Introduction
Ake Senning, Professor of Surgery at the University of Zurich from 1961 to 1985, was a great protagonist of the pioneering phase of cardiac surgery. His contribution to the treatment of heart diseases consists of several original methods and techniques, extraordinary ideas and intuitions covering a wide spectrum of cardiac pathologies. His work reflects great versatility, multiplicity of interests, extremely wide knowledge and a rigorous scientific background. Already at that time he definitely applied an attitude of multidisciplinary approach in treating patients with heart diseases.
In
Table 1, the most important contributions of Professor Senning to the treatment of cardiac pathologies are listed.
The evolution of cardiac surgery
In the first half of the previous century, some congenital anomalies of the heart (coarctation of the aorta and patent ductus arteriosus) were corrected and other intracardiac defects (like tetralogy of Fallot and other anomalies with decreased pulmonary flow) have been palliated. Furthermore, patients with mitral stenosis benefited from closed mitral commissurotomy.
With the advent of pump oxygenators and cardiopulmonary by-pass in 1953, open-heart surgery began and a large number of new cardiac operations were introduced in the clinical practice.
By 1970, at the end of the pioneering phase of cardiac surgery, the great majority of congenital anomalies and acquired cardiac diseases could be surgically treated, and heart transplantation was offered to selected patients with end-stage heart failure. Later on, consistent improvements and refinements were constantly introduced to increase safety and to make results more predictable. A large variety of strategies, methods and techniques were consolidated, deeply scrutinised and rigorously validated using scientific methods.
In the last 15–20 years, changes in epidemiology of the population requiring treatment for cardiac problems, along with the rapid development of technology and imaging modalities, resulted in a gradual but substantial transformation of cardiac surgical practice.
Strictly related to the aging of the population and to the presence of comorbidities, less invasive or hybrid approaches are nowadays often offered to patients as a reasonable alternative to conventional surgery. Minimally invasive procedures are frequently carried out at any age, in order to decrease the trauma of surgery and to facilitate prompt recovery. Importantly, patients are generally evaluated in a multidisciplinary environment, and responsibilities for decision-making and management are shared among different specialists.
The future
Where are we going? Prediction can be relatively easy regarding some aspects of our profession, because of a number of well established and irreversible trends. For sure, the number of elderly patients with structural heart diseases, atherosclerotic changes in the coronary arteries and other vessels, heart failure and arrhythmias is expected to increase further in the future. This typically high-risk population, often characterised by comorbidities and/or frailty, will represent the overlapping targets of cardiac surgeons and cardiologists, and transcatheter procedures will be the preferred therapeutic modality when feasible.
The heart-team approach has been proven to be effective and convenient, and it is here to stay.
There is no question that the treatment modality will be chosen according to risk assessment, clinical characteristics, anatomical features and wishes of the individual patient (personalised care).
Optimal care can only be offered in institutions where the largest spectrum of therapeutic options is available. Prediction regarding the management of specific cardiac pathologies in the entire population with heart disease (including low- and intermediate-risk patients) is a bit more difficult and certainly still controversial. The expected evolution in the treatment of coronary artery disease, aortic stenosis and mitral regurgitation will be herein discussed.
Coronary artery disease
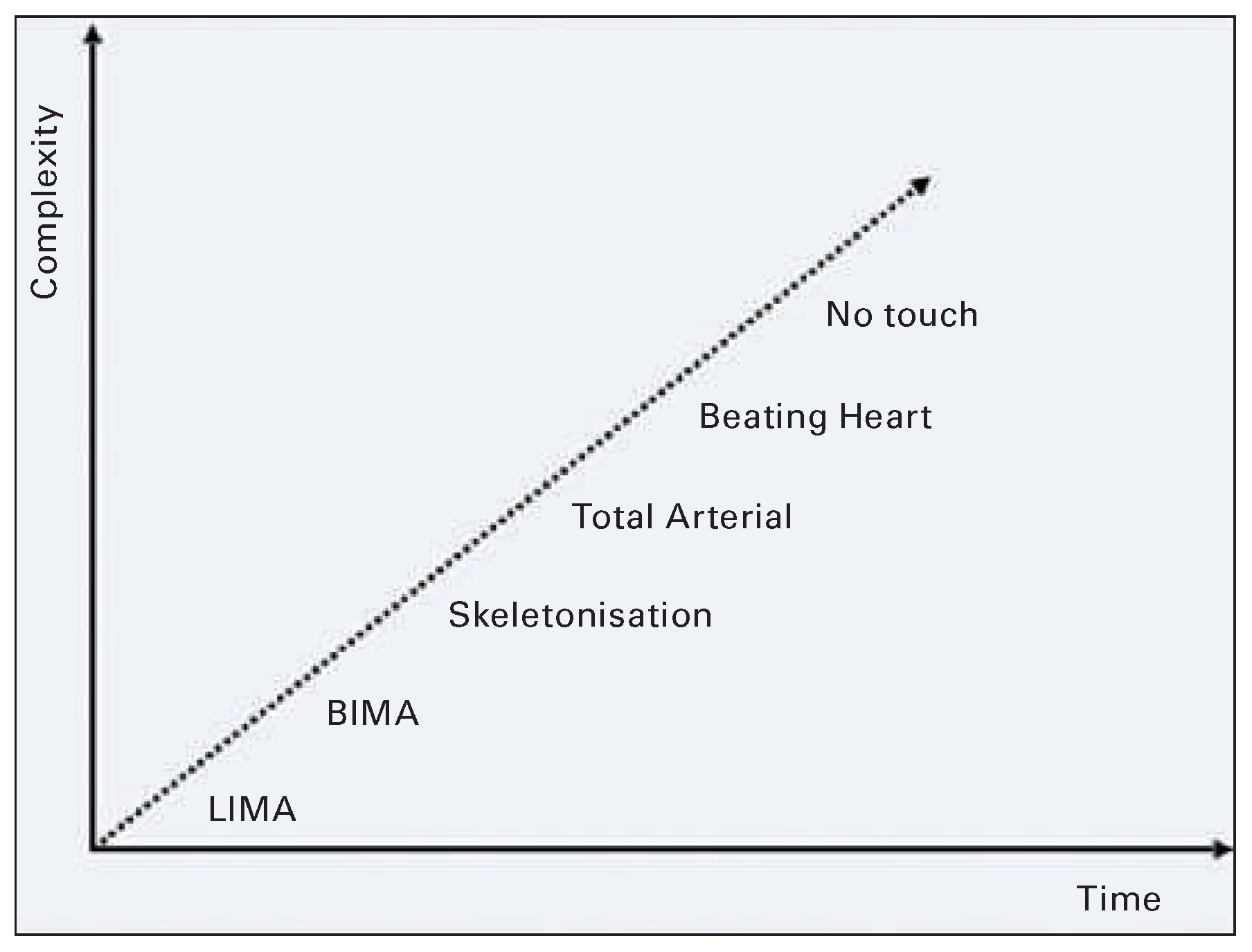
It is likely that coronary surgery (coronary artery bypass grah; CABG) will be gradually disappearing in the future, and percutaneous coronary intervention (PCI) will be the only therapeutic modality for patients with acute and chronic coronary obstructive disease. This statement is somehow in contrast with the current guidelines on myocardial revascularisation. However, it has to be recognised that “progress” in coronary surgery over time has been associated with increased complexity (
Figure 1).
The “ideal” operation should be one which achieves complete arterial revascularisation with use of bilateral skeletonised internal mammary arteries and is performed on a beating heart with a no-touch technique. Such an operation is very complex and technically demanding, time-consuming and not easily reproducible. Intraand postoperative complications are expected to be not negligible even in patients without relevant comorbidities. Early hospital readmission rates after discharge can be up to 10% or even more [
1]. Minimally invasive approaches using robotic technology have been applied by some talented surgeons in an attempt to reduce surgical trauma [
2,
3], but this option is adding further complexity and, therefore, is decreasing reproducibility. Looking at this surgical scenario and considering the ongoing rapid evolution in percutaneous interventions, it is easily predictable that CABG, compared with PCI, will be progressively less competitive in the treatment of coronary artery disease.
Chronic total occlusion (CTO) was considered a condition favouring CABG in the choice of strategy for myocardial revescularisation. Recent data, however, show that in experienced hands CTO can be successfully treated percutaneously in more than 90% of cases [
4].
Aortic stenosis
A variety of alternatives are today available to treat patients with aortic stenosis. According to recent guidelines [
5,
6], transcatheter aortic valve implantation (TAVI) is definitely recommended in inoperable patients with a life expectancy of more than 12 months, and should be considered in high-risk patients. These recommendations are supported by the evidence provided by large prospective randomised trials [
7,
8,
9]. In daily clinical practice, however, intermediate- and low-risk elderly patients are also often offered TAVI rather than surgical aortic valve replacement.
Off-label indications for TAVI are rapidly expanding, and this trend is likely to continue along with improvements in technology and the introduction of new and better devices.
The haemodynamic performance of transcatheter heart valves is already at least equivalent to that of surgical bioprosthesis, The safety profile, in terms of mortality and stroke, is gradually improving and will be mostly solved in the near future. Progress in valve technology will lead to the almost complete disappearance of paravalvular regurgitation, as suggested by the promising results obtained with the new generation devices. Vascular complications will be kept to a minimum, mainly a result of the continuous decrease in the profile of transcatheter valves. The incidence of conduction defects is not negligible at present, but it will decrease over time. The durability of the transcatheter valves is anticipated to be similar to that of the surgical bioprostheses.
It is likely that TAVI will be carried out almost exclusively through a transfemoral approach, and transapical TAVI will be exceptional. The postoperative hospital stay will be reduced to only a couple of days for most low- or intermediate-risk patients.
As predicted by Vahanian [
10], in a few years surgical valve replacement will be limited to patients with a contraindication to TAVI or to those who need concomitant cardiac or aortic surgery. It is expected that in the future surgical aortic valve replacement will be carried out almost exclusively with tissue valves, whereas mechanical valves will be implanted only occasionally in special circumstances. Degenerated bioprostheses will be treated with repeated transcatheter valve-in-valve interventions, for which the only anticipated limitation would be the small size of the prosthesis. Sutureless bioprostheses are likely to become the most commonly used devices for surgical aortic valve replacement. Conventional bioprostheses requiring sutures for implantation will become obsolete, as soon as equivalent results with time-saving sutureless valves will be definitely documented.
Mitral regurgitation
In the years to come, degenerative mitral regurgitation will continue to be preferentially treated with an open heart reconstructive operation carried out either through a midline sternotomy or a minimally invasive approach with or without robotic technology. As a matter of fact, surgical mitral valve repair, when performed at the appropriate time, is able to restore normal life expectancy and quality. In reference centres, the repair rate for degenerative mitral regurgitation is close to 100% and the risk of the procedure is negligible.
A great variety of repair techniques can be applied by the surgeon according to individual anatomy to obtain a perfectly competent mitral valve.
Percutaneous methods of mitral repair can only be considered when the surgical risk is excessively high. On the contrary, functional mitral regurgitation will be preferentially treated percutaneously, particularly with the mitral clip. This modality of treatment has been proven to be safe even in patients with poor left ventricular function and a high risk profile. In the clinical context of functional mitral regurgitation, surgical repair is not attractive because it is often associated with a relevant operative risk and a considerable rate of recurrence of mitral regurgitation.
The spectrum of percutaneous methods to manage mitral regurgitation is expected to become wider and includes various annuloplasty devices and systems for transcatheter mitral valve implantation. The complementary role of percutaneous interventions for mitral repair and replacement has been recently discussed by Maisano et al. [
11]. In
Figure 2, the possible future application of the available percutaneous interventions in different clinical subsets is envisaged.
The new specialist
Because of the future scenario in the treatment of cardiac diseases, the speciality of cardiac surgery, as it used to be in the past, is losing its attraction.
Beside the ongoing evolution in therapeutic modalities, there are reasons that discourage the choice of this profession, for instance the paucity of innovations, the limited range of operations and the excessive exposure to external scutiny along with publication of outcomes, as pointed out by Westaby et al. [
12]. Several changes in the profession of cardiac surgery are ongoing and many more are expected to occur. The cardiac surgeon of the future is therefore likely to be different in many aspects from the specialist who has been the product of conventional training. First of all, the new specialist necessarily work in a multidisciplinary environment, continuously interacting with colleagues having different competences and skills (teamwork). It is likely that the practice of cardiac surgery will be exclusively concentrated in large units, where all techniques and technologies are available, and the heart team approach for decision making and treatment is adopted. In such an environment the optimal therapeutic option for an individual patient will be chosen and then delivered. The new specialist will be obliged to acquire new skills and to be an active part of disease-oriented groups. The education should be individually tailored according to the role which has to be played.
Innovations in the treatment of heart diseases require substantial changes in the training of cardiac surgeons, who should be prepared to perform less invasive procedures and to be familiar with transcatheter interventions