Rivaroxaban Dissolves Postinfarction Left Ventricular Thrombus
Abstract
Introduction
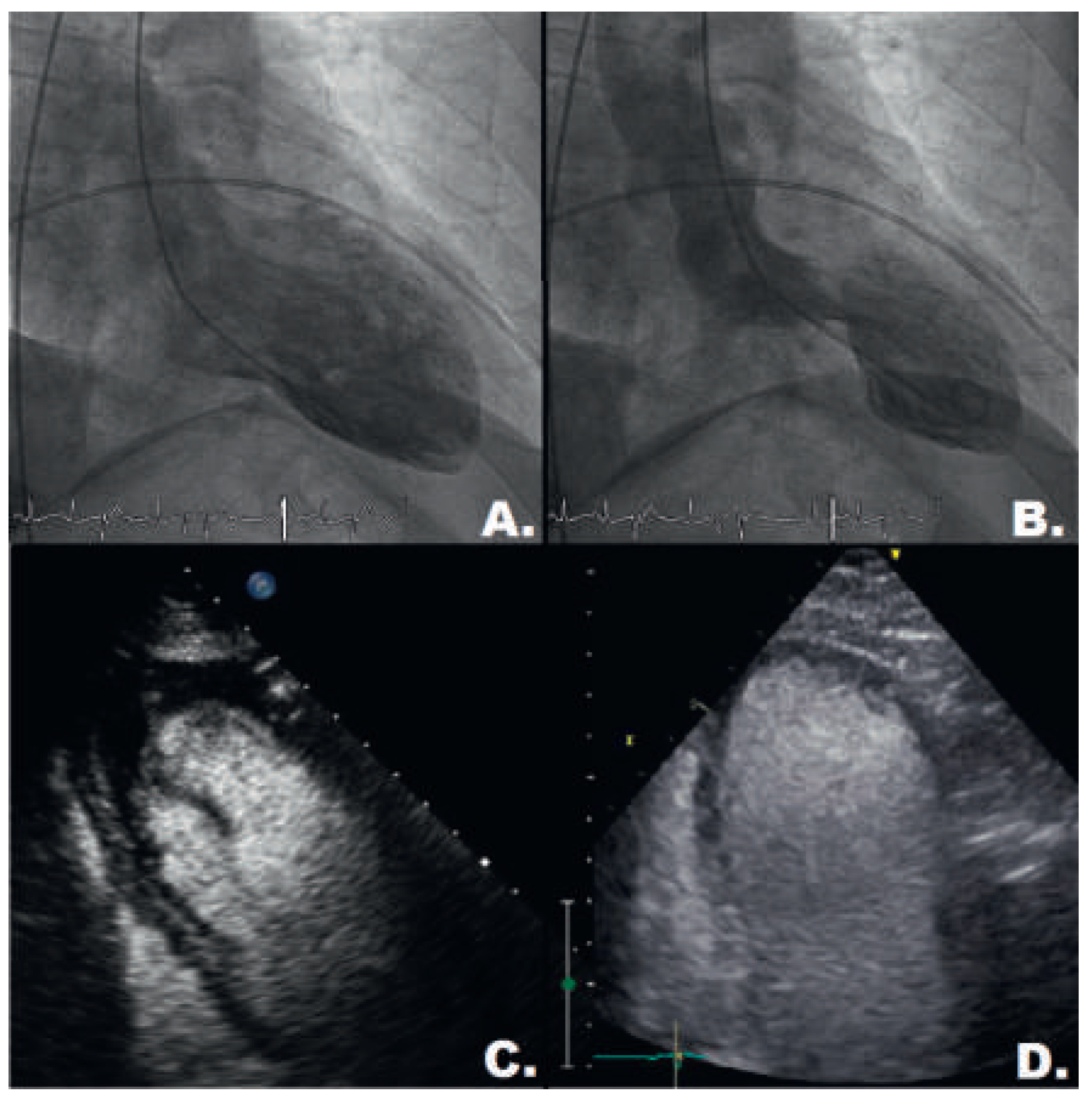
Case description
Discussion
Conclusion
Disclosure statement
References
- Solheim, S.; Seljeflot, I.; Lunde, K.; Bjornerheim, R.; Aakhus, S.; Forfang, K.; et al. Frequency of left ventricular thrombus in patients with anterior wall acute myocardial infarction treated with percutaneous coronary intervention and dual antiplatelet therapy. Am. J. Cardiol. 2010, 106, 1197–1200. [Google Scholar] [CrossRef] [PubMed]
- Osherov, A.B.; Borovik-Raz, M.; Aronson, D.; Agmon, Y.; Kapeliovich, M.; Kerner, A.; et al. Incidence of early left ventricular thrombus after acute anterior wall myocardial infarction in the primary coronary intervention era. Am. Heart J. 2009, 157, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.; Kandalker, H.; Iakobishvili, Z.; Sagie, A.; Imbar, S.; Battler, A.; et al. Leh ventricular mural thrombus after anterior ST-segmentelevation acute myocardial infarction in the era of aggressive reperfusion therapy—Still a frequent complication. Coron. Artery Dis. 2005, 16, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Task Force on the management of STseamiotESoC; Steg, P.G.; James, S.K.; Atar, D.; Badano, L.P.; Blomstrom-Lundqvist, C.; et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2012, 33, 2569–2619. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Lip, G.Y.; De Caterina, R.; Savelieva, I.; Atar, D.; Hohnloser, S.H.; et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012, 33, 2719–2747. [Google Scholar] [PubMed]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef] [PubMed]
- Harder, S. Pharmacokinetic and pharmacodynamic evaluation of rivaroxaban: Considerations for the treatment of venous thromboembolism. Thromb. J. 2014, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Kaku, B. Intra-cardiac thrombus resolution after anti-coagulation therapy with dabigatran in a patient with mid-ventricular obstructive hypertrophic cardiomyopathy: A case report. J. Med. Case Rep. 2013, 7, 238. [Google Scholar] [CrossRef] [PubMed]
- Nagamoto, Y.; Shiomi, T.; Matsuura, T.; Okahara, A.; Takegami, K.; Mine, D.; et al. Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels. 2014, 29, 560–562. [Google Scholar] [CrossRef] [PubMed]
- Padilla Perez, M.; Salas Bravo, D.; Garcelan Trigo, J.A.; Vazquez Ruiz de Castroviejo, E.; Torres Llergo, J.; Lozano Cabezas, C.; et al. Resolution of left ventricular thrombus by rivaroxaban. Future Cardiol. 2014, 10, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Nakasuka, K.; Ito, S.; Noda, T.; Hasuo, T.; Sekimoto, S.; Ohmori, H.; et al. Resolution of left ventricular thrombus secondary to tachycardiainduced heart failure with rivaroxaban. Case Rep. Med. 2014, 2014, 814524. [Google Scholar] [CrossRef] [PubMed]
- Agnelli, G.; Gallus, A.; Goldhaber, S.Z.; Haas, S.; Huisman, M.V.; Hull, R.D.; et al. Treatment of proximal deep-vein thrombosis with the oral direct factor Xa inhibitor rivaroxaban (BAY 59-7939): The ODIXaDVT (Oral Direct Factor Xa Inhibitor BAY 59-7939 in Patients With Acute Symptomatic Deep-Vein Thrombosis) study. Circulation 2007, 116, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Takasugi, J.; Yamagami, H.; Okata, T.; Toyoda, K.; Nagatsuka, K. Dissolution of the left atrial appendage thrombus with rivaroxaban therapy. Cerebrovasc. Dis. 2013, 36, 322–323. [Google Scholar] [CrossRef] [PubMed]
- Hammerstingl, C.; Potzsch, B.; Nickenig, G. Resolution of giant left atrial appendage thrombus with rivaroxaban. Thromb. Haemost. 2013, 109, 583–584. [Google Scholar] [CrossRef] [PubMed]
- Windecker, S.; Kolh, P.; Alfonso, F.; Collet, J.P.; Cremer, J.; Falk, V.; et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014, 35, 2541–2619. [Google Scholar] [PubMed]
- Alexander, J.H.; Lopes, R.D.; James, S.; Kilaru, R.; He, Y.; Mohan, P.; et al. Apixaban with antiplatelet therapy after acute coronary syndrome. N. Engl. J. Med. 2011, 365, 699–708. [Google Scholar] [CrossRef] [PubMed]
- Mega, J.L.; Braunwald, E.; Wiviott, S.D.; Bassand, J.P.; Bhatt, D.L.; Bode, C.; et al. Rivaroxaban in patients with a recent acute coronary syndrome. N. Engl. J. Med. 2012, 366, 9–19. [Google Scholar] [CrossRef] [PubMed]

© 2016 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Azizi, A.; Puricel, S.; Cook, S.; Brugger, N. Rivaroxaban Dissolves Postinfarction Left Ventricular Thrombus. Cardiovasc. Med. 2016, 19, 25. https://doi.org/10.4414/cvm.2016.00381
Azizi A, Puricel S, Cook S, Brugger N. Rivaroxaban Dissolves Postinfarction Left Ventricular Thrombus. Cardiovascular Medicine. 2016; 19(1):25. https://doi.org/10.4414/cvm.2016.00381
Chicago/Turabian StyleAzizi, Assadullah, Serban Puricel, Stéphane Cook, and Nicolas Brugger. 2016. "Rivaroxaban Dissolves Postinfarction Left Ventricular Thrombus" Cardiovascular Medicine 19, no. 1: 25. https://doi.org/10.4414/cvm.2016.00381
APA StyleAzizi, A., Puricel, S., Cook, S., & Brugger, N. (2016). Rivaroxaban Dissolves Postinfarction Left Ventricular Thrombus. Cardiovascular Medicine, 19(1), 25. https://doi.org/10.4414/cvm.2016.00381



