Case presentation
An 82-year-old man presented to the emergency department with severe pain and progressive blue discolouration of the left foot. On admission, his blood pressure was 159/58 mm Hg and his heart rate was 43 bpm. On physical examination, the patient had a cold left foot with a marbled pattern. The leftdorsalis pedis and posterior tibial pulses were not palpable and acute occlusion of the popliteal artery was confirmed by Duplex ultrasonography. The patient underwent emergency intra-arterial lysis therapy and embolectomy.
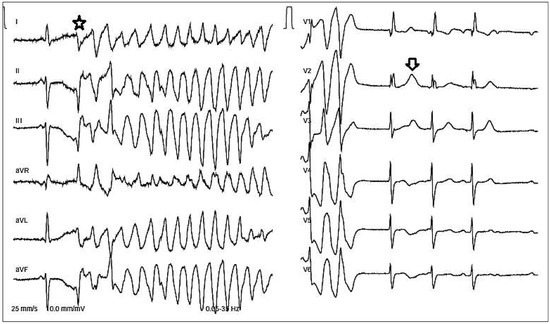
Figure 1.
ECG on admission.
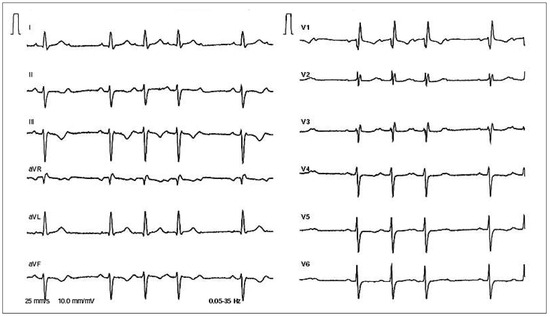
Figure 2.
Follow-up ECG in the emergency department.
Questions
Commentary
The first ECG (Figure 1) essentially shows an episode of nonsustained torsades de pointes (TdP) induced by a premature beat (asterisk) with a relatively narrow QRS. Upon cessation of the episode, three beats with a right bundle branch block morphology can be seen. The first two are most likely junctional (or fascicular) beats (a P wave fused with the QRS complex can be seen with the second of these three beats), whereas the third beat is preceded by a P wave and represents a sinus beat. After the last beat, a blocked P wave can be seen. Moreover, a TU wave augmentation can be observed after the first QRS after the TdP (arrow). The QT interval is difficult to measure in this ECG, but in a subsequent ECG showing second degree atrioventricular (AV) block Mobitz type II with 2:1 AV conduction, it was prolonged (QTc = 501 msec; ECG not shown). The patient received 2 grams of magnesium sulfate intravenously in the emergency department. The occurrence of TdP should always prompt the search for a cause. There was no history of syncope or a family history of sudden death. The patient was not on any QT prolonging drugs. Electrolytes were within normal range. The second ECG (Figure 2) proved useful in the search for a cause in that it shows sinus rhythm with a second degree AV block Mobitz type I (Wenckebach), right bundle branch block and a left anterior fascicular block. The relatively small increments of the PR intervals between beats and the presence of bundle branch block are suggestive of infra-Hisian Wenckebach, but this was not further investigated by electrophysiologic testing.
The pauses after the last conducted P wave (Figure 2) created long-short initiating sequences for TdP. Although the beats before the episode of TdP are not seen on the first ECG, bradycardia-induced QT prolongation (and early after-depolarisation) is the most likely mechanism behind the occurrence of TdP in this patient. The patient subsequently underwent dual-chamber pacemaker implantation. The implantation of an ICD is not indicated because the cause of the tachycardia is reversible, in this case by means of implantation of a pacemaker. At the time of pacemaker implantation, the patient was in second degree AV block Mobitz type II.
It should be noted that, before pacemaker implantation, transthoracic and transoesophageal echocardiography was performed and showed no abnormalities (normal ejection fraction, no thrombus). Because ischaemia is a common cause of polymorphic ventricular tachycardia, coronary angiography was also performed to exclude any coronary artery disease. Genetic testing was not performed in this elderly patient, but long QT syndrome is not ruled out. Unfortunately, no previous ECG was available. Nevertheless, it may be reasonable to avoid QT prolonging drugs in the future.
The patient received oral anticoagulation because systemic embolism as a cause of acute arterial occlusion was suspected. Pacemaker interrogation during follow-up will be used to search for silent episodes of atrial fibrillation.
A final thought that merits consideration is the following: the AV conduction disorder in this patient was most likely preexisting, but its time course is unknown. Although no electrolyte disturbances were detected, it remains speculative whether the “toxic” state during acute limb ischaemia was a facilitator for the occurrence of torsade de pointes.
Disclosures
No financial support and no other potential conflict of interest relevant to this article was reported.
© 2015 by the author. Attribution-Non-Commercial-NoDerivatives 4.0.