Abstract
An anomalous coronary artery from the opposite sinus of Valsalva (ACAOS) is a rare inherited cardiac condition with a prevalence of around 1% in the general population. ACAOS is associated with sudden cardiac death in young athletes and therefore its exclusion by means of cardiac imaging is crucial in young symptomatic individuals. With the increasing use of noninvasive imaging modalities to exclude coronary artery disease (CAD) in the middle-aged and older population, physicians are faced with an increased absolute number of patients with the incidental finding of ACAOS. However, it seems that in the middle-aged population the intrinsic risk of ACAOS moves into the background compared with the gradually increasing risk associated with CAD. The assessment of high-risk anatomical features, such as slit-like ostium, acute take-off angle, interarterial course, intramural course with elliptical vessel shape and proximal narrowing of the anomalous vessel is a cornerstone in the evaluation of patients with ACAOS. Further, downstream testing in order to evaluate haemodynamic relevance by means of perfusion imaging of anatomic high-risk features in ACAOS is critical. Perfusion can be tested with single-photon emission computed tomography (SPECT) or positron-emission tomography (PET), allowing fusion with coronary computed tomography angiography and enabling differentiation of perfusion defects from an anomalous coronary artery and from possible concomitant CAD. As to date no randomised prospective trials are available, the therapeutic approach to sports restriction and/or surgery is mainly based on experts’ opinions and recommendations with a low level of evidence, and is usually chosen on an individual case-by-case basis. A presumed prognostic benefit from surgical repair and sports restriction should be carefully balanced against the risk of surgery and possible impairment to quality of life, and patient management should be chosen only after considering symptoms, age, sports behaviour, and imaging information.
Background
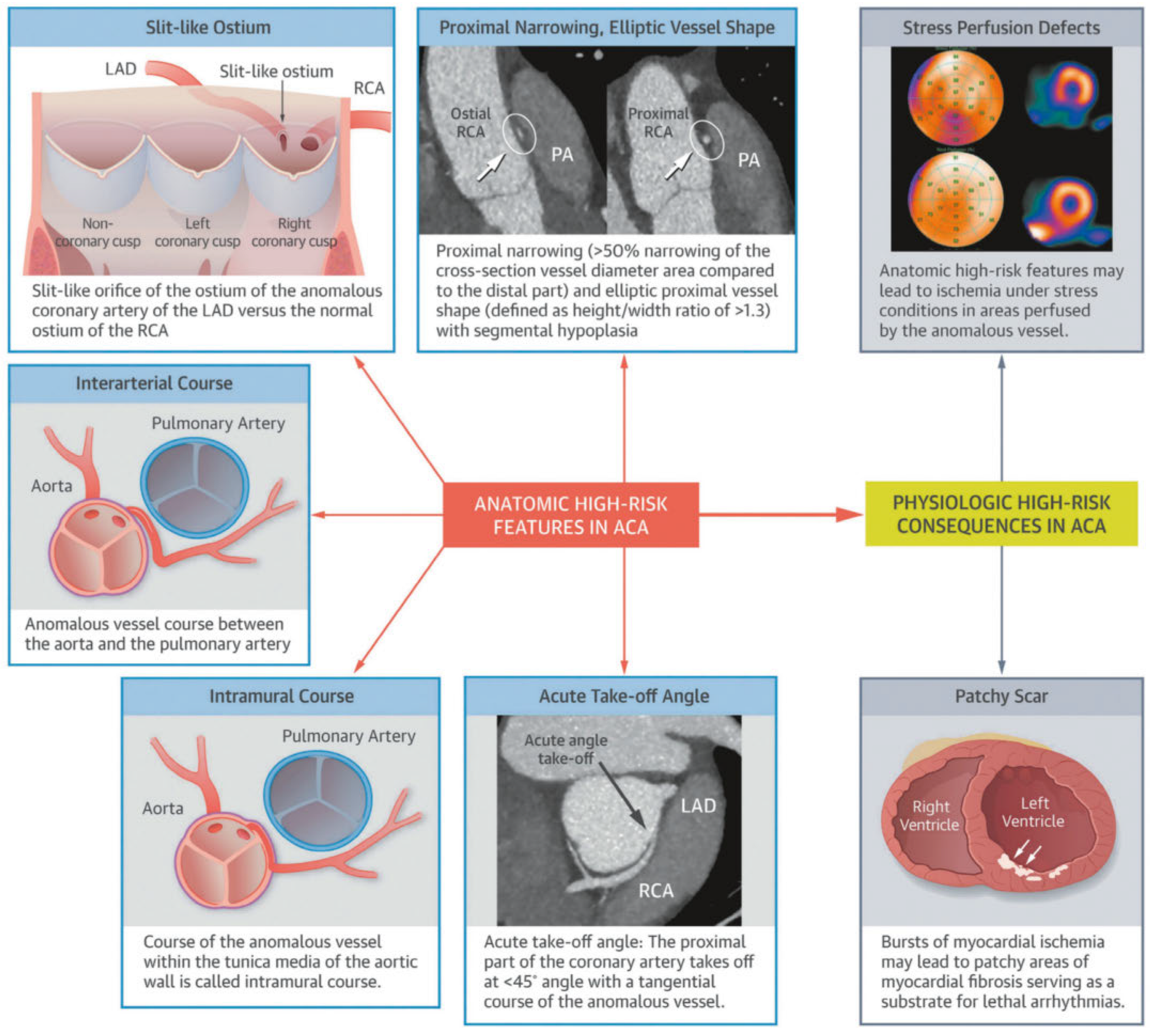
Coronary artery anomalies are a rare inborn disease featuring an anomalous origin, course and/or termination of the native coronary vessel [1]. Important and most common coronary artery anomalies are an anomalous origin from the opposite sinus of Valsalva (ACAOS, Figure 1) [2,3,4]. The course of an ACAOS may be ventral, retroaortic or interarterial (the anomalous coronary artery running between the aorta and the pulmonary artery, Figure 2) [2]. The latter is a so-called “malignant” variant and is associated with sudden cardiac death (SCD) in young athletes [5], whereas the remaining variants are considered “benign”. Other variants of coronary artery anomalies are coronary fistula, with an abnormal termination of the coronary artery. Bland-White-Garland Syndrome is an anomaly with the origin of a coronary artery from the pulmonary artery, which may result in a “steal-phenomenon” caused by reversed flow from the coronary artery into a pulmonary artery due to the decreased pulmonary artery pressure aher birth. Another form, myocardial bridging, is considered a normal variant as it appears in up to 43% of cases in coronary computed tomography angiography (CCTA) studies [6]. Beside the “malignant” variant of ACAOS with an interarterial course of the anomalous coronary artery, other anatomical high-risk features are a slit-like ostium, acute take-off angle, intramural course (the proximal part of the anomalous vessel passing within the tunica media of the aortic wall) with elliptical vessel shape and proximal narrowing of the anomalous vessel (Figure 3) [1,7]. These anatomical features are considered high risk as it is hypothesised that during exercise aortic expansion may lead to valve-like obstruction of the slit-like ostium, and coronary flow might further be impaired by angulation of the acute take-off of the anomalous vessel.
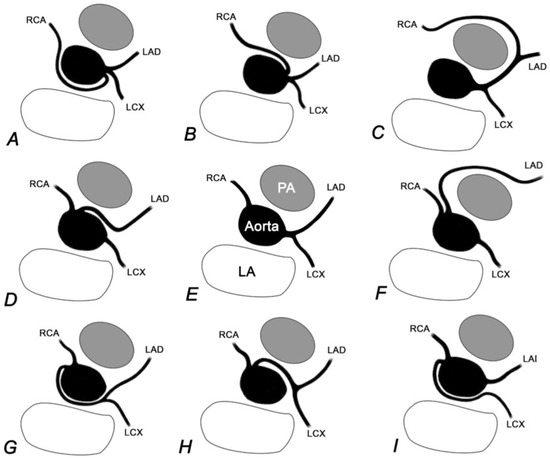
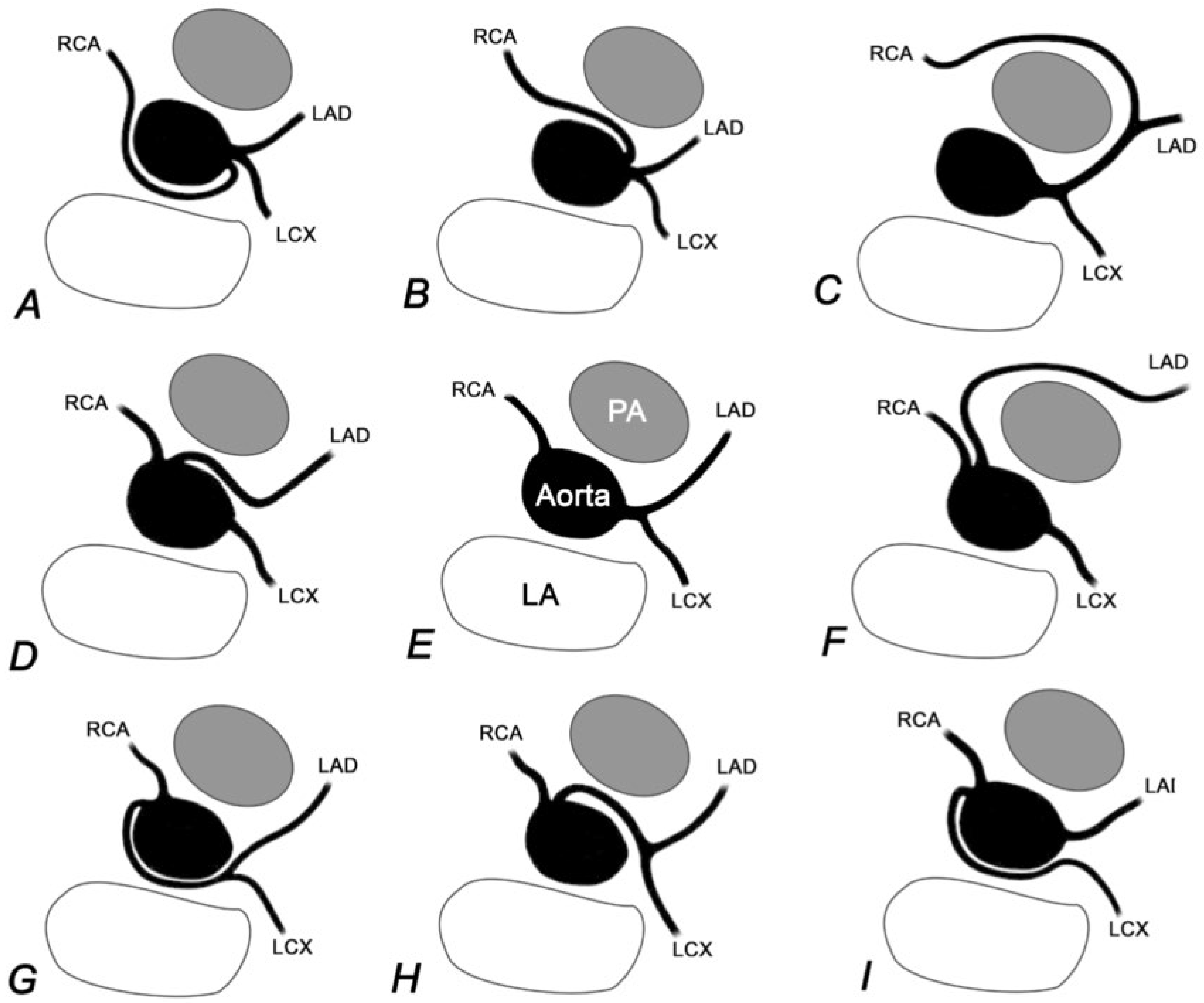
Figure 1.
Schematic illustration of a selection of coronary artery anomalies. For comparison, the normal anatomy is given in the middle (i.e., Panel E). A: ACAOS with RCA originating from the LCS with a retroaortic course. B: ACAOS with RCA originating from the LCS with an interarterial course. C: “Single left” coronary artery with a RCA originating from the LAD and a pre-pulmonary course. D: ACAOS with LAD originating from the RCS with an interarterial course. F: ACAOS with LAD originating from the RCS with a prepulmonary course. G: ACAOS with LM originating from the RCS with a retroaortic course. H: ACAOS with LM originating from the RCS with an interarterial course. I: ACAOS with LCX originating from the RCS with a retroaortic course. LAD = left anterior descending artery; LCS = left coronary sinus; LCX = left circumflex coronary artery; LM = left main stem; RCA = right coronary artery; RCS = right coronary sinus. Reproduced with permission of EMH Swiss Medical Publishers Ltd. from Ref. [2].
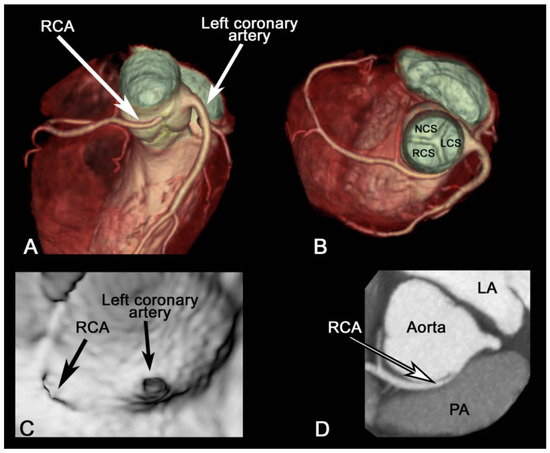
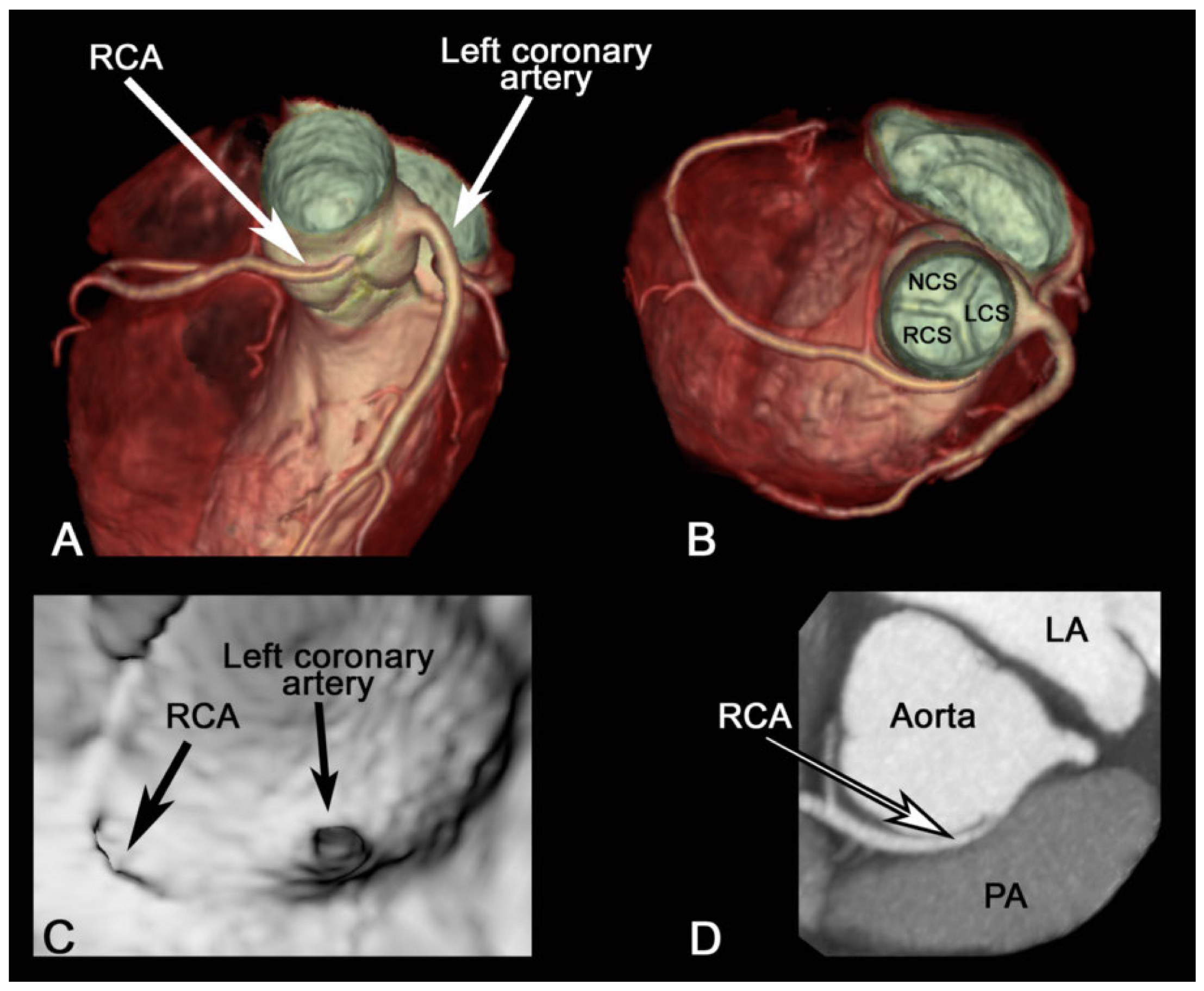
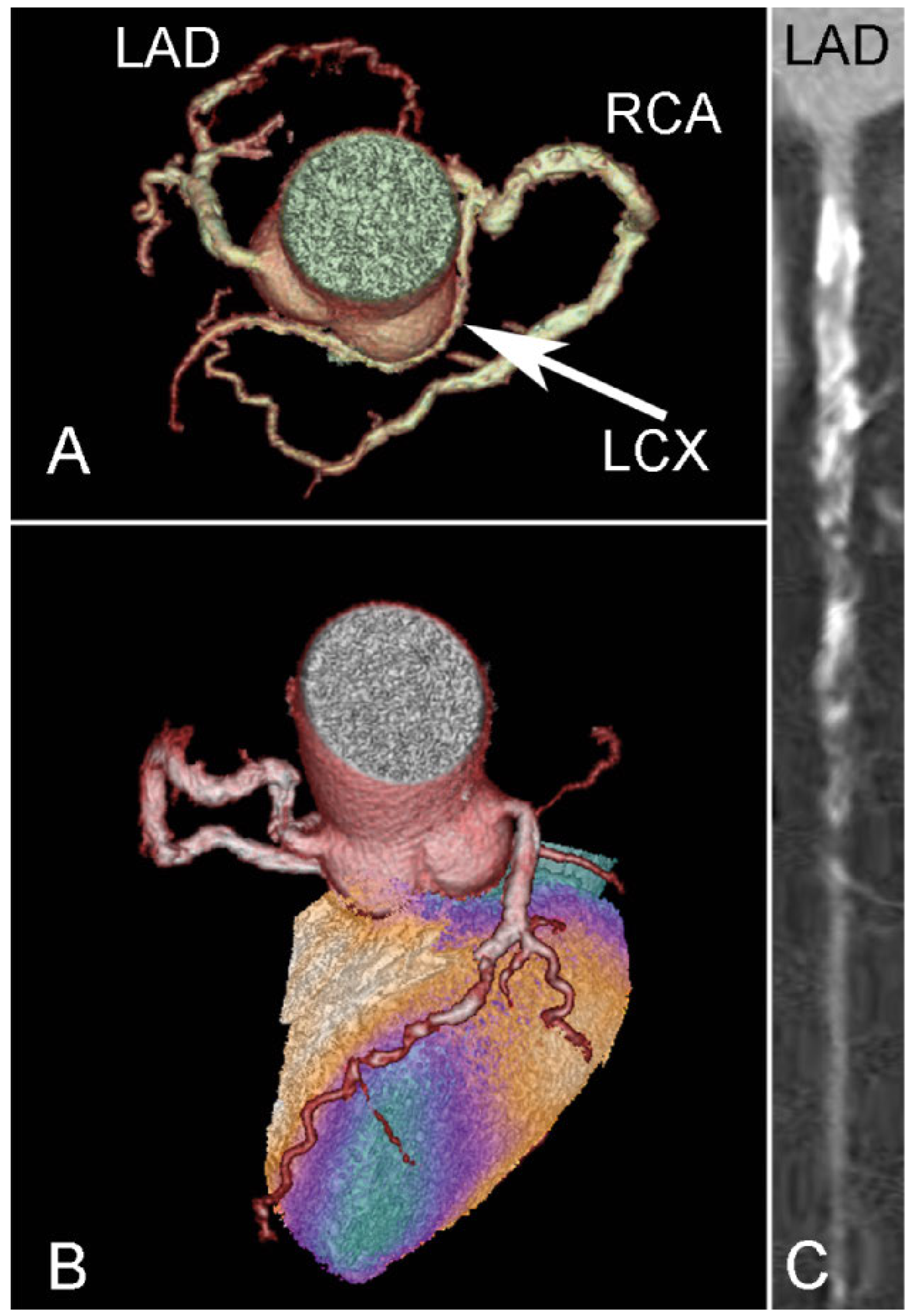
Figure 2.
Volume renderings (A and B) depict an ACAOS and virtual angiography demonstrates origin of the RCA from the LCS. (C). Double-oblique multiplanar image re-formation clearly depicts an IAC of the RCA between the aorta and the PA (D). RCA = right coronary artery; LCS = left coronary sinus, RCS = right coronary sinus; NCS = non-coronary sinus; LA = left atrium; PA = pulmonary artery; IAC = interarterial course. Adapted with permission of the Oxford University Press from Ref. [14].
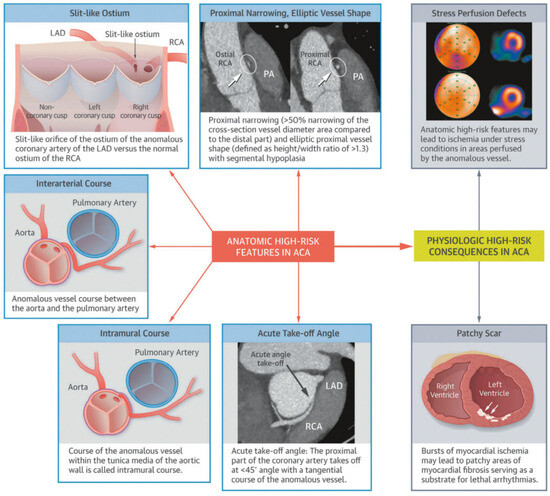
Figure 3.
Anatomical high-risk features and physiological high-risk consequences of ACA (anomalous coronary arteries, this abbreviation has the same meaning as ACAOS) are depicted. Various anatomical high-risk features, such as interarterial course, slit-like ostium, acute take-off angle, intramural course, elliptic vessel shape, and proximal vessel narrowing of the anomalous vessels of patients with ACA/ACAOS are shown. Possible underlying mechanisms in patients with anatomical high-risk features may lead to physiological high-risk consequences, such as a myocardial perfusion defect and myocardial scar. LAD = left anterior descending artery; PA = pulmonary artery; RCA = right coronary artery. Adapted with permission of Elsevier from Ref. [7].
Moreover, the associated aortic dilation during exercise may lead to lateral compression of the proximal and narrowed intramural, elliptical vessel segments. Strenuous sports activity, which results in an increased heart rate and shortened diastolic filling time further contributes to the decreased perfusion of the anomalous coronary artery [7].
In a large registry of the Cleveland Clinic foundation where invasive coronary angiography data from 126 595 patients were analysed, the prevalence of anomalous coronary artery was 1.3%, [8]. In a recent study from our centre, we analysed 5634 consecutive CCTAs between March 2007 and July 2015, and found 145 pa-=tients with coronary anomalies, which represents a prevalence of 2.6% for all coronary anomalies and a prevalence of 1.2% for ACAOS (Table 1) [2]. Due to the increased temporal and spatial resolution of newer generation scanners, the three-dimensional visualisation of anomalies with CCTA is superior to that with other modalities such as echocardiography or invasive coronary angiography (Table 2) and it seems that the prevalence also depends on the imaging modality [6,7]. With the increasing use of noninvasive imaging modalities, a rise in absolute numbers of patients with detected anomalies is expected. Therefore, knowledge about downstream testing options and treatment counselling is gaining importance for family practitioners, cardiologists, heart surgeons and sports medicine physicians alike.

Table 1.
Classification and prevalence of coronary artery anomalies in 5634 consecutive patients undergoing CCTA.

Table 2.
Different imaging modalities in evaluating anomalous coronary arteries.
Anomalous coronary arteries and the risk of adverse cardiac events
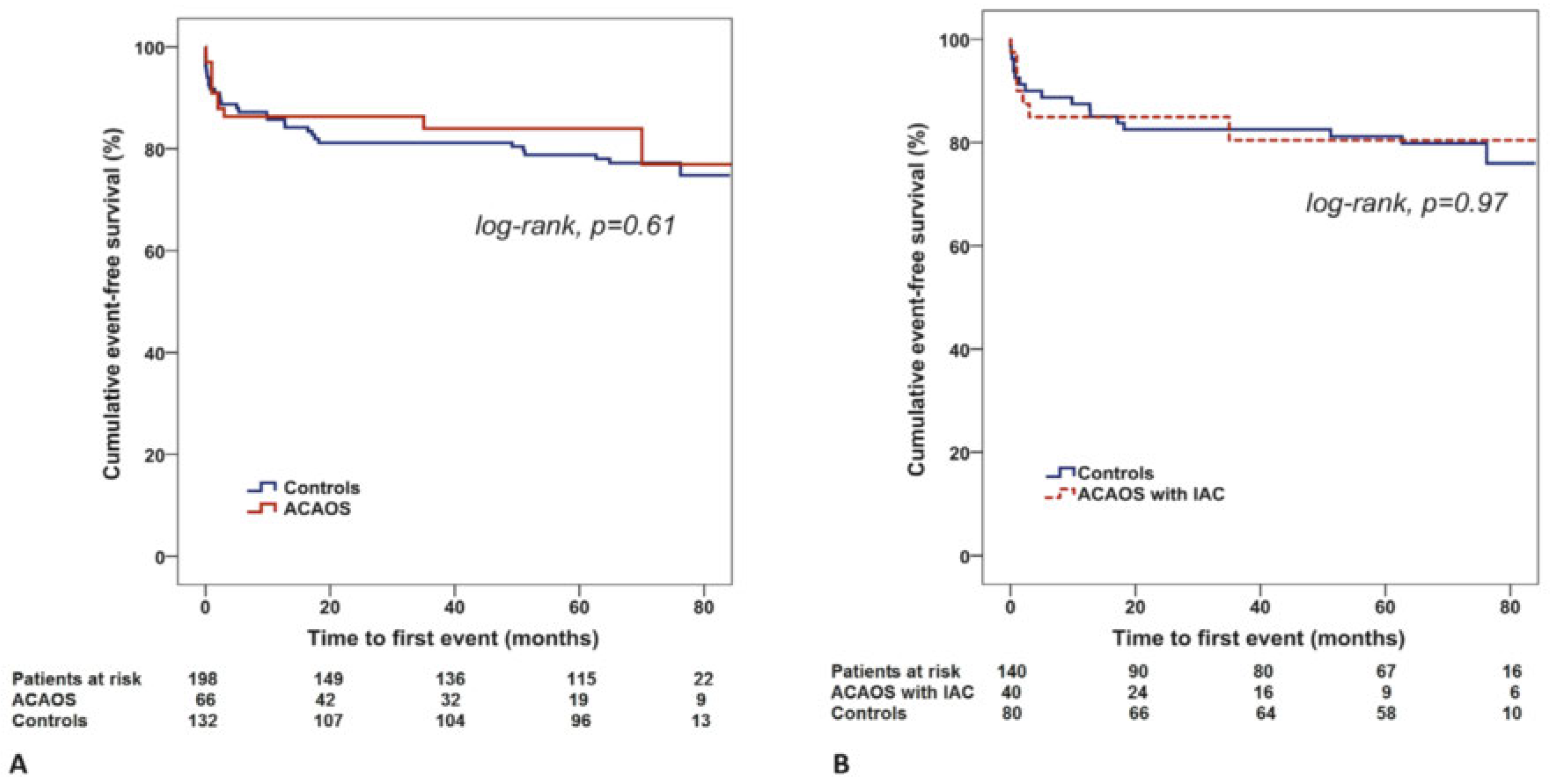
Autopsy series showed that, aher hypertrophic cardiomyopathy, ACAOS is the second most common cause of sports-related SCD in young athletes during or shortly aher strenuous exercise [5,9]. In 80% of the cases where athletes died of an ACAOS, the course of the anomalous vessel was interarterial [10]. In another series of 6.3 million young US military recruits, who underwent an intensive 8-week boot camp, 64 sudden deaths were considered to be of cardiac origin. One third of the SCD cases showed an ACAOS, in all of which the leh coronary artery arose from the right sinus of Valsalva (leh-ACAOS), with an interarterial course between the pulmonary artery and aorta [11]. Others also have reported adverse cardiac events associated with right coronary arteries originating from the leh coronary sinus (right-ACAOS) [12]. In a Swiss study, where we analysed autopsies of sports-related SCDs in young athletes (<40 years of age), 7% showed an anomalous coronary artery, with a similar prevalence compared with arrhythmogenic right ventricular cardiomyopathy or aortic dissection [13]. The underlying mechanisms by which anomalous coronary arteries lead to adverse cardiac events are not clearly understood. As mentioned above, it is suggested that high-risk anatomical features may all contribute to malperfusion of the myocardium and lead to ischaemia and scarring, especially under strenuous physical exercise conditions (see also Figure 3). As SCD with ACAOS was mainly reported in young athletes, it is unknown whether this holds true for older individuals with newly diagnosed ACAOS, especially in the setting of coronary artery disease (CAD) exclusion. We recently published data of 66 middle-aged patients (mean age 56 ± 11 years) with newly detected ACAOS on CCTA and compared their outcome with a cohort matched for age, gender, history of coronary revascularisation and segment stenosis score (a score quantifying CAD burden). Each patient with ACAOS was matched to two controls without ACAOS and was followed-up for 4 years, and major adverse cardiac events (myocardial infarction, revascularisation and cardiac death) were recorded for all patients and controls. Interestingly, the annual event rate of ACAOS patients compared with controls was not significantly different at 4.9 versus 4.8% and a hazard ratio of 0.94 (95% confidence interval [CI] 0.39–2.28, p = 0.89). In the subgroup with ACAOS with an interarterial course (40 patients, 65%), the annual event rate was also not significantly different from their matched controls, at 5.2 and 4.3%, respectively and a hazard ratio of 1.01 (95% CI 0.39–2.58, p = 0.99) (Figure 4) [14]. Thus, in this middle-aged population with newly diagnosed ACAOS and possible concomitant CAD, mid-term outcome was favourable and not statistically different from the matched control cohort without an anomalous coronary artery, regardless of whether or not ACAOS with an interarterial course were present. Whether older patients with ACAOS are less susceptible to adverse cardiac events, or whether a selection bias towards low-risk patients who survived childhood may have influenced our results remains unclear. Whichever is the case, it may be hypothesised that with ageing the risk for cardiovascular morbidity and mortality due to ACAOS moves into the background compared with the increasing risk of CAD-related events [15] and that surgery of ACAOS might not be mandatory for all these incidental findings. Indeed, when a subgroup of this middle-aged population with ACAOS who underwent hybrid imaging with CCTA and single photon emission computed tomography (SPECT) was analysed, myocardial ischaemia due to ACAOS was exceedingly rare and was more likely attributable to concomitant CAD [15].
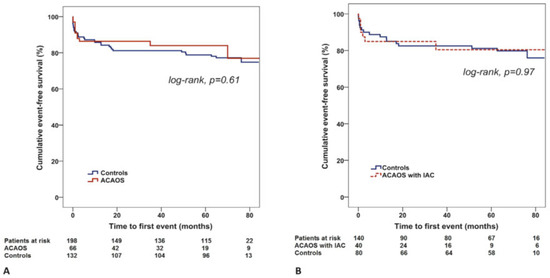
Figure 4.
Kaplan-Meier cumulative event-free survival for patients with ACAOS vs controls (A) and ACAOS and IAC vs Controls. (B). IAC = interarterial course. Adapted with permission of the Oxford University Press from Ref. [14].
Imaging modalities in the assessment of coronary artery anomalies
CCTA has undergone substantial technical advances over the last decade, particularly with regard to spatial resolution and reduction of patients’ exposure to radiation to an average range of 0.21 to 0.5 mSv in daily clinical routine [16]. Therefore in most centres, CCTA has become the first-line imaging modality to assess the anatomy, i.e., the full course, of coronary artery anomalies [2]. Cardiac magnetic resonance imaging (CMR) also offers three-dimensional imaging at high spatial resolution (slightly lower than coronary CCTA), but without radiation exposure, and allows visualisation of the origin and the full course of the ACAOS, including its relationship to the great vessels. Furthermore, CMR offers other additional relevant information including valvular function, ventricular function, regional contractility and myocardial viability, all of which could be important considerations during the pre- or postoperative evaluation [17]. Echocardiography is also a valid alternative for assessing primarily the origin of ACAOS.
If an anomalous coronary artery with a high-risk anatomical feature is detected, downstream imaging for assessment of haemodynamic relevance is indicated. As pharmacological (adenosine) testing would not adequately represent strenuous exercise, maximum physical stress imaging, using SPECT (or also physical stress echocardiography, especially in children) is preferred in patients with ACAOS [15,18,19]. Alternatively, stress testing with dobutamine – which mimics physical exercise better than adenosine [20] – with use of other imaging modalities can also be considered where, for technical and procedural reasons, adequate maximum intensity exercise stress testing is not possible (e.g., stress-CMR, positron emission tomography [PET]). However, there is no evidence comparing the different imaging modalities in this particular clinical setting. Beside the advantage of the feasibility of physical stress imaging, SPECT also allows fusion of the functional imaging with the anatomical information from CCTA (Figure 5) [15,21]. In more than half of patients with no coronary anomalies, the so-called standard distribution of myocardial perfusion territories does not correspond with individual anatomy [22], and it is even more challenging in patients with ACAOS to correctly assign territories to the subtending coronary arteries. Therefore, hybrid CCTA/SPECT and hybrid CCTA/PET represents a valuable noninvasive tool for discriminating the impact of ACAOS from that of concomitant CAD on myocardial ischaemia and correctly allocating ischaemia to the subtended anomalous or nonanomalous vessel.
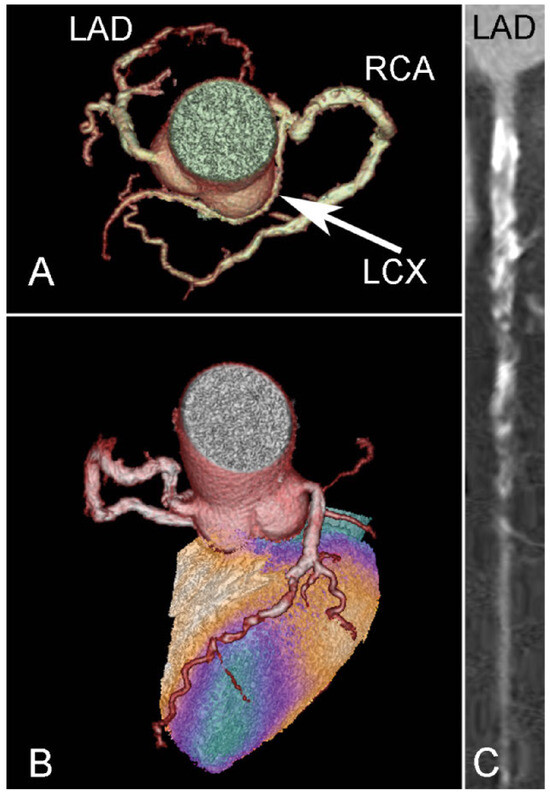
Figure 5.
CCTA shows a patient with a benign ACAOS variant and a retroaortic course of the LCX (A). Hybrid CCTA/SPECT (using the CT attenuation-corrected stress dataset) reveals an anteroapical ischaemia matching the perfusion area of the LAD (B). CCTA demonstrates severe coronary atherosclerosis with subtotal stenosis of the middle LAD (C). LAD = left anterior descending artery; LCX = left cirumflex artery; RCA = right coronary artery. Reproduced with permission of Springer from Ref. [15].
Incorporating current knowledge of the literature of ACAOS, we propose the following imaging evaluation steps, treatment options and sport restriction recommendations (Figure 6) [7]. In “benign” ACAOS with absent high-risk anatomical features, no downstream testing, treatment and follow-up is generally needed. In “malignant” ACAOS with high-risk anatomical features, further imaging evaluation is needed in order to rule out ischaemia. Whether no finding of ischaemia fully reassures the physician and prognosticates absence of ACAOS-related future adverse cardiac events, remains unclear to date.
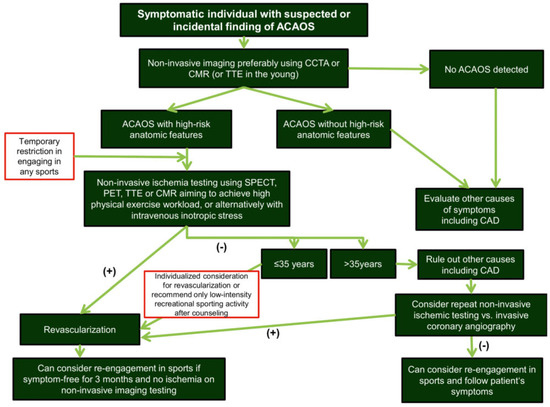
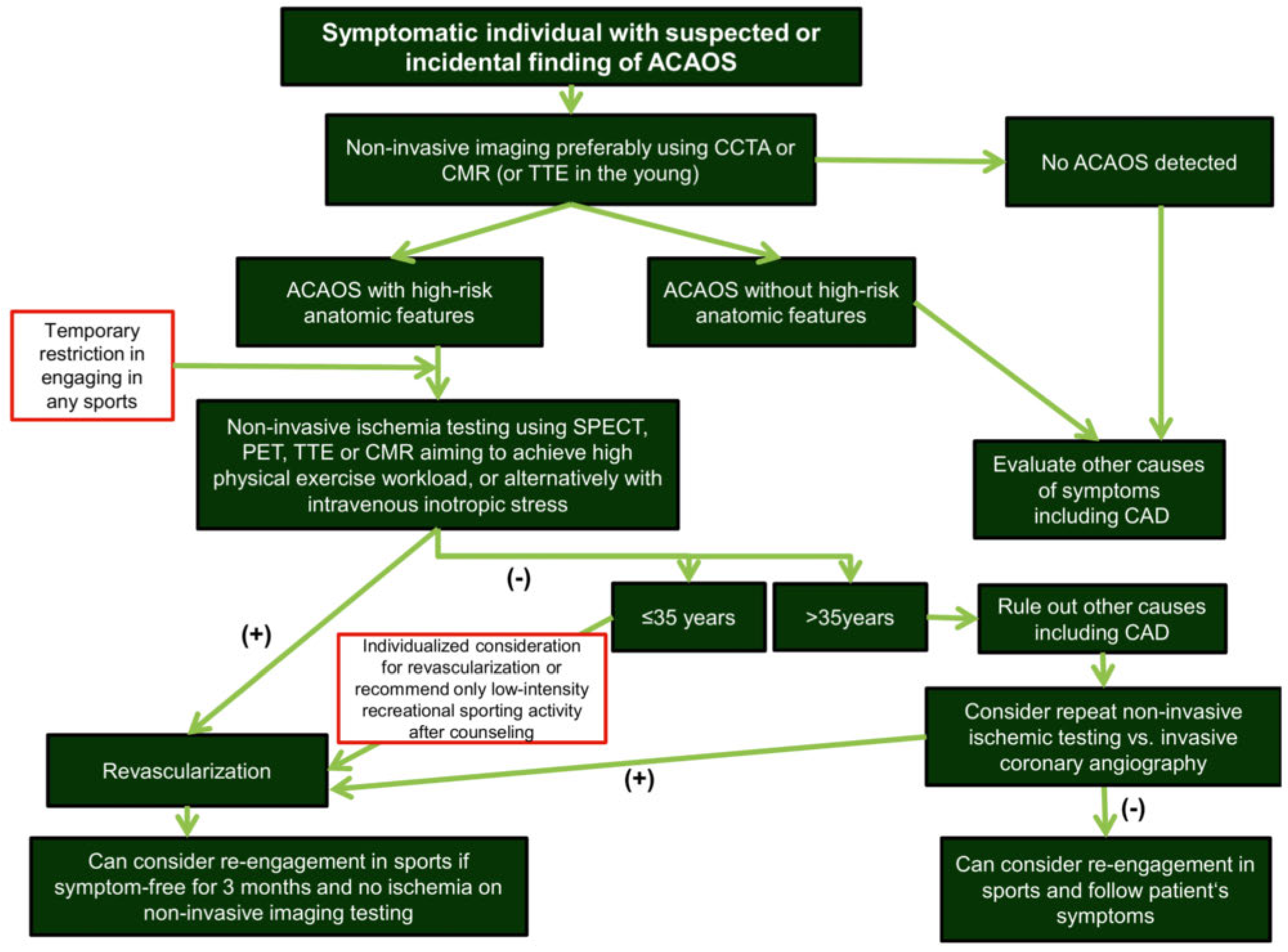
Figure 6.
Flow chart for evaluation of symptomatic individuals with suspected or incidental finding of ACAOS. Initial steps are CCTA (or alternatively CMR or echocardiography) for evaluation of cases with high-risk anatomical features, followed by noninvasive ischaemia testing, preferably with use of maximum physical exercise to mimic real life conditions. Alternatively, dobutamine stress testing can be used to achieve high heart rates and imitate physical exercise. Beside SPECT, PET and CMR, stress-echocardiography might also play a role, especially in children to assess hemodynamic relevance [18,25]. TTE = transthoracic echocardiography. Adapted with permission of Elsevier from Ref. [7].
Therapeutic options in individuals with coronary artery anomalies
Although there are no long-term follow-up data showing a benefit of surgery over conservative treatment, it is generally recommended that, especially young patients with leh-ACAOS and an interarterial course or documented ischaemia, should undergo surgery [23]. These patients also should be restricted from any competitive sports before surgery, based on the recent American Heart Association / American College of Cardiology Task Force 4 recommendations [24]. As an exception, participation in low static or low dynamic (class IA sports, such as bowling, cricket, curling, golf, rifle shooting and yoga) is allowed. This applies to patients with symptomatic or asymptomatic ACAOS diagnosed in either intentional or incidental conditions. This recommendation applies also to patients with right-ACAOS and either symptoms or a positive exercise stress test. In athletes with uncorrected right-ACAOS who exhibit symptoms, arrhythmias, or signs of ischaemia on exercise stress testing, participation in all competitive sports, except for class IA sports, is also not recommended before a surgical repair. For patients with right-ACAOS but no symptoms or ischaemia on an adequately performed exercise stress test, participation in competitive sports can be considered aher adequate counselling of the athlete or the athlete’s parents [24].
The operative correction technique most used is socalled unroofing, where the intramural segment in the aorta is opened and a neo-ostium is created. Alternatively, re-implantation of the aberrant coronary artery or bypass surgery can be performed. However, this last technique is usually less effective as the bypass grah is prone to closure because of competing flow in the native vessel [7].
In other haemodynamically relevant coronary artery anomalies, namely Bland-White-Garland Syndrome, an operation is almost always indicated [23]. The primary aim is to re-implant the aberrant coronary artery in the aortic root or to tunnel aortic blood flow through the pulmonary artery to the ostium of the aberrant coronary artery (Takeuchi operation). Large coronary artery fistulas should be corrected with an operation or interventionally [23]. In smaller fistulas, pre-interventional ischaemia, leh ventricular dysfunction or arrhythmia should be documented [23].
The evidence on which therapeutic recommendations in patients with anomalous coronary arteries is scarce and mainly based on anecdotal reports, case series and experts’ opinions. There are no prospective, randomised multicentre trials. Mostly, the choice of surgery, sports restriction or no treatment is made on a case-by-case discussion. The combination of clinical symptoms, age, sports behaviour and presence or absence of high-risk features / ischaemia, and individualised discussion between the treating physician, patient and heart surgeon leads to the final decision. In order to adapt current recommendations, more evidence, based on multicentre registries and prospective trials with follow-up studies are needed.
The findings of the discussed research in this review were presented at the occasion of the Young Swiss Investigator Session on Friday, June 9, 2017 at the Swiss Society of Cardiology in Baden and were awarded with the Swiss AMGEN Cardiology Award 2017.
Conclusions and key messages
- Increased use of noninvasive imaging results in increasing absolute numbers of patients detected with ACAOS
- In middle-aged individuals with newly diagnosed ACAOS, outcome is not statistically different from that of a matched control cohort without anomalies
- Hybrid CCTA/SPECT discriminates the impact of ACAOS from concomitant CAD on myocardial ischaemia/scarring. Impairment of myocardial perfusion due to ACAOS per se seems to be exceedingly rare and such impairment is much more likely attributable to concomitant CAD.
- In patients with ACAOS, any presumed prognostic benefits from surgical repair and sports restriction should be individually carefully balanced against the risk of a surgery and possible impairment of quality of life
- Decisions about patient management should be made after considering all available information, such as symptoms, age, sports behaviour, and imaging of high-risk anatomical features and possible haemodynamic consequences
- More evidence based on prospective trials and multicentre registries with follow-up studies is imperatively needed to modify current recommendations.
Funding / potential competing interests
No financial support and no other potential conflict of interest relevant to this article was reported.
Abbreviations
| ACAOS: | anomalous origin of the coronary artery from the opposite sinus of Valsalva |
| CAD: | coronary artery disease |
| CCTA: | coronary computed tomography angiography |
| CMR: | cardiac magnetic resonance imaging |
| PET: | positron emission tomography |
| SCD: | sudden cardiac death |
| SPECT: | single photon emission computed tomography |
References
- Angelini, P. Coronary artery anomalies: an entity in search of an identity. Circulation 2007, 115, 1296–1305. [Google Scholar] [CrossRef]
- Gräni, C.; Benz, D.C.; Schmied, C.; Vontobel, J.; Possner, M.; Clerc, O.F.; et al. Prevalence and characteristics of coronary artery anomalies detected by coronary computed tomography angiography in 5634 consecutive patients in a single centre in Switzerland. Swiss Med Wkly 2016, 146, w14294. [Google Scholar] [CrossRef] [PubMed]
- Cheezum, M.K.; Ghoshhajra, B.; Bittencourt, M.S.; Hulten, E.A.; Bhatt, A.; Mousavi, N.; et al. Anomalous origin of the coronary artery arising from the opposite sinus: prevalence and outcomes in patients undergoing coronary CTA. Eur Heart J Cardiovasc Imaging 2017, 18, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.A.; Marler, A.T.; Lin, C.K.; McDonough, R.J.; Prentice, R.L.; Malik, J.A.; et al. A review of anomalous origination of a coronary artery from an opposite sinus of Valsalva (ACAOS) impact on major adverse cardiovascular events based on coronary computerized tomography angiography: a 6-year single center review. Ther Adv Cardiovasc Dis 2014, 8, 237–241. [Google Scholar] [CrossRef]
- Maron, B.J.; Haas, T.S.; Ahluwalia, A.; Murphy, C.J.; Garberich, R.F. Demographics and Epidemiology of Sudden Deaths in Young Competitive Athletes: From the United States National Registry. Am J Med 2016, 129, 1170–1177. [Google Scholar] [CrossRef]
- Ghadri, J.R.; Kazakauskaite, E.; Braunschweig, S.; Burger, I.A.; Frank, M.; Fiechter, M.; et al. Congenital coronary anomalies detected by coronary computed tomography compared to invasive coronary angiography. BMC Cardiovasc Disord 2014, 14, 81. [Google Scholar] [CrossRef]
- Gräni, C.; Buechel, R.R.; Kaufmann, P.A.; Kwong, R.Y. Multimodality Imaging in Individuals With Anomalous Coronary Arteries. JACC Cardiovasc Imaging 2017, 10, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Yamanaka, O.; Hobbs, R.E. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn 1990, 21, 28–40. [Google Scholar] [CrossRef]
- Lorenz, E.C.; Mookadam, F.; Mookadam, M.; Moustafa, S.; Zehr, K.J. A systematic overview of anomalous coronary anatomy and an examination of the association with sudden cardiac death. Rev Cardiovasc Med 2006, 7, 205–213. [Google Scholar]
- Maron, B.J.; Shirani, J.; Poliac, L.C.; Mathenge, R.; Roberts, W.C.; Mueller, F.O. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA 1996, 276, 199–204. [Google Scholar] [CrossRef]
- Eckart, R.E.; Scoville, S.L.; Campbell, C.L.; Shry, E.A.; Stajduhar, K.C.; Potter, R.N.; et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med 2004, 141, 829–834. [Google Scholar] [CrossRef]
- Jo, Y.; Uranaka, Y.; Iwaki, H.; Matsumoto, J.; Koura, T.; Negishi, K. Sudden cardiac arrest: associated with anomalous origin of the right coronary artery from the leh main coronary artery. Tex Heart Inst J 2011, 38, 539–543. [Google Scholar]
- Gräni, C.; Chappex, N.; Fracasso, T.; Vital, C.; Kellerhals, C.; Schmied, C.; et al. Sports-related sudden cardiac death in Switzerland classified by static and dynamic components of exercise. Eur J Prev Cardiol 2016, 23, 1228–1236. [Google Scholar] [CrossRef]
- Gräni, C.; Benz, D.C.; Steffen, D.A.; Clerc, O.F.; Schmied, C.; Possner, M.; et al. Outcome in middle-aged individuals with anomalous origin of the coronary artery from the opposite sinus: a matched cohort study. Eur Heart J. 2017, 38, 2009–2016. [Google Scholar] [CrossRef]
- Gräni, C.; Benz, D.C.; Schmied, C.; Vontobel, J.; Mikulicic, F.; Possner, M.; et al. Hybrid CCTA/SPECT myocardial perfusion imaging findings in patients with anomalous origin of coronary arteries from the opposite sinus and suspected concomitant coronary artery disease. J Nucl Cardiol 2017, 24, 226–234. [Google Scholar] [CrossRef]
- Benz, D.C.; Gräni, C.; Hirt Moch, B.; Mikulicic, F.; Vontobel, J.; Fuchs, T.A.; et al. Minimized Radiation and Contrast Agent Exposure for Coronary Computed Tomography Angiography: First Clinical Experience on a Latest Generation 256-slice Scanner. Acad Radiol 2016, 23, 1008–1014. [Google Scholar] [CrossRef]
- Ripley, D.P.; Saha, A.; Teis, A.; Uddin, A.; Bijsterveld, P.; Kidambi, A.; et al. The distribution and prognosis of anomalous coronary arteries identified by cardiovascular magnetic resonance: 15 year experience from two tertiary centres. J Cardiovasc Magn Reson 2014, 16, 34. [Google Scholar] [CrossRef]
- Kimball, T.R. Pediatric stress echocardiography. Pediatr Cardiol 2002, 23, 347–357. [Google Scholar] [CrossRef] [PubMed]
- De Luca, L.; Bovenzi, F.; Rubini, D.; Niccoli-Asabella, A.; Rubini, G.; De Luca, I. Stress-rest myocardial perfusion SPECT for functional assessment of coronary arteries with anomalous origin or course. J Nucl Med 2004, 45, 532–536. [Google Scholar] [PubMed]
- Nagaoka, H.; Isobe, N.; Kubota, S.; Iizuka, T.; Imai, S.; Suzuki, T.; et al. Comparison of adenosine, dobutamine, and exercise radionuclide ventriculography in the detection of coronary artery disease. Cardiology 1997, 88, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Gräni, C.; Benz, D.C.; Possner, M.; Clerc, O.F.; Mikulicic, F.; Vontobel, J.; et al. Fused cardiac hybrid imaging with coronary computed tomography angiography and positron emission tomography in patients with complex coronary artery anomalies. Congenit Heart Dis 2017, 12, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Javadi, M.S.; Lautamaki, R.; Merrill, J.; Voicu, C.; Epley, W.; McBride, G.; et al. Definition of vascular territories on myocardial perfusion images by integration with true coronary anatomy: a hybrid PET/CT analysis. J Nucl Med 2010, 51, 198–203. [Google Scholar] [PubMed]
- Warnes, C.A.; Williams, R.G.; Bashore, T.M.; Child, J.S.; Connolly, H.M.; Dearani, J.A.; et al. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation 2008, 118, e714–833. [Google Scholar] [PubMed]
- Van Hare, G.F.; Ackerman, M.J.; Evangelista, J.A.; Kovacs, R.J.; Myerburg, R.J.; Shafer, K.M.; et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 4: Congenital Heart Disease: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015, 66, 2372–2384. [Google Scholar] [CrossRef]
- Lameijer, H.; Ter Maaten, J.M.; Steggerda, R.C. Additive value of dobutamine stress echocardiography in patients with an anomalous origin of a coronary artery. Neth Heart J 2015, 23, 139–140. [Google Scholar] [CrossRef]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.