Acute Heart Failure: From Pathophysiology to Optimal Treatment
Abstract
Introduction
Congestion and the pathophysiology of acute heart failure
Diagnosis and initial treatment



Hospital discharge and the vulnerable phase
Key points
- -
- Acute heart failure is a life-threatening condition requiring immediate diagnosis and initiation of treatment.
- -
- Systemic congestion, promoted by the activation of several pathophysiological mechanisms, is the central feature of acute heart failure and causes the typical symptoms and leads to organ dysfunction.
- -
- Cardiogenic shock is the most severe form of acute heart failure and is defined by the presence of reduced cardiac output and end-organ hypoperfusion.
- -
- Decongestive therapy is the mainstay in the initial treatment of acute heart failure with congestion. Inotropes are used in cardiogenic shock patients with reduced myocardial contractility to restore end-organ perfusion.
- -
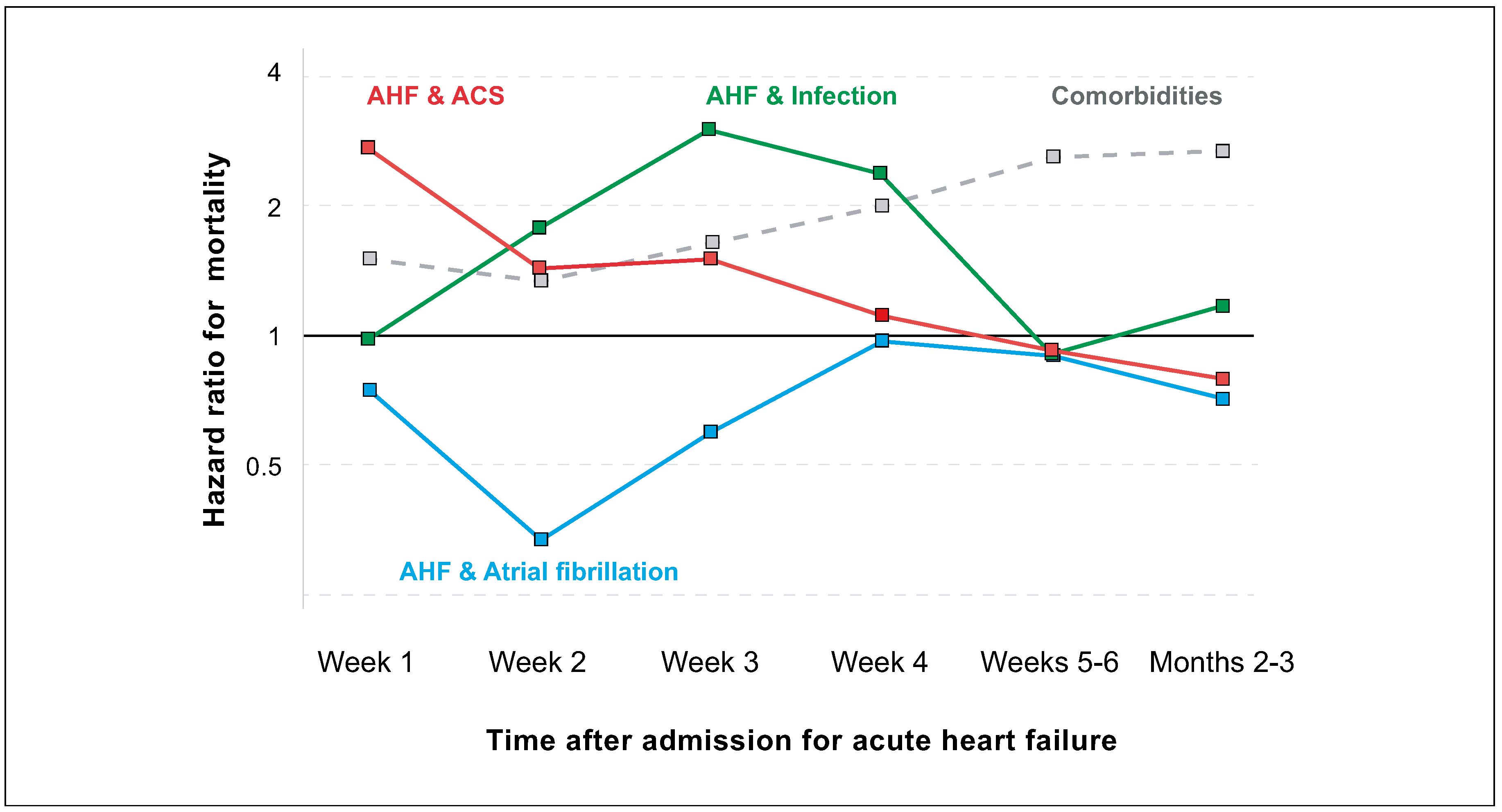
- The first 3 months after an acute heart failure episode—the vulnerable phase—are characterised by high readmission and mortality rates. Optimal patient management before and after hospital discharge is crucial to improve patient outcome.
Disclosure Statement
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; et al. Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016, 37, 2129–200. [Google Scholar] [CrossRef]
- Braunwald, E. Heart failure. JACC Heart Fail 2013, 1, 1–20. [Google Scholar] [CrossRef]
- Rudiger, A.; Harjola, V-P.; Müller, A.; Mattila, E.; Säila, P.; Nieminen, M.; et al. Acute heart failure: clinical presentation, one-year mortality and prognostic factors. Eur J Heart Fail 2005, 7, 662–670. [Google Scholar] [CrossRef]
- Arrigo, M.; Gayat, E.; Parenica, J.; Ishihara, S.; Zhang, J.; Choi, D.J.; et al. GREAT Network. Precipitating factors and 90-day outcome of acute heart failure: a report from the intercontinental GREAT registry. Eur J Heart Fail 2017, 19, 201–208. [Google Scholar] [CrossRef]
- Arrigo, M.; Parissis, J.T.; Akiyama, E.; Mebazaa, A. Understanding acute heart failure: pathophysiology and diagnosis. Eur Heart J Suppl 2016, 18 (suppl G), G11–G18. [Google Scholar] [CrossRef]
- McKie, P.M.; Schirger, J.A.; Costello-Boerrigter, L.C.; Benike, S.L.; Harstad, L.K.; Bailey, K.R.; et al. Impaired natriuretic and renal endocrine response to acute volume expansion in pre-clinical systolic and diastolic dysfunction. J Am Coll Cardiol 2011, 58, 2095–2103. [Google Scholar] [CrossRef]
- Zile, M.R.; Bennett, T.D.; St John Sutton, M.; Cho, Y.K.; Adamson, P.B.; Aaron, M.F.; et al. Transition from chronic compensated to acute decompensated heart failure: pathophysiological insights obtained from continuous monitoring of intracardiac pressures. Circulation 2008, 118, 1433–1441. [Google Scholar] [CrossRef]
- Nijst, P.; Verbrugge, F.H.; Grieten, L.; Dupont, M.; Steels, P.; Tang, W.H.; et al. The pathophysiological role of interstitial sodium in heart failure. J Am Coll Cardiol 2015, 65, 378–388. [Google Scholar] [CrossRef]
- Cotter, G.; Metra, M.; Milo-Cotter, O.; Dittrich, H.C.; Gheorghiade, M. Fluid overload in acute heart failure - re-distribution and other mechanisms beyond fluid accumulation. Eur J Heart Fail 2008, 10, 165–169. [Google Scholar] [CrossRef]
- Gandhi, S.K.; Powers, J.C.; Nomeir, A.M.; Fowle, K.; Kitzman, D.W.; Rankin, K.M.; et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 2001, 344, 17–22. [Google Scholar] [CrossRef]
- Viau, D.M.; Sala-Mercado, J.A.; Spranger, M.D.; O’Leary, D.S.; Levy, P.D. The pathophysiology of hypertensive acute heart failure. Heart 2015, 101, 1861–1867. [Google Scholar] [CrossRef]
- Colombo, P.C.; Onat, D.; Harxhi, A.; Demmer, R.T.; Hayashi, Y.; Jelic, S.; et al. Peripheral venous congestion causes inflammation, neurohormonal, and endothelial cell activation. Eur Heart J 2014, 35, 448–454. [Google Scholar] [CrossRef]
- Harjola, V.-P.; Mullens, W.; Banaszewski, M.; Bauersachs, J.; Brunner-La Rocca, H.P.; Chioncel, O.; et al. Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 2017, 19, 821–836. [Google Scholar] [CrossRef]
- Mullens, W.; Abrahams, Z.; Francis, G.S.; Sokos, G.; Taylor, D.O.; Starling, R.C.; et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol 2009, 53, 589–596. [Google Scholar] [CrossRef]
- Poelzl, G.; Ess, M.; Mussner-Seeber, C.; Pachinger, O.; Frick, M.; Ulmer, H. Liver dysfunction in chronic heart failure: prevalence, characteristics and prognostic significance. Eur J Clin Invest 2012, 42, 153–163. [Google Scholar] [CrossRef]
- Ishihara, S.; Gayat, E.; Sato, N.; Arrigo, M.; Laribi, S.; Legrand, M.; et al. Similar hemodynamic decongestion with vasodilators and inotropes: systematic review, meta-analysis, and meta-regression of 35 studies on acute heart failure. Clin Res Cardiol 2016, 105, 971–980. [Google Scholar] [CrossRef]
- Mebazaa, A.; Yilmaz, M.B.; Levy, P.; Ponikowski, P.; Peacock, W.F.; Laribi, S.; et al. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur J Heart Fail 2015, 17, 544–558. [Google Scholar] [CrossRef]
- Forrester, J.S.; Diamond, G.; Chatterjee, K.; Swan, H.J. Medical therapy of acute myocardial infarction by application of hemodynamic subsets (first of two parts). N Engl J Med 1976, 295, 1356–1362. [Google Scholar] [CrossRef]
- Forrester, J.S.; Diamond, G.A.; Swan, H.J. Correlative classification of clinical and hemodynamic function after acute myocardial infarction. Am J Cardiol 1977, 39, 137–145. [Google Scholar] [CrossRef]
- Harjola, V.-P.; Lassus, J.; Sionis, A.; Køber, L.; Tarvasmäki, T.; Spinar, J.; et al. CardShock Study Investigators; GREAT network. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail 2015, 17, 501–509. [Google Scholar] [CrossRef]
- Rudiger, A.; Gasser, S.; Fischler, M.; Hornemann, T.; von Eckardstein, A.; Maggiorini, M. Comparable increase of B-type natriuretic peptide and amino-terminal pro-B-type natriuretic peptide levels in patients with severe sepsis, septic shock, and acute heart failure. Crit Care Med 2006, 34, 2140–2144. [Google Scholar] [CrossRef]
- Mebazaa, A.; Tolppanen, H.; Mueller, C.; Lassus, J.; DiSomma, S.; Baksyte, G.; et al. Acute heart failure and cardiogenic shock: a multidisciplinary practical guidance. Intensive Care Med 2016, 42, 147–163. [Google Scholar] [CrossRef]
- Cotter, G.; Metzkor, E.; Kaluski, E.; Faigenberg, Z.; Miller, R.; Simovitz, A.; et al. Randomised trial of high-dose isosorbide dinitrate plus low-dose furosemide versus high-dose furosemide plus low-dose isosorbide dinitrate in severe pulmonary oedema. Lancet 1998, 351, 389–393. [Google Scholar] [CrossRef]
- Matsue, Y.; Damman, K.; Voors, A.A.; Kagiyama, N.; Yamaguchi, T.; Kuroda, S.; et al. Time-to-Furosemide Treatment and Mortality in Patients Hospitalized With Acute Heart Failure. J Am Coll Cardiol 2017, 69, 3042–3051. [Google Scholar] [CrossRef]
- Mebazaa, A.; Parissis, J.; Porcher, R.; Gayat, E.; Nikolaou, M.; Boas, F.V.; et al. Short-term survival by treatment among patients hospitalized with acute heart failure: the global ALARM-HF registry using propensity scoring methods. Intensive Care Med 2011, 37, 290–301. [Google Scholar] [CrossRef]
- Wilhelm, M.J. Extracorporeal membrane oxygenation for acute cardiogenic shock. Cardiovasc Med 2016, 19, 39–43. [Google Scholar] [CrossRef]
- Arrigo, M.; Tolppanen, H.; Sadoune, M.; Feliot, E.; Teixeira, A.; Laribi, S.; et al. GREAT Network. Effect of precipitating factors of acute heart failure on readmission and long-term mortality. ESC Heart Fail 2016, 3, 115–121. [Google Scholar] [CrossRef]
- Rudiger, A.; Streit, M.; Businger, F.; Schmid, E.R.; Follath, F.; Maggiorini, M. The impact of infections on critically ill acute heart failure patients: an observational study. Swiss Med Wkly 2010, 140, w13125. [Google Scholar]
- Greene, S.J.; Fonarow, G.C.; Vaduganathan, M.; Khan, S.S.; Butler, J.; Gheorghiade, M. The vulnerable phase after hospitalization for heart failure. Nat Rev Cardiol 2015, 12, 220–229. [Google Scholar] [CrossRef]
- Ambrosy, A.P.; Fonarow, G.C.; Butler, J.; Chioncel, O.; Greene, S.J.; Vaduganathan, M.; et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 2014, 63, 1123–1133. [Google Scholar] [CrossRef]
- Ambrosy, A.P.; Pang, P.S.; Khan, S.; Konstam, M.A.; Fonarow, G.C.; Traver, B.; et al. EVEREST Trial Investigators. Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. Eur Heart J 2013, 34, 835–843. [Google Scholar] [CrossRef]
- Logeart, D.; Thabut, G.; Jourdain, P.; Chavelas, C.; Beyne, P.; Beauvais, F.; et al. Predischarge B-type natriuretic peptide assay for identifying patients at high risk of re-admission after decompensated heart failure. J Am Coll Cardiol 2004, 43, 635–641. [Google Scholar] [CrossRef]
- Arrigo, M.; Truong, Q.A.; Onat, D.; Szymonifka, J.; Gayat, E.; Tolppanen, H.; et al. Soluble CD146 Is a Novel Marker of Systemic Congestion in Heart Failure Patients: An Experimental Mechanistic and Transcardiac Clinical Study. Clin Chem 2017, 63, 386–393. [Google Scholar] [CrossRef]
- Kubena, P.; Arrigo, M.; Parenica, J.; Gayat, E.; Sadoune, M.; Ganovska, E.; et al. GREAT Network. Plasma Levels of Soluble CD146 Reflect the Severity of Pulmonary Congestion Better Than Brain Natriuretic Peptide in Acute Coronary Syndrome. Ann Lab Med 2016, 36, 300–305. [Google Scholar] [CrossRef]
- Prins, K.W.; Neill, J.M.; Tyler, J.O.; Eckman, P.M.; Duval, S. Effects of Beta-Blocker Withdrawal in Acute Decompensated Heart Failure: A Systematic Review and Meta-Analysis. JACC Heart Fail 2015, 3, 647–653. [Google Scholar] [CrossRef]
- Gayat, E.; Arrigo, M.; Littnerova, S.; Sato, N.; Parenica, J.; Ishihara, S.; et al. GREAT Network. Heart failure oral therapies at discharge are associated with better outcome in acute heart failure: a propensity-score matched study. Eur J Heart Fail 2017, 18, 613. [Google Scholar]
- Komajda, M.; Tavazzi, L.; Swedberg, K.; Böhm, M.; Borer, J.S.; Moyne, A.; et al. SHIFT Investigators. Chronic exposure to ivabradine reduces readmissions in the vulnerable phase after hospitalization for worsening systolic heart failure: a post-hoc analysis of SHIFT. Eur J Heart Fail 2016, 18, 1182–1189. [Google Scholar] [CrossRef]
- Hindricks, G.; Taborsky, M.; Glikson, M.; Heinrich, U.; Schumacher, B.; Katz, A.; et al. IN-TIME study group*. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet 2014, 384, 583–590. [Google Scholar] [CrossRef]
- Abraham, W.T.; Adamson, P.B.; Bourge, R.C.; Aaron, M.F.; Costanzo, M.R.; Stevenson, L.W.; et al. CHAMPION Trial Study Group. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet 2011, 377, 658–666. [Google Scholar] [CrossRef]
 |
 |
© 2017 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Arrigo, M.; Rudiger, A. Acute Heart Failure: From Pathophysiology to Optimal Treatment. Cardiovasc. Med. 2017, 20, 229. https://doi.org/10.4414/cvm.2017.00520
Arrigo M, Rudiger A. Acute Heart Failure: From Pathophysiology to Optimal Treatment. Cardiovascular Medicine. 2017; 20(10):229. https://doi.org/10.4414/cvm.2017.00520
Chicago/Turabian StyleArrigo, Mattia, and Alain Rudiger. 2017. "Acute Heart Failure: From Pathophysiology to Optimal Treatment" Cardiovascular Medicine 20, no. 10: 229. https://doi.org/10.4414/cvm.2017.00520
APA StyleArrigo, M., & Rudiger, A. (2017). Acute Heart Failure: From Pathophysiology to Optimal Treatment. Cardiovascular Medicine, 20(10), 229. https://doi.org/10.4414/cvm.2017.00520




