect of valsartan. Circulation 2005, 112, 1428–1434. [Google Scholar] [CrossRef]
- Maisel, A.S.; Krishnaswamy, P.; Nowak, R.M.; McCord, J.; Hollander, J.E.; Duc, P.; et al. Breathing Not Properly Multinational Study Investigators Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N. E. J. Med. 2002, 347, 161–167. [Google Scholar] [CrossRef]
- Januzzi, J.L.; van Kimmenade, R.; Lainchbury, J.; Bayes-Genis, A.; Ordonez- Llanos, J.; Santalo-Bel, M.; et al. NT-proBNP testing for diagnosis and short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1256 patients: the International Collaborative of NT-proBNP Study. Eur. Heart J. 2006, 27, 330–337. [Google Scholar] [CrossRef]
- Pfisterer, M.; Buser, P.; Rickli, H.; Gutmann, M.; Erne, P.; Rickenbacher, P.; et al. TIME-CHF Investigators. BNP-guided vs. symptom-guided heart failure therapy: the Trial of Intensified vs. Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. JAMA 2009, 301, 383–392. [Google Scholar] [CrossRef]
- Troughton, R.W.; Frampton, C.M.; Brunner-La Rocca, H.P.; Pfisterer, M.; Eurlings, L.W.; Erntell, H.; et al. Effect of B-type natriuretic peptide-guided treatment of chronic heart failure on total mortality and hospitalization: an individual patient meta-analysis. Eur. Heart J. 2014, 35, 1559–1567. [Google Scholar] [CrossRef]
- Bettencourt, P.; Azevedo, A.; Pimenta, J.; Friões, F.; Ferreira, S.; Ferreira, A. N-terminal-pro-brain natriuretic peptide predicts outcome after hospital discharge in heart failure patients. Circulation 2004, 110, 2168–2174. [Google Scholar] [CrossRef]
- Hartmann, F.; Packer, M.; Coats, A.J.S.; Fowler, M.B.; Krum, H.; Mohacsi, P.; et al. Prognostic impact of plasma N-terminal pro-brain natriuretic peptide in severe chronic congestive heart failure: a substudy of the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) trial. Circulation 2004, 110, 1780–1786. [Google Scholar] [CrossRef] [PubMed]
- Eurlings, L.W.; van Pol, P.E.; Kok, W.E.; van Wijk, S.; Lodewijks-van der Bolt, C.; Balk, A.H.; et al. Management of chronic heart failure guided by individual N-terminal pro-B-type natriuretic peptide targets: results of the PRIMA (Can PRo-brain-natriuretic peptide guided therapy of chronic heart failure IMprove heart fAilure morbidity and mortality?) study. J. Am. Coll. Cardiol. 2010, 56, 2090–2100. [Google Scholar] [CrossRef]
- Felker, G.M.; Anstrom, K.J.; Adams, K.F.; Ezekowitz, J.A.; Fiuzat, M.; Houston-Miller, N.; et al. Effect of Natriuretic Peptide-Guided Therapy on Hospitalization or Cardiovascular Mortality in High-Risk Patients With Heart Failure and Reduced Ejection Fraction: A Randomized Clinical Trial. JAMA 2017, 318, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Brann, A.; Chang, K.W.; Maisel, A.S. The Confounding Effects of Non-cardiac Pathologies on the Interpretation of Cardiac Biomarkers. Curr. Heart Fail. Rep. 2018, 15, 239–49. [Google Scholar] [CrossRef] [PubMed]
- Srisawasdi, P.; Vanavanan, S.; Charoenpanichkit, C.; Kroll, M.H. The effect of renal dysfunction on BNP, NT-proBNP, and their ratio. Am. J. Clin. Pathol. 2010, 133, 14–23. [Google Scholar] [CrossRef]
- Bayes-Genis, A.; Zamora, E.; de Antonio, M.; Galán, A.; Vila, J.; Urrutia, A.; et al. Soluble ST2 serum concentration and renal function in heart failure. J. Card Fail. 2013, 19, 768–75. [Google Scholar] [CrossRef]
- Mehra, M.R.; Uber, P.A.; Park, M.H.; Scott, R.L.; Ventura, H.O.; Harris, B.C.; et al. Obesity and suppressed B-type natriuretic peptide levels in heart failure. J. Am. Coll. Cardiol. 2004, 43, 1590–1595. [Google Scholar] [CrossRef]
- Corell, P.; Gustafsson, F.; Kistorp, C.; Madsen, L.H.; Schou, M.; Hildebrandt, P. Effect of atrial fibrillation on plasma NT-proBNP in chronic heart failure. Int. J. Cardiol. 2007, 117, 395–402. [Google Scholar] [CrossRef]
- Wang, T.J.; Larson, M.G.; Levy, D.; Benjamin, E.J.; Corey, D.; Leip, E.P.; et al. Heritability and genetic linkage of plasma natriuretic peptide levels. Circulation 2003, 108, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Sanada, S.; Hakuno, D.; Higgins, L.J.; Schreiter, E.R.; McKenzie, A.N.J.; Lee, R.T. IL-33 and ST2 comprise a critical biomechanically induced and cardioprotective signaling system. J. Clin. Invest. 2007, 117, 1538–1549. [Google Scholar] [CrossRef] [PubMed]
- Seki, K.; Sanada, S.; Kudinova, A.Y.; Steinhauser, M.L.; Handa, V.; Gannon, J.; et al. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail. 2009, 2, 684–691. [Google Scholar] [CrossRef]
- Pascual-Figal, D.A.; Januzzi, J.L. The biology of ST2: the International ST2 Consensus Panel. Am. J. Cardiol. 2015, 115 (Suppl. S7), 3B–7B. [Google Scholar] [CrossRef] [PubMed]
- Bayés-Genís, A.; Núñez, J.; Lupón, J. Soluble ST2 for Prognosis and Monitoring in Heart Failure: The New Gold Standard? J. Am. Coll. Cardiol. 2017, 70, 2389–2392. [Google Scholar] [CrossRef]
- Bartunek, J.; Delrue, L.; Van Durme, F.; Muller, O.; Casselman, F.; De Wiest, B.; et al. Nonmyocardial production of ST2 protein in human hypertrophy and failure is related to diastolic load. J. Am. Coll. Cardiol. 2008, 52, 2166–2174. [Google Scholar] [CrossRef]
- Sun, Z.J.; Chang, B.X.; Gao, M.M.; Zhang, J.Y.; Zou, Z.S. IL-33-ST2 Axis in Liver Disease: Progression and Challenge. Mediat Inflamm. 2017. [CrossRef]
- Wu, A.H.; Wians, F.; Jaffe, A. Biological variation of galectin-3 and soluble ST2 for chronic heart failure: implication on interpretation of test results. Am. Heart J. 2013, 165, 995–999. [Google Scholar] [CrossRef]
- Coglianese, E.E.; Larson, M.G.; Vasan, R.S.; Ho, J.E.; Ghorbani, A.; McCabe, E.L.; et al. Distribution and clinical correlates of the interleukin receptor family member soluble ST2 in the Framingham Heart Study. Clin. Chem. 2012, 58, 1673–1681. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Snider, J.V.; Grenache, D.G. Establishment of reference intervals for soluble ST2 from a United States population. Clin. Chim. Acta. 2010, 411, 1825–1826. [Google Scholar] [CrossRef]
- Rehman, S.U.; Mueller, T.; Januzzi, J.L., Jr. Characteristics of the novel interleukin family biomarker ST2 in patients with acute heart failure. J. Am. Coll. Cardiol. 2008, 52, 1458–1465. [Google Scholar] [CrossRef] [PubMed]
- Januzzi, J.; Grp, P.S. Measurement of soluble ST2 concentrations is useful for the evaluation of patients with acute dyspnea. Eur. Heart J. 2007, 28, 552. [Google Scholar]
- Shah, R.V.; Chen-Tournoux, A.A.; Picard, M.H.; van Kimmenade, R.R.J.; Januzzi, J.L. Serum levels of the interleukin-1 receptor family member ST2, cardiac structure and function, and long-term mortality in patients with acute dyspnea. Circ Heart Fail. 2009, 2, 311–319. [Google Scholar] [CrossRef]
- Broch, K.; Ueland, T.; Nymo, S.H.; Kjekshus, J.; Hulthe, J.; Muntendam, P.; et al. Soluble ST2 is associated with adverse outcome in patients with heart failure of ischaemic aetiology. Eur. J. Heart Fail. 2012, 14, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Manzano-Fernández, S.; Mueller, T.; Pascual-Figal, D.; Truong, Q.A.; Januzzi, J.L. Usefulness of soluble concentrations of interleukin family member ST2 as predictor of mortality in patients with acutely decompensated heart failure relative to left ventricular ejection fraction. Am. J. Cardiol. 2011, 107, 259–267. [Google Scholar] [CrossRef]
- Boisot, S.; Beede, J.; Isakson, S.; Chiu, A.; Clopton, P.; Januzzi, J.; et al. Serial sampling of ST2 predicts 90-day mortality following destabilized heart failure. J. Card Fail. 2008, 14, 732–738. [Google Scholar] [CrossRef]
- van Vark, L.C.; Lesman-Leegte, I.; Baart, S.J.; Postmus, D.; Pinto, Y.M.; Orsel, J.G.; et al. TRIUMPH Investigators. Prognostic Value of Serial ST2 Measurements in Patients With Acute Heart Failure. J. Am. Coll. Cardiol. 2017, 70, 2378–2388. [Google Scholar] [CrossRef]
- Manzano-Fernández, S.; Januzzi, J.L.; Pastor-Pérez, F.J.; Bonaque-González, J.C.; Boronat-Garcia, M.; Pascual-Figal, D.A.; et al. Serial monitoring of soluble interleukin family member ST2 in patients with acutely decompensated heart failure. Cardiology 2012, 122, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Breidthardt, T.; Balmelli, C.; Twerenbold, R.; Mosimann, T.; Espinola, J.; Haaf, P.; et al. Heart failure therapy-induced early ST2 changes may offer long-term therapy guidance. J. Card Fail. 2013, 19, 821–828. [Google Scholar] [CrossRef]
- Aimo, A.; Vergaro, G.; Ripoli, A.; Bayes-Genis, A.; Pascual Figal, D.A.; de Boer, R.A.; et al. Meta-Analysis of Soluble Suppression of Tumorigenici-ty-2 and Prognosis in Acute Heart Failure. JACC Heart Fail. 2017, 5, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, E.O.; Shimpo, M.; Hurwitz, S.; Tominaga, S.; Rouleau, J.L.; Lee, R.T. Identification of serum soluble ST2 receptor as a novel heart failure bio- marker. Circulation 2003, 107, 721–726. [Google Scholar] [CrossRef]
- Felker, G.M.; Fiuzat, M.; Thompson, V.; Shaw, L.K.; Neely, M.L.; Adams, K.F.; et al. Soluble ST2 in ambulatory patients with heart failure: Association with functional capacity and long-term outcomes. Circ Heart Fail. 2013, 6, 1172–1179. [Google Scholar] [CrossRef]
- Gaggin, H.K.; Motiwala, S.; Bhardwaj, A.; Parks, K.A.; Januzzi, J.L., Jr. Soluble concentrations of the interleukin receptor family member ST2 and β-blocker therapy in chronic heart failure. Circ Heart Fail. 2013, 6, 1206–1213. [Google Scholar] [CrossRef] [PubMed]
- O’Meara, E.; Prescott, M.F.; Claggett, B.; Rouleau, J.L.; Chiang, L.M.; Solomon, S.D.; et al. Independent Prognostic Value of Serum Soluble ST2 Measure- ments in Patients With Heart Failure and a Reduced Ejection Fraction in the PARADIGM-HF Trial (Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure). Circ Heart Fail. 2018, 11. [Google Scholar] [CrossRef]
- Puelacher, C.; Lurati Buse, G.; Seeberger, D.; Sazgary, L.; Marbot, S.; Lampart, A.; et al. BASEL-PMI Investigators. Perioperative Myocardial Injury After Noncardiac Surgery: Incidence, Mortality, and Characterization. Circulation 2018, 137, 1221–1232. [Google Scholar] [CrossRef]
- Maisel, A.S.; Di Somma, S. Do we need another heart failure biomarker: focus on soluble suppression of tumorigenicity 2 (sST2). Eur. Heart J. 2017, 38, 2325–2333. [Google Scholar]
- Wang, T.J.; Wollert, K.C.; Larson, M.G.; Coglianese, E.; McCabe, E.L.; Cheng, S.; et al. Prognostic utility of novel biomarkers of cardiovascular stress: the Framingham Heart Study. Circulation 2012, 126, 1596–1604. [Google Scholar] [CrossRef]
- Hughes, M.F.; Appelbaum, S.; Havulinna, A.S.; Jagodzinski, A.; Zeller, T.; Kee, F.; et al.; FINRISK and BiomarCaRE investigators ST2 may not be a useful predictor for incident cardiovascular events, heart failure and mortality. Heart 2014, 100, 1715–1721. [Google Scholar] [CrossRef] [PubMed]
| Male gender | Age | Obesity | Non White | Renal Impairment | During Dialysis | Sepsis | Afib | |
|---|---|---|---|---|---|---|---|---|
| Troponin | ↑ | ↑ | ↑ | ↑ | ↑ | ↓ | ↑ | ↑ |
| (NTpro)BNP | ↓ | ↑ | ↓ | ↓ | ↑ | ↓ | ↑ | ↑ |
| PCT | n/a | n/a | ↑ | n/a | ↑ | ↓ | ↑ | n/a |
| sST2 | ↑ | ↑ | <-> | <-> | <-> | <-> | ↑ | <-> |
| Men, Percentile | Women, Percentile | |||||||
|---|---|---|---|---|---|---|---|---|
| Age group, years | 2.5th | 50th | 97.5th | 99th | 2.5th | 50th | 97.5th | 99th |
| Empirical reference limits | ||||||||
| 35–44 | 10.6 | 22.9 | 47.6 | 49.3 | 10.4 | 17.1 | 33.2 | 45.9 |
| 45–54 | 11.5 | 22.3 | 43.7 | 64.4 | 9.8 | 17.7 | 30.7 | 36.7 |
| 55–64 | 12.4 | 22.7 | 43.3 | 46.4 | 9.9 | 17.5 | 34.3 | 39.3 |
| 65–74 | 13.2 | 24.5 | 45.2 | 54.7 | 9.3 | 19.2 | 45.1 | 53.0 |
| Quantile regression reference limits | ||||||||
| 35–44 | 10.3 | 21.3 | 46.5 | 46.7 | 10.2 | 16.6 | 29.4 | 29.5 |
| 45–54 | 11.2 | 22.0 | 45.8 | 48.7 | 10.0 | 17.2 | 31.2 | 34.0 |
| 55–64 | 12.1 | 22.8 | 45.2 | 50.8 | 9.8 | 17.8 | 33.2 | 39.3 |
| 65–74 | 13.1 | 23.6 | 44.6 | 53.0 | 9.6 | 18.5 | 35.3 | 45.3 |
© 2019 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Patric, B.; Camille, A.; Mauro, I.; Angelika, H.-L.; Tobias, B.; Christian, M.; Alan, M.; Frank, R. Soluble ST2—A New Biomarker in Heart Failure. Cardiovasc. Med. 2019, 22, w02008. https://doi.org/10.4414/cvm.2019.02008
Patric B, Camille A, Mauro I, Angelika H-L, Tobias B, Christian M, Alan M, Frank R. Soluble ST2—A New Biomarker in Heart Failure. Cardiovascular Medicine. 2019; 22(1):w02008. https://doi.org/10.4414/cvm.2019.02008
Chicago/Turabian StylePatric, Biaggi, Ammann Camille, Imperiali Mauro, Hammerer-Lercher Angelika, Breidthardt Tobias, Müller Christian, Maisel Alan, and Ruschitzka Frank. 2019. "Soluble ST2—A New Biomarker in Heart Failure" Cardiovascular Medicine 22, no. 1: w02008. https://doi.org/10.4414/cvm.2019.02008
APA StylePatric, B., Camille, A., Mauro, I., Angelika, H.-L., Tobias, B., Christian, M., Alan, M., & Frank, R. (2019). Soluble ST2—A New Biomarker in Heart Failure. Cardiovascular Medicine, 22(1), w02008. https://doi.org/10.4414/cvm.2019.02008




