Abstract
A growing number of patients with severe and diffuse obstructive coronary artery disease who are not candidates for revascularisation have debilitating angina despite medical therapy. We report the case of a 67-year-old man suffering from chronic refractory angina who was effectively treated with a coronary sinus reducer.
Case report
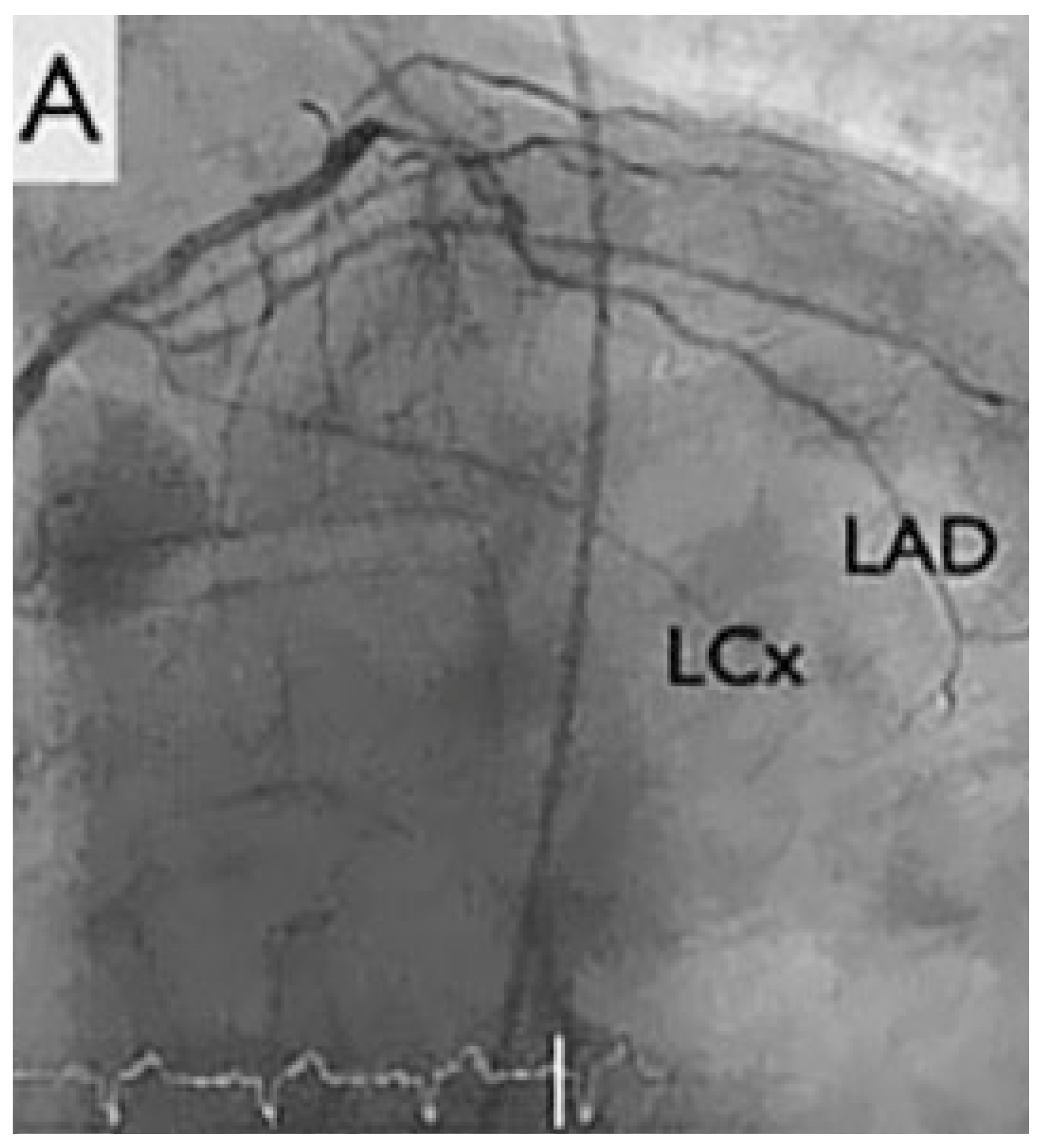
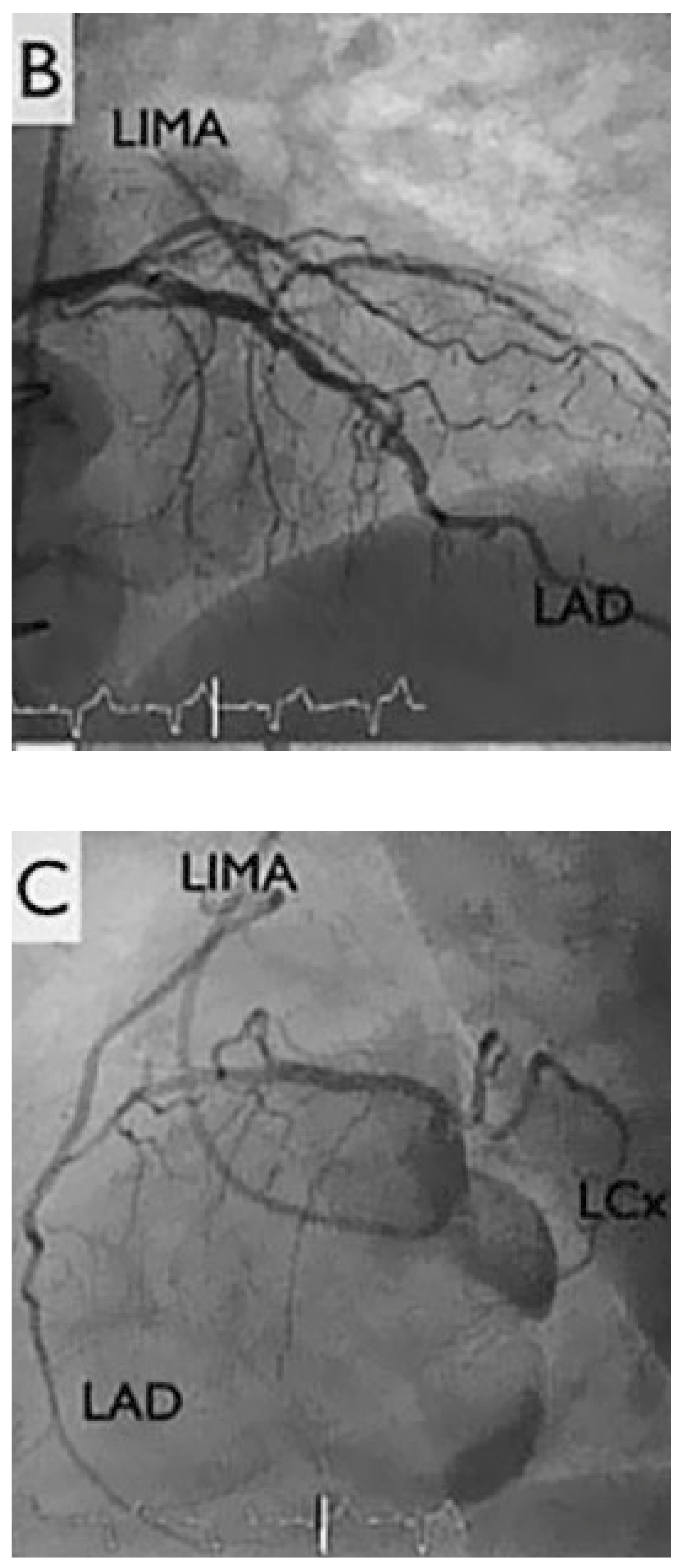
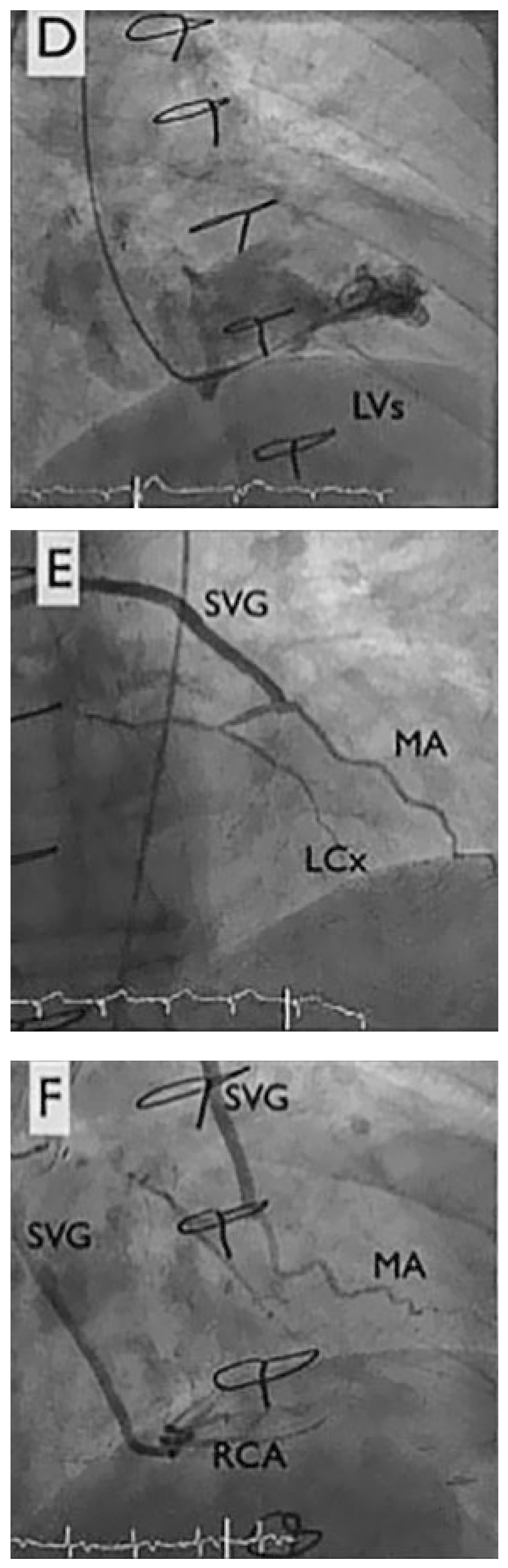
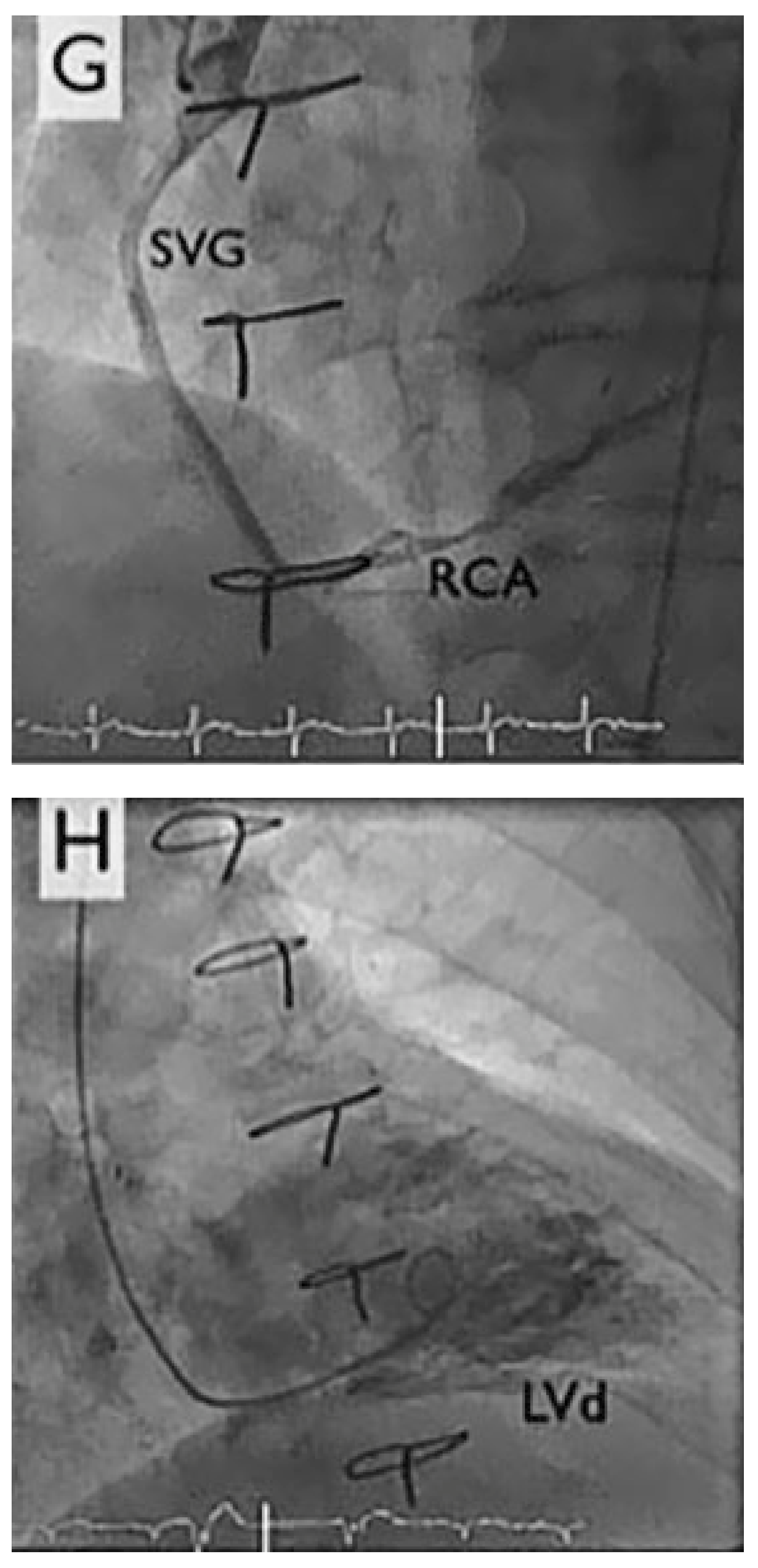
A 67-year-old diabetic patient with three-vessel coronary artery disease (Figure 1) and prior coronary artery bypass graft surgery (left internal mammary artery to left anterior descending artery, vein to marginal branch, vein to right coronary artery) suffered from refractory angina. Coronary angiography demonstrated good results after surgical revascularisation, but also a diffuse infiltration of the left coronary tree. Left ventricular systolic function was normal. The patient presented refractory angina despite optimal antianginal therapy comprising beta-blockers, nitrates, ranolazine (Ranexa®) and molsidomine (Corvaton®). The patient was severely disabled, being unable to walk 200 metres without nitrates, and waking up every 2 hours because of angina and paroxysmal dyspnoea. The treadmill test showed ischaemia.
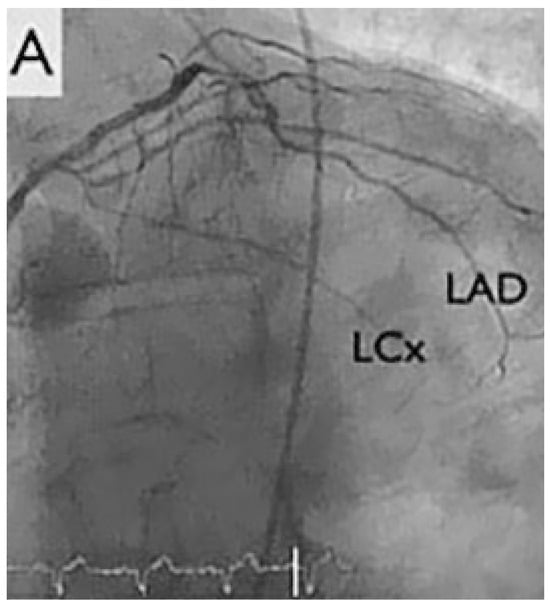
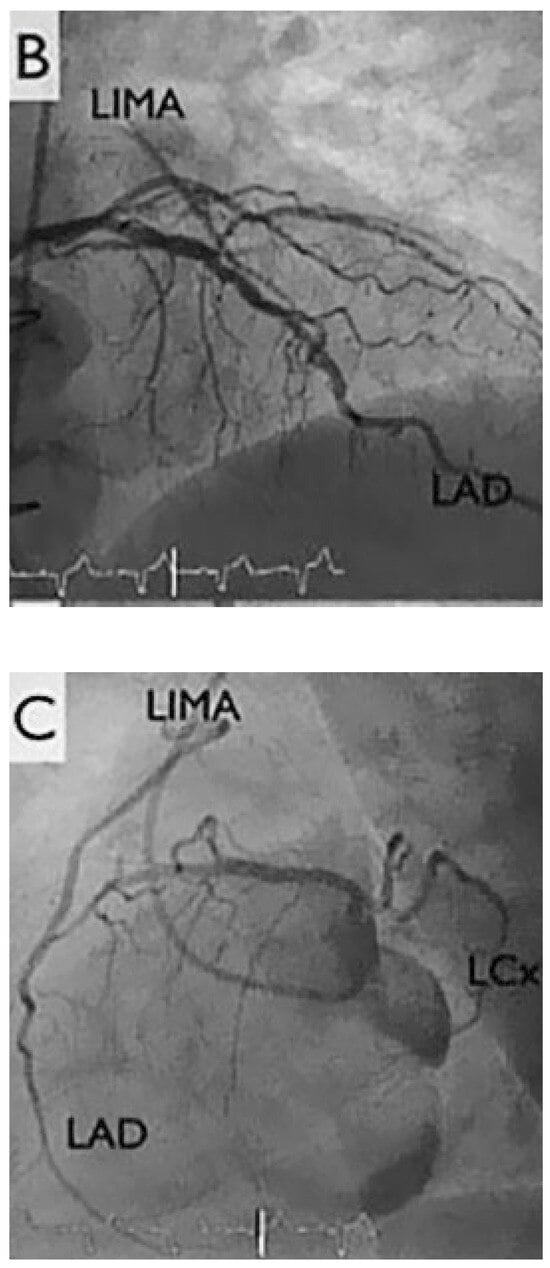
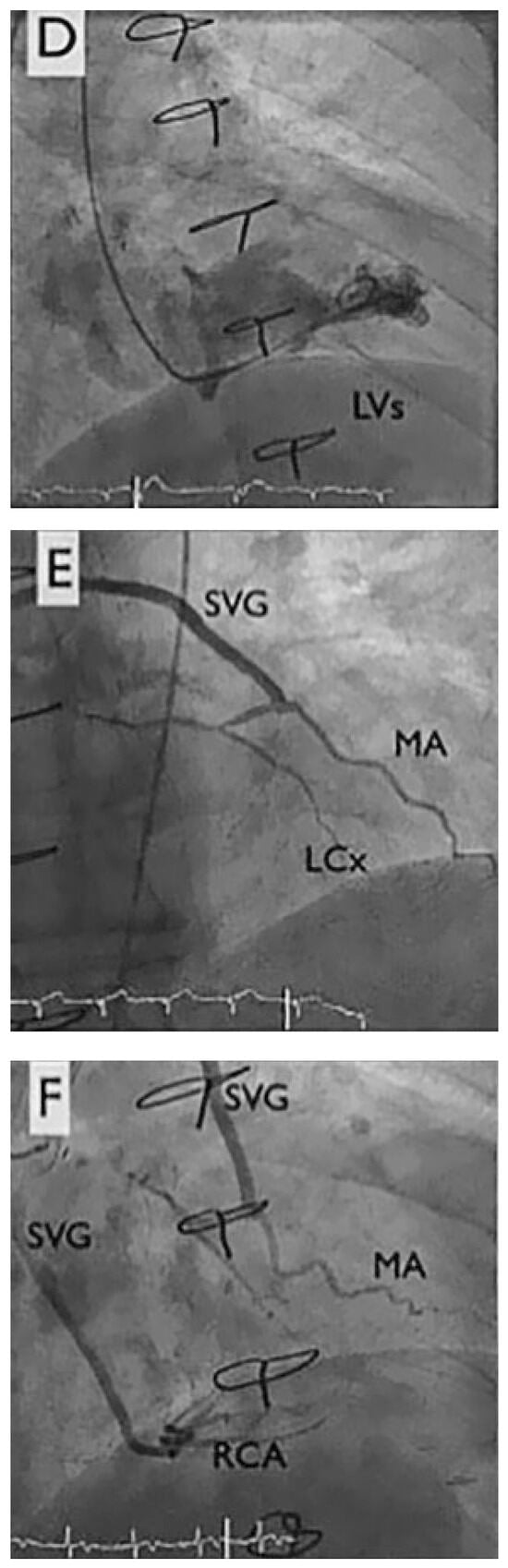
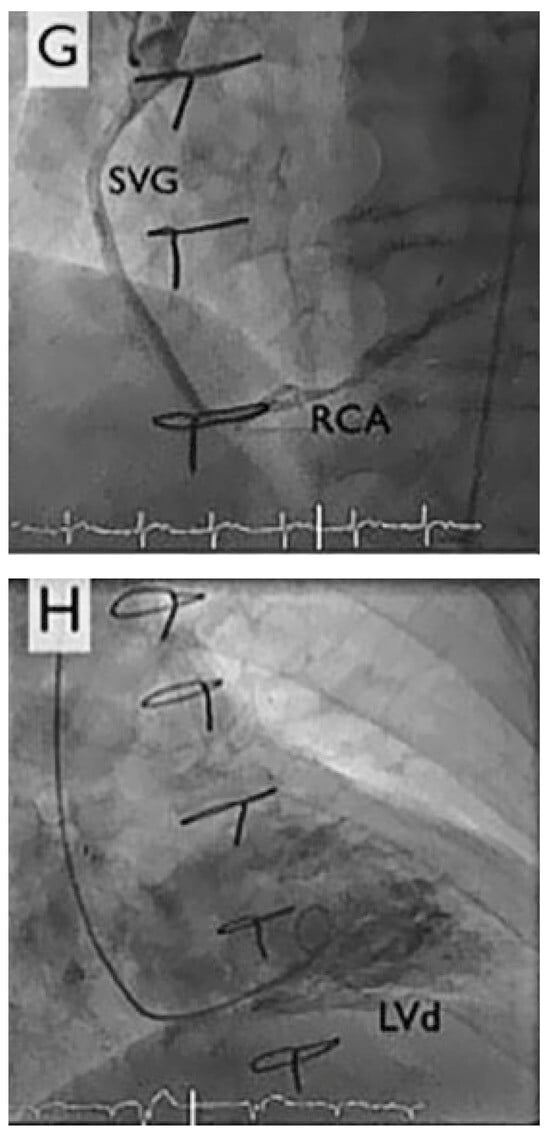
Figure 1.
Coronary angiogram. LAD: left anterior descending artery, LCx: left circumflex artery, LIMA: left internal mammary artery, MA: marginal artery, RCA: right coronary artery, ous vein graft; LVS: left ventricular tele-systolic volume; LVD: left ventricular tele-diastolic volume.
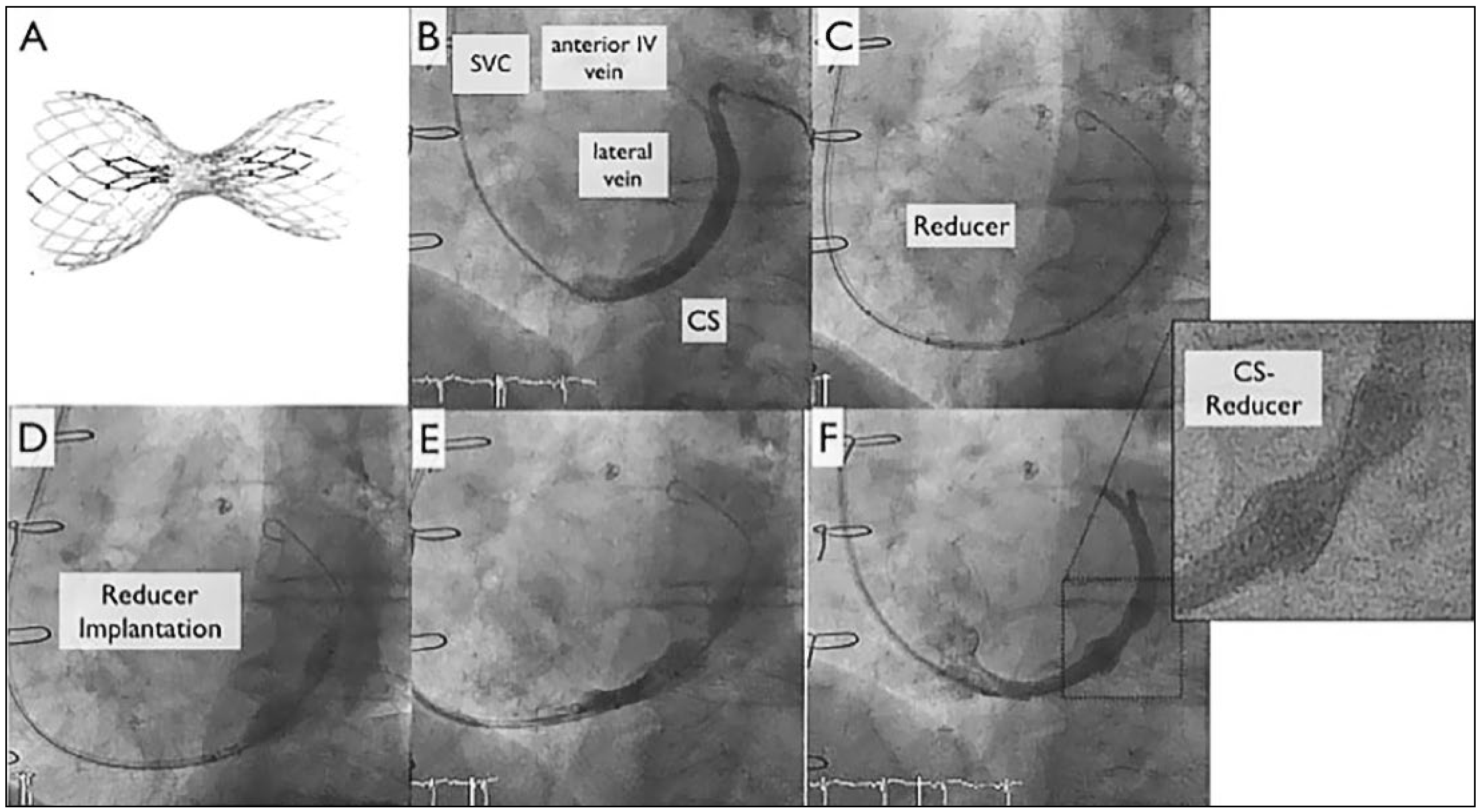
Coronary reduction (Figure 2A–F)
The right internal jugular vein was accessed under ultrasound guidance, followed by venography and measurement of the coronary sinus diameter (7 mm, central part). A 9 French delivery sheath was placed within the coronary sinus under fluoroscopic guidance. The reducer stent (Neovasc Inc., Richmond B.C., Canada) (Figure 2A), premounted on an hourglass shaped balloon catheter, was implanted downstream from the middle cardiac vein in the coronary sinus after a 5 atm. inflation of the balloon (Figure 2D). After de-inflation of the balloon and withdrawal of the balloon catheter, venography showed a 3-mm central restriction with good results (Figure 2F). The intervention was without complications such as occlusion, dissection of the coronary sinus, or bleeding at the jugular puncture site. The patient was discharged with 6 months of dual antiplatelet therapy (aspirin and clopidogrel). At 3-month follow-up, the patient was significantly improved, with complete disappearance of nocturnal events, significant improvement in exercise tolerance and improvement by two Canadian Cardiovascular Society (CCS) angina classes (IV to II).
Figure 2.
Coronary sinus reduction. Panel A by courtesy of Neovasc Inc., Richmond B.C., Canada. CS: coronary sinus, SVC: superior vena cava.
Figure 2.
Coronary sinus reduction. Panel A by courtesy of Neovasc Inc., Richmond B.C., Canada. CS: coronary sinus, SVC: superior vena cava.
Discussion
Refractory angina is defined as the persistence of angina pectoris despite optimal conventional therapy. The incidence of refractory angina is variable depending on the definition, but it is estimated to affect 5% of patients with chronic coronary heart disease. Despite significant advances in revascularisation options (surgical and/or percutaneous), the incidence of refractory angina has increased over the recent decades, in line with increased life expectancy. First-line treatment options include chronotropic agents (beta-blockers, ivabradine) and vasoactive agents (calcium channel blockers, nitrates or other direct nitric oxide donors, ATP-sensitive potassium channel openers, late sodium current inhibitors and rho-kinase inhibitors). In a minority of patients, additional therapies are needed: epidural neuromodulation, extracorporeal shockwave therapy, stem cell therapy and, more recently, coronary sinus reduction.
Beck and Leighninger first described a surgical procedure involving partial occlusion of the coronary sinus to treat refractory angina [2]. The putative mechanism is that the increase of pressure in the coronary sinus leads to a reduction of subendocardial ischaemia by redistribution of collateral blood flow from non- ischaemic epicardium to ischaemic endocardium. Percutaneous coronary sinus reduction consists of implanting an hourglass-shaped stent within the coronary sinus [3]. The subsequent healing of the stent creates a narrowing of the coronary sinus and increases the venous coronary blood draining pressure. Recently, a randomised, single-blinded, sham-controlled trial including 104 patients suffering from refractory angina of CCS class III or IV with evidence of reversible ischaemia and a left ventricular ejection fraction >25%, showed significant improvement in symptoms and quality of life [4].
Implantation of the coronary sinus reducer to reduce refractory angina is a safe procedure. Potential complications include dissection, perforation, thrombotic occlusion of the coronary sinus or migration of the device. So far, only one case of coronary sinus perforation following reducer implantation has been described [5]. The procedure is believed to relieve symptoms in 70 to 80% of patients. Nonresponse in the remaining 20 to 30% is thought to be due to: suboptimal patient selection, symptoms caused by heart failure and not ischaemia, and the presence of an existing alternative drainage venous system of the myocardium (the Thebesian venous system) [1]. Measurement of right atrial pressure before implantation and of coronary sinus systolic pressure during balloon occlusion has recently been reported as an simple method that could predict, during the intervention, good responders who will achieve a high differential pressure [6].
Coronary sinus reduction is unsuitable in cases of right coronary artery ischaemia as some small cardiac veins from this territory drain close to the coronary sinus ostium, and the device is usually placed more distally, 2 cm downstream from the ostium [1].
More studies are needed in the field, especially with objective measures of myocardial ischemia improvement, such as positron emission tomography-computed tomography or cardiac magnetic resonance imaging. Currently, a European multicentre observational clinical trial aiming to enrol 400 patients is underway, and a double-blind randomised sham trial is expected to start shortly in the United States and Canada.
Conflicts of Interest
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Konigstein, M.; Giannini, F.; Banai, S. The Reducer device in patients with angina pectoris: mechanisms, indications, and perspectives. Eur Heart J. 2017, 209, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Beck, C.S.; Leighninger, D.S. Operations for coronary artery disease. J Am Med Assoc. 1954, 156, 1226–1233. [Google Scholar] [CrossRef] [PubMed]
- Banai, S.; Ben Muvhar, S.; Parikh, K.H.; Medina, A.; Sievert, H.; Seth, A.; et al. Coronary sinus reducer stent for the treatment of chronic refractory angina pectoris: a prospective, open-label, multicenter, safety feasibility first-in-man study. J Am Coll Cardiol. 2007, 49, 1783–1789. [Google Scholar] [CrossRef] [PubMed]
- Verheye, S.; Jolicoeur, E.M.; Behan, M.W.; Pettersson, T.; Sainsbury, P.; Hill, J.; et al. Efficacy of a device to narrow the coronary sinus in refractory angina. N Engl J Med. 2015, 372, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Cortese, B.; Di Palma, G.; Latini, R. Coronary sinus perforation during reducer implantation. Catheter Cardiovasc Interv. 2018, 00, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Baldetti, L.; Colombo, A.; Banai, S.; Latib, A.; Esposito, A.; Palmisano, A.; et al. Coronary sinus Reducer non-responders: insights and perspectives. EuroIntervention. 2018, 13, 1667–1669. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.