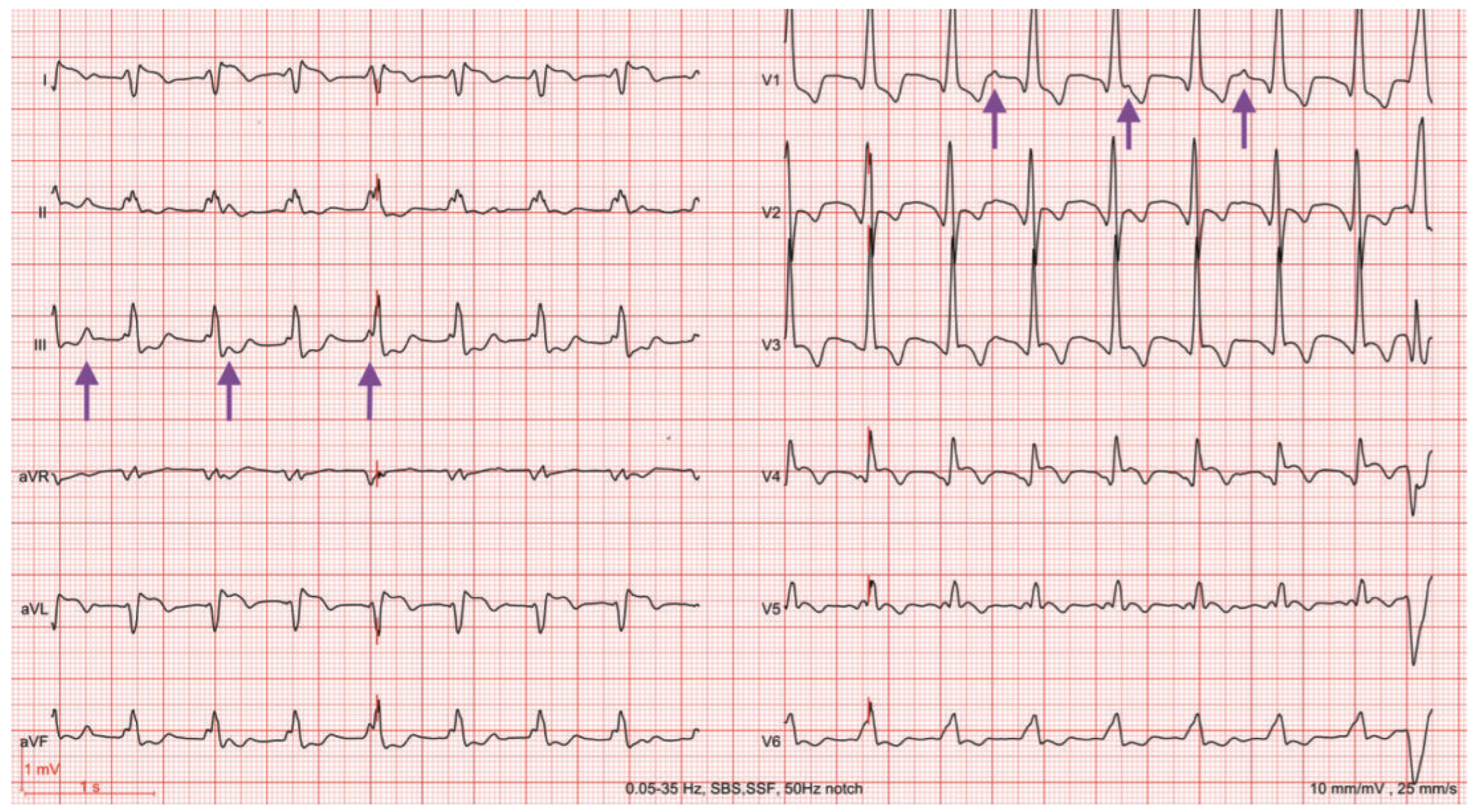
Loss of Biventricular Pacing: What’s the Problem?
Case presentation
Question
Commentary
Conflicts of Interest
References
- Brugada, P.; Brugada, J.; Mont, L.; Smeets, J.; Andries, E.W. A new approach to the di erential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991, 83, 1649–1659. [Google Scholar] [CrossRef] [PubMed]
- Vereckei, A.; Duray, G.; Szenasi, G.; Altenose, G.T.; Miller, J.M. New algorithm using only lead aVR for di erential diagnosis of wide QRS complex tachycardia. Heart Rhythm 2008, 5, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Kutyifa, V.; Klein, H.U.; Wang, P.J.; McNitt, S.; Polonsky, B.; Zima, E.; Merkely, B.; Moss, A.J.; Zareba, W. Clinical significance of ventricular tachyarrhythmias in patients treated with CRT-D. Heart Rhythm. 2013, 10, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Bänsch, D.; Castrucci, M.; Böcker, D.; Breithardt, G.; Block, M. Ventricular tachycardias above initially programmed tachycardia detection interval in patients with implantable cardioverter-defibrillators: incidence, prediction and significance. J Am Coll Cardiol 2000, 36, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Israel, C.W.; Burmistrava, T. Optimal tachycardia programming in ICDs: Recommendations in the post-MADIT-RIT era. Herzschrittmacherther Elektrophysiol. 2016, 27, 163–170. [Google Scholar] [CrossRef] [PubMed]


© 2017 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Cochard, S.; Schläpfer, J. Loss of Biventricular Pacing: What’s the Problem? Cardiovasc. Med. 2017, 20, 74. https://doi.org/10.4414/cvm.2017.00469
Cochard S, Schläpfer J. Loss of Biventricular Pacing: What’s the Problem? Cardiovascular Medicine. 2017; 20(3):74. https://doi.org/10.4414/cvm.2017.00469
Chicago/Turabian StyleCochard, Sylvie, and Jürg Schläpfer. 2017. "Loss of Biventricular Pacing: What’s the Problem?" Cardiovascular Medicine 20, no. 3: 74. https://doi.org/10.4414/cvm.2017.00469
APA StyleCochard, S., & Schläpfer, J. (2017). Loss of Biventricular Pacing: What’s the Problem? Cardiovascular Medicine, 20(3), 74. https://doi.org/10.4414/cvm.2017.00469



