Should We Measure PCSK9 Levels in Patients with Acute Coronary Syndromes?
Abstract
Dyslipidaemia and atherosclerosis
Summary about discovery and clinical importance of PCSK9
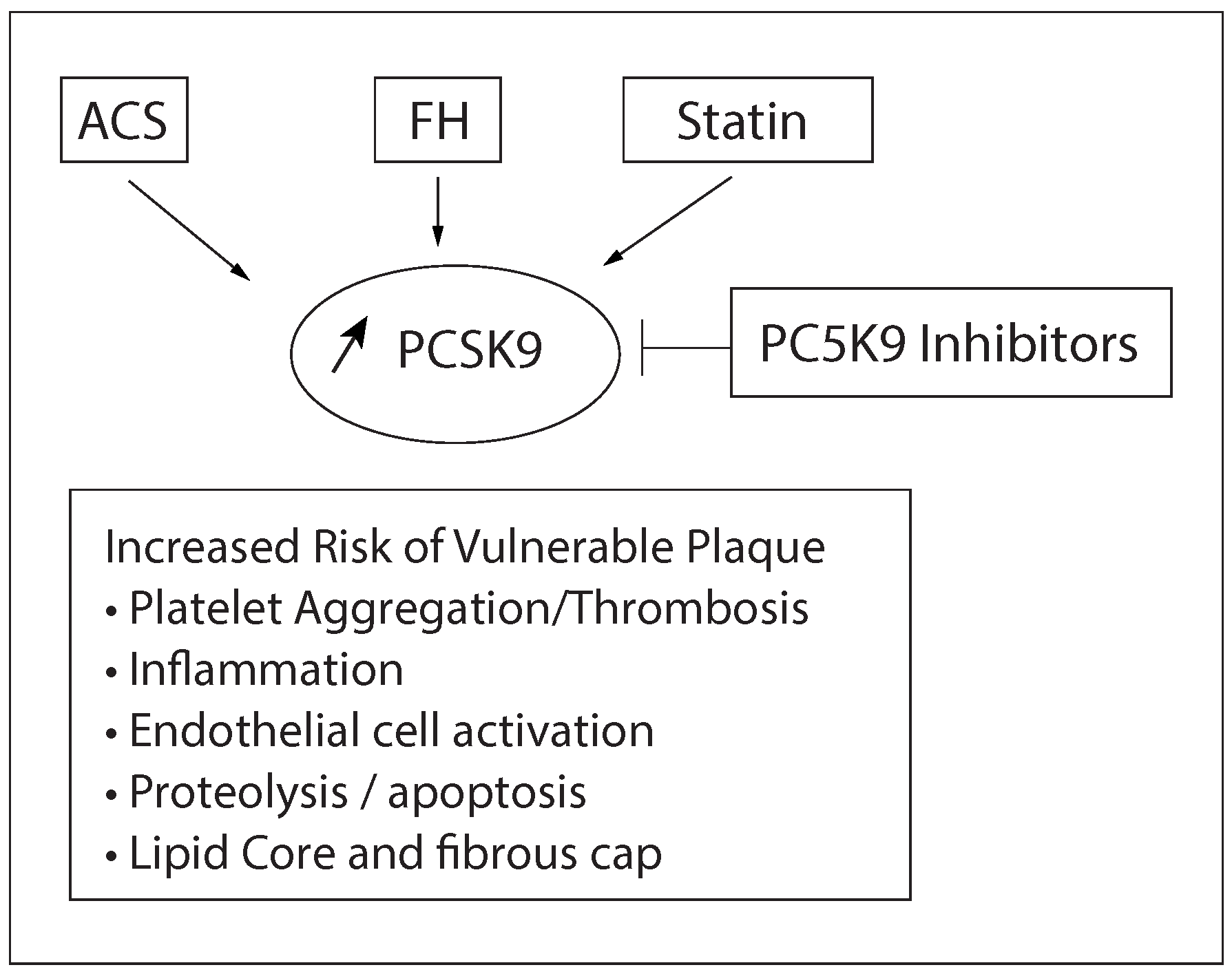
The effect of PCSK9 inhibitors in patients with coronary artery disease and ACS
Why do this research?
What are the most significant findings?
What are the implications for future research and for patient care?
- 1.
- Proof of concept—do novel marker levels differ between subjects with and without outcome?
- 2.
- Prospective validation—does the novel marker predict development of future outcome in a prospective cohort?
| 2015 ESC guidelines on NSTE-ACS [21] |
| In patients with LDL-C ≥70 mg/dl (≥1.8 mmol/l) despite a maximum tolerated statin dose, further reduction in LDL-C with a non-statin agent are recommended (IIa, B). |
| NLA Dyslipidemia Recommendations [39] |
| Until cardiovascular outcome trials with PCSK9 inhibitors are completed, these drugs should be considered primarily in: (1) patients with ASCVD who have LDL-C ≥100 mg/dL while on maximally-tolerated statin (±ezetimibe) (strength B, quality moderate); (2) heterozygous FH patients without ASCVD who have LDL-C ≥130 mg/dL (non-HDL-C ≥160 mg/dL) while on maximally-tolerated statin (±ezetimibe) (strength B, quality moderate). |
| In addition, PCSK9 inhibitor use may be considered for selected high risk patients with ASCVD (e.g., recurrent ASCVD events) who have atherogenic cholesterol levels below the specified values, but above their treatment goals (i.e., LDL-C ≥70 mg/dL [non-HDL-C ≥100 mg/dL]). Strength C, quality low) |
| PCSK9 inhibitor use may be considered in selected high or very high risk patients who meet the definition of statin intoleranceand who require substantial additional atherogenic cholesterol lowering, despite the use of other lipid lowering therapies. (Strength C, quality low) |
- 3.
- Incremental value—does the novel marker add predictive information to established, standard risk markers?
- 4.
- Clinical utility—does the novel risk marker change predicted risk sufficiently to change recommended therapy?
- 5.
- Clinical outcomes—does use of the novel risk marker improve clinical outcomes, especially when tested in a randomised clinical trial?
- 6.
- Cost-effectiveness—does use of the marker improve clinical outcomes sufficiently to justify the additional costs of testing and treatment?
Conclusion
Disclosure Statement
References
- Gencer, B.; Montecucco, F.; Nanchen, D.; et al. Prognostic value of PCSK9 levels in patients with acute coronary syndromes. Eur Heart J. 2016, 37, 546–553. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016. [Google Scholar]
- Gencer, B.; Mach, F. Sweetless’n low LDL-C targets for PCSK9 treatment. Eur Heart J. 2015, 36, 1146–1148. [Google Scholar] [CrossRef][Green Version]
- Gencer, B.; Lambert, G.; Mach, F. PCSK9 inhibitors. Swiss Med Wkly. 2015, 145, w14094. [Google Scholar] [CrossRef] [PubMed]
- Shimada, Y.J.; Cannon, C.P. PCSK9 (Proprotein convertase subtilisin/ kexin type 9) inhibitors: Past, present, and the future. Eur Heart J. 2015, 36, 2415–2424. [Google Scholar] [CrossRef]
- Jackson, R.; Kerr, A.; Wells, S. Vascular risk calculators: Essential but flawed clinical tools? Circulation 2013, 127, 1929–1931. [Google Scholar]
- Navarese, E.P.; Kolodziejczak, M.; Schulze, V.; et al. Effects of Proprotein Convertase Subtilisin/Kexin Type 9 Antibodies in Adults With Hypercholesterolemia: A Systematic Review and Meta-analysis. Ann Intern Med. 2015, 163, 40–51. [Google Scholar]
- Nordestgaard, B.G.; Chapman, M.J.; Humphries, S.E.; et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: Guidance for clinicians to prevent coronary heart disease: Consensus statement of the European Atherosclerosis Society. Eur Heart J. 2013, 34, 3478–3490a. [Google Scholar] [CrossRef]
- Wiegman, A.; Gidding, S.S.; Watts, G.F.; et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur Heart J. 2015, 36, 2425–2437. [Google Scholar] [CrossRef]
- Nanchen, D.; Gencer, B.; Auer, R.; et al. Prevalence and management of familial hypercholesterolaemia in patients with acute coronary syndromes. Eur Heart J. 2015, 36, 2438–2445. [Google Scholar] [CrossRef]
- Gencer, B.; Nanchen, D. Identifying familial hypercholesterolemia in acute coronary syndrome. Curr Opin Lipidol. 2016, 27, 375–381. [Google Scholar] [PubMed]
- Gencer, B.; Auer, R.; Nanchen, D.; et al. Expected impact of applying new 2013 AHA/ACC cholesterol guidelines criteria on the recommended lipid target achievement after acute coronary syndromes. Atherosclerosis 2015, 239, 118–124. [Google Scholar]
- Gaudet, D.; Kereiakes, D.J.; McKenney, J.M.; et al. Effect of alirocumab, a monoclonal proprotein convertase subtilisin/kexin 9 antibody, on lipoprotein(a) concentrations (a pooled analysis of 150 mg every two weeks dosing from phase 2 trials). Am J Cardiol. 2014, 114, 711–715. [Google Scholar] [PubMed]
- Stroes, E.S.; Thompson, P.D.; Corsini, A.; et al. Statin-associated muscle symptoms: Impact on statin therapy-European Atherosclerosis Society Consensus Panel Statement on Assessment, Aetiology and Management. Eur Heart J. 2015, 36, 1012–1022. [Google Scholar] [CrossRef]
- Yusuf, S.; Bosch, J.; Dagenais, G.; et al. Cholesterol Lowering in Intermediate-Risk Persons without Cardiovascular Disease. N Engl J Med. 2016, 374, 2021–2031. [Google Scholar]
- Gencer, B.; Rodondi, N.; Auer, R.; et al. Reasons for discontinuation of recommended therapies according to the patients after acute coronary syndromes. Eur J Intern Med. 2015, 26, 56–62. [Google Scholar] [CrossRef]
- Ascher, S.B.; Charlton, B.R.; Redberg, R.F. Low-Density Lipoprotein Cholesterol Levels and Statin Treatment-A Moving Target? JAMA Intern Med. 2016, 176, 1113. [Google Scholar][Green Version]
- Gencer, B.; Laaksonen, R.; Buhayer, A.; Mach, F. Use and role of monoclonal antibodies and other biologics in preventive cardiology. Swiss Med Wkly. 2015, 145, w14179. [Google Scholar] [CrossRef]
- Tice, J.A.; Kazi, D.S.; Pearson, S.D. Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Inhibitors for Treatment of High Cholesterol Levels: Effectiveness and Value. JAMA Intern Med. 2016, 176, 107–108. [Google Scholar]
- Shrank, W.H.; Barlow, J.F.; Brennan, T.A. New Therapies in the Treatment of High Cholesterol: An Argument to Return to Goal-Based Lipid Guidelines. JAMA 2015, 314, 1443–1444. [Google Scholar] [CrossRef]
- Roffi, M.; Patrono, C.; Collet, J.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016, 37, 267–315. [Google Scholar]
- Baigent, C.; Blackwell, L.; Emberson, J.; et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010, 376, 1670–1681. [Google Scholar]
- Cannon, C.P.; Braunwald, E.; McCabe, C.H.; et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004, 350, 1495–1504. [Google Scholar]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 130, e344–426. [Google Scholar]
- Gencer, B.; Nanchen, D. Identifying familial hypercholesterolemia in acute coronary syndrome. Curr Opin Lipidol. 2016, 27, 375–381. [Google Scholar] [CrossRef]
- Cannon, C.P.; Blazing, M.A.; Giugliano, R.P.; et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med. 2015, 372, 2387–2397. [Google Scholar]
- Navarese, E.P.; Kolodziejczak, M.; Kereiakes, D.J.; Tantry, U.S.; O’Connor, C.; Gurbel, P.A. Proprotein Convertase Subtilisin/Kexin Type 9 Monoclonal Antibodies for Acute Coronary Syndrome: A Narrative Review. Ann Intern Med. 2016, 164, 600–607. [Google Scholar]
- Robinson, J.G.; Farnier, M.; Krempf, M.; et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015, 372, 1489–1499. [Google Scholar] [CrossRef] [PubMed]
- Sabatine, M.S.; Giugliano, R.P.; Wiviott, S.D.; et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015, 372, 1500–1509. [Google Scholar] [CrossRef] [PubMed]
- Kamani, C.H.; Gencer, B.; Montecucco, F.; et al. Stairs instead of elevators at the workplace decreases PCSK9 levels in a healthy population. Eur J Clin Invest. 2015, 45, 1017–1024. [Google Scholar] [PubMed]
- Zhang, Y.; Liu, J.; Li, S.; et al. Proprotein convertase subtilisin/kexin type 9 expression is transiently up-regulated in the acute period of myocardial infarction in rat. BMC Cardiovasc Disord. 2014, 14, 192. [Google Scholar] [CrossRef]
- Gierens, H.; Nauck, M.; Roth, M.; et al. Interleukin-6 stimulates LDL receptor gene expression via activation of sterol-responsive and Sp1 binding elements. Arterioscler Thromb Vasc Biol. 2000, 20, 1777–1783. [Google Scholar] [CrossRef]
- Mayne, J.; Dewpura, T.; Raymond, A.; et al. Plasma PCSK9 levels are significantly modified by statins and fibrates in humans. Lipids Health Dis. 2008, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Berthold, H.K.; Seidah, N.G.; Benjannet, S.; Gouni-Berthold, I. Evidence from a randomized trial that simvastatin, but not ezetimibe, upregulates circulating PCSK9 levels. PLoS ONE 2013, 8, e60095. [Google Scholar] [CrossRef] [PubMed]
- Dubuc, G.; Chamberland, A.; Wassef, H.; et al. Statins upregulate PCSK9, the gene encoding the proprotein convertase neural apoptosis-regulated convertase-1 implicated in familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2004, 24, 1454–1459. [Google Scholar] [CrossRef] [PubMed]
- Hlatky, M.A.; Greenland, P.; Arnett, D.K.; et al. Criteria for evaluation of novel markers of cardiovascular risk: A scientific statement from the American Heart Association. Circulation 2009, 119, 2408–2416. [Google Scholar] [CrossRef]
- Leander, K.; Malarstig, A.; Van’t Hooh, F.M.; et al. Circulating Proprotein Convertase Subtilisin/Kexin Type 9 (PCSK9) Predicts Future Risk of Cardiovascular Events Independently of Established Risk Factors. Circulation 2016, 133, 1230–1239. [Google Scholar] [CrossRef]
- Ridker, P.M.; Rifai, N.; Bradwin, G.; Rose, L. Plasma proprotein convertase subtilisin/kexin type 9 levels and the risk of first cardiovascular events. Eur Heart J. 2016, 37, 554–560. [Google Scholar] [CrossRef]
- Jacobson, T.A.; Ito, M.K.; Maki, K.C.; et al. National lipid association recommendations for patient-centered management of dyslipidemia: Part 1—Full report. J Clin Lipidol. 2015, 9, 129–169. [Google Scholar] [CrossRef]
| Familial hypercholesterolaemia (e.g., PCSK9 gene mutations) |
| High levels of low-density and small dense lipoprotein cholesterol |
| High triglycerides |
| Physical inactivity |
| Inflammation (e.g., C-Reactive Protein) |
| Acute phase of acute coronary syndromes |
| Long chest pain duration |
| Use of statins or fibrates |
| Insulin resistance |
| Women and postmenopause |
| HIV-infected patients |
| Peripheral arterial disease |
| 1. Proof of concept—do novel marker levels differ between subjects with and without outcome? | Probable |
| 2. Prospective validation—does the novel marker predict development of future outcomes in a prospective cohort or nested case-cohort/ case-cohort study? | Possible, still controversial |
| 3. Incremental value—does the novel marker add predictive information to established, standard risk markers? | Improbable |
| 4. Clinical utility—does the novel risk marker change predicted risk sufficiently to change recommended therapy? | No data |
| 5. Clinical outcomes—does use of the novel risk marker improve clinical outcomes, especially when tested in a randomized clinical trial? | No data |
| 6. Cost-effectiveness—does use of the marker improve clinical outcomes sufficiently to justify the additional costs of testing and treatment? | No data |
© 2016 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Gencer, B. Should We Measure PCSK9 Levels in Patients with Acute Coronary Syndromes? Cardiovasc. Med. 2016, 19, 249. https://doi.org/10.4414/cvm.2016.00439
Gencer B. Should We Measure PCSK9 Levels in Patients with Acute Coronary Syndromes? Cardiovascular Medicine. 2016; 19(10):249. https://doi.org/10.4414/cvm.2016.00439
Chicago/Turabian StyleGencer, Baris. 2016. "Should We Measure PCSK9 Levels in Patients with Acute Coronary Syndromes?" Cardiovascular Medicine 19, no. 10: 249. https://doi.org/10.4414/cvm.2016.00439
APA StyleGencer, B. (2016). Should We Measure PCSK9 Levels in Patients with Acute Coronary Syndromes? Cardiovascular Medicine, 19(10), 249. https://doi.org/10.4414/cvm.2016.00439




